Abstract
Purpose
Urinary tract infection (UTI) is a common complication after flexible ureteroscopy (fURS) despite technical precautions to avoid infectious complications. The aim was to investigate incidence and predictive risk factors of UTI following fURS procedure.
Patients and methods
We conducted a retrospective study including consecutive fURS performed in our center from January 2015 to March 2019. The indications were: nephrolithiasis management and diagnosis and conservative treatment of upper urinary tract urothelial carcinomas (UTUC). Since 2015, we had technical precautions to avoid postoperative infectious complications: centralized collection of preoperative urine cultures which are examined daily by an urologist and a service provider, systematic use of ureteral access sheath and application of standardized antibiotic prophylaxis measures. The primary endpoint was occurrence of UTI within 15 days following fURS.
Results
Six hundred and four fURS were included for nephrolithiasis (n = 462) and UTUC management (n = 142). The median (IQR) age in the study cohort was 61(48–68) years, 268 female patients were included (44.4%), the median (IQR) Charlson score was 2(1–4) and single-use fURS were used in 186 cases (30.8%). Postoperative UTI occurred in 41 cases (6.7%). In multivariate analysis, female gender (OR 2.20 [1.02–5.02], p = 0.04), UTI within the last 6 months (OR 2.34 [1.12–5.11], p = 0.02), preoperative polymicrobial urine culture (OR 4.53 [1.99–10.56], p < 0.001) and increased operative time (OR 1.02 [1.002–1.031], p = 0.02) remain associated with postoperative UTI.
Conclusions
In a large cohort study, female gender, prior UTI, increased operative time and preoperative polymicrobial urine culture were associated with the occurrence of postoperative UTI. Limiting operative time and improving our knowledge of polymicrobial urine cultures could reduce the infectious risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The escalating technical refinements in flexible ureteroscopy (fURS) greatly expanded its use and improved its safety. Ureteroscopy is associated with a high success rate and relatively few complications. Flexible ureteroscopy underwent many improvements [1] leading to a widening of its indications with diagnostic and therapeutic management of upper urinary tract pathologies such as urolithiasis [2] and urothelial tumors [3].
In addition to its widely applicable diagnostic and therapeutic benefits, fURS may be associated with noticeable complications, most of which are Clavien grade I or II [4]. Urinary tract infection (UTI) is a common complication after fURS responsible for patient’s suffering, increased hospitalization time and additional costs to society [5]. Few studies have involved risk factors of UTI after ureteroscopy. Most of these studies had several biases including technical heterogeneity in performing ureteroscopy (rigid or flexible ureteroscopy were included) [6, 7] and the populations included were limited to urinary lithiasis [8,9,10,11]. Since 2015, we have performed fURS with a standardized technique including technical precautions to avoid infectious complications of upper urinary tract: centralized collection of preoperative urine cultures which are examined daily by an urologist and a service provider, systematic use of ureteral access sheath and drainage of upper urinary tracts by ureteral stent.
The objective of this study was to investigate predictive risk factors of urinary tract infection (UTI) following flexible ureteroscopy procedure, including all indications, in a tertiary center.
Materials and methods
Study population
We conducted a monocentric retrospective study including all patients who underwent fURS in our university medical institution from January 2015 to March 2019. Exclusion criteria were the use of rigid ureteroscope and antegrade ureteroscopy, to focus on a homogeneous population of retrograde fURS. The study was declared and approved by the Ethics Committee of the Association Française d’Urologie (CERU_2019002). The study also guaranteed compliance at all times to Law Jardé on the Research including Humans Persons (18th November 2016, French Government).
The following variables were recorded in a dedicated database: patient age and gender, body mass index (BMI), age-adjusted Charlson comorbidity index, serum creatinine level (µmol/l), creatinine clearance (ml/min/1.73 m2) estimated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [12], residence (home or institution), presence of comorbidity of interest (indwelling transurethral catheterization, diabetes mellitus, cystinuria and immunosuppression), medical issues within the last 6 months (ureteroscopy, hospitalization, urinary infection/colonization and antibiotherapy), preoperative ureteral stenting, results of preoperative urine culture (sterile, polymicrobial or colonization), indication (lithiasis or tumor), nephrolithiasis size over 20 mm, type of fURS used (single-use ureteroscope or reusable ureteroscope), procedural laterality (unilateral or bilateral), operative time, and postoperative drainage using ureteral stent.
