Abstract
Background
The efficacy of infrahepatic inferior vena cava (IVC) semi-clamping for reducing blood loss during hepatic resection and its safety remain unclear. The aim of this study was to validate the effectiveness of IVC semi-clamping for reducing blood loss during hepatic resection and to confirm its safety.
Methods
Patients who underwent anatomical hepatic resection between January 2011 and May 2018 were analysed by propensity score-matched and multivariate analyses.
Results
Of 437 patients who underwent anatomical hepatic resection, IVC semi-clamping was performed in 196 patients (44.9%; clamping group). A propensity score-matched analysis demonstrated that even though there was no significant difference in the characteristics of the 141 patients in each group, IVC semi-clamping reduced the blood loss during hepatic resection (clamping group versus non-clamping group: 836 ± 123 vs. 1198 ± 124 ml, P = 0.04). Regarding post-operative complications, the multivariate analysis identified IVC semi-clamping as an independent risk factor for acute kidney injury on post-operative day 1 (P = 0.01, odds ratio = 9.23). A significant positive correlation was found between the duration of IVC semi-clamping and an increased level of serum creatinine (sCre) (P = 0.03), and a significant inverse correlation was found between the blood pressure after clamping and an increased level of sCre (P = 0.02). A receiver operating characteristic analysis revealed the duration and mean blood pressure after clamping that indicated a high risk of acute kidney injury to be 116 min and 65 mmHg, respectively.
Conclusion
IVC semi-clamping can reduce blood loss during hepatic resection but still necessitates monitoring in order to avoid acute kidney injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The success of hepatic resection strongly depends on the intraoperative blood loss, as a large amount of intraoperative blood loss and subsequent blood transfusion has been recognized to correlate with post-operative morbidity and the long-term outcomes [1,2,3,4]. One of the principal concerns of liver surgeons is how to reduce blood loss during liver resection.
Blood loss during liver resection can be attributed to two sources: the inflow system, including the hepatic artery and portal vein, and the outflow system, consisting of reflux from the hepatic veins. The intermittent clamping of the portal triad, known as the Pringle manoeuvre, has been widely employed to reduce blood loss from the inflow system [5,6,7]. When substantial blood loss arises under control of the inflow system, injury to the hepatic veins is the main cause [8, 9]. Therefore, several anaesthesiological approaches and outflow vascular clamping to achieve a low central venous pressure (CVP) have been developed in order to reduce blood loss from the outflow system [10, 11]. However, the safety, tolerability and usefulness are widely varied among the approaches.
Some approaches to achieve a low CVP in the surgical field have been reported. Total vascular exclusion (TVE) [12] has been reported as a viable technique, including supra- and infrainferior vena cava (IVC) clamping in addition to the clamping of the portal pedicle. However, the indications of these techniques are limited because of their influence on the systemic haemodynamics, liver damage caused by prolonged ischaemia and complicated aspects of the procedures [12]. Recently, complete IVC clamping of the infrahepatic IVC and its efficacy for reducing the blood loss during hepatic resection have been reported [13, 14]. These results suggest that IVC clamping may be an alternative way to reduce the CVP and blood loss during liver resection. However, substantial limitations regarding its indication and concerns about adverse effects remain because of its influence on the systemic haemodynamics. Semi-clamping of the infrahepatic IVC has been performed as a novel solution to the limitations of complete IVC clamping. To date, however, few studies have examined the effects of semi-clamping of the infrahepatic IVC, with conflicting results reported concerning its efficacy. As such, its safeness remains unclear [15, 16].
The aim of this study was to validate the effectiveness of infrahepatic IVC semi-clamping for reducing blood loss during hepatic resection and to confirm its safety in a large-scale cohort using the propensity score-matched method.
Methods
Study population
A retrospective review was performed of a prospectively maintained hepatic resection database. Patients underwent anatomical hepatic resection between January 2011 and May 2018. Of these, patients who underwent laparoscopic hepatic resection, patients who underwent simultaneous resection of other organs and patients who underwent hepatic resection with extrahepatic bile duct resection and reconstruction were excluded from this study (Fig. 1). The study was approved by the institutional review board.
