Abstract
Background
The purpose of this study was to evaluate postoperative voice outcomes and functional parameters in total thyroidectomy via a transaxillary (TA) approach.
Methods
Seventy-six patients who underwent total thyroidectomy via a TA approach (TA group) were included. A total of 204 patients who underwent conventional open total thyroidectomy (conventional group) in the same time period were analyzed as a control group. All patients underwent prospective functional evaluations before surgery and at 1 week and 1, 3, 6, and 12 months postoperatively using a comprehensive battery of functional assessments.
Results
There was no conversion to conventional open thyroidectomy in the TA group. Operation time and the amount of drainage were significantly higher in the TA group than in the conventional group (p < 0.001 and p = 0.033, respectively), while vocal cord paralysis, hypoparathyroidism, and hematoma were not different among two groups (p = 0.215, 0.290, and 0.385, respectively). Regarding GRBAS, the TA group showed a more aggravated tendency postoperatively, although statistical significance was attained only at postoperative 6 months (p = 0.043). The voice handicap index abruptly increased postoperatively in the TA group, showing significant differences with the conventional group at postoperative 1 week and 1 month (p < 0.001 and p = 0.001, respectively). Fundamental frequency and maximal vocal pitch did not significantly change postoperatively in either group. The conventional group showed a more rapid decline in pain than the TA group, and paresthesias on the neck and chest were more aggravated in the TA group during the early postoperative period. The dysphagia handicap index was higher in the TA group, while cosmesis was better in the TA group at all postoperative periods.
Conclusions
Although cosmetic outcome was better with the TA approach, the longer operation time, aggravated subjective voice outcomes, paresthesia, and swallowing function need to be considered in selecting the operative approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Conventional open thyroidectomy using the Kocher incision has been used as the standard approach until the emergence of endoscopic and robotic technologies. Recently, many surgeons have attempted extracervical approaches via axillae or breast for improved esthetic results [1]. Among extracervical approaches, the gasless transaxillary (TA) endoscopic thyroidectomy and the gasless TA robotic thyroidectomy were introduced in 2006 and 2009, respectively [2, 3]. These techniques are known to be safe and efficacious in the hands of experienced surgeons, and cosmetic and surgical outcomes are known to be comparable with conventional open thyroidectomy [4, 5].
Besides the well-known complication of thyroidectomy, TA thyroidectomy poses additional risks, which are not typically associated with thyroid surgery but rather related to the new approach and surrounding anatomy. These include stretch injury to the brachial plexus, perforation of the esophagus, and injury to the carotid artery and/or internal jugular vein [6, 7]. Moreover, rare complications due to injury of neck muscles and traction injury have also been reported recently [8]. Transaxillary thyroidectomy has an additional disadvantage in that it is significantly more expensive than the standard cervical approach, especially for robotic thyroidectomy [9].
In addition to these disadvantages, the lack of data on long-term outcomes regarding voice and functional parameters of patients with total thyroidectomy mandate the need for prospective studies, although some reports have demonstrated the excellence of TA thyroidectomy (including both hemithyroidectomy and total thyroidectomy) in cosmetic and functional outcomes even with neck dissection [10]. Clinically, we sometimes encounter patients with stiff neck, especially around the sternocleidomastoid muscle, and voice or swallowing dysfunction long after surgery with a TA approach. In this prospective study, we aimed to evaluate the long-term voice and functional outcomes of TA total thyroidectomy in comparison with conventional open thyroidectomy.
Materials and methods
Study population
The study protocol was approved by the Institutional Review Board (IRB) of the Korea University College of Medicine. From May 2011 to December 2013, patients undergoing total thyroidectomy with either of the two approaches were included in this prospective study. Inclusion criteria for enrollment were as follows: (1) underwent total thyroidectomy; (2) no clinical evidence of neck node involvement (central or lateral); and (3) age ≥ 20 years. Enrollment exclusion criteria were as follows: (1) a diagnosis of anaplastic or medullary carcinoma; (2) preoperative evidence of nodal disease or lymph node dissection of any lateral compartment during the initial operative intervention; and (3) patients who did not complete 1 year of follow-up.
