Abstract
Background
The purpose of this study was to evaluate the long-term voice function after robotic thyroidectomy in comparison with conventional transcervical thyroidectomy.
Methods
We prospectively evaluated the voice functions of 54 patients with thyroid nodules who underwent robotic thyroidectomy by a gasless unilateral axillary or axillo-breast approach and of 70 patients who underwent conventional thyroidectomy. Subjective voice symptom score (VSS) was evaluated in questionnaires before thyroidectomy and then at 3, 6, 12, and 24 months after surgery. Objective acoustic parameters analyzed during the same period included fundamental frequency, jitter, shimmer, noise-to-harmonic ratio, highest frequency, frequency and intensity range, and maximal phonation time.
Results
At 3 months after surgery, VSS was better in the robotic group than in the conventional group. At 2 years after surgery, VSS had recovered to the pre-operative level in the robotic group, whereas it remained significantly worse at 2 years in the conventional group. The phonatory frequency range and highest frequency were significantly wider and higher, respectively, in the robotic group than the conventional group at 6, 12, and 24 months post-operatively. Within the robotic group, the frequency range and highest frequency recovered to pre-operative levels by 6 months, whereas in the conventional group they remained below the pre-operative levels at 2 years post-operatively. There were no differences in other acoustic parameters between the two groups of patients at any period.
Conclusion
Up to 2 years post-operatively, robotic thyroidectomy has advantages in terms of recovery of voice symptoms and acoustic parameters over conventional thyroidectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robotic thyroidectomy has gained popularity worldwide [1–7], offering a scar-less neck and greater cosmetic satisfaction to the patients [8], while it offers a three-dimensional magnified view, hand-tremor filtration, and multi-articulated hand-like motions to surgeons [3]. During the initial period of adopting the robotic system in thyroid surgery, studies were focused on the technical feasibility, safety, and complications of robotic thyroidectomy [3, 9, 10]. Recently, surgical completeness and functional outcomes affecting patients’ quality of life have been investigated [11–13].
Voice alteration is one of the main issues affecting the quality of life of patients after thyroidectomy, and prevention of voice impairment is considered a primary goal of thyroidectomy procedures. It is well known that damage to the laryngeal nerve causes vocal cord paralysis and hoarseness. However, in many cases, voice impairment after thyroidectomy is not related to impairment of the recurrent laryngeal nerve (RLN) or external branch of the superior laryngeal nerve (EBSLN) [14–16].
Voice change following robotic thyroidectomy has not been thoroughly evaluated, although the short-term voice outcomes after transaxillary robotic thyroidectomy have been reported recently by us and others [17–19]. In the present study, we prospectively compared long-term voice functions after robotic thyroidectomy and conventional thyroidectomy. Voice outcomes were evaluated both subjectively and objectively, with evaluation of serial changes. To our knowledge, this is the first report on long-term functional voice outcomes after robotic thyroid surgery.
Patients and methods
Patients
We prospectively enrolled a consecutive cohort of patients undergoing conventional transcervical thyroidectomy or robotic thyroidectomy using a gasless unilateral axillary (GUA) or gasless unilateral axillo-breast (GUAB) approach between March 2011 and August 2012. The inclusion criteria were patients undergoing thyroidectomy with or without central neck dissection for treatment of thyroid nodule(s) and who provided informed consent for voice evaluation. The study was approved by the Institutional Review Board of Hanyang University Hospital.
Indications for robotic thyroidectomy included benign thyroid nodules less than 5 cm in diameter, differentiated thyroid carcinoma less than 3–4 cm with small nodal metastases [20]. The exclusion criteria were identical to those in our previous study evaluating short-term voice function after robotic thyroidectomy: age <18 or >70 years, vocal fold lesions and movement disorders, evidence of injury to the RLN or EBSLN on videolaryngostroboscopic or flexible laryngoscopic examination, history of surgery or irradiation to the neck, maximal extrathyroidal extension, or distant metastasis [18]. We also excluded male patients to eliminate the bias in acoustic parameters, due to the difference of acoustic parameters between male and female patients.
Videolaryngostroboscopic examination with an EndoSTROB DX (Xion, Berlin, Germany) or fiberoptic flexible laryngoscopy was routinely performed the day before surgery and again post-operatively to evaluate paralysis of the RLN or EBSLN. We estimated the motion of the vocal folds, vocal fold mucosal lesions and wave, symmetry of arytenoid excursion, bowing, and degree of glottic closure [18].
