Abstract
The aim of this study was to elucidate risk factors associated with postoperative febrile UTI after URS for urinary stones. Data from 153 patients undergoing URS for renal and/or ureteral stones between 2011 and 2013 at a single center were reviewed to detect factors predicting postoperative febrile UTI. URS for residual stones was excluded. Postoperative febrile UTI was defined as body temperature >38 °C and was graded according to the Clavien grading system. The definition of pyuria was 10 or more white blood cells per high power field. Median age of the patients was 57 (range 17–89) years. Of the 153 patients, 98 (64.1 %) were male, 10 (6.5 %) had Eastern Cooperative Oncology Group performance status 2 or greater, 14 (9.2 %) had Charlson comorbidity index 3 or greater. Before URS, 69 (45.1 %) had pyuria, 27 (17.6 %) had acute pyelonephritis, 42 (27.5 %) had ureteral stent, and 50 (32.7 %) were treated with antibiotics. After URS, 28 (18.3 %) developed febrile UTI (Clavien grade I, n = 16; grade II, n = 10; grade III, n = 1; grade IV, n = 1). Preoperative pyuria and acute pyelonephritis were significant factors for postoperative febrile UTI (pyuria: odds ratio 3.62, 95 % CI 1.26–8.11, P value 0.017; pyelonephritis: odds ratio 4.43, 95 % CI 1.06–11.16, P value 0.044). Degree of pyuria was likely to be associated with severity of postoperative febrile UTI, and two cases (1.3 %) with severe pyuria developed sepsis. Careful management is needed for patients with preoperative pyelonephritis or pyuria; risk factors for postoperative febrile UTI to avoid sepsis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Technological advancements in ureteroscopy (URS) have resulted in many advantages for treatment of urinary stones, including decreased procedural invasiveness and a higher treatment success rate. URS is now an established standard treatment for urinary tract stones [1]. de la Rosette et al. analyzed 11,885 patients treated with URS between 2010 and 2012 using the Clinical Research Office of the Endourological Society (CROES) database, which consisted of data from 114 centers in 32 countries, and reported that the stone-free rate was 85.6 % and that the postoperative complication rate was 3.5 % [2]. In that study, the most frequent complication was fever (2.8 %), and the majority of complications were Clavien grade 1 or 2. Such a high success rate and low complication rate have resulted in explanation of URS indications to larger and more complicated stones and to elderly patients with significant comorbidities. However, these wider indications might result in a higher incidence of severe complications, including febrile urinary tract infection (UTI), need for blood transfusion, renal dysfunction or septic shock. In fact, Daels et al. analyzed the same CROES database and reported that the risk of complication was highest among elderly patients who presented with comorbidities [3]. Those investigators found that certain risk factors (e.g., diabetes mellitus, anticoagulation use, cardiovascular disease or obesity) were associated with complications; but the influence of preoperative infectious conditions (e.g., pyuria, prior pyelonephritis), antibiotic use or ureteral stent on the complication rate was not mentioned.
Postoperative infectious complications are a frequent and important problem for URS, especially as its indications expand to include elderly or comorbid patients and those patients with large or complicated stones. However, factors associated with infectious complications or sepsis have not been well studied among this cohort defined by wider indications. Therefore, we examined the impact of preoperative conditions on postoperative infectious complications in cases treated with URS for upper urinary tract stones between 2011 and 2013.
Patients and methods
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institution committee and with the 1964 Helsinki declaration and its amendments or comparable ethical standards. Informed consent was obtained from all patients before URS for urinary stones. Between 2011 and 2013, 153 patients underwent URS for renal and/or ureteral stones. Clinical information was prospectively recorded and analyzed retrospectively. Patients undergoing URS for residual stones were excluded from this study.
Preoperative clinical information included age, gender, Eastern Cooperative Oncology Group performance status (PS) [4], Charlson comorbidity index (CCI) [5], body mass index, stone history (primary or recurrent), presence of pyuria, acute pyelonephritis (APN) within 6 months, preoperative ureteral stent and use of antibiotics. Pyuria was defined as 10 or more white blood cells per high power field (HPF). Degree of pyuria was classified into six groups, 0–1/1–4/5–9/10–49/50–99/ ≥ 100 white blood cells per HPF.
