Abstract
Purpose
Infrahepatic inferior vena cava (IIVC) clamping is beneficial for reducing the amount of bleeding during hepatic surgery, although the associated systemic circulatory deterioration is noticeable. The relationship between changes in the degree of IIVC clamping and postoperative renal function was retrospectively evaluated.
Methods
A total of 59 patients who underwent elective hepatic surgery with surgical IIVC clamping in the two years were analyzed. In 2016, constant 80% clamping of the IIVC was performed (29 cases), and in 2017, hemodynamically adjusted IIVC clamping was performed (30 cases). Intraoperative parameters, including total blood loss and number of blood transfusions, were examined. The use of each vasoactive agents was analyzed. Renal function in the acute postoperative phase was evaluated using serum creatinine (Cr) and estimated glomerular filtration rate (eGFR) values.
Results
Comparison of the two groups showed that bolus doses of both ephedrine and phenylephrine were significantly higher in the 2016 group (P = 0.0221, 0.0017). Continuous doses of dopamine were significantly higher in the 2016 group, while those of noradrenaline were not. Postoperative serum Cr levels relative to baseline (%) were significantly higher in the 2016 group immediately after surgery and on postoperative day (POD) 1 (P = 0.0143, 0.0012). Postoperative eGFR relative to baseline (%) was significantly higher in the 2016 group immediately postoperatively and on PODs 1 and 2 (P = 0.0042, 0.0003, 0.0382).
Conclusion
Hemodynamically adjustable IIVC clamping might be superior to uniformly fixed clamping in preserving renal function without compromising the desired effect on hemostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impaired renal function after hepatic surgery is common. The main mechanism of this is believed to be intraoperative hypoxic damage resulting in acute tubular necrosis [1, 2]. This is caused, for example, by hemodynamic instability secondary to massive intraoperative bleeding [3]. Furthermore, low central venous pressure (CVP) management with restrictive infusion, which is used to minimize bleeding during surgery on this highly vascular organ, has the potential to cause renal hypoperfusion by a dehydration effect [4, 5].
Infrahepatic inferior vena cava (IIVC) clamping is a surgical method used to effectively lower CVP and reduce the amount of bleeding [6]. This effect seems to be popular among surgeons because small amounts of bleeding are well known to lead to better postoperative outcomes after hepatic surgery [7,8,9]. However, the safety of this technique has been questioned in the past [10, 11]. Article have discussed the high incidence of pulmonary embolism and the high rate of in-hospital mortality and reoperation during the postoperative period after hepatic surgery using the total (100%) IIVC clamping procedure. During anesthesia management, there are concerns about the hemodynamic effects of this technique that significantly prevents venous return. When IIVC clamping was an earlier method of total hepatic vascular exclusion (THVE), with complete isolation of hepatic blood vessels by infra- and supra-hepatic IVC clamping with portal triad clamping, hemodynamic disturbance was a critical issue [12]. The resulting systemic hypoperfusion was associated with postoperative dysfunction of abdominal organs including the kidneys [13]. In addition, anesthesia expertise was required for careful circulatory monitoring and large volume infusions.
In our institute, IIVC clamping was introduced in 2016. Initially, the degree of IIVC clamping was fixed at 80%. However, despite successfully reducing the amount of bleeding, the procedure resulted in severe hypotension (systolic blood pressure < 80 mmHg), such that large doses of vasoactive agents were needed to ameliorate the hemodynamic instability. From 2017 onward, the degree of IIVC clamping was adjusted to below 80%, based on the hemodynamic tolerance of each patient. This management protocol of IIVC clamping significantly reduced hemodynamic instability, and systolic blood pressure was maintained above 80 mmHg with only low doses of vasoactive agents. Hence, we hypothesized that changes in the IIVC clamping protocol could affect renal perfusion during surgery. The purpose of this study was to retrospectively examine whether changes in the degree of IIVC clamping in the last two years were associated with postoperative renal functional outcomes.
Methods
The study protocols were approved by the ethics committee of our institute (2017-276). Written, informed consent was obtained from all patients. Clinical data were obtained from the patients’ anesthesia records (CAP-2000 clinical network system; Nihon Kohden, Japan) and medical records (MagaOak; NEC, Japan).