Evaluations of the surgical approach
All patients were informed about the operative techniques for both conventional open and TA approach thyroidectomy, and patients subsequently chose their preferred surgical procedure. Informed consent was obtained from each patient for the endoscopic thyroidectomy and for the possibility of a conversion to an open thyroidectomy. All surgery was performed by a single high-volume surgeon (KY Jung), and the surgical procedure was described previously elsewhere [11]. Patients were categorized as the TA group (those with TA approach thyroidectomy) and the conventional group (those with conventional open thyroidectomy).
Preoperative evaluations were completed for all patients using ultrasonography, fine-needle aspiration cytology, computed tomography, and thyroid hormone tests. Intraoperative and pathologic findings, including invasion to surrounding tissue, tumor and thyroid size, tumor side and location, multiplicity, extrathyroidal extension, and number of inadvertently excised parathyroid glands, were evaluated. Operative time, amount of total drainage, and complications, including vocal cord paralysis, hypoparathyroidism, and postoperative hematoma, were evaluated and compared between surgical groups.
Analysis of voice quality
All patients underwent repeated functional evaluations before surgery and postoperatively at 1 week and 1, 3, 6, and 12 months using a comprehensive battery of functional assessments. Acoustic voice analysis was performed under identical conditions by a single voice specialist. The voice specialist performed a perceptual rating of subjective voice assessments using the GRBAS scale. The GRBAS scale consists of the following five parameters: overall grade of hoarseness (G), roughness (R), breathiness (B), asthenia (A), and strain (S). A 4-point grading scale was used for each parameter, where 0 = normal, 1 = slight, 2 = moderate, and 3 = severe. Acoustic voice analysis was performed using the multi-dimensional voice program (MDVP) and the voice range profile program (VRP) of the CSL for maximal vocal pitch (MVP) (Kay Elemetrics, Lincoln Park, NJ, USA).
Assessment of subjective functional status and satisfaction
The subjective voice outcome was analyzed using the voice handicap index (VHI) [12], which included functional, physical, and emotional subscales that measure defects in verbal communication. Each item on the VHI is scored using a 5-point scale (range 0–4), with a highest possible score of 120 points. The dysphagia handicap index (DHI) [13] is a 25-item statement that describes the handicapping effect of dysphagia, including functional, physical, and emotional subscales, and measures defects in swallowing function. Each item on the DHI is scored according to a 3-point scale, with the highest possible score being 75 points. On both the VHI and DHI, a higher score is indicative of a greater perception of functional disability.
To assess patients’ subjective pain and cosmetic satisfaction, a visual analogue scale (VAS) was used for pain (0 = no pain, 5 = moderate pain, and 10 = most severe pain) and patient satisfaction (0 = dissatisfied, 1 = acceptable, 2 = satisfied, and 3 = extremely satisfied). Paresthesias in the neck and chest areas were evaluated using a questionnaire. For each item on the questionnaire, patients were asked to rate their response on a 4-point scale, where 0 = not at all, 1 = mild, 2 = moderate, and 3 = severe, using a reference period.
Statistical analysis
Results for continuous variables are presented as mean ± standard deviation (SD), and results for categorical variables are presented as frequencies and group percentages. Continuous outcomes were analyzed using independent (2-sample) t tests; one-way analysis of variance (ANOVA) was used for comparison of three or more groups. Dichotomous outcomes were analyzed using the Chi-square test for trend. All statistical analyses were performed using SPSS Statistics for Windows, version 20.0 (IBM. Armonk, NY, USA). P values <0.05 were considered statistically significant.
Results
General characteristics and complications
A total of 280 patients were enrolled in this study. The mean age was 49.5 ± 11.9, and the male-to-female ratio was 1:4.71. Seventy-six patients were included in the TA group and 204 in conventional group (Table 1). Age at diagnosis was significantly lower in the TA group than in the conventional group (p < 0.001). Male-to-female ratio, body mass index, diagnosis, tumor size, and thyroid size were not significantly different between groups (p = 0.495, 0.297, 0.144, 0.281, and 0.430, respectively), nor were gross operative findings (p = 0.084). However, bilateral tumor was more prevalent in the TA group (p = 0.004), and tumor in the mid-portion of thyroid was more prevalent in conventional group (p = 0.012). Multiplicity and extrathyroidal extension showed no significant differences between the two groups.
