Abstract
Background and aims
Bleeding from the hepatic vein is closely related to central venous pressure (CVP). To evaluate the effect of low central venous pressure during a hepatectomy, the infrahepatic inferior vena cava (IVC) was half clamped.
Patients and methods
Between 2006 and 2007, 20 patients undergoing major hepatectomy with the IVC half clamping (half-clamping group) were compared with 58 patients undergoing hepatectomy without IVC half clamping between 2003 and 2005 (control group). The types of liver resection, amount of blood loss during the hepatectomy, volume of blood transfusion, length of hospital stay, and complications were compared between the two groups.
Results
In the half-clamping group, blood loss was decreased in comparison to the control group (p = 0.041) and the suprahepatic CVP was low (2.4 ± 1.8 mmHg; p = 0.0002). The diameter at the root of the right hepatic vein was reduced in comparison to before clamping (5.8 ± 1.6 mm; p < 0.001). There were no complications of half clamping on any hemodynamic and blood electrolytic parameters.
Conclusion
Using the half clamping technique of the IVC, intra-operative CVP was maintained below 3 mmHg without any side effects, and the low CVP significantly reduced the bleeding from hepatic veins during a major hepatectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intra-operative blood loss is one of the major causes for post-operative morbidity and mortality. Recently, several techniques, such as total hepatic vascular exclusion [1–4], intermittent vascular inflow occlusion through clamping of the portal triad (Pringle maneuver), and low central venous pressure (CVP) anesthesia [5–9] have been shown to reduce blood loss during a hepatic resection. Intermittent vascular inflow occlusion, or the Pringle maneuver, minimizes hepatic arterial and portal blood flow to the liver during a transection of the hepatic parenchyma [10]. However, a substantial cause of blood loss during liver resection is often hepatic vein injury [8]. To decrease bleeding from the outflow system, surgeons previously had performed total vascular exclusion (TVE) [1–4], which involves clamping the infra- and suprahepatic inferior vena cava (IVC). However, TVE or total clamping of inferior vena cava results in major central hypovolemia, as well as renal and heart disturbances [7].
Therefore, the possibility that half clamping the infrahepatic inferior vena cava (IVC) could reduce the CVP in patients with high CVP (>5 mmHg) was investigated. In this study, the trial was conducted by comparing the IVC half clamping (half-clamping group) and no clamping (control group) using the Pringle maneuver during major hepatectomies.
Materials and methods
From January 2006 until April 2007, 20 patients undergoing a major hepatectomy were assigned to undergo a hepatectomy with intermittent pedicular clamping (Pringle maneuver) and the IVC half clamping during a liver resection (half-clamping group). We performed the half-clamping technique with all the patients undergoing major hepatectomy during the study period. A major hepatectomy was defined as the resection of one or more liver segments except a left lateral hepatectomy by Couinaud’s definition. Right hepatectomy (V + VI + VII + VIII), right trisectionectomy (I + IV + V + VI + VII + VIII), left hepatectomy (II + III + IV), left trisectionectomy (I + II + III + IV + V + VIII), right posterior hepatectomy (VI + VII), and right anterior hepatectomy (V + VIII) have all been defined as a major hepatectomies according to Couinaud’s classification.
These patients with the IVC half clamping were compared with 58 consecutive patients undergoing a major hepatectomy without IVC half clamping between 2003 and 2005 (control group). Operations during the study period were performed by two surgeons (H.Y. and K.U.) and there were no changes about the transection techniques and equipments, other knowledge of liver surgery, and other intra-operative management techniques, between the different study periods. The patients who required either a concomitant bowel resection or contra lateral hepatic resection were excluded in the study. The hepatic veins were divided and revealed after transection of the liver parenchyma. In the present series, there were no cases of biliary reconstruction, portal vein tumor thrombectomy, or combined resection of the diaphragm or IVC.