Patients
Data from 133 cases who underwent elective partial and major hepatic resection between 2016 and 2017 at our institute were analyzed. Inclusion criteria were patients who underwent laparotomy for elective hepatic surgery using the IIVC clamping technique. The following cases were excluded: 59 cases in whom IIVC clamping was not performed due to intraperitoneal adhesions or laparoscopic surgery, one case in which IIVC clamping was immediately canceled because of extremely severe hypotension, two cases of exploratory laparotomy for disease progression, two cases with simultaneous surgery at another site (gastric and rectal), and one case of emergency surgery for impending rupture of the lesion. The remaining 68 eligible cases were divided into two groups based on the IIVC clamping management strategy, resulting in 34 cases in each group.
Anesthesia management
Most patients underwent thoracic epidural catheter insertion at the T7/8-8/9 level prior to anesthesia induction. General anesthesia was induced using 1–2 mg/kg propofol and 0.6–1.0 mg/kg rocuronium, followed by endotracheal intubation, and maintained with inhalation of 1.5–2.0% sevoflurane or 4.0–6.0% desflurane in 40–45% oxygen. Mechanical ventilation with a tidal volume of 8–10 ml/kg and respiratory rate of 8–15 breaths/min was adjusted to maintain end-tidal carbon dioxide at 30–40 mmHg. Bolus doses of local anesthetics (0.125–0.375% ropivacaine and/or 0.1–0.25% levobupivacaine) and low doses of opioids (morphine 1–2 mg or fentanyl 100 µg) were infused into the epidural space for intraoperative analgesia. During surgery, arterial blood pressure was continuously monitored using a circulatory index monitoring device (Vigileo/FloTrac®; Edwards Lifesciences, Irvine, CA, USA), and the remifentanil infusion dose was adjusted between 0.05 and 0.4 µg/kg/min to ensure appropriate hemodynamics. In all cases, each anesthesiologist performed the anesthetic protocols to reduce the amount of bleeding. Systemic infusions were restricted until hepatic resection was completed while monitoring CVP or stroke volume variation (SVV). A generally recognized CVP target value of less than 5 mmHg was applied, which was above 10% in the case of SVV [14, 15]. During hepatic resection, the respiratory settings were changed to a low tidal volume setting without positive end expiratory pressure [16]. Vasodilators were not administered intravenously in any case. Bed rotation was performed when requested by the surgeons. Fluid resuscitation was allowed after hepatic resection. Continuous epidural analgesia or intravenous patient-controlled analgesia was used to relieve postoperative pain.
Surgical procedures to reduce bleeding during the hepatic surgery
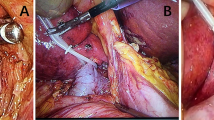
Two kinds of vascular clamping were performed during hepatic resection, portal triad clamping and IIVC clamping. Portal triad clamping by the Pringle maneuver was repeated regularly, with 15 min of ischemic time and 5 min of reperfusion time [17]. As illustrated in a previous article [18], IIVC clamping was performed using a loop-tourniquet system surrounding the vena cava. The degree of IIVC clamping indicated the percentage of occlusion to caval diameter before tightening and was performed continuously from just before resection to its completion. In the year 2016, the degree of IIVC clamping was fixed at 80%. However, at the end of 2016, we discussed with the surgeons regarding the degree of IIVC clamping to maintain hemodynamics at an acceptable level. Later in 2017, the degree of IIVC clamping decreased and was adjusted from a maximum of 80% to less than 80% as follows. Surgeons predicted the optimal degree of clamping of less than 80% based on the IIVC tension, followed the procedure in a staged manner to ensure that the systolic arterial blood pressure exceeded 80 mmHg, and this was confirmed for a minute. When excessive bleeding or breakdown of hemodynamics occurred during the resection, further adjustment was performed.