Surgical techniques
All robotic thyroid surgeries were performed by a single experienced surgeon (K.T.). The surgical procedures for robotic thyroidectomy using GUA and GUAB approaches have been described in previous reports [2, 3, 21]. Conventional thyroidectomy was performed by the usual method, with a 5–6 cm low-collar skin incision [13]. We routinely identified and preserved the RLN during thyroidectomy. However, we did not identify the EBSLN routinely to minimize the EBSLN injury in the both groups.
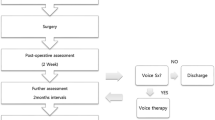
Evaluation of subjective voice symptoms
Voice symptoms were evaluated subjectively and objectively the day before surgery and again at 3, 6, 12, and 24 months after the operation. Subjective voice symptom score (VSS) was evaluated using a questionnaire to estimate discomforts associated with thyroid surgery [18]. The questionnaire comprised five questions on changes in voice pitch, range, intensity, fatigability, and singing quality: (1) Do you have vocal fatigue? (2) Do you have a hoarse voice? (3) Is it difficult to produce a high pitch? (4) Is your voice weak or breathy? (5) Do you have difficulty in singing? All questions were scaled as 0 (no symptom), 1 (mild), 2 (moderate), 3 (severe), or 4 (very severe) [18]. The VSS was estimated as the sum of the scores for the five questions.
Objective acoustic parameters and aerodynamic study
Acoustic analysis and aerodynamic measurements were made using voice range profile (VRP) analysis and the multidimensional voice program (MDVP) with Computerized Speech Lab software (MDVP model 4150B, KayPENTAX, Lincoln Park, NJ, USA). The acoustic analysis was recorded by an experienced speech-language pathologist (B.R.Y).
For VRP analysis, patient was instructed to phonate the sustained vowel/a/as loudly and as softly as possible from the lowest frequency to the highest. The lowest frequency (F-low, Hz), highest frequency (F-high, Hz), frequency range (Hz), and intensity range (dB) were measured. For MDVP analysis, the patient produced a sustained vowel/a/at the most comfortable pitch/amplitude for at least 5 s. The parameters measured were noise-to-harmonic ratio (NHR), jitter (%), shimmer (%), and fundamental frequency (F0, Hz). For the aerodynamic study, maximal phonation time (MPT, seconds) was measured by asking the patient to produce the vowel/a/for as long as possible. This was repeated three times and the longest measurement was selected.
Statistical analysis
Student’s t test, Chi squared test, and Fischer’s exact test were used to compare factors between the robotic and conventional thyroidectomy groups of patients. Paired t tests were used to compare pre-operative and post-operative variables. SPSS version 18.0 software (SPSS Chicago, IL, USA) was used for all statistical analyses. A value of p < 0.05 indicated statistical significance.
Results
Clinicopathological characteristics
During the study period, an overall total of 321 patients with thyroid nodules underwent robotic (97 cases) or conventional (224 cases) thyroidectomy. Of these, 165 patients were excluded from the present study due to exclusion criteria. Two further patients who underwent robotic thyroidectomy and four who underwent conventional thyroidectomy were observed to have transient RLN paralysis after operation and they were excluded from the study. Among the 150 female patients, 124 (82.6 %) successfully completed all of the acoustic analysis. Finally, the robotic group comprised 54 patients, and the conventional group comprised 70 patients. The clinical and pathological data of the both groups are summarized in Table 1. The mean age of the robotic group was lower, and operative time was longer than the conventional group.
Analysis of subjective voice symptoms
A comparison of VSS in the two groups of patients is shown in Table 2. At 3 months after surgery, the VSS was significantly lower (corresponding to less voice impairment) in the robotic group than in the conventional group (p = 0.025); however, no difference between the groups was observed at 6 months, 1 year, and 2 years post-operatively (p = 0.203, 0.536, and 0.785, respectively). Within the robotic group, the VSS at 3 months was significantly higher than the pre-operative VSS, but by 2 years there was no significant difference from the pre-operative level. In contrast, the VSS at 2 years in the conventional group remained significantly above the pre-operative VSS.
Measurement of objective acoustic and aerodynamic parameters
The results of measurement of aerodynamic and acoustic parameters in the two groups of patients are listed in Table 3. The F-high and the frequency range were higher and wider, respectively, in the robotic group than in the conventional group at 6 months, 1 year, and 2 years after surgery. Within the robotic group, the F-high and the frequency range recovered to pre-operative levels by 6 months after surgery. In contrast, in the conventional group, these parameters had not recovered to pre-operative levels at 2 years. No differences were found between the two groups regarding intensity range, F0, jitter, shimmer, NHR, and MPT.