Patients enrolled in the study. A total of 669 patients underwent anatomical hepatic resection between January 2011 and May 2018. Of these, the patients who underwent laparoscopic hepatic resection, patients who underwent simultaneous resection of other organs and patients who underwent hepatic resection with extrahepatic bile duct resection and reconstruction were excluded from this study. Consequently, a total of 437 patients were enrolled in this study
Surgical strategy and surgical procedures
The indications for hepatectomy and the types of operative procedures were usually determined based on the tumour location, tumour extension and the patients’ liver function. The type of hepatectomy was defined as the resection of liver segments by Couinaud’s definition [17]. Removal of one liver segment or more, excluding the left lateral segment, was defined as major hepatectomy, and left lateral segmentectomy and subsegmentectomy were defined as minor hepatectomies in the present study. The details of the surgical strategy and procedure have been reported previously [18,19,20]. Liver dissection was mainly done using an ultrasonic device. For liver dissection, we basically used the Pringle manoeuvre, with clamping for 15 min followed by a 5-min de-clamping, or the selective hemi-hepatic clamping method if indicated [21]. The amount of blood loss was measured from the aspirator and gauze through the operation.
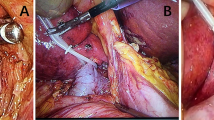
IVC semi-clamping method
IVC semi-clamping has been employed in expectation of CVP reduction and blood loss reduction for cases predicted to have a large amount of blood loss preoperatively or judged to be prone to haemorrhaging intraoperatively. The IVC was isolated and encircled below the liver and taped and then semi-clamped with a tourniquet prior to liver resection. If the systolic blood pressure dropped below 80 mmHg because of central hypovolemia, we loosened the tape gradually. IVC semi-clamping was discontinued when the systolic blood pressure could not be maintained above 80 mmHg even when the clamping tape was loosened. If the patient could not tolerate IVC semi-clamping, transection of the parenchyma was started without IVC semi-clamping. The arterial pressure was measured by puncturing the radial artery, and the mean arterial blood pressure (MAP) was evaluated before and after IVC semi-clamping. Indwelling central venous catheter and monitoring of CVPs were not routinely performed.
Statistical analyses
The Chi-square test was used to analyse categorical variables, whereas the t test was used to analyse continuous variables. When applicable, the results were expressed as mean ± SD. The logistic regression model was used for further evaluations of the multivariate analysis. To avoid bias due to the difference between the clamping and non-clamping groups in patients’ characteristics, surgical types and tumour factors, one-to-one matching was applied using a propensity score analysis with a calliper width equal to 0.05 standard deviations. The sex, age, body mass index (BMI), indication of resection, liver damage, background liver disease, operation type and experience of the surgeon were used in the propensity model. All statistical analyses were performed using the JMP software package, version 14.0 for Mac (SAS Institute Inc., Cary, NC, USA). P < 0.05 was considered to indicate statistical significance.
Results
A Comparison of the clinical characteristics between the IVC semi-clamping group and the non-clamping group in the whole study series
A total of 669 patients underwent anatomical hepatic resection between January 2011 and May 2018. Of these, 437 patients were enrolled in this study (Fig. 1). Of the 437 patients, IVC semi-clamping was performed in 196 (44.9%; clamping group). Semi-clamping of the IVC was attempted in two patients, but they were unable to tolerate it because of hypo-haemodynamics, so liver transection was performed without IVC semi-clamping. The two patients were classified into non-clamping group in the present study. Table 1 shows the comparison of the patients’ characteristics, indication of resection, background liver disease, liver damage and surgical features between the patients with and without IVC semi-clamping among all enrolled patients.
The comparison of the blood loss during hepatectomy and blood transfusion between the groups with and without IVC semi-clamping after propensity score matching
To avoid bias due to the different covariates for the two groups, a propensity score-matched analysis was employed. After one-to-one matching, 141 patients in the IVC semi-clamping group and 141 patients in the non-clamping group had no significant differences in characteristics (Table 1). In the analysis under the case–control method, the patients with IVC semi-clamping showed significantly less blood loss during hepatectomy than those without IVC semi-clamping (846 ± 121 vs. 1196 ± 121 ml, P = 0.04, Table 2). There was also no significant difference in the rate of intra- (13% vs. 13%, P = 0.98) or peri-operative blood transfusion (13% vs. 19%, P = 0.20).