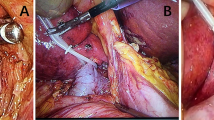
After an ultrasonographic study, the gallbladder was removed and the liver was mobilized. The IVC was isolated and encircled with a cloth tape below the liver in patients of the half-clamping group. In IVC half-clamping method, the IVC was taped by a cloth tape and the girth measured; 2/3 laps parts of the cloth tape were marked and 2/3 laps of the IVC were clamped with a tourniquet during the liver resection. The diameter of the right hepatic vein root was measured using ultrasonography (US) exploration during the pre- and post IVC half clamping. The resection of the liver was performed using an ultrasonic dissector under intermittent clamping by means of occlusion of blood inflow, both pedicular or selective, 20 min and then released for 5 min using a rubber tape with a tourniquet [11]. The amount of blood loss was measured from the volume of blood collected in the container of the aspirator and the ultrasonic dissector and from the weight of the soaked pieces of gauze.
In patients belonging to the half-clamping group, intra-operative hemodynamic monitoring included the venous central right subclavian and the right femoral dual-channel catheters with one channel being connected to the transducer for continuously monitoring CVPs. Arterial pressure was measured by puncture of the radial artery and electrolytic parameters (pH, PaO2, PaCO2, HCO3 −, base excess, lactic acid) and CVPs at the site of the supra- and infra-IVC clamping were monitored throughout the operation.
The data are presented as the mean ± standard deviation. For statistical analyses, Welch’s paired t test and the chi-square test were used to evaluate the differences in surgical parameters between the half clamping and control groups by Stat View program (version 5 Hulinks, Tokyo, Japan). Statistical significance was defined as a p value of <0.05.
Results
Surgical outcomes using the half clamping method
Twenty patients were included in the half-clamping group and 58 in the control group. The groups were equally matched according to age, sex, diagnosis, degree of fibrosis and steatosis of the nontumorous liver (Table 1). The patients with liver disease were distributed homogeneously between the two groups. There were no intra-operative complications related with the surgical techniques and there were no significant differences between the two groups regarding the type of liver resection performed or associated surgical procedures (Table 2). The duration of the whole procedure was approximately 4 h, and there were no differences between groups. No differences were observed in the overall ischemic duration (Pringle’s maneuver) and the total volume of fluid infusion. Patients in the control group experienced more blood loss than the half-clamping group of patients (p = 0.025). Four patients required a transfusion intra-operatively in the half-clamping group (20%), which was significantly different from the control group (p = 0.049). There were no differences in the post-operative mean hospital stay between the groups (Table 3).
Influence of IVC half clamping on intra-operative hemodynamic evolution
There were no intra-operative deaths and serious complications, such as air embolisms resulting from a low CVP. There were no differences in the post-operative morbidity between groups (Table 4). Five patients experienced minor complications in the half-clamping group and 14 patients had minor complications in the control group; however, there were no serious complications in either group and all patients left the hospital in good condition.
In the half-clamping group, IVC half clamping had no influence on the intra-operative blood pressure (Table 5). During the clamping period, CVP at the site of the supra-clamping was significantly low in comparison to that before clamping (5.5 ± 1.8 vs. 2.4 ± 1.8 mmHg; p < 0.0001) and the diameter at the root of the right hepatic vein was significantly reduced in comparison to that before clamping (8.3 ± 1.8 vs. 5.8 ± 1.6 mm; p < 0.0001). In the half-clamping group, the pH, PaCO2, HCO3 −, base excess, and lactic acid levels were measured in addition to the arterial blood electrolytic parameters (Table 6). There were no changes between the periods of pre-clamping, during clamping, and post de-clamping.
Discussion
This is the first report to demonstrate that the IVC half clamping decreases blood loss during a major hepatectomy. It was thought that the volume of blood loss during the hepatectomy correlated with the CVP [7, 8]. From these data, using the IVC half clamping and lowering the CVP to <3 mmHg is a simple and effective way to reduce blood loss during liver surgery.