Preoperative urine culture management
Since January 2015, urine cultures were collected centrally by an independent external service provider. All urine cultures were examined daily by the service provider and an urologist. Standardized protocol was defined according to the result of the urine culture: sterile, polymicrobial or positive. Urine culture was obtained 10 days before the procedure. Patients having sterile preoperative urine culture received single-dose prophylactic IV antibiotics consisting of 2 g cefazoline or 5 mg/kg gentamicin in case of penicillin allergy [13]. Patients having polymicrobial preoperative urine culture (defined by a urine culture isolating at least three microorganisms, of which none is predominant) were treated by ceftriaxone 48 h before the intervention which was continued until 1 day after surgery. Those having positive urine culture were contacted by the urologist to assess if they had symptoms of UTI. In asymptomatic cases, according to the specific pathogens identified, a full course of antibiotics was started 5 days prior to surgery until 48 h after the intervention. For those having clinically significant infection, intervention was deferred.
Ureteroscopy technique
Ureteroscopy procedures were programmed and performed by eight urologists for the following indications: nephrolithiasis management, diagnosis and conservative treatment of upper urinary tract urothelial carcinomas. During the study, our instrumentation of reusable fURS included three fibered and two numeric ureteroscopes. In 2017, single-use fURS were integrated (UscopePU3022™, Zhuhai Pusen Medical Technology Company Limited, China) in our endoscopic activities. Ureteroscopy was performed using a standard technique. Hydrophilic-coated ureteral access sheaths were systematically used. Irrigation was provided with saline serum and a pressurized pump (Endoflow, Rocamed©) with pressure at 60–70 cmH20. Lithotripsy was done using the holmium laser system, which is currently the optimum standard for fURS [14].
Endpoints and assessments
The primary endpoint was occurrence of UTI within 15 days following fURS. The diagnosis of UTI included physical exam findings (UTI was suggested by fever > 38 °C, flank pain, costovertebral angle tenderness, vomiting), radiologic features (CT scan was always performed to detect nephritis or pyelo-ureteritis, perirenal fat stranding, obstruction of the upper urinary tracts, abscess or perirenal fluid collection and ureteral stent migration), and laboratory works including blood count and C-reactive protein to find inflammatory signs. In addition, urine culture, blood culture and antimicrobial susceptibility testing were performed in all cases of UTI. According to the previous studies, postoperative UTI was defined as the occurrence of a temperature higher than 38 °C associated with pyuria and/or bacteriuria without any other focal infectious sites. Significant leukocyturia without bacterial growth (aseptic leukocyturia) did not exclude the diagnosis of UTI, because the prevalence of preoperative antibiotic therapy, influencing results of urine culture, could be high. All cases of UTI were reviewed by two separate reviewers (MB and RB) and this demonstrated measurement concordance.
Data analysis
Demographic data, preoperative clinical information, perioperative and follow-up variables were extracted from medical files and recorded in a dedicated database. Descriptive statistics were delineated for the available variables. Quantitative variables were reported in median and interquartile range [IQR] and analyzed by the Mann–Whitney test. Categorical variables were described as numbers and percentages and were analyzed by Fisher’s exact test and Chi square test. Variables with p < 0.20 were then considered to be included in a Firth’s penalized likelihood method in the multivariate logistic regression model to calculate the adjusted ORs and 95% CIs. To detect multicollinearity, we calculated the variance inflation factors of each variable included in the model. No clinically relevant factors and factors with variance inflation factor (VIF) > 3 were excluded. The area under the receiver operating characteristic (ROC) curve was used to evaluate the model discrimination. Statistical analysis was performed using R Version 3.5.3 (The R Foundation for Statistical Computing). For all tests, a two-sided p < 0.05 was considered statistically significant.
Results
A total of 604 consecutive fURS were performed in our institution from January 2015 to March 2019. Forty-one patients (6.7%) had postoperative UTI (patients with UTI) and 563 patients (93.3%) did not develop postoperative infection (patients without UTI).
Clinical and demographic characteristics
Table 1 shows the baseline characteristics. The median (IQR) age in the study cohort was 61 (48–68) years, 268 patients (44.4%) were women, the median (IQR) Charlson score was 2 (1–4) and the median (IQR) body mass index was 25.9 (23.5–30.4). Renal function, history of diabetes mellitus, immunosuppression and cystinuria were comparable between both groups. Hospitalization within the last 6 months was found in 467 patients (77.3%) related to history of complicated pyelonephritis or previous ureteroscopy. Of all patients, 391 (64.7%) had a ureteric stent inserted before surgery. Preoperative double-J stents were inserted in cases with history of complicated UTI or for passive ureteral dilation to facilitate insertion of the ureteral access sheath.
