Abstract
Primary central nervous system lymphoma (PCNSL) is a rare form of extranodal non-Hodgkin’s lymphoma and a limited number of cases have been reported from China. This study aimed to investigate the clinicopathological features of newly diagnosed PCNSLs from a single center in eastern China and to identify the potential prognostic factors for overall survival (OS) and progression-free survival (PFS). All consecutive patients with histopathologically diagnosed PCNSLs at our center between January 2003 and October 2017 were recruited. Demographic and clinicopathological data were collected and reviewed retrospectively. The potential risk factors for OS and PFS were identified using the log-rank test and Cox regression analysis. A total of 167 immunocompetent cases were enrolled. The median age was 58 years (range 17–96 years), and the male:female ratio was 3:2. Headache (n = 65; 39%) and cerebral hemisphere (n = 96; 57%) were the most common presenting complaint and location, respectively. Out of 167 cases, 150 cases were diffuse large B cell lymphomas. With a median follow-up of 25 months (range 1–152 ), the median OS and PFS were 37 months (95% CI, 25–49) and 17 months (95% CI, 13–20), respectively. Residual tumor after operation, chemotherapy without HD-MTX and palliative treatment was revealed as independent prognostic markers. Moreover, ECOG > 3, multifocal lesions, and palliative treatment were revealed as unfavorable independent prognostic markers for PFS. In conclusion, Chinese patients with PCNSL have distinct characteristics. Further studies are warranted to confirm the prognostic value of these factors and to optimize treatments for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is a rare form of extranodal non-Hodgkin’s lymphoma (NHL), which is defined as lymphoma restricted to the brain, leptomeninges, cerebrospinal fluid, eyes, or spinal cord without evidences of a systemic lymphoma at the time of diagnosis. PCNSL accounts for only 2–4% of intracranial tumors and 4–6% of extranodal lymphomas in the Western world [1, 2], whereas in China, the incidence has not been reported. Although most patients are immunocompetent, human immunodeficiency virus (HIV) infection, organ transplantation, and other immunocompromised states are the high risk factors [3,4,5]. Diffuse large B cell lymphoma (DLBCL) is the most common subtype of PCNSL (approximately 95%), and the remaining cases are low grade B cell lymphoma, or rarely, T cell lymphoma or Burkitt lymphoma [6, 7]. PCNSL-DLBCL can further be subdivided into germinal center B cell (GCB) and non-germinal center B cell (non-GCB) subtype, depending on the gene expression profiling [8]. Despite remarkable medical progression, the overall prognosis for PCNSL remains poor for the majority of cases and less than 30% of patients can be cured successfully [9]. Although an increasing number of cases have been reported from Western countries, a limited number of cases have been reported from China.
The role of various clinical predictors for the prognosis of PCNSL is controversial. Several prognostic classifications have been proposed for PCNSL to guide risk stratification and optimal treatment selection. The International Extranodal Lymphoma Study Group (IELSG) prognostic score proposes five independent adverse prognostic factors, including age > 60 years, elevated cerebrospinal fluid (CSF) protein level, performance status (ECOG > 1), high lactate dehydrogenase (LDH) level, and deep brain involvement [10]. In this prognostic system, each positive variable is assigned one point and the final score is applied to distinguish various risk groups among PCNSLs. The Nottingham/Barcelona score includes performance status (ECOG ≥ 2), age ≥ 60 years, and extent of brain disease (multifocal and/or meningeal disease) [11]. Using this prediction score, each adverse prognostic factor is assigned one point and a higher final score is associated with a shorter overall survival (OS). The Memorial Sloan-Kettering Cancer Center score proposes Karnofsky scores (KPS ≥ 70) and age ≥ 50 years as adverse prognostic factors [12]. In this prognostic system, the following three distinct prognostic groups significantly distinguish overall survival and failure-free survival: group 1 (age < 50 years), group 2 (age ≥ 50 years; KPS ≥ 70), and group 3 (age ≥ 50 years; KPS < 70). The absolute lymphocyte count–based model proposes three adverse prognostic factors, including ECOG > 1, age > 50 years, and lymphopenia (≤ 875/μL) [13]. In this prognostic system, one point is assigned to each factor and the final score indicates the prognosis. A number of other prognostic factors (such as immunophenotyping) have been proposed, but most of these are not uniformly reported.
In this study, we conducted a retrospective analysis on 167 immunocompetent cases with PCNSL who were consecutively diagnosed between January 2003 and October 2017 in our center. We aimed to specify the clinicopathological features and evaluate the potential prognostic factors for overall survival and progression-free survival (PFS) of these PCNSLs.