Recently, several techniques, such as total hepatic vascular exclusion (TVE) [1–4], intermittent vascular inflow occlusion (Pringle maneuver), low central venous pressure anesthesia [5–9, 12], and acute isovolemic hemodilution have been shown to reduce blood loss during hepatic resection [13]. TVE involves clamping the portal pedicle and the infra- and suprahepatic IVC has been considered to be the most effective method to decrease blood loss. However, TVE or total clamping of the inferior vena cava can induce a major central hypovolemia and may be associated with intra- and post-operative renal and heart disturbance [1, 14, 15]. Some surgeons encountered paradoxical bleeding from the cut surface with TVE, and this was thought to be due to obstruction of the drainage routes of the adrenal and subphrenic vein by TVE [16].
Complete IVC clamping of the vena cava below the liver with the inflow occlusion has been reported [16]. However, using the total IVC clamping method is associated with a low blood pressure in some cases and may be difficult in patients with severe cirrhosis [16].
Using the intermittent vascular inflow occlusion, the blood loss during a liver resection tends to mainly occur from the hepatic and short hepatic vein [5, 6]. Some reports have suggested a relationship between blood loss and the CVP, showing that lowering the CVP reduced blood loss during a hepatectomy because the hepatic sinusoidal pressure is directly related to the CVP [8]. While the hepatic inflow of the blood is controlled, with a lowering of the pressure in the inferior vena cava, the hepatic venous pressure and hepatic sinusoidal pressure is decreased. The volume of blood loss during a liver resection has also been reported to correlate with the CVP [7, 8] while low CVP (<5 mmHg) anesthesia with intermittent vascular inflow occlusion has been reported to cause a decrease in bleeding [13]. As a result, this remains a very attractive method; however, it is often associated with complications and may be contraindicated in patients with severe cirrhosis [14].
In the present study, using the IVC half clamping technique with the Pringle maneuver, the intra-operative blood loss was reduced because the supra-clamping CVP was remarkably low and the diameter at the root of the right hepatic vein was significantly reduced in comparison to that before clamping. Moreover, no complications were observed and the clamping had no effect on the hemodynamic and blood electrolytic parameters. Using the IVC half clamping technique with the Pringle maneuver, the intra-operative CVP can be maintained below 3 mmHg without side effects, and it significantly reduces the risk of bleeding from the hepatic veins during a major hepatectomy in which the hepatic veins are exposed. In addition, reducing the transfusion volume is also helpful in the recovery of the patient’s immunological function and the prevention of tumor recurrence.
However, with a low CVP, injuries in the hepatic veins may increase the risk of air embolism. Therefore, patients are quickly placed in a 15-degree Trendelenburg’s position at the time of injuries in these vessels [17]. This treatment reduces the risk of air embolism and also improves venous return to the heart [18]. However, so far, no instances of air embolism have been reported using this technique. About the renal function after half clamping accompanied with increasing of renal venous pressure, there is no bad influence to renal function intra- and post-operatively comparing with control group from the data of serum BUN, creatine, and urine volume.
Recently, we take into account new technical improvements such as in-line radiofrequency ablation system [19] to minimize blood loss in hepatic parenchymal transaction. Using this new device with half clamping of the IVC below the liver, the supra-clamping CVP is lowered (<3 mmHg) and intra-operative blood loss can be decreased without any serious side effects, especially in cases with major hepatectomies in which the hepatic veins are exposed. This is the first report to demonstrate the efficacy of the half clamping technique which limits the blood loss during a hepatectomy without changing the hemodynamic characteristics in such patients.