Preoperative urine culture was collected from the majority of patients (n = 602 patients, 99.6%). Most of them were sterile (n = 398, 65.9%). A hundred patients (16.6%) had preoperative polymicrobial urine culture and were treated by ceftriaxone 48 h before the intervention. Finally, 104 patients (17.2%) had preoperative positive urine culture and were treated with a full course of antibiotics according to the specific pathogens identified.
Flexible ureteroscopy characteristics
Flexible ureteroscopy was performed for urolithiasis in 462 cases (76.5%) and for diagnostic purposes or conservative treatment of upper urinary tract urothelial carcinoma in 142 cases (23.5%). These interventions were mostly unilateral (n = 578, 95.7%) and employed a single-use ureteroscope in 186 cases (30.8%). Ureteral access sheath was systematically used for all patients. Median (IQR) operative time was 60 (40–75) min. Postoperative ureteral stenting was performed in 576 patients (95.4%).
Incidence of UTI and predictive risk factors
Of the included 604 patients, 41 patients (6.7%) developed postoperative UTI. The rate of UTI per year was stable during the study period (p = 0.47). The median (IQR) time before postoperative UTI occurred was 2 (1–3) days. Hemodynamic instability was reported in four patients. The evolution of cases was favorable with antibiotic therapy except for one death that occurred after 46 days of admission of the patient to intensive care unit.
In univariate analysis (Table 1), female gender (p < 0.001), urinary tract infection or colonization within the last 6 months (p < 0.001), antibiotherapy within the last 6 months (p < 0.001), preoperative polymicrobial urine culture (p < 0.0001), preoperative colonization urine culture (p = 0.03), lithiasis indication (p = 0.03), kidney stone greater than 20 mm (p < 0.001) and operative time (p < 0.001) were associated with post-ureteroscopy UTI.
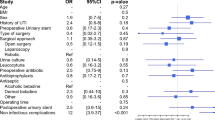
In multivariate logistic regression analysis adjusted for these variables (Table 2 and Fig. 1), female gender (OR 2.20 [1.02–5.02], p = 0.04), UTI within the last 6 months (OR 2.34 [1.12–5.11], p = 0.02), preoperative polymicrobial urine culture (OR 4.53 [1.99–10.56], p < 0.001) and increased operative time (OR 1.02 [1.002–1.031], p = 0.02) remained associated with postoperative UTI.
Discussion
We examined a single-institution contemporary series of consecutive patients undergoing fURS as management of nephrolithiasis and upper urinary tract urothelial carcinoma. Incidence of infectious complication after fURS in the current study was 6.7% going with the previously reported rates ranging from 2 to 28% [15].
We reported that female gender, urinary tract infection/colonization within the last 6 months, polymicrobial preoperative urine culture and increased operating time were associated with UTI after fURS although technical precautions to avoid infectious complication were systematically applied. Female gender and UTI within the last 6 months are well -known risks already described in previous studies [7, 9, 16].
The latest European guidelines [17] have recently evoked the need for highest quality infectious risk management in endourology by suggesting simple principles that allow urologists to reduce urinary infection risk. In our study, we did not find a significant association between positive preoperative urine cultures and postoperative UTI. This finding contrasts with those of several earlier studies, which found positive preoperative urine culture to be a significant predictor of postoperative sepsis in patients undergoing ureteroscopy [6, 9]. Explanation may be that patients were treated before intervention with a full course of antibiotics till the specific pathogens were identified. Nevertheless, polymicrobial urine culture was associated with an increased risk of UTI. The last recommendations [17] do not refer to the management of this common clinical situation. In our study, patients having polymicrobial preoperative urine culture were treated by ceftriaxone 48 h before the intervention. This protocol does not seem to be suitable because as shown in multivariate analysis this subgroup of patients had an increased risk of UTI. A recent review evaluated the management of polymicrobial urine cultures in endourology [18]. The authors concluded that fosfomycin-tromethamine treatment appeared to be a good compromise in this indication. Its spectrum of activity covers most of the bacteria responsible for UTI other than Gram-positive cocci bacteria [19, 20]. As mentioned in recommendations, treatment could be started 48 h before the surgical procedure with a single dose renewed the morning of the intervention. However, these results must be confirmed by subsequent studies.