Methods
Patient selection
All consecutive cases of PCNSL that were histopathologically diagnosed between January 2003 and October 2017 were collected from the pathology database of the Second Affiliated Hospital, School of Medicine, Zhejiang University, China. The diagnosis of PCNSL was confirmed by two pathologists, and agreements were reached on each patient. To exclude systemic lymphoma, all patients received bone marrow aspirate and biopsy, whole-body CT scan or PET/CT, and a testicular ultrasound evaluation for elderly male patients. Lymphomas with evidence of systemic lymphomas or relapsed lymphomas were excluded. This study obtained ethical approval by the Human Ethics Committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University, China. An informed consent was obtained from all individual participants included in the study.
Demographic and clinical data
Demographic data and clinical features of all patients were collected retrospectively from the medical record, including age, sex, initial neurologic symptoms, performance status (ECOG), HIV status, absolute lymphocyte count (ALC), LDH, CSF protein level, immunohistochemical profile, location of lesions, size of lesions, number of lesions, biopsy type, surgical resection and outcomes, and treatments. The location, number, and size of lesions were evaluated by magnetic resonance imaging (MRI) for all patients. Deep brain involvement (corpus callosum, basal ganglia, periventricular region, brainstem, and/or cerebellum) was determined as described by the IELSG [10].
Histology and immunohistochemistry
The specimens were routinely preserved in 10% neutral buffered formalin and then embedded in paraffin. All immunohistochemical stains were performed using 4-μm paraffin tissue sections with the two-step method. For CD10, Bcl-6, MUM-1, and Bcl-2, positive staining in more than 25% of lymphoma cells was considered positive. PCNSL was further subdivided into GCB and non-GCB groups as proposed by Hans et al. [8]. Briefly, the Hans algorithm depends on Bcl-6, MUM-1, and CD10 immunoexpression. The phenotype of non-GCB was defined as (CD10−, Bcl-6+, MUM-1+) or (CD10−, Bcl-6−, MUM-1+). The GCB phenotype was defined as (CD10+, Bcl-6+/−, MUM-1+/−) or (CD10−, Bcl-6+, MUM-1−).
Treatment data
Between January 2003 and October 2017, treatment choices and therapy dosing for each patient with PCNSL were physician dependent because these cases were scattered throughout the departments of neurology, oncology, radiotherapy, and hematology. Treatment options also changed as treatment development. Data of initial treatments were obtained, dividing into palliative treatment, radiotherapy alone, chemotherapy alone, or a combination of them. Cycles and regimens of chemotherapy as well as radiotherapy protocol were recorded.
Outcomes data
Follow-up data was obtained from patient records or by telephone. PFS and OS were taken as the endpoint in this study. The day of the last follow-up was April 30, 2018. OS was assessed from the date of first diagnosis until the date of last follow-up or death. PFS was calculated from the date of first diagnosis to the date of progression, relapse, death, or last contact.
Statistical analysis
Categorical parameters between groups were compared using the chi-square test. The OS and PFS were estimated by the Kaplan-Meier’s method. Survival distributions according to potential prognostic factors were compared using univariate analysis by the log-rank test. All variables with p values less than 0.10 in the univariate analysis were involved in the multivariate analysis, using the Cox proportional hazards model to further investigate the relationship between prognostic factors. A formal cutoff point was calculated, using the receiver operating characteristic (ROC) curve analysis to determine the optimal values (age, tumor size, ECOG, ALC, LDH, CSF protein level) that were most strongly associated with OS. All statistical analyses were conducted by SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL). All differences were interpreted as statistically significant when p < 0.05.
Results
Demographic and clinical data at diagnosis
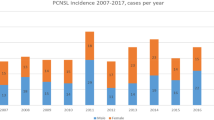
A total of 183 patients with PCNSL were identified in our pathology database. All patients were HIV negative and had no history of immunosuppressive diseases. Thirteen patients were excluded due to the evidences of systemic non-Hodgkin’s lymphoma with brain involvement, and three patients were excluded due to relapsed specimens without initial biopsy records in our hospital. Finally, a total of 167 patients were involved in our analyses. The median age at diagnosis was 58 years (range 17–96). The male:female sex ratio was 3:2 (100:67). The prevalence increased with age, reaching a peak in the age range of 60–69 years in both genders as shown in Fig. 1. All patients underwent a diagnostic biopsy procedure. A total of 62 (37%) patients underwent a gross total resection of their mass, 43 (26%) patients underwent an incisional biopsy, and 62 patients (37%) underwent a stereotactic biopsy. No cases of lymphoma were diagnosed based on the cerebrospinal fluid analysis. A total of 39 patients (23%) received steroids prior to the diagnosis. The mean symptom duration was 81 days (range 7–1833). Initial presentations of the 167 cases are summarized in Table 1. Headache (n = 65; 39%) and motor symptoms (n = 53; 32%) were the most common symptoms, while B symptoms (n = 4; 2%) were rare.