Urine culture was performed in most cases with preoperative pyuria and antibiotics before URS was used for all patients who presented with APN or symptomatic pyuria, but was not always used for patients with asymptomatic pyuria. Antibiotic type depended on the results of urine culture or, in some cases, physicians’ discretion.
Operative information included number of stones (single/multiple), presence of kidney stones, stone size, methods of URL (semi-rigid/flexible/combined), operative time, and residual stones. Stone size was calculated as the sum of diameter of each stone in the case of multiple stones. Stone free was defined as no obvious stones or stones less than 2 mm according to X-ray or ultrasound examination at 1 month after URS.
Complications were evaluated according to the modified Clavien grading system [6]. Postoperative febrile UTI was defined as body temperature >38 °C without any symptoms except for those related to the urinary tract, and was classified as grade I (febrile UTI without additional treatment), grade II (febrile UTI with additional antibiotic treatment), grade III (sepsis without intensive care unit management), or grade IV (sepsis with intensive care unit management).
URS was performed under general and lumbar anesthesia in all cases with semi-rigid and/or flexible URS. Renal and/or ureteral stones were fractionated by a Ho:YAG laser. Ureteral sheath and basket catheter were used for extraction of fractionated stones if necessary. A ureteral stent was inserted in all cases at the end of the procedure.
All statistical analyses were performed using JMP 10.0.2 (SAS institute, Cary, NC, USA). Preoperative and operative parameters were compared using the Chi-square test according to presence of postoperative febrile UTI. Multivariate analysis was used to find risk factors for postoperative febrile UTI while adjusting covariates determined by univariate analysis. A P value <0.05 was considered to be statistically significant.
Results
Between 2011 and 2013, 182 URS procedures were performed for patients with upper urinary tract stones, including 29 URS for residual stones. In total, 153 URS procedures for 153 patients, excluding URS used for residual stones, were analyzed. The median age of the patients was 57 (range 17–89) years old. Of these, 28 (18.3 %) had postoperative febrile UTI. Table 1 shows the comparison of clinical information between patients with and without postoperative febrile UTI. Patients with postoperative febrile UTI had a higher rate of preoperative pyuria (P < 0.001), APN (P < 0.001) and preoperative ureteral stent (P = 0.013) than those without postoperative febrile UTI, whereas age, gender, PS, CCI, body mass index and use of preoperative antibiotics were not significantly different between the two groups. No operative variables were significantly different between the two groups (Table 2).
Table 3 shows complications related to URS according to the modified Clavien grading system. Of the 28 postoperative febrile UTI, grade I, II, III, and IV occurred in 16, 10, one, and one case, respectively. Other complications included grade I macrohematuria (7), grade II tamponade (1), grade II urinary retention (1), and grade III complication that required general anesthesia because of difficulty in removing the stent (1). Grade III febrile UTI consisted of sepsis that did not require intensive care unit management and responded to conservative treatment within a few days, while grade IV febrile UTI consisted of sepsis that required intensive care unit management due to the need for continuous hemodiafiltration. A 76-year-old female with PS 2 and CCI 3 died of aspiration pneumonia at 7 days after URS (grade V).
Multivariate analysis adjusting for covariates determined by univariate analysis showed that preoperative pyuria (odds ratio 3.62, 95 % CI 1.26–9.11, P value 0.017) and preoperative APN (odds ratio 4.43, 95 % CI 1.06–11.16, P value 0.044) were significant risk factors for postoperative febrile UTI (Table 4).
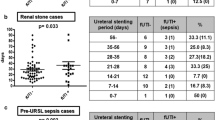
Table 5 shows the association between degree of preoperative pyuria and severity of postoperative febrile UTI. Degree of pyuria was likely to be associated with the severity of febrile UTI. Grade ≥2 febrile UTI in patients without pyuria (white blood cells <10/HPF) and those with pyuria (white blood cells ≥10/HPF) occurred in 2.4 % (2/84) and 14.5 % (10/69), respectively (P = 0.011). Two patients with severe pyuria (white blood cells ≥50/HPF) developed sepsis.
Stone compositions were analyzed in most cases [calcium oxalate 98 (64.1 %)/calcium phosphate 18 (11.8 %)/uric acid 9 (5.9 %)/cystine 4 (2.6 %)/magnesium ammonium phosphate (MAP) 7 (4.6 %)/others 3 (2.0 %)/unknown 14 (9.2 %)].