We also found that there is an association between increased operative time of fURS and infectious complication. Prior studies have also shown that increased operative time has been associated with higher rates of postoperative complication [21, 22]. Our results suggest that increased operative time was associated with an increased risk of subsequent UTI. It is commonly accepted that the duration of the intervention should not exceed 1 h. For longer procedures, systematic drainage of the upper urinary tract and additional antibiotic prophylaxis should be taken into consideration. Ureteral access sheath was systematically used in our center during the study period and we have not been able to report a possible protective effect related to its use.
Ureteroscopes play an important diagnostic and therapeutic role in urology. However, if endoscopes do not attain a sufficiently high level of sterilization, they may cause outbreaks of healthcare-acquired infections. Recently, Ofstead et al have examined 16 ureteroscopes after manual cleaning and sterilization. Tests detected contamination in 100% of ureteroscopes (including hemoglobin, adenosine triphosphate, protein) and microbial cultures were positive for samples from 2 of 16 ureteroscopes [23]. In front of growing concerns regarding the transmission of severe infections through reusable endoscopes [24], it is supposed that operating with a single-use fURS would help avoiding cross-contamination of rURS and thus decrease postoperative infectious complication [25]. We found that there is no significant difference in postoperative UTI rates based on the type of fURS used, single use or reusable. To our knowledge, this is the first study to compare UTI rates according to the type of fURS used.
The main limitation of our study is its retrospective design. However, our series reports extensive data from a large cohort of patients. The homogenicity of the ureteroscopy technique in our series is a major advantage compared to the previously published series: exclusion of rigid ureteroscopes and antegrade ureteroscopy, systematic use of a ureteral access sheath, standardized management of preoperative urine cultures and application of identical antibiotic prophylaxis measures throughout the study period. Another limitation of the study is not to mention the lithiasis composition which may affect the postoperative infection risk and also that stone burden was not objectively assessed by a stone morphometric score. Finally, one of the main strengths of the study is to compare the risk of UTI according to the type of fURS (reusable or single use) used, which to our knowledge, has never been described in the literature.
Conclusion
In a large cohort study, female gender, UTI within the last 6 months, increased operative time and preoperative polymicrobial urine culture were associated with the occurrence of postoperative UTI. In our study, patients having polymicrobial preoperative urine culture had an increased risk of urinary infection despite antibiotic coverage. These data show the insufficiency of current knowledge to define a simple and optimal management of this common situation in urology. The necessity of well-conducted prospective studies is therefore urgent to answer this clinical question: what is the optimal management of preoperative polymicrobial urine culture, such as molecule, dosing and duration of antibiotic therapy and the possible benefit of antibiotic combination versus monotherapy.
References
Johnston WK 3rd, Low RK, Das S (2004) The evolution and progress of ureteroscopy. Urol Clin N Am 31(1):5–13
Türk C, Neisius A, Petřík A, Seitz C, Skolarikos A, Tepeler A, Thomas K (2017) EAU guidelines on urolithiasis. https://uroweb.org/guideline/urolithiasis. Accessed 21 Oct 2017
Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester RJ, Burger M, Cowan NC, Gontero P, Van Rhijn BWG, Mostafid AH, Palou J, Shariat SF (2018) European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2017 update. Eur Urol 73(1):111–122
de la Rosette J, Denstedt J, Geavlete P et al (2014) The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 28:131–139
Moses RA, Ghali FM, Pais VM Jr, Hyams ES (2016) Unplanned hospital return for infection following ureteroscopy-can we identify modifiable risk factors? J Urol 195(4 Pt 1):931–936
Sohn DW, Kim SW, Hong CG, Yoon BI, Ha US, Cho YH (2013) Risk factors of infectious complication after ureteroscopic procedures of the upper urinary tract. J Infect Chemother 19(6):1102–1108
Nevo A, Mano R, Baniel J, Lifshitz DA (2017) Ureteric stent dwelling time: a risk factor for post-ureteroscopy sepsis. BJU Int 120(1):117–122
