Abstract
Background
The success of hepatectomy can be associated with intraoperative blood loss because massive blood loss causes a poor prognosis. This study was designed to evaluate the effect of infrahepatic inferior vena cava (IVC) clamping on the bleeding amount during hepatectomy.
Methods
Eighty-five patients scheduled to undergo hepatic resection were randomly assigned to the IVC clamping or an IVC nonclamping group according to age, indocyanine green retention rate at 15 minutes, operative procedure, and number of tumors by prospective, randomized method. All analyses were compared by Mann-Whitney U test.
Results
Forty-three patients were assigned to the IVC clamping group and 42 to the nonclamping group (IVC clamping group vs. non-clamping): total blood loss (499 vs. 584 ml; p = 0.567), amount of bleeding during hepatectomy (233 vs. 285 ml; p = 0.474), amount of bleeding during hepatectomy/area of dissection (4.9 vs. 6.6 ml/cm2; p = 0.63), CVP difference (−3 cmH2O vs. −1 cmH2O; p < 0.01), and diameter of the right hepatic vein (−2.2 cm vs. 0; p < 0.01).
Conclusions
Although we had speculated that infrahepatic IVC clamping would reduce blood loss during hepatectomy, we failed to demonstrate any beneficial effects in this clinical setting with low CVP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rates of morbidity and mortality after hepatic resection have been shown to correlate with excessive intraoperative blood loss and blood transfusion [1, 2]. Any strategy that can reduce blood loss during liver resection may benefit both the patient and the surgeon. Because in most cases the Pringle maneuver is employed for controlling blood inflow to the liver [3], blood loss during hepatic dissection is mainly attributable to bleeding from the hepatic veins. It has been reported that the volume of blood loss during hepatic resection is correlated with the central venous pressure (CVP) and that lowering the CVP to less than 5 cmH2O is a simple and effective way to reduce blood loss during liver surgery [4, 5]. Maintenance of a low CVP precludes vena caval distention and facilitates mobilization of the liver and dissection of the retrohepatic and major hepatic veins. Therefore, it is clinically important to maintain a low CVP during hepatic resection.
We hypothesized that a low CVP created by clamping the infrahepatic inferior vena cava (IVC) would induce a low pressure in the hepatic veins and sinusoids, subsequently decreasing blood loss during hepatic dissection. We conducted the present prospective, randomized, controlled trial to clarify the effect of this maneuver on the amount of bleeding during hepatic transection.
Patients and methods
Study design
This study was designed to clarify the effect of infrahepatic IVC clamping on the amount of bleeding during hepatic dissection. Eighty-five patients who underwent hepatic resection between June 2002 and May 2006 were randomly assigned to an IVC clamping or an IVC nonclamping group by the minimization method with stratified factors of age (60 years ≥ or <60 years), indocyanine green retention rate at 15 minutes (≥20% or <20%), operative procedure (resection of less than or more than one Couinaud’s segment), and number of tumors (single or multiple). We obtained informed consent from all of the patients.
At our department, the mean (SD) blood loss during hepatic resection was 320 ml (260 ml). We hypothesized that a low CVP created by clamping the IVC could decrease blood loss by 160 ml, a clinically valuable reduction. Eighty-three patients in both groups would be required to detect a significant difference with a 2-tailed type 1 error of 5% and a statistical power of 80% (http://www.swogstat.org/statoolsout.html).
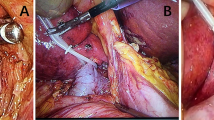
Surgical intervention
The hepatectomy procedure was decided according to criteria based on hepatic functional reserve, as described elsewhere [6]. The infrahepatic IVC cranial to the bilateral renal veins was dissected and taped. All resections were performed with intermittent total (15-minute) occlusion (each with a 5-minute release) of inflow vessels. In the IVC clamping group, the infrahepatic IVC was clamped for 15 minutes simultaneously. Hepatic parenchymal dissection was performed with an ultrasonic dissector (Cavitron Ultrasonic Surgical Aspirator System 200; Valleylab Inc., Boulder, CO; amplitude, 40–70 W). In both groups, tiny vessels were cauterized, vessels >1 mm in diameter were ligated and cut, and bleeding or bile leakage points were fine-sutured. Fibrin glue was then spread on the cut surface.