Changes in hemodynamics after IIVC clamping
Interrupting IVC flow causes significant hemodynamic changes, whereas the hemodynamic effects of portal triad clamping are limited to a 10% reduction in the cardiac index [19]. The cardiovascular reflex after IIVC clamping was not clarified previously, but the THVE method was thoroughly investigated [20]. An example of data measured with a Vigileo/FloTrac system in 2017 was stored to analyze the hemodynamic effects of IIVC clamping. The analysis was performed by averaging three measurements per minute, updated every 20 s. In all cases, to compare the blood pressure drop immediately after IIVC clamping between the 2016 and 2017 groups, five measurements of arterial blood pressure and heart rate at one-minute intervals for five minutes were averaged before and after IIVC clamping combined with portal triad clamping. If data collection was hindered due to the non-invasive blood pressure measurements or blood sampling, the other data were averaged.
Intraoperative use of vasoactive agents
Vasoactive agents were administered when a drop in systolic blood pressure to below 80 mmHg occurred during surgery. If bolus injection failed to ameliorate hypotension, the drug was administered continuously at the discretion of the anesthesiologist. In 2016, the kinds of vasoactive agents used were freely selected; whereas in 2017, the kinds and dosages of vasoactive agents allowed in the previous study were as follows [10]: the first choice was phenylephrine for bolus injection and low-dose noradrenaline (within 0.1 µg/kg/min) for continuous injection. In all cases over the entire study period, ephedrine or phenylephrine was administered by bolus injection. Furthermore, noradrenaline or dopamine was administered by continuous injection in most cases, although there were two cases during 2016 in which a continuous phenylephrine infusion was administered.
Study objective
The objective of this study was to examine whether postoperative renal function was affected by the change in management of the degree of IIVC clamping. Postoperative blood biochemistry tests were routinely performed daily from the day of surgery to postoperative day 2 (POD 2) and day 7 (POD 7), and randomly between them. In three cases during 2016, when POD 7 was a national holiday, measurements were taken on day 8 (POD 8) instead. The primary outcome measure was the absolute values of serum creatinine (Cr) and estimated glomerular filtration rate (eGFR) immediately after surgery and on postoperative day 1 (POD 1) and their values relative to baseline (%). In addition, increased serum Cr levels were diagnosed for acute kidney injury (AKI) using the KDIGO criteria within 48 h after surgery [21]. In these analyses, patients with strong AKI risk factors associated with hepatic surgery were excluded: clinically diagnosed with abnormal serum Cr values or chronic kidney disease (CKD), cirrhosis, or biliary obstruction [3]. Preoperative comorbidities and medications that may adversely affect postoperative renal function were also investigated.
Statistical analysis
All data are expressed as means ± standard deviation (SD) or numbers of patients. Student’s t-test was used for statistical analysis of means if a normal distribution was verified by the Shapiro–Wilk test; otherwise, the Mann–Whitney U test was used. Fisher’s exact test was used for categorical data. GraphPad Prism 7 software (GraphPad Software Inc., San Diego, CA, USA) was used for all analyses, and a P value of < 0.05 was considered significant. Post hoc analysis was performed using G* Power 3.1 software (https://www.gpower.hhu.de/; Heinrich Heine University, Düsseldorf, Germany) with postoperative elevation of serum Cr values from baseline (%) as the primary endpoint, and an adequate power of > 80% was confirmed.
Results
Thirty-four patients who underwent hepatic surgery using the IIVC clamping technique were initially enrolled in each of the two groups. After excluding five patients from the 2016 group and four from the 2017 group because of preoperatively diagnosed renal dysfunction (eight cases) or cirrhosis (one case), 29 and 30 patients in the 2016 and 2017 groups, respectively, were finally analyzed. Table 1 shows the demographic and operative characteristics of the patients. The duration of IIVC clamping was equivalent between the two groups; the average was within 2 h. There was no significant difference between the two groups in terms of anesthetic technique, overall surgery and anesthesia time, and preoperative comorbidities or medications.
Hemodynamic changes in the two types of hepatic vascular clamping.
An example of hemodynamic changes after IIVC clamping is shown in Table 2. There were no effect of bolus administration of vasoactive agents on the results, but a slight amount of noradrenaline (0.01–0.02 µg/kg/min) was administered after T3 onwards. Consistent with hormonal and hemodynamic changes associated with THVE [20], IIVC clamping greatly reduced stroke volume and cardiac output along with CVP, and then greatly increased the systemic vascular resistance index (SVRI) and SVV (T0 to T2). As previously reported [22], the SVRI once increased gradually decreased as portal triad clamping was repeatedly released (T3–T8). The changes in arterial blood pressure and heart rate immediately after IIVC clamping combined with portal triad clamping in all cases are shown in Table 3. There were no significant differences in baseline blood pressure and heart rate between the 2016 and 2017 groups. However, blood pressure after IIVC clamping was significantly different between the two groups; both systolic and mean blood pressures were significantly lower in the 2016 group (P = 0.0068, 0.0344), whereas diastolic blood pressure was comparable. The increased heart rate after IIVC clamping was not significantly different between the two groups.