Senocak C, Ozcan C, Sahin T, Yilmaz G, Ozyuvali E, Sarikaya S, Resorlu B, Oguz U, Bozkurt OF, Unsal A, Adsan O (2018) Risk factors of infectious complications after flexible uretero-renoscopy with laser lithotripsy. Urol J 15(4):158–163
Mitsuzuka K, Nakano O, Takahashi N, Satoh M (2016) Identification of factors associated with postoperative febrile urinary tract infection after ureteroscopy for urinary stones. Urolithiasis 44(3):257–262
Blackmur JP, Maitra NU, Marri RR, Housami F, Malki M, McIlhenny C (2016) Analysis of Factors’ Association with risk of postoperative urosepsis in patients undergoing ureteroscopy for treatment of stone disease. J Endourol 30(9):963–969
Uchida Y, Takazawa R, Kitayama S, Tsujii T (2018) Predictive risk factors for systemic inflammatory response syndrome following ureteroscopic laser lithotripsy. Urolithiasis 46(4):375–381
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI et al (2009) CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration): a new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Antibioprophylaxie in surgery and interventionnelle medicine (adult patients). Actualization (2018) Société Française d’Anesthésie Réanimation
Pierre S, Preminger GM (2007) Holmium laser for stone management. World J Urol 25:235
De S, Autorino R, Kim FJ et al (2015) Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol 67:125–137
Bloom J, Fox C, Fullerton S, Matthews G, Phillips J (2017) Sepsis after elective ureteroscopy. Can J Urol 24(5):9017–9023
Bonkat G (Co-chair), Pickard R (Co-chair), Bartoletti R, Cai T, Bruyère F, Geerlings SE, Köves B, Wagenlehner F, Guidelines Associates, Pilatz A, Pradere B, Veeratterapillay R (2018) EAU Guidelines. Edn. presented at the EAU Annual Congress Barcelona 2019. ISBN 978-94-92671-04-2
Vallée M, Cattoir V, Malavaud S, Sotto A, Cariou G, Arnaud P, Bugel H, Coloby P, Chartier-Kastler E, Bruyère F (2019) Perioperative infectious risk in urology: management of preoperative polymicrobial urine culture. A systematic review. By the infectious disease Committee of the French Association of urology. Prog Urol 29(5):253–262
Caron F, Galperine T, Flateau C, Azria R, Bonacorsi S, Bruyère F et al (2018) Practice guidelines for the management of adult community-acquired urinary tract infections. Med Mal Infect 48(5):327–358
Segre CG, Bianchi E, Cataldi A, Zannini G (1987) Pharmacokinetic profile of fosfomycin trometamol (Monuril). Eur Urol 13(Suppl 1):56–63
Atis G, Gurbuz C, Arikan O et al (2012) Ureteroscopic management with laser lithotripsy of renal pelvic stones. J Endourol 26:983
Skolarikos Andreas, Gross Andreas J, Krebs Alfred, Unal Dogan, Bercowsky Eduardo, Eltahawy Ehab, Somani Bhaskar, de la Rosette Jean (2015) Outcomes of flexible ureterorenoscopy for solitary renal stones in the CROES URS global study. J Urol 194(1):137–143
Ofstead CL, Heymann OL, Quick MR, Johnson EA, Eiland JE, Wetzler HP (2017) The effectiveness of sterilization for flexible ureteroscopes: a real-world study. Am J Infect Control 45(8):888–895. https://doi.org/10.1016/j.ajic.2017.03.016Epub 2017 Jun 15
Epstein L, Hunter JC, Arwady MA et al (2014) New Delhi metallo-beta-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA 312:1447–1455
Chang CL, Su LH, Lu CM et al (2013) Outbreak of ertapenem-resistant Enterobacter cloacae urinary tract infections due to a contaminated ureteroscope. J Hosp Infect 85:118–124
Funding
None. Administrative, technical, or material support: Baboudjian, Boissier, Lechevallier, Gondran-Tellier, Akiki, Abdallah, Gaillet, Delaporte and Karsenty. Supervision: Boissier and Lechevallier.
Author information
Authors and Affiliations
Contributions
Study concept and design: MB, RB and EL. Acquisition of data: MB, RB. Analysis and interpretation of data: MB, RB and EL. Drafting of the manuscript: MB, RB and EL. Critical revision of the manuscript for important intellectual content: Lechevallier. Statistical analysis: BG-T.
Corresponding author
Ethics declarations
Conflict of interest
None of the contributing authors has a conflict of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
Ethical approval
The study was declared and approved by the ethics committee of the Association Française d’Urologie (AFU). The study has guaranteed compliance at all times with the Law of Jardé on the Research including Human Persons (November 18, 2016, French Government).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baboudjian, M., Gondran-Tellier, B., Abdallah, R. et al. Predictive risk factors of urinary tract infection following flexible ureteroscopy despite preoperative precautions to avoid infectious complications. World J Urol 38, 1253–1259 (2020). https://doi.org/10.1007/s00345-019-02891-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02891-8