Discussion
This study examined the impact of preoperative characteristics and operative procedure on postoperative infectious complications. Postoperative fever is the most frequent complication of URS [2, 7], and it is important to identify patients at risk of developing infectious complications of URS, including sepsis, as URS now could be indicated almost all patients without any specific contraindications.
The incidence of postoperative febrile UTI in the present study was 18.3 %, much higher than that seen in previous reports. Sohn et al. analyzed 531 patients who underwent diagnostic URS or URS for stones and reported that 3.8 % of patients had infectious complications [8]. The higher incidence of infectious complications in our patients than that in the Sohn’s study may derive from the difference in the study inclusion criteria, patient characteristics, use of antibiotics or definition of infectious complications between the studies. The present study strictly counted febrile UTI and body temperature >38 °C at any point postoperatively that did not require any additional treatment as grade I febrile UTI. In fact, the rate of grade ≥ II febrile UTI which required additional treatments was 7.8 %. Moreover, the present study did not include diagnostic URS and may have higher rate of complicated cases than Sohn’s study (i.e., diabetes mellitus 31.4 vs. 11.1 %, preoperative ureteral stent 27.5 vs. 19.0 %). Stone size may also influence the complication rate, because a median stone size of 15 mm may be much larger than that in previous reports that studied the complications of URS or endourological procedures [7, 9]. However, stone size was not significantly different between patients with and without UTI in this study (P = 0.139).
In multivariate analysis, preoperative pyuria and APN were significant risk factors for postoperative febrile UTI. Sohn et al. revealed that bacteriuria and catheterization were the strongest risk factors for febrile complications, while age or diabetes mellitus was not a significant factor for febrile complications [8]. Youssef et al. demonstrated that URS with preoperative sepsis had higher complication rates, including postoperative high fever and sepsis, than URS without preoperative sepsis [10]. Although sepsis before URS was not recorded in the present study, these results would be almost compatible with our results that preoperative pyuria and APN was associated with a significantly increased rate of postoperative febrile UTI. The significance of preoperative ureteral stent on infectious complications remains unclear [11–13]. In the present study, preoperative stent was associated with a higher incidence of febrile UTI in univariate analysis but not in multivariate analysis. About half of the patients with preoperative ureteral stent simultaneously presented acute pyelonephritis (APN). APN was a more significant predicting factor for postoperative febrile UTI than preoperative ureteral stent (Table 4), which may make it difficult to determine the infectious risk of ureteral stent itself. Stone diameter, kidney stones, multiple stones or longer operative time, which were considered to predict residual stones or complications in previous studies [12, 14, 15], was not associated with postoperative febrile UTI in our patients, which might indicate that preoperative infectious conditions, like APN or pyuria, have a large impact on postoperative infectious complications.
Moreover, the degree of preoperative pyuria was likely to be associated with postoperative febrile UTI in this study. The incidence of grade ≥2 febrile UTI was 14.5 % in patients with pyuria, and 2.4 % in those without pyuria (P = 0.011). Two patients with severe pyuria presented with sepsis despite preoperative antibiotics. Matsumoto et al. investigated antimicrobial prevention among 353 upper urinary tract examinations, or treatments such as retrograde pyelography, single or double J stenting or percutaneous nephrostomy, and showed that pyuria or hydronephrosis prior to examinations or treatments was an independent risk factor for infectious complications [16]. Pyuria is very easy to recognize, and the degree of pyuria might reflect a potential risk of infectious complications after URS.
Sepsis after URS is a major complication to be avoided. The incidence of sepsis in the present study was 1.3 % (two cases). Only a few studies clearly described the incidence of sepsis after URS or endourological procedures. Geavlete reported that the incidence of fever and sepsis was 1.13 % among 2735 cases of semi-rigid URS at a single center [17]. Eswara et al. reported that the incidence of sepsis was 3.0 % (11/328) after endourological procedures, including 54 cases of percutaneous nephrolithotomy [9]. Youssef et al. reported sepsis developed postoperatively in two patients (1.4 %) with diabetes (one with and one without previous sepsis), and postoperative fever developed in five patients with previous sepsis. [10]. Appropriate antibiotics administration, lower irrigation pressure with unobstructed perioperative urinary drainage, or intraoperative urine or stone culture may be important in preventing postoperative infectious complications, including sepsis [18].