Neuroimaging studies
The number, size, and location of the lesions were determined from the evaluations of cranial magnetic resonance studies. The locations of all masses are summarized in Table 2. The cerebral hemisphere (n = 96; 57%) was the most commonly involved site, in which the frontal lobe (n = 53; 32%) was the most common lobe, followed by basal ganglia and thalamus (n = 43; 26%). Only four lesions (2%) located in leptomeninges and three lesions (2%) located in spine. Multifocal lesions were observed in 73 patients (44%). Deep brain involvement (corpus callosum, basal ganglia, periventricular region, brainstem and/or cerebellum) was involved in 65% of the patients (n = 109). Most of these lesions were small, with 11% of lesions (n = 18) larger than 5 cm.
Pathology examination
The pathological types of 167 cases are summarized in Table 3. In the histopathological review, 160 cases (96%) were B cell lymphoma, and seven cases (4%) were T cell lymphoma. Diffuse large B cell lymphoma (n = 150; 90%) was the most common pathological type. Eighty-six percent (112/130) of these cases were positive for MUM-1 staining, 76% (94/124) of these cases were positive for Bcl-6 staining, 59% (63/107) of these cases were positive for Bcl-2 staining, and 16% (21/133) of these cases were positive for CD10 staining. The Hans algorithm indicated that 100 cases (81%) belonged to the non-GCB subtype and only 23 cases (19%) belonged to the GCB subtype among the 123 cases examined.
Treatments
Treatment information was available for 90% (151/167) of these patients. Among the 151 patients, 137 (91%) cases were treated with curative intention, whereas 14 (9%) patients received palliative treatment due to advanced age, poor performance status, or rapid disease progression. Finally, 25 patients (17%) received radiotherapy alone as an initial treatment, 47 patients (31%) received chemotherapy alone as an initial therapy, and 65 patients (43%) were treated with both radiotherapy and chemotherapy as the initial therapy. No patients received autologous stem cell transplantation (ASCT). Radiotherapy was given in 1.8–2-Gy fractions for a maximum dose of 40-Gy whole brain irradiation and additional 1.8–2-Gy fractions were given for a maximum dose of 10-Gy boost to the tumor bed. Among the 112 patients who received chemotherapy, most patients (n = 75; 67 %) were given high-dose methotrexate (HD-MTX ≥ 3.5 g/m2), and 31 patients (34%) were treated with rituximab as part of the initial therapy. Other treatment options included CHOP-like regimens (n = 6; 5%) and temozolomide alone (n = 10; 9%), and the data for the remaining 21 patients were not available. Among the 65 patients who received combined therapy, 34 patients received chemotherapy prior to radiotherapy and 31 patients received chemotherapy after radiotherapy.
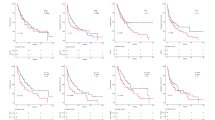
Prognostic factors and overall survival
All patients achieved sufficient follow-up data available for analysis. With a median follow-up of 25 months (range 1–152), 85 patients died and the median OS was 37.0 months (95% CI, 25.1–48.9). The 1-year, 3-year, and 5-year OS probability rates were 72% (95% CI, 68–76%), 50% (95% CI, 46–54%), and 35% (95% CI, 30–40%), respectively. A univariate analysis was performed separately for 18 potential prognostic factors. These factors included age, gender, multifocal lesions, deep brain involvement, biopsy type, gross total resections, tumor size, ECOG, LDH, absolute lymphocyte count (ALC), CSF protein level, Bcl-2 expression, Bcl-6 expression, CD10 expression, MUM-1 expression, Hans pathology phenotype (GCB vs. non-GCB), and treatments as summarized in Table 4. The univariate analysis revealed that age > 72 years, LDH level > 215 U/L, CSF protein level > 90 mg/L, ECOG > 3, multifocal lesions, residual tumor after operation, MUM-1 positivity, chemotherapy without HD-MTX, and palliative treatment were significant predictors of worse OS as shown in Fig. 2. Patients with gross total resection had an improved median OS of 62.0 (95% CI, 15.4–108.6) months when compared with those with residual tumor after operation with a median OS of 33.0 (95% CI, 19.4–46.6) months (p = 0.036). Deep brain involvement was not confirmed as statistically significant variable in the univariate analysis. Multivariable Cox regression analyses revealed that gross total resection, curative intention treatment, and HD-MTX-based chemotherapy were independent prognostic markers with improved OS (p = 0.001, HR = 0.193 (95% CI, 0.073–0.516); p = 0.000, HR = 0.070-0.121; and p = 0.025, HR = 0.374 (95% CI, 0.158–0.886), respectively). In terms of treatment, initial treatments including HD-MTX were associated with a significantly better median OS of 45.0 (95% CI, 40.2–49.8) months when compared with those without HD-MTX with median OS of 23.0 months (95% CI, 5.3–40.7) (p = 0.003).