Usage and duration of vasoactive agents
The main anesthetics, including vasoactive agents, used during hepatic surgery are listed in Table 4. In addition, thiopental was used in one case in 2017 instead of propofol due to soy allergy. In one case in 2016 and two cases in 2017, 1% mepivacaine was administered into the epidural space in addition to the test dose of catheter insertion. There was no difference between the two groups in the type of inhalation anesthetic and the amount of intravenous anesthetic used, but rocuronium, a muscle relaxant, was used significantly less in the 2017 group (P = 0.0091). Regarding vasoactive agents, there was a rule in 2017 that phenylephrine and noradrenaline were the first choices compared to the free choice in 2016. Nonetheless, bolus phenylephrine was used less in 2017 than in 2016 (P = 0.0017). Continuous norepinephrine administration in the 2017 group was not associated with any significant differences in the number of cases, mean injection time, and mean amount per dose. The use of significantly less vasoactive agents in 2017 was also seen for bolus ephedrine (P = 0.0221) and, in particular, continuously administered dopamine (P = 0.0221, 0.0007, 0.0045), although the aforementioned rules may have affected use. The doses of agents used for intraoperative analgesia differed partially between the two groups. The amount of intravenous fentanyl used was significantly higher in the 2017 group than in the 2016 group (P = 0.0199); while remifentanil usage was similar between the two groups. The amount of local anesthetic administered epidurally was significantly lower in 2017 for levobupivacaine than in the 2016 group (P = 0.0442), but comparable for ropivacaine.
Transient deterioration of renal function after hepatic surgery
In both groups, a temporary increase of the serum Cr level and a decrease of eGFR were observed in the acute phase after surgery, as shown in Table 5. There was a significant difference in the degree of renal deterioration between the two groups. The increase in serum Cr was greater in the 2016 than in the 2017 group on POD 1 (P = 0.0220). When an analysis of percentage increase in the serum Cr level relative to baseline was performed, a significant difference was seen in the levels both immediately after surgery and on PODs 1 and 2 (P = 0.0143, 0.0012, 0.0046). The decrease in eGFR was greater in the 2016 than in the 2017 group both immediately after surgery and on POD 1 (P = 0.0318, 0.0067). Furthermore, analysis of the percentage decrease in eGFR relative to baseline demonstrated a significant difference both immediately after surgery and on PODs 1 and 2 (P = 0.0042, 0.0003, 0.0382). These cases of deteriorated renal function were investigated for the incidence of AKI using the KDIGO criteria, and the 2017 group tended to have less severe AKI than the 2016 group.
Discussion
In the present study, a retrospective analysis of the relationship between the change in the degree of IIVC clamping and resultant postoperative renal function was performed. Patients who underwent surgery in 2016 and who received constant 80% IIVC clamping required copious use of vasoactive agents to treat hemodynamic instability and also experienced greater deterioration in renal function than the subsequent 2017 group who received adjustable IIVC clamping.
There are a variety of combined surgical and anesthetic protocols to minimize the amount of bleeding in hepatic surgery. Since intermittent portal triad clamping successfully prevents the inflow of blood into the liver during resection [23], most of the other protocols aim to reduce blood flow in the outflow system, i.e., the hepatic vein. Fluid restriction is practiced by the anesthesiologist to lower hepatic venous pressure while monitoring CVP. IIVC clamping was introduced to surgically lower CVP as an alternative to anesthetic fluid restriction [6]. The effect of IIVC clamping to reduce the amount of bleeding is certain [7], but the safety of this technique remains uncertain. One problem is the risk of pulmonary embolism from thrombosis due to venous stasis that occurs in the lower body after clamping [10]. Perhaps in this study, surgeons moderated the degree of IIVC clamping compared to complete blockade to avoid venous thrombus formation. The other is a potential adverse effect on hemodynamics due to inseparability from the central circulation. To avoid serious complications of THVE [13], IIVC clamping was introduced on the premise that the effect of blocking venous return did not cause any hemodynamic disturbance and preserved renal function [6, 10]. However, in our experience, IIVC clamping also led to compromise of systemic hemodynamics. It has been reported that hemodynamics after 100% IIVC clamping was well maintained and was protective of renal function, which was because of abundant infusion [10]. In the present study, IIVC clamping was performed on the poorer fluid conditions by anesthesia, which may have consequently increased the negative systemic hemodynamic effects with even less than 100% clamping.