Discussion
Thyroidectomy causes post-thyroidectomy syndrome, including voice impairment and discomfort during swallowing. Injury to the RLN is the main cause of functional voice impairment after thyroidectomy. The prevalence of RLN paralysis after conventional thyroidectomy is 0.77–7.2 % [22–24]. In earlier studies, no difference was reported in the incidence of RLN injury between patients who underwent robotic and conventional thyroidectomy [3, 21, 25]. Nonetheless, impairment of vocal or throat functions occur in 15–84 % of patients who undergo thyroidectomy, even without definite injury of the laryngeal nerves [26]. These impairments may remain for a long period of time after thyroidectomy.
Studies that have evaluated the long-term voice outcomes after thyroidectomy were all confined to conventional thyroidectomy [15, 26, 27]. One prospective observational study evaluating long-term voice functions after conventional thyroidectomy showed that vocal frequency range was narrower, perceptual voice remained rougher, and subjective parameters of vocal symptoms remained worse than during the pre-operative period, even up to 12 months after thyroidectomy [26]. In another study with a mean follow-up period of 4 years, voice change persisted in 28 % of the patients in the absence of definite laryngeal nerve injury [15]. At present, there is no consensus on the definition of a long-term post-operative period in evaluating post-thyroidectomy syndrome. In one study on assessment of post-thyroidectomy voice function, 1–2 weeks after thyroidectomy was considered the early post-operative and 3 months the late post-operative period [28]. However, in the present study, we considered 1 year or more after the surgery as long-term, in accordance with other reports [13, 27].
Previously, we have reported short-term results for voice and swallowing function following robotic thyroidectomy [18]. In our previous study, subjective voice impairment following robotic thyroidectomy was less than with conventional thyroidectomy at 1 day, 1 month, and 3 months post-operatively. In addition, measurements of acoustic parameters gave better results for vocal frequency range and F-high in the robotic group than in the conventional group at 3 months after surgery. These results were reproduced in the present study, even though the patient groups differed and surgery took place later than in the earlier study [18]. In the present study, we analyzed the extended long-term serial voice outcomes up to 2 years post-operatively. Long-term subjective and objective outcomes were significantly better in the robotic group than in the conventional group. At 3 months post-operatively, subjective voice functions were better in the robotic group and voice symptoms had recovered to the pre-operative level by 2 years, whereas voice symptoms had not recovered by 2 years in the conventional group. However, the difference in recovery of VSS to pre-operative levels in the two groups must be interpreted with caution, since the VSS at 2 years was not significantly different between the two groups.
In the robotic group, the F-high was higher and the frequency range was wider at 6 months, 1 year, and 2 years after surgery than in the conventional group. The F-high and the frequency range recovered to pre-operative levels by 6 months in the robotic group, whereas those parameters had not recovered by 2 years post-operatively in the conventional group. We additionally compared the risk factors between patients with VSS or F-high (Hz) that were >10 % increase than pre-operative baseline at 2 years (56 patients) and patients with VSS and F-high ≤10 % increase (68 patients). The analyzed risk factors were robotic versus conventional surgery, total thyroidectomy versus lobectomy, central neck dissection, age ≤30 versus 30 <age ≤50 versus age >50, laryngopharyngeal reflux, smoking, alcohol, and body mass index. In univariate analysis, age (p = 0.039) and conventional thyroidectomy (p = 0.011) were risk factors for worsening VSS/acoustic parameter. In multivariate logistic regression analysis, only conventional thyroidectomy was an independent risk factor (OR = 2.298, 95 % confidence interval 1.029–5.132, p = 0.042).
The proposed factors that affect voice symptoms following thyroidectomy in cases without apparent laryngeal nerve injury are delayed healing, surgical trauma of the strap muscles or cricothyroid muscle, laryngotracheal fixation, subclinical hematoma, laryngeal edema caused by disturbance of venous or lymphatic drainages, local neck pain, vocal fold changes, and injury of the arytenoid caused by orotracheal intubation [14, 18, 28–32]. Acoustic and aerodynamic parameters that are influenced by thyroid surgery are decreases in the MPT, fundamental frequency, F-high, and frequency range, and increases in jitter, shimmer, and the NHR [29, 31]. After thyroidectomy, subjective voice symptoms without laryngeal nerve injury are more common than objective acoustic abnormalities [13, 33]. The discordance between objective parameter abnormalities and subjective vocal symptoms is found in approximately one-third of patients who undergo thyroidectomy [28, 34].