Anesthesia management
Patients with normal liver or mild fibrosis received fluid infusion at 7 to 8 ml/kg per hour, and patients with liver cirrhosis did so at 5 to 6 ml/kg per hour . Before starting hepatic dissection, an infrahepatic IVC clamping test was performed to determine whether a patient would be able to tolerate the procedure (systolic blood pressure >80 mmHg). When the pressure decreased to <80 mmHg as a result of this procedure, 100 to 500 ml of fluid was infused and then the test was repeated. After confirming that a patient was able to tolerate the procedure, hepatic dissection was started.
Outcome measures
The primary outcome measure was blood loss during hepatic resection. The amount of blood loss was measured in total and during hepatic resection, and blood loss per unit area of transection was calculated. Secondary outcome measures included the differences in CVP and diameter of the right hepatic vein before and during hepatic resection, the duration of the Pringle maneuver, postoperative renal function and length of hospitalization. We measured the CVP (from a zero point at the mid atrial level via a catheter inserted into the superior vena cava) by using DS-5300W DYNASCOPE (Fukuda Denshi Co., Ltd., Tokyo, Japan). The diameter of the right hepatic vein was measured by tracing the transverse length of the right hepatic vein at the confluence to IVC by using intraoperative ultrasonography.
Statistical analysis
The results were expressed as medians and ranges. The Mann-Whitney U test was used to compare variables. Significance was defined as p < 0.05.
Results
Background characteristics
Forty-three patients were assigned to the IVC clamping group and 42 to the IVC nonclamping group (Fig. 1). The background characteristics of the two groups are summarized in Table 1. There were no differences in the stratification factors between the two groups.
Surgical outcomes
All the patients underwent hepatic resection and the 43 patients in the IVC clamping group tolerated the procedure well. The surgical outcomes are summarized in Table 2. The total blood loss in the IVC clamping and IVC nonclamping groups was 499 (range, 60–1,254) ml and 584 (range, 28–2,226) ml, respectively (p = 0.56). The respective amounts of bleeding during hepatectomy were 233 (range, 40–875) ml and 285 (range, 8–1397) ml (p = 0.47). The area of dissection was estimated to be 55 (range, 7.5–119) cm2 in the IVC clamping group and 50 (range, 3–162.2) cm2 in the IVC nonclamping group (p = 0.59). The respective amounts of bleeding during hepatectomy / the area of dissection were calculated to be 4.9 (range, 1.1–14.9) ml/cm2 and 6.6 (range, 0.3–14) ml/cm2 (p = 0.63). The Pringle time was 55 (range, 15–108) min in the IVC clamping group and 49 (range, 7–157) min in the IVC nonclamping group (p = 0.33). The CVP was decreased from 7 (range, 3–14) cmH2O to 4 (range, 0–13) cmH2O in the IVC clamping group, and from 7 (range, 2–16) cmH2O to 6 (range, 1–14) cmH2O in the IVC nonclamping group. The respective decreases were −3 cmH2O (−7 ∼ −1) and −1 cmH2O (−5 ∼ 2) (p < 0.01). The diameter of the right hepatic vein was significantly decreased in the IVC clamping group compared with the IVC nonclamping group (−2.2 cm (−4 ∼ −0.1) vs. 0; p < 0.01). No whole blood was transfused in any of the patients.
The anesthesia time was 7 (range, 5.5–10) hours in the IVC clamping group and 7.2 (range, 4.5–14.5) hours in the IVC nonclamping group (p = 0.36). The total amount of fluid infusion during anesthesia was 2,850 (range, 1,060–5,920) ml in the IVC clamping group and 2,950 (range, 1,680–6,900) ml in the IVC nonclamping group (p = 0.15). The values of (total amount of infusion – amount of bleeding)/kg per hour in the two groups were 5.7 ml/kg per hour and 5.8 ml/kg per hour, respectively. Urine volume/kg per hour was similar in the two groups.