Kaplan-Meier overall survival curve stratified by various risk factors. Factors including age > 72 years (a), ECOG > 3 (b), LDH level > 215 U/L (c), MUM-1 positivity (d), multifocal lesions (e), residual tumor after operation (f), chemotherapy without HD-MTX (g), and palliative treatment (h) are associated with worse overall survival
Prognostic factors and progression-free survival
At the last follow-up, 113 patients had experienced progression (progression, relapse, or death), and the median PFS was 17.0 months (95% CI, 13.6–20.4). The 1-year, 3-year, and 5-year PFS probability rates were 58% (95% CI, 54–62%), 33% (95% CI, 29–37%), and 20% (95% CI, 16–24%), respectively. As summarized in Table 5, in the univariate analysis, LDH level > 215 U/L, ECOG > 3, multifocal lesions, residual tumor after operation, non-GCB phenotype, and palliative treatment were significant predictors of short PFS as shown in Fig. 3. Multifocal lesions were associated with a shorter median PFS of 12.0 months (95% CI, 6.2–17.8), compared with those with a single lesion with the median PFS of 20.0 months (95% CI, 9.3–30.7) (p = 0.006). ECOG > 3 was associated with a shorter median PFS of 6.0 months (95% CI, 0–12.4), compared with 18.0 months (95% CI, 13.5–22.5) for patients with ECOG ≤ 3 (p = 0.033). In the multivariate analysis, ECOG > 3, multifocal lesions, and palliative treatment were significant independent predictors of short PFS (p = 0.019, HR = 1.26 (95% CI, 1.04–1.53); p = 0.003, HR = 2.07 (95% CI, 1.29–3.33); p = 0.00, HR = 1.14-7.44, respectively).
Kaplan-Meier progression-free survival curve stratified by various risk factors. Factors including LDH level > 215 U/L (a), ECOG > 3 (b), non-GCB phenotype (c), multifocal lesions (d), residual tumor after operation (e), and palliative treatment (f) were associated with short progression-free survival
Discussion
This study investigated the clinicopathological features of PCNSL from a single center in eastern China. The features of these patients are distinct from those reported by a previous study from other countries [5, 14, 15] (Table 6). These patients of our study are more likely to be younger, male predominance, more deep brain involvement, more multifocal lesions, and more symptoms of increased intracranial pressure and focal deficit. In the current study, we demonstrated that gross total resection after operation is a significant independent favorable prognostic marker for OS. Moreover, ECOG > 3 and multifocal lesions are significant independent unfavorable prognostic markers for PFS. However, we failed to demonstrate any association of age and deep brain involvement with prognosis. In terms of treatment, our findings support the application of HD-MTX-based chemotherapy to improve OS.
The prognostic impact of many previously defined factors in PCNSL is controversial. The most consistent prognostic factors are age and performance status [10, 12]. In our retrospective analysis, we also found that ECOG was an independent prognostic factor for PFS. However, we failed to confirm the association between ECOG and OS. Moreover, we did not observe any association of LDH and deep brain involvement with either OS or PFS, which was not in accordance with the IELSG [10]. These differences may be attributed to the relatively distinct characteristics of Chinese patients with PCNSL.
The role of surgery in PCNSLs is commonly restricted to diagnostic biopsy. Aggressive surgery for PCNSL has been discouraged because of the high rates of significant postoperative neurologic deficits and other associated risks. It is believed that attempting surgical resection induces an unnecessary risk, since PCNSL is indeed highly sensitive to chemotherapy and radiotherapy. Moreover, the surgery resection is considered to be impractical because 65% of lesions involve deep brain structures and 44% of lesions are multifocal. At autopsy, lymphoma cells are infiltrative in the brain regions that no lesions were identified on radiographic imaging, indicating that the total surgical resection is impossible [16]. In agreement with these, most retrospective studies have failed to confirm a survival benefit of surgical resections [5, 17]. However, this long-held belief regarding the therapeutic role of surgery resection for PCNSL has been challenged in recent years by a secondary retrospective analysis [18]. In this secondary analysis of the German PCNSL Study Group-1 phase 3 trial, patients with gross or subtotal total resections had significantly longer PFS and OS, compared with biopsied patients. When the results were adjusted for numbers of lesions, the PFS benefit was still statistically significant [18]. Recently, a comprehensive review including 24 articles showed that these 15 articles against surgery resection were of relatively small sample sizes and outdated chemotherapies, on the other side, the 9 articles supporting surgery resection were larger and more recent series [19]. In our series, a high percentage of 63% patients received surgical resection. This may be attributed to the low percentage of preoperative diagnosis of cerebral lymphoma by imaging findings. We found that gross total resections significantly improved OS compared with patients with residual mass, which was confirmed as an independent prognostic factor in the multivariate analysis. Moreover, technical advances in neurosurgery have contributed to the safety of surgical resections of PCNSL [20, 21]. Therefore, future studies are warranted to evaluate tumor removal in PCNSL patients. Despite increasing evidences challenging the traditional concept of surgical resections, these evidences remain insufficient to support its routine use. We propose the reconsideration of tumor removal in the treatment of single lesions amenable to resection, as long as the resection seems safe.