Post-operative arterial blood gas analyses and the renal function
The post-operative results of the arterial blood gas analysis and post-operative changes in the serum creatinine (sCre) levels are listed in Table 3. Regarding the results of the arterial blood gas analysis, including base excess and lactate, no significant differences were noted between the IVC semi-clamping group and the non-clamping group in the matched-pair data set. For the evaluation of the influence of IVC semi-clamping on the post-operative renal function, the increase rate of the sCre levels on post-operative days 1, 3 and 5 compared to preoperative sCre was investigated. The increase rate of more than 2.0 times is diagnosed as acute kidney injury (AKI) according to the definition of acute kidney injury (AKI) of Kidney Disease Improving Global Outcomes (KDIGO) [22]. As a result, IVC semi-clamping was significantly associated with AKI on post-operative day 1 in the matched-pair data set (P = 0.04, Table 3). On days 3 and 5, the significant correlation between IVC semi-clamping and AKI was not found. For further validation of these results, a multivariate logistic analysis was performed in whole study series. This analysis identified IVC semi-clamping as an independent risk factor for AKI at post-operative day 1 (P = 0.01, OR = 9.21, Table 4).
Influence of the duration of IVC semi-clamping and blood pressure after IVC semi-clamping on the post-operative renal function
In the present study, the duration of IVC clamping was 133.3 ± 4.5 min, and the pre- and post-clamping mean arterial blood pressure (MAP) was 85.4 ± 0.8 and 70.7 ± 0.8 mmHg. A significant positive correlation was found between the duration of IVC semi-clamping and increased sCre levels (P = 0.03, Fig. 2a). A receiver operating characteristic (ROC) analysis revealed the optimal cut-off value of the duration of clamping that resulted in a high risk of AKI to be 116 min for AKI (Fig. 2b). A significant inverse correlation was found between the MAP after IVC semi-clamping and increased levels of sCre (P < 0.01, Fig. 2c). In addition, an ROC analysis revealed the optimal cut-off value of MAP after IVC semi-clamping indicating a high risk of AKI to be 65 mmHg for AKI (Fig. 2d).
Influence of the duration of IVC semi-clamping and blood pressure after IVC semi-clamping on the post-operative renal function. A significant positive correlation was found between the duration of IVC semi-clamping and an increased level of serum creatinine (Cre) (P = 0.03, a). A receiver operating characteristic (ROC) analysis revealed the optimal cut-off value of the duration of clamping that resulted in a high risk of AKI to be 116 min (b). A significant inverse correlation was found between the mean arterial blood pressure (MAP) after inferior vena cava (IVC) semi-clamping and increased levels of sCre (P < 0.01, c). An ROC analysis revealed the optimal cut-off value of MAP after IVC semi-clamping indicating a high risk of AKI to be 65 mmHg (d)
Post-operative complications
The incidence of post-operative complications other than AKI is listed in Table 5. The incidence of pleural effusion was found to be more frequent in the IVC semi-clamping group than in the non-clamping group (matched-pair data set, 4% vs. 0%, P = 0.01). Regarding other complications, no significant differences were found according to IVC semi-clamping.
Discussion
The amount of blood loss from the outflow system during hepatic resection is widely accepted to correlate with the CVP [23]. There are two main approaches to reducing the CVP: an anaesthesiological approach, such as via fluid restriction, pharmacological interventions and hypoventilation [24], and outflow vascular (i.e. IVC) clamping in the operative field. Although several manners of IVC clamping [5,6,7, 16], such as TVE [12, 25], complete clamping [13] and semi-clamping [14, 15, 26], have been reported, the efficacy, safety and tolerability have varied among the approaches, and a consensus concerning the optimal method has not been established. The present study successfully demonstrated that the promising method of IVC semi-clamping was able to reduce the blood loss during hepatic resection among patients with various background characteristics using a propensity score-matched analysis. Furthermore, IVC semi-clamping was well tolerated, with intolerability found in only two patients (1.0%). The present results suggest that the IVC semi-clamping may be a useful novel technique for reducing the CVP and that its addition to inflow occlusion may become a standard procedure for controlling haemorrhaging during hepatic resection.
In addition to its effectiveness, the present study demonstrated for the first time the associated risk of renal injury with IVC semi-clamping. Previous studies have reported that even complete IVC clamping could be performed safely with no marked difference in the rate of post-operative acute renal failure between the complete IVC clamping group and the control group [13, 14]. A few studies on semi-clamping IVC also reported that semi-clamping IVC was able to be performed without any side effects [26]. However, most of these studies were designed to demonstrate the effectiveness of the techniques, so the number of patients with IVC complete clamping or semi-clamping was relatively small, ranging from 20 to 65 patients [13,14,15]. The present study demonstrated that IVC semi-clamping was associated with AKI on post-operative day 1 using two different statistical approaches—a propensity score-matched analysis and multivariate logistic regression analysis—to overcome any bias due to the diverse background of our large-scale cohort compared to previous reports.