Postoperative renal function was preserved in all patients in the two groups. There were no significant intergroup differences in the values of BUN and creatinine on postoperative days 1, 3, and 5 (Fig. 2).
There was no morbidity related to IVC clamping, including air embolism, and no mortality in the two groups. The length of hospitalization was almost the same in the two groups (26 (range, 17–89) days vs. 30 (range, 13–79) days; p = 0.92).
Discussion
Clinically, a low CVP can be achieved using several strategies. Anesthesia is one of the important factors affecting the CVP. Reduction of intravenous fluid administration has been demonstrated to lower the CVP [7]. Furthermore, morphine can reduce the CVP by inducing venous vasodilation through histamine release and μ3 receptor activation [8]. A combination of extradural blockade and systemic nitroglycerine infusion also effectively lowers the CVP, thus providing a favorable environment for hepatic resection [9]. Although a reduction of tidal volume is suspected to lower the CVP, Hasegawa et al. [10] have reported that this has no beneficial effect on bleeding.
Devascularization maneuvers have been designed to decrease blood loss during hepatic resection. Total hepatic vascular exclusion (THVE) has been used selectively and is associated with significant risks and complications. The technique cannot be employed in all patients because of decreased cardiac output and consequent hypotension [11–13]. Although hepatic vascular exclusion with preservation of caval flow may be an alternative procedure for effective control of blood outflow [14, 15], the technique is still complicated and cannot be used for all patients with liver cirrhosis.
Before performing the present study, we hypothesized that a low CVP achieved by clamping the infrahepatic IVC would be accompanied by low blood pressure in the hepatic veins and sinusoids, subsequently decreasing blood loss during hepatic dissection while preserving hemodynamics. We, therefore, assessed the clinical effect of this maneuver prospectively. Although THVE can lower the CVP significantly in comparison with our technique, most patients can tolerate infrahepatic IVC clamping without serious complications. The infrahepatic IVC can be encircled easily, even in patients with liver cirrhosis, without any bleeding. Stratification factors used in our study included age, ICG15, operative procedure, and the number of tumors, because these were considered to influence the amount of bleeding. Using the minimization method, the patients were assigned to an infrahepatic IVC clamping group or a nonclamping group, and there were no significant differences in background characteristics between the two groups. Although some patients who underwent infrahepatic IVC clamping showed a blood pressure of <80 mmHg, all patients were able to tolerate the procedure after fluid infusion. Unlike the THVE, blood draining from the subphrenic vein, adrenal veins, and lumbar veins may contribute to maintenance of hemodynamics.
In our patients, total blood loss was 499 ml in the IVC clamping group and 584 ml in the IVC nonclamping group, without any significant difference. Because the total blood loss included not only the bleeding as a result of liver transection but also the bleeding attributable to other surgical procedures, such as laparotomy and exudates, the amount of bleeding solely attributable to liver transection was measured. Although the amount of bleeding during liver transection tended to be smaller in the IVC clamping group than in the IVC nonclamping group, the difference between the two groups was not significant. Furthermore, because the amount of bleeding during hepatectomy was influenced by the area that was dissected, the amount of bleeding during hepatectomy / area of dissection (ml/cm2) was calculated. However, there was no significant difference between the values for the two groups. In a retrospective study, Otsubo et al. [16] concluded that IVC clamping is very effective for reducing blood loss during hepatectomy when the CVP is elevated and cannot be reduced pharmacologically or by fluid restriction. They said that the percentage of patients requiring blood transfusion was decreased significantly only in the subgroup with a CVP >10 cmH2O before IVC clamping. They did not use the procedure in patients with a CVP <5 cmH2O. In our patients, the CVP before clamping was 7 cm H2O in both groups. The CVP decreased from 7 to 4 cmH2O in the IVC clamping group and from 7 to 6 cmH2O in the IVC nonclamping group. The former reduction was the result of both the Pringle maneuver and IVC clamping, whereas the latter was only due to the Pringle maneuver. During surgery, the CVP was maintained at a low level, which might have minimized the difference in the amount of bleeding between the two groups. Among the operative outcome parameters, only the differences in CVP and right hepatic vein diameter showed significant changes. The procedure achieved an obvious reduction of the CVP but not to such a degree that the amount of bleeding was significantly decreased.