Laryngotracheal fixation and altered strap muscle or cricothyroid muscle movement can be the major causes of voice change after thyroidectomy [35]. Adhesion of the strap muscle to the larynx and trachea is caused by scar formation after thyroidectomy, and results in defective pitch control during phonation [14, 18]. Strap muscle movement effects laryngotracheal movement, and damage to the muscles by retraction and adhesion is associated with a reduction in fundamental frequency and range [36, 37]. The impairment of cricothyroid muscle movement is usually related to paralysis of the EBSLN or surgical trauma of the muscle, and it results in lowered pitch, loss of upper range and projection, vocal fatigue, and breathiness [14]. Typical cricothyroid dysfunction can be observed by a shift of the posterior commissure toward the affected side, weak tension, and shortened vocal fold on videostroboscopic examination [14].
We assume that the better long-term results for voice symptoms and vocal pitch after robotic thyroidectomy compared with conventional thyroidectomy might be mainly due to reduced adhesion of the skin flap, the strap muscles and the laryngotracheal structure, and fewer traumas to the strap muscles [18]. Robotic transaxillary approach avoids the need to make an incision in the skin of the neck, and permits limited dissection of strap muscles and fine dissection of the thyroid gland; therefore, laryngotracheal fixation is reduced. The better results for phonatory pitch after robotic surgery may be the result of reduced injury to the EBSLN in comparison with conventional thyroidectomy. Robotic procedures allow fine dissection in a ×10 magnified view, and provide a better view of the small branches of neurovascular structures compared with direct vision, or viewing with a surgical loupe.
The present study has several limitations. First, the different distribution of age between the two groups might have affected the results. Second, electromyography to confirm EBSLN injury was not used in this study, because of the reluctance of patients to undergo an invasive procedure, although we excluded cases with definite EBSLN injury on videostroboscopy examination [33, 38]. Third, the study lacks randomization of the robotic or conventional thyroidectomy techniques. Randomized clinical trial of robotic thyroidectomy is difficult because robotic thyroidectomy is not covered by the national health insurance system in our country and costs 4–5 times more than conventional thyroidectomy. A further study with randomization and a larger patient pool may minimize these limitations. Fourth, VSS questionnaire is not validated. However, VSS questionnaire has been used in the previous study, and was effective in evaluating specific voice symptoms related with thyroidectomy, and showed high compliance due its conciseness [18].
Conclusion
In the long-term post-operative period of up to 2 years after surgery, robotic thyroidectomy via a GUA/GUAB approach has advantages in recovery of subjective voice symptoms and better acoustic parameters of frequency range and highest frequency than with conventional thyroidectomy.
References
Ban EJ, Yoo JY, Kim WW et al (2014) Surgical complications after robotic thyroidectomy for thyroid carcinoma: a single center experience with 3,000 patients. Surg Endosc 28:2555–2563
Song CM, Cho YH, Ji YB et al (2013) Comparison of a gasless unilateral axillo-breast and axillary approach in robotic thyroidectomy. Surg Endosc 27:3769–3775
Tae K, Ji YB, Jeong JH et al (2011) Robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach: our early experiences. Surg Endosc 25:221–228
Holsinger FC, Terris DJ, Kuppersmith RB (2010) Robotic thyroidectomy: operative technique using a transaxillary endoscopic approach without CO2 insufflation. Otolaryngol Clin North Am 43:381–388
Kuppersmith RB, Holsinger FC (2011) Robotic thyroid surgery: an initial experience with North American patients. Laryngoscope 121:521–526
Kandil E, Abdelghani S, Noureldine SI et al (2012) Transaxillary gasless robotic thyroidectomy: a single surgeon’s experience in North America. Arch Otolaryngol Head Neck Surg 138:113–117
Lee KE, Kim E, Koo do H et al (2013) Robotic thyroidectomy by bilateral axillo-breast approach: review of 1,026 cases and surgical completeness. Surg Endosc 27:2955–2962
Song CM, Ji YB, Bang HS et al (2014) Quality of life after robotic thyroidectomy by a gasless unilateral axillary approach. Ann Surg Oncol 21:4188–4194