The prognostic value of multifocal lesions (extent of brain disease) has been debated. Multifocal lesions are demonstrated as an independent adverse prognostic factor for OS but not for PFS in the Nottingham/Barcelona score system [11]. In contrast, multifocal lesions are not confirmed as a prognostic factor associated with prognosis in the IELSG prognostic index [10] and in almost all subsequent studies [13]. In our analysis, multifocal lesions were an independent adverse prognostic factor for PFS. Patients with multifocal lesions had a dramatically shorter median PFS, compared with those with a single lesion. In theory, similar to the role of more than one extranodal site in the IPI score for systemic NHL, multifocal lesions (extent of brain disease) correspond with advanced stage, which inevitably indicated a poor prognosis. However, further investigations are required to confirm the prognostic value of multifocal lesions.
Most patients with PCNSL are DLBCL similar to systemic NHLs. However, compared with systemic DLBCLs, PCNSLs have more non-GCB subtype and bear a worse prognosis (13.7 months vs. 30.9 months) [22]. Hans et al. have proposed an algorithm including a cluster of immunohistochemical markers (MUM-1, CD10, and Bcl-6) to differentiate the GCB subgroup from the non-GCB subgroup, the latter corresponding to poor prognosis in systemic lymphoma [8, 23]. However, the prognostic impact of the Hans algorithm on PCNSL is controversial. In certain studies, GCB or Bcl-6 has been determined to be a favorable prognostic marker [24], whereas other studies did not reveal any significant association of these factors with prognosis [6, 25]. In agreement with previous research [14], the majority (81%) of our PCNSLs belonged to the non-GCB subgroup. When compared with the GCB subtype, non-GCB subtype appears to be more adverse in both OS and PFS, although no statistical difference was observed in the multivariate analysis.
So far, there are no standard therapeutic approaches for PCNSLs. The cornerstone of effective chemotherapy is methotrexate. The current treatment strategy is to optimize the frontline therapy, such as combined treatment of HD-MTX with other drugs, WBRT, or ASCT to increase the survival while limit toxicities. Ferreri et al. reported that the combination of HD-MTX with cytarabine has significant advantages over HD-MTX alone in a randomized phase 2 trial [26]. Combination arm has significantly higher complete responses compared with those with MTX alone (46% vs. 18%, p = 0.006). The IELSG32 trial (a multicenter randomized phase 2 trial) evaluated the efficacy of adding rituximab with or without thiotepa to methotrexate-cytarabine combination therapy at initial randomization, inducing three different induction chemotherapy groups: group 1 (methotrexate and cytarabine), group 2 (rituximab, methotrexate, and cytarabine), and group 3 (rituximab, thiotepa, methotrexate, and cytarabine). The IELSG32 trial indicates that more induction drugs are associated with much higher complete response rates and better survival [27, 28]. Whole-brain radiotherapy (WBRT) is an effective treatment method for PCNSL, but WBRT alone is associated with a low OS of only 12–18 months [29, 30]. Therefore, investigations have also assessed the employment of radiotherapy to HD-MTX-based chemotherapy. The G-PCNSL-SG-1 trial (randomized phase 3 trial) evaluated the efficacy of HD-MTX-based chemotherapy with or without WBRT [31]. This trial demonstrated that the WBRT group has a longer PFS than the control group. However, patients in the WBRT group do not have any OS benefit, but have a higher rate of delayed neurotoxicity, which indicates that consolidation therapy of WBRT does not improve OS. The results of the G-PCNSL-SG-1 trial were criticized because of several defects in the study design and undertaking. ASCT has been a standard consolidation therapy for aggressive systemic NHL [32]. In the IELSG32 trial, patients with responsive or stable disease after induction treatment were assigned to the WBRT or ASCT group at the second randomization, and the authors concluded that consolidation therapy of WBRT is as effective as ASCT for PCNSLs [28]. In our study, we confirmed that initial treatments including HD-MTX were associated with a significantly better median OS compared with those without HD-MTX in both univariate and multivariate analyses. However, we found that initial treatments with radio-chemotherapy did not improve OS and PFS when compared with chemotherapy or radiotherapy alone. This finding may be attributed to the fact that the majority of these patients were treated with WBRT as a salvage therapy after the failure of induction chemotherapy, rather than consolidation. Therefore, this conclusion must be cautiously interpreted in light of the retrospective nature of our study.
This study has several limitations including similar biases present in other retrospective studies. Our patients were scattered throughout the departments of neurology, oncology, radiotherapy, and hematology; thus, treatment options and therapy dosing for each patient were physician dependent. Additionally, we did not subclass the chemotherapy regimens for further survival analysis although it is known that patients with different chemotherapy regimens tend to have different prognosis. Moreover, more than half of our patients were not evaluated by lumbar puncture, so we did not include CSF protein levels in the multivariable Cox regression analyses, which may confound the final results, even though CSF protein levels have been found to negatively impact PCNSL [33, 34]. Even so, to the best of our knowledge, this study is the largest series of PCNSL patients reported from China and represents at least some of the characteristics of Chinese patients.