IVC semi-clamping causes potentially insufficient renal perfusion with a resulting decrease in the cardiac output. However, Uchiyama et al. [26] investigated the indicators of metabolic acidosis, such as the base excess and lactate, before and after semi-clamping and reported no significant differences in acidosis between the two points. The present study also revealed that the base excess and lactate just after operation were not significantly different between the IVC semi-clamping and non-clamping groups. These findings suggest other potential pathogeneses of renal injury in addition to systemic hypoperfusion. One speculation is that the increased renal venous pressure caused by IVC semi-clamping might cause an additional reduction in the renal flow and further degradation of the renal function. Several studies have reported that minimal changes in the serum creatinine could predict the clinical course and prognosis [27, 28]. We therefore feel that identifying the patients at a high risk of renal injury and careful indication specifically for patients at a high risk of renal failure might be required although the compromised renal function on post-operative day 1 was reversible and able to be restored over time by post-operative management in almost all cases in the present study.
The benefits of IVC semi-clamping may include its adjustability. Thus, the duration and the strength of clamping could be tailored for individuals by liver surgeons under monitoring of several haemodynamic parameters. The present study clearly proposes that the duration of IVC semi-clamping be limited to 116 min and the strength of clamping be set to keep the MAP above 65 mmHg in order to prevent post-operative AKI. These concrete and simple cut-off values will be informative for liver surgeons in clinical situations.
Regarding post-operative morbidity, Rahbari et al. reported a potential association between complete IVC clamping and post-operative pulmonary embolisms, indicating serious concerns. In the present study, the incidence of pulmonary embolisms was not found in either the IVC semi-clamping or non-clamping group. During complete IVC clamping, venous return can be maintained only via blood drainage from the inferior phrenic, adrenal, and retroperitoneal veins [29]. One might speculate that passing the venous return through the semi-clamped IVC might prevent this potentially serious adverse event caused by congestion in the veins. Indeed, the incidence of deep vein thrombosis, which is a main cause of pulmonary embolisms, was also very low (0.2%), and no significant difference in its incidence according to the IVC semi-clamping was found.
Several limitations associated with the present study warrant mention. One major limitation is that the indication of IVC semi-clamping was not unified and depended on the surgeons’ consideration and intraoperative findings of a bleeding tendency in this retrospective study. Nevertheless, the present study was able to successfully demonstrate the efficacy of IVC semi-clamping for reducing blood loss during hepatic resection regardless of this bias using propensity score matching. Another limitation is that the CVP during surgery was not routinely monitored in the present study. However, the MAP was identified as an alternative indicator for the strength of IVC semi-clamping. An indwelling central venous catheter carries a considerable risk of complications [30]. Measuring the MAP might be less invasive and easier than measuring the CVP, so the placement of an indwelling central venous catheter does not seem to be essential when performing hepatic resection under IVC semi-clamping. In addition, the present study enrolled few patients with liver cirrhosis, and patients classified as Child–Pugh A comprised 99% of the study population. Therefore, the efficacy and safety of IVC semi-clamping for patients with liver cirrhosis remain unclear. Care should be practiced when IVC semi-clamping is considered to be indicated for patients with liver cirrhosis. Finally, the AUCs were seems to be insufficient in the ROC analysis for the optimal cut-off value of duration and strength of IVC semi-clamping for preventing AKI. Indeed, the AUC was not so high, but the present study firstly proposed the ideal conditions for the technique, including the advised duration and strength of clamping.
Conclusions
IVC semi-clamping is a novel method of reducing blood loss during hepatic resection, although potential AKI must still be monitored. IVC semi-clamping must be performed only when explicitly indicated and under strict conditions, especially for patients at a high risk of renal dysfunction. The results of the present study will aid in the establishment of standard techniques for controlling blood loss during hepatic resection.