Kang SW, Jeong JJ, Yun JS et al (2009) Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc 23:2399–2406
Lee KE, Koo do H, Kim SJ et al (2010) Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery 148:1207–1213
Lee S, Lee CR, Lee SC et al (2014) Surgical completeness of robotic thyroidectomy: a prospective comparison with conventional open thyroidectomy in papillary thyroid carcinoma patients. Surg Endosc 28:1068–1075
Tae K, Song CM, Ji YB et al (2014) Comparison of surgical completeness between robotic total thyroidectomy versus open thyroidectomy. Laryngoscope 124:1042–1047
Song CM, Ji YB, Bang HS et al (2014) Long-term sensory disturbance and discomfort after robotic thyroidectomy. World J Surg 38:1743–1748. doi:10.1007/s00268-014-2456-8
Hong KH, Kim YK (1997) Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg 117:399–404
Pereira JA, Girvent M, Sancho JJ et al (2003) Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery 133:318–322
Silva IC, Netto Ide P, Vartanian JG et al (2012) Prevalence of upper aerodigestive symptoms in patients who underwent thyroidectomy with and without the use of intraoperative laryngeal nerve monitoring. Thyroid 22:814–819
Lee J, Nah KY, Kim RM et al (2010) Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc 24:3186–3194
Tae K, Kim KY, Yun BR et al (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26:1871–1877
Lee J, Na KY, Kim RM et al (2012) Postoperative functional voice changes after conventional open or robotic thyroidectomy: a prospective trial. Ann Surg Oncol 19:2963–2970
Tae K, Ji YB, Jeong JH et al (2013) Comparative study of robotic versus endoscopic thyroidectomy by a gasless unilateral axillo-breast or axillary approach. Head Neck 35:477–484
Tae K, Ji YB, Cho SH et al (2012) Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years’ experience. Head Neck 34:617–625
Bhattacharyya N, Fried MP (2002) Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg 128:389–392
Debruyne F, Ostyn F, Delaere P et al (1997) Acoustic analysis of the speaking voice after thyroidectomy. J Voice 11:479–482
Steurer M, Passler C, Denk DM et al (2002) Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope 112:124–133
Lee S, Ryu HR, Park JH et al (2011) Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg 253:1060–1066
Ryu J, Ryu YM, Jung YS et al (2013) Extent of thyroidectomy affects vocal and throat functions: a prospective observational study of lobectomy versus total thyroidectomy. Surgery 154:611–620
Lombardi CP, Raffaelli M, De Crea C et al (2009) Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery 146:1174–1181
Stojadinovic A, Shaha AR, Orlikoff RF et al (2002) Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 236:823–832
Lombardi CP, Raffaelli M, D’Alatri L et al (2008) Video-assisted thyroidectomy significantly reduces the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg 32:693–700. doi:10.1007/s00268-007-9443-2
Lombardi CP, Raffaelli M, D’Alatri L et al (2006) Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery 140:1026–1032
Maeda T, Saito M, Otsuki N et al (2013) Voice quality after surgical treatment for thyroid cancer. Thyroid 23:847–853
Kark AE, Kissin MW, Auerbach R et al (1984) Voice changes after thyroidectomy: role of the external laryngeal nerve. Br Med J 289:1412–1415
de Pedro Netto I, Fae A, Vartanian JG et al (2006) Voice and vocal self-assessment after thyroidectomy. Head Neck 28:1106–1114
McIvor NP, Flint DJ, Gillibrand J et al (2000) Thyroid surgery and voice-related outcomes. Aust N Z J Surg 70:179–183
Dursun G, Sataloff RT, Spiegel JR et al (1996) Superior laryngeal nerve paresis and paralysis. J Voice 10:206–211
Hong KH, Ye M, Kim YM et al (1997) The role of strap muscles in phonation–in vivo canine laryngeal model. J Voice 11:23–32
Hirano M, Koike Y, von Leden H (1967) The sternohyoid muscle during phonation. Electromyographic studies. Acta Otolaryngol 64:500–507
Soylu L, Ozbas S, Uslu HY et al (2007) The evaluation of the causes of subjective voice disturbances after thyroid surgery. Am J Surg 194:317–322
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Chang Myeon Song, Bo Ram Yun, Yong Bae Ji, Eui Suk Sung, Kyung Rae Kim, and Kyung Tae have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Song, C.M., Yun, B.R., Ji, Y.B. et al. Long-Term Voice Outcomes After Robotic Thyroidectomy. World J Surg 40, 110–116 (2016). https://doi.org/10.1007/s00268-015-3264-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3264-5