Perioperative renal protection primarily requires the prevention of hypoxic damage to the renal medulla [2]. For this, to maintain renal perfusion, it is recommended to first correct hypovolemia [24] and maintain mean blood pressure at the reference value [25]. The dehydration effects of fluid restriction can compromise the suitability of both intravascular volume and blood pressure. The results of the present study showed that IIVC clamping, the same outflow control method as fluid restriction, can also impair renal function. As shown in the example of hemodynamic changes measured with the Vigileo/FloTrac system, the IIVC clamping causes a sudden decrease in preload, and the resulting low cardiac output significantly lowers blood pressure. Although the blood pressure decrease is reflexively compensated by increased peripheral vascular resistance, it is transient and may not be sufficient to maintain hemodynamics for a long time. In the present study, the constant greater degree of IIVC clamping in the 2016 group caused a more significant decrease of blood pressure immediately after IIVC clamping compared to the hemodynamically adjusted IIVC clamping in the 2017 group. Subsequent blood pressure may have been maintained equally in both groups by vasoactive agents, but cardiac output that theoretically affects renal perfusion should have decreased more in the 2016 group [26]. Furthermore, the renoprotective effect is not evident among cardiovascular drugs used in the current clinical setting [24]. In various major surgeries, attention has been focused on the relationship between small changes in creatinine levels in the early postoperative period and patient prognosis [27, 28]. AKI after hepatic surgery is also associated with worse short-term outcomes during hospitalization [29,30,31], but the impact on long-term outcomes, including renal function, does not seem major [30, 32]. When focusing on low CVP-assisted hepatic surgery, most cases of AKI were normalized, and clinical impacts were considered limited [5]. In the present study, AKI occurred at a higher rate than previously reported, at approximately 15% [33], but renal deterioration was similarly reversible.
In the present study, surgeons also attempted to lower CVP using IIVC clamping, while the anesthesiologists limited infusion and lowered CVP. The conflicting relationship between IIVC clamping and fluid loading may be involved in the background. The surgical literature recommends that the rate of infusion during hepatic surgery be very strictly reduced to 1 ml/kg/h [18], but anesthesiologists may often not agree with this. In the 2016 group, a constant greater degree of IIVC clamping was probably applied to counteract the effects of anesthetic fluid loading. Years after the first publication of the IIVC clamping method, the surgeon proposed a reference CVP value over the low 4 mmHg as an indication for IIVC clamping due to concerns about air embolism when the CVP is exposed to negative pressure [18]. Therefore, in the present study, it can be surmised that the IIVC clamping technique is aimed at reducing the CVP at the initiative of the surgeon, controlling the outflow system more strictly than anesthesia control alone, and resulting in much less blood loss. In that case, the conservative nature of the central circulation previously assumed in the IIVC clamping method is easily ignored. While the adjustable IIVC clamping was expected to be less effective at reducing blood loss than the fixed degree of clamping, there was instead a trend toward efficacy in terms of blood loss and transfusion. This may be because the more rapid infusions administered with vasoactive agents in the 2016 group counteracted the bleeding reduction effect of the IIVC clamping through the route from the superior vena cava through the cardiac pump to the hepatic vein. Thus, it may be suggested that both slow infusion rates and acceptable hemodynamics which allow slow fluid administration may be important for the coexistence of efficacy and safety of the IIVC clamping, which is in contrast to the bulk infusion allowed in the THVE method.