We also evaluated the fluid volume during surgery but found no significant difference between the two groups. Both groups underwent the same form of intraoperative management. Because the IVC was encircled at a site proximal to the bilateral renal veins, there was a risk of renal function impairment due to venous blood congestion. However, there were no significant intergroup differences in intraoperative urine volume, postoperative BUN, and creatinine values. Infrahepatic IVC clamping is considered to have little influence on renal function. Even when the CVP was <5 cmH2O, air embolism was not observed. Finally, there was no morbidity related to IVC clamping and no mortality in the two groups, and both groups required almost the same length of hospitalization.
Conclusions
Although infrahepatic IVC clamping was confirmed to reduce the CVP significantly, we failed to demonstrate any beneficial effects for reducing blood loss during liver transection in this clinical setting. However, this procedure may be useful for selected patients with high CVP.
References
Yanaga K, Kanematsu T, Takenaka K et al (1988) Hepatic resection for hepatocellular carcinoma in elderly patients. Am J Surg 155:238–241
Nagao T, Goto S, Kawano N et al (1986) Hepatic resection for hepatocellular carcinoma. Ann Surg 205:33–40
Man K, Fan ST, Ng IOL et al (1997) Prospective evaluation of Pringle maneuver in hepatectomy for liver tumors by a randomized study. Ann Surg 226:704–713
Jones RM, Moulton CE, Hardy KJ (1998) Central venous pressure and its effect on blood loss during liver resection. Br J Surg 85:1058–1060
Johnson M, Mannar R, Wu AVO (1998) Correlation between blood loss and inferior vena caval pressure during liver resection. Br J Surg 85:188–190
Makuuchi M, Kosuge T, Takayama T et al (1993) Surgery for small liver cancers. Semin Surg Oncol 9:298–304
Melendez JA, Arslan V, Fischer ME et al (1998) Perioerative outcomes of major hepatic resections under low central venous pressure anesthesia: Blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187:620–625
Grossman M, Aboise A, Tangphao O et al (1996) Morphine-induced venodilation in humans. Clin Pharmacol Ther 60:554–560
Rees M, Plant G, Wells J, Bygrave S (1996) One hundred and fifty hepatic resections: evolution of technique towards bloodless surgery. Br J Surg 83:1526–1529
Hasegawa K, Takayama T, Orii R et al (2002) Effect of hypoventilation on bleeding during hepatic resection. Arch Surg 137:311–315
Bismuth H, Castaing D, Garden J (1989) Major hepatic resection under total vascular exclusion. Ann Surg 210:13–19
Huguet C, Addario-Chieco P, Gavelli A et al (1992) Technique of hepatic vascular exclusion for extensive liver resection. Am J Surg 163:602–605
Belghiti J, Noun R, Zante E, Ballet T, Sauvanet A (1996) Portal triad clamping or hepatic vascular exclusion for major liver resection. A controlled study. Ann Surg 224:155–161
Ellias D, Lasser P, Dabaene B et al (1995) Intermittent vascular exclusion of the liver (without vena cava clamping) during major hepatectomy. Br J Surg 82:1535–1539
Cherqui D, Malassagne B, Colau PI et al (1999) Hepatic vascular exclusion with preservation of the caval flow for liver resection. Ann Surg 230:24–30
Otsubo T, Takahashi K, Yamamoto M et al (2004) Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery 135:67–73
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kato, M., Kubota, K., Kita, J. et al. Effect of Infra-Hepatic Inferior Vena Cava Clamping on Bleeding During Hepatic Dissection: A Prospective, Randomized, Controlled Study. World J Surg 32, 1082–1087 (2008). https://doi.org/10.1007/s00268-007-9445-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9445-0