References
Azoulay D, Eshkenazy R, Andreani P, Castaing D, Adam R, Ichai P, Naili S, Vinet E, Saliba F, Lemoine A, Gillon MC, Bismuth H (2005) In situ hypothermic perfusion of the liver versus standard total vascular exclusion for complex liver resection. Ann Surg 241:277–285
Batignani G, Zuckermann M (2005) Inferior approach for the isolation of the left-middle hepatic veins in liver resections: a safe way. Arch Surg 140:68–971
Smyrniotis V, Arkadopoulos N, Kostopanagiotou G, Farantos C, Vassiliou J, Contis J, Karvouni E (2005) Sharp liver transection versus clamp crushing technique in liver resections: a prospective study. Surgery 137:306–311
Smyrniotis VE, Kostopanagiotou GG, Gamaletsos EL, Vassiliou JG, Voros DC, Fotopoulos AC, Contis JC (2002) Total versus selective hepatic vascular exclusion in major liver resections. Am J Surg 183:173–178
Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y, Blumgart LH (1998) Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187:620–625
Wang WD, Liang LJ, Huang XQ, Yin XY (2006) Low central venous pressure reduces blood loss in hepatectomy. World J Gastroenterol 12:935–939
Jones RM, Moulton CE, Hardy KJ (1998) Central venous pressure and its effect on blood loss during liver resection. Br J Surg 85:1058–1060
Chen H, Merchant NB, Didolkar MS (2000) Hepatic resection using intermittent vascular inflow occlusion and low central venous pressure anesthesia improves morbidity and mortality. J Gastrointest Surg 4:162–167
Rees M, Plant G, Wells J, Bygrave S (1996) One hundred and fifty hepatic resections: evolution of technique towards bloodless surgery. Br J Surg 83:1526–1529
Hasegawa K, Takayama T, Orii R, Sano K, Sugawara Y, Imamura H, Kubota K, Makuuchi M (2002) Effect of hypoventilation on bleeding during hepatic resection: a randomized controlled trial. Arch Surg 137:311–315
Uchiyama K, Ueno M, Hama T, Kawai M, Tani M, Terasawa H, Ozawa S, Uemura R, Nakase T, Yamaue H (2005) Recurrence of primary hepatocellular carcinoma after hepatectomy—differences related to underlying hepatitis virus species. Hepatogastroenterology 52:591–595
Figueras J, Llado L, Ruiz D, Ramos E, Busquets J, Rafecas A, Torras J, Fabregat J (2005) Complete versus selective portal triad clamping for minor liver resections: a prospective randomized trial. Ann Surg 241:582–590
Chen H, Sitzmann JV, Marcucci C, Choti MA (1997) Acute isovolemic hemodilution during major hepatic resection—an initial report: does it safely reduce the blood transfusion requirement. J Gastrointest Surg 1:461–466
MacKenzie S, Dixon E, Bathe O, Sutherland F (2005) Intermittent hepatic vein—total vascular exclusion during liver resection: anatomic and clinical studies. J Gastrointest Surg 9:658–666
Yin ZY, Wang XM, Yu RX, Zhang BM, Yu KK, Li N, Li JS (2003) Total vascular exclusion technique for resection of hepatocellular carcinoma. World J Gastroenterol 9:2194–2197
Otsubo T, Takasaki K, Yamamoto M, Katsuragawa H, Katagiri S, Yoshitoshi K, Hamano M, Ariizumi S, Kotera Y (2004) Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery 135:67–73
Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J (1999) Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg 229:322–330
Chau GY, Lui WY, King KL, Wu CW (2005) Evaluation of effect of hemihepatic vascular occlusion and the Pringle maneuver during hepatic resection for patients with hepatocellular carcinoma and impaired liver function. World J Surg 29:1374–1383
Haghighi KS, Wang F, King J, Daniel S, Morris DL (2005) In-line radiofrequency ablation to minimize blood loss in hepatic parenchymal transection. Am J Surg 190:43–47
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uchiyama, K., Ueno, M., Ozawa, S. et al. Half clamping of the infrahepatic inferior vena cava reduces bleeding during a hepatectomy by decreasing the central venous pressure. Langenbecks Arch Surg 394, 243–247 (2009). https://doi.org/10.1007/s00423-008-0297-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0297-3