Conclusions
In summary, in this 14-year retrospective study of PCNSL in a single center from China, we retrospectively analyzed the demographic and clinicopathological features of PCNSL and investigated the potential prognostic factors for OS and PFS. Gross total resection is an independent favorable prognostic factor for OS. ECOG > 3 and multifocal lesions were independent adverse prognostic factors for PFS. Initial treatments including HD-MTX are associated with a significantly better median OS. We propose the reconsideration of tumor removal in the treatment of single lesions amenable to resection, as long as the resection seems safe. More studies with much larger patient cohorts are warranted to illuminate the prognostic factors and optimum treatments for Chinese patients with PCNSL.
Abbreviations
- PCNSL:
-
primary central nervous system lymphoma
- NHL:
-
non-Hodgkin’s lymphoma
- HIV:
-
human immunodeficiency virus
- DLBCL:
-
diffuse large B cell lymphoma
- GCB:
-
germinal center B cell
- Non-GCB:
-
non-germinal center B cell
- IELSG:
-
international Extranodal Lymphoma Study Group
- LDH:
-
lactate dehydrogenase
- CSF:
-
cerebrospinal fluid
- OS:
-
overall survival
- KPS:
-
Karnofsky scores
- PFS:
-
progression-free survival
- ALC:
-
absolute lymphocyte count
- MRI:
-
magnetic resonance imaging
- HD-MTX:
-
high-dose methotrexate
- ASCT:
-
autologous stem cell transplantation
References
Dolecek TA, Propp JM, Stroup NE, Kruchko C (2012) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro-Oncology 14(Suppl 5):v1–v49. https://doi.org/10.1093/neuonc/nos218
Patrick LB, Mohile NA (2015) Advances in primary central nervous system lymphoma. Curr Oncol Rep 17(12):60. https://doi.org/10.1007/s11912-015-0483-8
Ruiz A, Post JD, Bundschu C, Ganz WI, Georgiou M (1997) Primary central nervous system lymphoma in patients with AIDS. Neuroimaging Clin N Am 7(2):281
Phan TG, O’Neill BP, Habermann TM (1999) Post-transplant primary central nervous system lymphoma. Ann Neurol 46(3):463–463
Bataille B, Delwail V, Menet E, Vandermarcq P, Ingrand P, Wager M, Guy G, Lapierre F (2000) Primary intracerebral malignant lymphoma: report of 248 cases. J Neurosurg 92(2):261–266. https://doi.org/10.3171/jns.2000.92.2.0261
Raoux D, Duband S, Forest F, Trombert B, Chambonniere ML, Dumollard JM, Khaddage A, Gentil-Perret A, Peoc’h M (2010) Primary central nervous system lymphoma: immunohistochemical profile and prognostic significance. Neuropathology 30(3):232–240. https://doi.org/10.1111/j.1440-1789.2009.01074.x
Sierra del Rio M, Rousseau A, Soussain C, Ricard D, Hoang-Xuan K (2009) Primary CNS lymphoma in immunocompetent patients. Oncologist 14(5):526–539. https://doi.org/10.1634/theoncologist.2008-0236
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Muller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan ZG, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103(1):275–282. https://doi.org/10.1182/blood-2003-05-1545
Norden AD, Drappatz J, Wen PY, Claus EB (2011) Survival among patients with primary central nervous system lymphoma, 1973-2004. J Neuro-Oncol 101(3):487–493. https://doi.org/10.1007/s11060-010-0269-7
Ferreri AJ, Blay JY, Reni M, Pasini F, Spina M, Ambrosetti A, Calderoni A, Rossi A, Vavassori V, Conconi A, Devizzi L, Berger F, Ponzoni M, Borisch B, Tinguely M, Cerati M, Milani M, Orvieto E, Sanchez J, Chevreau C, Dell’Oro S, Zucca E, Cavalli F (2003) Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol 21(2):266–272. https://doi.org/10.1200/JCO.2003.09.139
Bessell EM, Graus F, Lopez-Guillermo A, Lewis SA, Villa S, Verger E, Petit J (2004) Primary non-Hodgkin’s lymphoma of the CNS treated with CHOD/BVAM or BVAM chemotherapy before radiotherapy: long-term survival and prognostic factors. Int J Radiat Oncol Biol Phys 59(2):501–508. https://doi.org/10.1016/j.ijrobp.2003.11.001
Abrey LE, Ben-Porat L, Panageas KS, Yahalom J, Berkey B, Curran W, Schultz C, Leibel S, Nelson D, Mehta M, DeAngelis LM (2006) Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol 24(36):5711–5715. https://doi.org/10.1200/JCO.2006.08.2941