References
Yanaga K, Kanematsu T, Takenaka K et al (1988) Hepatic resection for hepatocellular carcinoma in elderly patients. Am J Surg 155:238–241
Nagao T, Inoue S, Goto S et al (1987) Hepatic resection for hepatocellular carcinoma. Clinical features and long-term prognosis. Ann Surg 205:33–40
Jamieson GG, Corbel L, Campion JP et al (1992) Major liver resection without a blood transfusion: is it a realistic objective? Surgery 112:32–36
Yamamoto J, Kosuge T, Takayama T et al (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115:303–309
Belghiti J, Noun R, Malafosse R et al (1999) Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg 229:369–375
Makuuchi M, Mori T, Gunven P et al (1987) Safety of hemihepatic vascular occlusion during resection of the liver. Surg Gynecol Obstet 164:155–158
Man K, Fan ST, Ng IO et al (1997) Prospective evaluation of Pringle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg 226:704–711
Yamamoto Y, Ikoma H, Morimura R et al (2014) Predictive scoring system assessing the need for intraoperative blood transfusions during hepatectomy for hepatocellular carcinoma. Anticancer Res 34:313–318
Yamamoto Y, Shimada K, Sakamoto Y et al (2011) Preoperative identification of intraoperative blood loss of more than 1,500 mL during elective hepatectomy. J Hepatobiliary Pancreat Sci 18:829–838
Huguet C, Addario-Chieco P, Gavelli A et al (1992) Technique of hepatic vascular exclusion for extensive liver resection. Am J Surg 163:602–605
Melendez JA, Arslan V, Fischer ME et al (1998) Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187:620–625
Bismuth H, Castaing D, Garden OJ (1989) Major hepatic resection under total vascular exclusion. Ann Surg 210:13–19
Rahbari NN, Koch M, Zimmermann JB et al (2011) Infrahepatic inferior vena cava clamping for reduction of central venous pressure and blood loss during hepatic resection: a randomized controlled trial. Ann Surg 253:1102–1110
Otsubo T, Takasaki K, Yamamoto M et al (2004) Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery 135:67–73
Ueno M, Kawai M, Hayami S et al (2017) Partial clamping of the infrahepatic inferior vena cava for blood loss reduction during anatomic liver resection: a prospective, randomized, controlled trial. Surgery 161:1502–1513
Kato M, Kubota K, Kita J et al (2008) Effect of infra-hepatic inferior vena cava clamping on bleeding during hepatic dissection: a prospective, randomized, controlled study. World J Surg 32:1082–1087. https://doi.org/10.1007/s00268-007-9445-0
Couinaud C (1957) Etudes Anatomiques et Chiugicales. Masson, Paris, pp 400–409
Okamura Y, Ito T, Sugiura T et al (2014) Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma: a case-controlled study with propensity score matching. J Gastrointest Surg 18:1994–2002
Makuuchi M, Hasegawa H, Yamazaki S (1985) Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet 161:346–350
Yamamoto Y, Ikoma H, Morimura R et al (2014) Clinical analysis of anatomical resection for the treatment of hepatocellular carcinoma based on the stratification of liver function. World J Surg 38:1154–1163. https://doi.org/10.1007/s00268-013-2369-y
Imamura H, Kokudo N, Sugawara Y et al (2004) Pringle’s maneuver and selective inflow occlusion in living donor liver hepatectomy. Liver Transpl 10:771–778
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120:c179–c184
Jones RM, Moulton CE, Hardy KJ (1998) Central venous pressure and its effect on blood loss during liver resection. Br J Surg 85:1058–1060
Hasegawa K, Takayama T, Orii R et al (2002) Effect of hypoventilation on bleeding during hepatic resection: a randomized controlled trial. Arch Surg 137:311–315
Evans PM, Vogt DP, Mayes JT 3rd et al (1998) Liver resection using total vascular exclusion. Surgery 124:807–813
Uchiyama K, Ueno M, Ozawa S et al (2009) Half clamping of the infrahepatic inferior vena cava reduces bleeding during a hepatectomy by decreasing the central venous pressure. Langenbeck’s Arch Surg Dtsch Ges Fur Chir 394:243–247
Chertow GM, Burdick E, Honour M et al (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Lassnigg A (2004) Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 15:1597–1605
Zhou YM, Sui CJ, Zhang XF et al (2016) Anterior approach combined with infrahepatic inferior vena cava clamping right hepatic resection for large hepatocellular carcinoma: a prospective randomized controlled trial. Medicine 95:e4159
Lalu MM, Fayad A, Ahmed O et al (2015) Ultrasound-guided subclavian vein catheterization: a systematic review and meta-analysis. Crit Care Med 43:1498–1507
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial to disclose.
Informed consent
The study was approved by the institutional review board, and each study subject provided their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Imamura, T., Yamamoto, Y., Sugiura, T. et al. Infrahepatic Inferior Vena Cava Semi-Clamping can Reduce Blood Loss During Hepatic Resection but Still Requires Monitoring to Avoid Acute Kidney Injury. World J Surg 43, 2038–2047 (2019). https://doi.org/10.1007/s00268-019-04992-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-04992-2