This study had several limitations. It was a retrospective study with a small sample size. The patients in this study were likely to have complicated conditions such as large or impacted stones and comorbid status since our institute is a tertiary referral center for stone treatments. Indications for ureteral stent or antibiotics were not clearly determined and were sometimes used at the physicians’ discretion. Information regarding intraoperative urine or stone culture, which is considered to be important for antibiotics selection to prevent severe infectious complications, was not available in the study.
Conclusions
Preoperative pyuria and APN were associated with postoperative febrile UTI. The degree of pyuria might be a marker of the severity of postoperative febrile UTI; however, this study was retrospective and lacked some important information (e.g., urine culture or indication for ureteral stent or antibiotics). Caution with regards the prevention of severe infectious complications, such as sepsis, should be taken by urologists.
References
European Association of Urology (2015) Guidelines on urolithiasis. http://uroweb.org/guideline/urolithiasis/. Accessed 24 Aug 2015
de la Rosette J, Denstedt J, Geavlete P et al (2014) The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 28:131–139
Daels FP, Gaizauskas A, Rioja J et al (2014) Age-related prevalence of diabetes mellitus, cardiovascular disease and anticoagulation therapy use in a urolithiasis population and their effect on outcomes: the Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol
Arbuck SG, Ivy SP, Setser A et al (1999) The Revised Common Toxicity Criteria: Version 2.0. Available at http://ctep.info.nih.gov
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Ozsoy M, Acar O, Sarica K et al (2014) Impact of gender on success and complication rates after ureteroscopy. World J Urol 2014 (Epub ahead of print)
Sohn DW, Kim SW, Hong CG, Yoon BI, Ha US, Cho YH (2013) Risk factors of infectious complication after ureteroscopic procedures of the upper urinary tract. J Infect Chemother 19:1102–1108
Eswara JR, Shariftabrizi A, Sacco D (2013) Positive stone culture is associated with a higher rate of sepsis after endourological procedures. Urolithiasis 41:411–414
Youssef RF, Neisius A, Goldsmith ZG et al (2014) Clinical outcomes after ureteroscopic lithotripsy in patients who initially presented with urosepsis: matched pair comparison with elective ureteroscopy. J Endourol 28:1439–1443
Lumma PP, Schneider P, Strauss A et al (2013) Impact of ureteral stenting prior to ureterorenoscopy on stone-free rates and complications. World J Urol 31:855–859
Shields JM, Bird VG, Graves R, Gómez-Marín O (2009) Impact of preoperative ureteral stenting on outcome of ureteroscopic treatment for urinary lithiasis. J Urol 182:2768–2774
Rubenstein RA, Zhao LC, Loeb S, Shore DM, Nadler RB (2007) Prestenting improves ureteroscopic stone-free rates. J Endourol 21:1277–1280
El-Nahas AR, El-Tabey NA, Eraky I et al (2009) Semirigid ureteroscopy for ureteral stones: a multivariate analysis of unfavorable results. J Urol 181:1158–1162
Rippel CA, Nikkel L, Lin YK et al (2012) Residual fragments following ureteroscopic lithotripsy: incidence and predictors on postoperative computerized tomography. J Urol 188:2246–2251
Matsumoto M, Shigemura K, Yamamichi F et al (2012) Prevention of infectious complication and its risk factors after urological procedures of the upper urinary tract. Urol Int 88:43–47
Geavlete P, Georgescu D, Niţă G, Mirciulescu V, Cauni V (2006) Complications of 2735 retrograde semirigid ureteroscopy procedures: a single-center experience. J Endourol 20:179–185
Troxel SA, Low RK (2002) Renal intrapelvic pressure during percutaneous nephrolithotomy and its correlation with the development of postoperative fever. J Urol 168:1348–1351
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Mitsuzuka, K., Nakano, O., Takahashi, N. et al. Identification of factors associated with postoperative febrile urinary tract infection after ureteroscopy for urinary stones. Urolithiasis 44, 257–262 (2016). https://doi.org/10.1007/s00240-015-0816-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-015-0816-y