Jang JE, Kim YR, Kim SJ, Cho H, Chung H, Lee JY, Park H, Kim Y, Cheong JW, Min YH, Kim JS (2016) A new prognostic model using absolute lymphocyte count in patients with primary central nervous system lymphoma. Eur J Cancer 57:127–135. https://doi.org/10.1016/j.ejca.2016.01.016
Preusser M, Woehrer A, Koperek O, Rottenfusser A, Dieckmann K, Gatterbauer B, Roessler K, Slavc I, Jaeger U, Streubel B, Hainfellner JA, Chott A (2010) Primary central nervous system lymphoma: a clinicopathological study of 75 cases. Pathology 42(6):547–552. https://doi.org/10.3109/00313025.2010.508786
Dalia S, Forsyth P, Chavez J, Price S, Shah B, Bello C, Sokol L, Pan E, Sotomayor E, Lee JH, Fisher K, Jaglal M (2014) Primary B-cell CNS lymphoma clinicopathologic and treatment outcomes in 89 patients from a single tertiary care center. Int J Hematol 99(4):450–456. https://doi.org/10.1007/s12185-014-1540-z
Lai R, Rosenblum MK, DeAngelis LM (2002) Primary CNS lymphoma: a whole-brain disease? Neurology 59(10):1557–1562
Bellinzona M, Roser F, Ostertag H, Gaab RM, Saini M (2005) Surgical removal of primary central nervous system lymphomas (PCNSL) presenting as space occupying lesions: a series of 33 cases. Ejso 31(1):100–105. https://doi.org/10.1016/j.ejso.2004.10.002
Weller M, Martus P, Roth P, Thiel E, Korfel A (2012) Surgery for primary CNS lymphoma? Challenging a paradigm. Neuro-Oncology 14(12):1481–1484. https://doi.org/10.1093/neuonc/nos159
Labak CM, Holdhoff M, Bettegowda C, Gallia GL, Lim M, Weingart JD, Mukherjee D (2019) Surgical resection for primary central nervous system lymphoma: a systematic review. World Neurosurg. https://doi.org/10.1016/j.wneu.2019.02.252
Cloney MB, Sonabend AM, Yun J, Yang J, Iwamoto F, Singh S, Bhagat G, Canoll P, Zanazzi G, Bruce JN, Sisti M, Sheth S, Connolly ES, McKhann G (2017) The safety of resection for primary central nervous system lymphoma: a single institution retrospective analysis. J Neuro-Oncol 132(1):189–197. https://doi.org/10.1007/s11060-016-2358-8
Yun J, Yang JY, Cloney M, Mehta A, Singh S, Iwamoto FM, Neugut AI, Sonabend AM (2017) Assessing the safety of craniotomy for resection of primary central nervous system lymphoma: a nationwide inpatient sample analysis. Front Neurol 8:478. https://doi.org/10.3389/Fneur.2017.00478
Lin CH, Ku KT, Chuang SS, Kuo SH, Chang JH, Chang KC, Hsu HC, Tien HF, Cheng AL (2006) Comparison of the expression and prognostic significance of differentiation markers between diffuse large B-cell lymphoma of central nervous system origin and peripheral nodal origin. Clin Cancer Res 12(4):1152–1156. https://doi.org/10.1158/1078-0432.CCR-05-1699
Pasqualucci L, Dalla-Favera R (2015) The genetic landscape of diffuse large B-cell lymphoma. Semin Hematol 52(2):67–76. https://doi.org/10.1053/j.seminhematol.2015.01.005
Levy O, DeAngelis LM, Filippa DA, Panageas KS, Abrey LE (2008) Bcl-6 predicts improved prognosis in primary central nervous system lymphoma. Cancer 112(1):151–156. https://doi.org/10.1002/cncr.23149
Liu J, Wang YM, Liu YT, Liu Z, Cui Q, Ji N, Sun SJ, Wang BX, Wang YJ, Sun XF, Liu YB (2017) Immunohistochemical profile and prognostic significance in primary central nervous system lymphoma: analysis of 89 cases. Oncol Lett 14(5):5505–5512. https://doi.org/10.3892/ol.2017.6893
Ferreri AJM, Reni M, Foppoli M, Martelli M, Pangalis GA, Frezzato M, Cabras MG, Fabbri A, Corazzelli G, Ilariucci F, Rossi G, Soffietti R, Stelitano C, Vallisa D, Zaja F, Zoppegno L, Aondio GM, Avvisati G, Balzarotti M, Brandes AA, Fajardo J, Gomez H, Guarini A, Pinotti G, Rigacci L, Uhlmann C, Picozzi P, Vezzulli P, Ponzoni M, Zucca E, Caligaris-Cappio F, Cavalli F, Ielsg (2009) High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet 374(9700):1512–1520. https://doi.org/10.1016/S0140-6736(09)61416-1