Limitations
In the present study, the rate of IVC diameter reduction during IIVC clamping was evaluated visually by a well-trained surgeon. A quantitative scale to precisely adjust the degree of IIVC clamping should be developed in the future. Furthermore, there were limitations inherent in the retrospective nature of the present study. The experience of anesthesiologists with cases during the previous observation period might have affected the anesthesia protocol that was used during the subsequent observation period. In particular, vasoactive agent selection, opioids, and epidural anesthesia doses that were different between the 2016 and 2017 groups may have affected the outcome of postoperative renal function and other collected data. Nevertheless, we believe that the present study provides useful clinical information on the safe management of hepatic surgery using the IIVC clamping technique.
Conclusion
IIVC clamping is an effective method for reducing intraoperative blood loss during hepatic surgery, although it has detrimental effects on systemic circulation. The previously practiced method of application of a constant greater degree of IIVC clamping was associated with a copious need for vasoactive agents to treat the resultant hypotension, and the significant, though transient, deterioration of postoperative renal function. Adjusting the degree of IIVC clamping to maintain hemodynamics might reduce postoperative renal deterioration, while still meeting the goal of reducing intraoperative bleeding.
References
Saner F. Kidney failure following liver resection. Transplant Proc. 2008;40:1221–4.
Sear JW. Kidney dysfunction in the postoperative period. Br J Anaesth. 2005;95:20–32.
Bredt LC, Peres LAB. Risk factors for acute kidney injury after partial hepatectomy. World J Hepatol. 2017;9:815–22.
Lukanovic NP. Hot topics in liver anesthesia. Transplant Proc. 2008;40:1187–9.
Correa-Gallego C, Berman A, Denis SC, Langdon-Embry L, O'Connor D, Arslan-Carlon V, Kingham TP, D'Angelica MI, Allen PJ, Fong Y, DeMatteo RP, Jarnagin WR, Melendez J, Fischer M. Renal function after low central venous pressure-assisted liver resection: assessment of 2116 cases. HPB. 2015;17:258–64.
Otsubo T, Takasaki K, Yamamoto M, Katsuragawa H, Katagiri S, Yoshitoshi K, Hamano M, Ariizumi S, Kotera Y. Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery. 2004;135:67–73.
Fancellu A, Petrucciani N, Melis M, Porcu A, Feo CF, Zorcolo L, Nigri G. Usefulness of infra-hepatic inferior vena cava clamping during liver resection: a meta-analysis of randomized controlled trials. J Gastrointest Surg. 2018;22:941–51.
Katz SC, Shia J, Liau KH, Gonen M, Ruo L, Jarnagin WR, Fong Y, D'Angelica MI, Blumgart LH, Dematteo RP. Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg. 2009;249:617–23.
Aramaki O, Takayama T, Higaki T, Nakayama H, Ohkubo T, Midorikawa Y, Moriguchi M, Matsuyama Y. Decreased blood loss reduces postoperative complications in resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2014;21:585–91.
Rahbari NN, Koch M, Zimmermann JB, Elbers H, Bruckner T, Contin P, Reissfelder C, Schmidt T, Weigand MA, Martin E, Büchler MW, Weitz J. Infrahepatic inferior vena cava clamping for reduction of central venous pressure and blood loss during hepatic resection: a randomized controlled trial. Ann Surg. 2011;253:1102–10.
Hamady Z, Toogood G. Infrahepatic inferior vena cava clamping for reduction of central venous pressure and blood loss during hepatic resection: a randomized controlled trial. Ann Surg. 2015;261:e8.
Belghiti J, Noun R, Zante E, Ballet T, Sauvanet A. Portal triad clamping or hepatic vascular exclusion for major liver resection. A controlled study. Ann Surg. 1996;224:155–61.
Smyrniotis VE, Kostopanagiotou GG, Gamaletsos EL, Vassiliou JG, Voros DC, Fotopoulos AC, Contis JC. Total versus selective hepatic vascular exclusion in major liver resections. Am J Surg. 2002;183:173–8.
Li Z, Sun YM, Wu FX, Yang LQ, Lu ZJ, Yu WF. Controlled low central venous pressure reduces blood loss and transfusion requirements in hepatectomy. World J Gastroenterol. 2014;20:303–9.