Ferreri AJM, Cwynarski K, Pulczynski E, Ponzoni M, Deckert M, Politi LS, Torri V, Fox CP, La Rosee P, Schorb E, Ambrosetti A, Roth A, Hemmoway C, Ferrari A, Linton KM, Ruda R, Binder M, Pukrop T, Balzarotti M, Fabbri A, Johnson P, Gorlov JS, Hess G, Panse J, Pisani F, Tucci A, Stilgenbauer S, Hertenstein B, Keller U, Krause SW, Levis A, Schmoll HJ, Covalli F, Finke J, Reni M, Zucca E, Illerhaus G, Ielsg (2016) Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 3(5):E217–E227. https://doi.org/10.1016/S2352-3026(16)00036-3
Ferreri AJM, Cwynarski K, Pulczynski E, Fox CP, Schorb E, La Rosee P, Binder M, Fabbri A, Torri V, Minacapelli E, Falautano M, Ilariucci F, Ambrosetti A, Roth A, Hemmaway C, Johnson P, Linton KM, Pukrop T, Gorlov JS, Balzarotti M, Hess G, Keller U, Stilgenbauer S, Panse J, Tucci A, Orsucci L, Pisani F, Levis A, Krause SW, Schmoll HJ, Hertenstein B, Rummel M, Smith J, Pfreundschuh M, Cabras G, Angrilli F, Ponzoni M, Deckert M, Politi LS, Finke J, Reni M, Cavalli F, Zucca E, Illerhaus G, Ielsg (2017) Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol 4(11):E510–E523. https://doi.org/10.1016/S2352-3026(17)30174-6
Nelson DF, Martz KL, Bonner H, Nelson JS, Newall J, Kerman HD, Thomson JW, Murray KJ (1992) Non-Hodgkin’s lymphoma of the brain: can high-dose, large volume radiation therapy improve survival? Report on a prospective trial by the Radiation. Therapy Oncology Group (RTOG): RTOG 8315 Int J Radiat Oncol 23(1):9–17. https://doi.org/10.1016/0360-3016(92)90538-S
Shibamoto Y, Ogino H, Hasegawa M, Suzuki K, Nishio M, Fujii T, Kato E, Ishihara SI, Sougawa M, Kenjo M, Kawamura T, Hayabuchi N (2005) Results of radiation monotherapy for primary central nervous system lymphoma in the 1990s. Int J Radiat Oncol 62(3):809–813. https://doi.org/10.1016/j.ijrpbp.2004.12.043
Thiel E, Korfel A, Martus P, Kanz L, Griesinger F, Rauch M, Roth A, Hertenstein B, von Toll T, Hundsberger T, Mergenthaler HG, Leithauser M, Birnbaum T, Fischer L, Jahnke K, Herrlinger U, Plasswilm L, Nagele T, Pietsch T, Bamberg M, Weller M (2010) High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol 11(11):1036–1047. https://doi.org/10.1016/S1470-2045(10)70229-1
Benekou K, Montoto S (2017) Role of stem cell transplant in lymphoma in the era of new drugs. Curr Opin Oncol 29(6):455–459. https://doi.org/10.1097/Cco.0000000000000403
Ghesquieres H, Drouet Y, Sunyach MP, Sebban C, Chassagne-Clement C, Jouanneau E, Honnorat J, Biron P, Blay JY (2013) Evidence of time-dependent prognostic factors predicting early death but not long-term outcome in primary CNS lymphoma: a study of 91 patients. Hematol Oncol 31(2):57–64. https://doi.org/10.1002/hon.2021
Kiewe P, Fischer L, Martus P, Thiel E, Korfel A (2010) Meningeal dissemination in primary CNS lymphoma: diagnosis, treatment, and survival in a large monocenter cohort. Neuro-Oncology 12(4):409–417. https://doi.org/10.1093/neuonc/nop053
Funding
This work was supported by Zhejiang Provincial Key Innovation Team (No. 2011R50015), National Natural Science Foundation of China grants (No. 81572920), National Basic Research Program of China (No. 2013CB911303), and Natural Science Foundation of Zhejiang Province of China (No. LY15H160038).
Author information
Authors and Affiliations
Contributions
XG Yuan analyzed the patient data and wrote the manuscript. Yu-Rong Huang, T Yu, Y Liang, and XH Zhang collected clinical data; Y Xu performed the statistical analysis; Xiao-Ying Zhao designed and supervised the research project. CR Sun analyzed and interpreted the patient data regarding the surgery and evaluations of cranial magnetic resonance (MRI). All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Human Ethics Committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University, China.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
An informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yuan, XG., Huang, YR., Yu, T. et al. Primary central nervous system lymphoma in China: a single-center retrospective analysis of 167 cases. Ann Hematol 99, 93–104 (2020). https://doi.org/10.1007/s00277-019-03821-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03821-9