Choi SS, Jun IG, Cho SS, Kim SK, Hwang GS, Kim YK. Effect of stroke volume variation-directed fluid management on blood loss during living-donor right hepatectomy: a randomised controlled study. Anaesthesia. 2015;70:1250–8.
Hasegawa K, Takayama T, Orii R, Sano K, Sugawara Y, Imamura H, Kubota K, Makuuchi M. Effect of hypoventilation on bleeding during hepatic resection: a randomized controlled trial. Arch Surg. 2002;137:311–5.
Belghiti J, Noun R, Malafosse R, Jagot P, Sauvanet A, Pierangeli F, Marty J, Farges O. Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg. 1999;229:369–75.
Otsubo T. Control of the inflow and outflow system during liver resection. J Hepatobiliary Pancreat Sci. 2012;19:15–8.
Lentschener C, Franco D, Bouaziz H, Mercier FJ, Fouqueray B, Landault C, Mazoit JX, Benhamou D. Haemodynamic changes associated with portal triad clamping are suppressed by prior hepatic pedicle infiltration with lidocaine in humans. Br J Anaesth. 1999;82:691–7.
Eyraud D, Richard O, Borie DC, Schaup B, Carayon A, Vézinet C, Movschin M, Vaillant JC, Coriat P, Hannoun L. Hemodynamic and hormonal responses to the sudden interruption of caval flow: insights from a prospective study of hepatic vascular exclusion during major liver resections. Anesth Analg. 2002;95:1173–8.
KDIGO Board Members. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
Choukèr A, Schachtner T, Schauer R, Dugas M, Löhe F, Martignoni A, Pollwein B, Niklas M, Rau HG, Jauch KW, Peter K, Thiel M. Effects of pringle manoeuvre and ischaemic preconditioning on haemodynamic stability in patients undergoing elective hepatectomy : a randomized trial. Br J Anaesth. 2004;93:204–11.
Man K, Fan ST, Ng IO, Lo CM, Liu CL, Wong J. Prospective evaluation of pringle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg. 1997;226:704–11.
Goren O, Matot I. Perioperative acute kidney injury. Br J Anaesth. 2015;115:ii3–14.
Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 2015;123:515–23.
Tang IY, Murray PT. Prevention of perioperative acute renal failure: what works? Best Pract Res Clin Anaesthesiol. 2004;18:91–111.
Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, Bihorac A. Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation. 2009;119:2444–533.
O’Connor ME, Kirwan CJ, Pearse RM, Prowle JR. Incidence and associations of acute kidney injury after major abdominal surgery. Intensive Care Med. 2016;42:521–30.
Tomozawa A, Ishikawa S, Shiota N, Cholvisudhi P, Makita K. Perioperative risk factors for acute kidney injury after liver resection surgery: an historical cohort study. Can J Anaesth. 2015;62:753–61.
Lim C, Audureau E, Salloum C, Levesque E, Lahat E, Merle JC, Compagnon P, Dhonneur G, Feray C, Azoulay D. Acute kidney injury following hepatectomy for hepatocellular carcinoma : incidence, risk factors and prognostic value. HPB. 2016;18:540–8.
Garnier J, Faucher M, Marchese U, Meillat H, Mokart D, Ewald J, Delpero JR, Turrini O. Severe acute kidney injury following major liver resection without portal clamping : incidence, risk factors, and impact on short-term outcomes. HPB. 2018;20:865–71.
Ishikawa S, Tanaka M, Maruyama F, Fukagawa A, Shiota N, Matsumura S, Makita K. Effects of acute kidney injury after liver resection on long-term outcomes. Korean J Anesthesiol. 2017;70:527–34.
Bressan AK, James MT, Dixon E, Bathe OF, Sutherland FR, Ball CG. Acute kidney injury following resection of hepatocellular carcinoma: prognostic value of the acute kidney injury network criteria. Can J Surg. 2018;61:11–6.
Acknowledgements
The authors would like to thank FORTE Science Communications for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ohta, J., Kadoi, Y., Murooka, Y. et al. Hemodynamically adjusted infrahepatic inferior venous cava clamping can reduce postoperative deterioration in renal function: a retrospective observational study. J Anesth 34, 320–329 (2020). https://doi.org/10.1007/s00540-020-02742-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02742-6