No surgeries were converted to a conventional open thyroidectomy in the TA group. Operation time was significantly longer in the TA group than in the conventional group (p < 0.001). The amount of drainage was also higher in the TA group (p = 0.033). Vocal cord paralysis, hypoparathyroidism, and hematoma were not different between the two groups (p = 0.215, 0.290, and, 0.385, respectively) (Table 2). In addition, there were no cases of great vessel, esophagus, trachea, brachial plexus, or marginal mandibular nerve injury.
Analysis of voice quality
Two patients in the TA group and three in the conventional open thyroidectomy were excluded from analysis due to postoperative vocal cord paralysis. GRBAS and VHI scores showed peak aggravation at 1 week in both groups, which gradually decreased to a level similar to the preoperative scale by 6 months (Fig. 1A). Preoperative GRBAS scores were not different between two groups. The TA group showed a more aggravated tendency postoperatively, although statistical significance from the conventional group was attained only at postoperative 6 months (p = 0.043). VHI abruptly increased postoperatively in the TA group, showing a significant difference from the conventional group at 1 week postoperatively and at 1 month (p < 0.001 and p = 0.001, respectively) (Fig. 1B). Fundamental frequency (F0) did not change significantly postoperatively in either group, although a slightly faster recovery was observed in the TA group (Fig. 1C). MVP also showed no difference between the two groups, showing recovery to the preoperative level at 6 months postoperatively (Fig. 1D).
Subjective functional satisfaction
Two patients in the TA group and three in the conventional group were excluded from analysis due to postoperative vocal cord paralysis. With regard to pain, both groups showed a gradual decrease in mean pain scores on VAS. The conventional group showed a faster decrease compared with the TA group, and statistical significance was observed at 1 year postoperatively (p = 0.030) (Fig. 2A). Paresthesias on the neck and chest were more aggravated in the TA group during the early postoperative period (Fig. 2B, C). Statistical significance was observed at 1 week for neck paresthesia (p = 0.001) and at 1 week and 1 month for chest paresthesia (p < 0.001 and p < 0.001, respectively). Paresthesia was roughly equal at postoperative 3 months. DHI was higher in the TA group. However, cosmesis was better in the TA group at all postoperative periods compared with the conventional group, with significant differences observed only at postoperative 3 and 6 months (p = 0.023 and p = 0.015, respectively) (Fig. 3).
Discussion
This study demonstrated that the complication rate with TA thyroidectomy is comparable to that of conventional open thyroidectomy, while postoperative functional outcomes of TA thyroidectomy showed a relatively slower recovery than conventional thyroidectomy. The difference between TA and conventional open thyroidectomy was apparent in VHI scores, pain, paresthesia, and swallowing, with the TA group showing more aggravated scores in the in the early postoperative period. Cosmesis was better in the TA group at postoperative months 3 and 6, while postoperative changes of fundamental frequency and maximal vocal pitch were about the same in both groups.
Since the first description of robotic or endoscopic thyroidectomy in 2007, several papers have been published describing the feasibility and safety of this new surgical approach. The associated functional results, cosmetic advantages, and technical limitations of this newer approach have been studied on large series of patients, and a learning curve for this technique has been proposed [14, 15]. Among the possible advantages of this approach, cosmetic results have been excellent, and the most common reason for selecting extracervical thyroidectomy is the need to hide the scar far away from the anterior neck [1]. This prospective study without randomization showed that younger female patients tended to elect TA thyroidectomy rather than conventional open thyroidectomy. As is shown in our results, cosmetic outcome was excellent, showing that the patient’s satisfaction was significantly higher at postoperative 3 and 6 months with this approach.
One important consideration regarding cosmetic results in previous studies is that none of the studies on cosmesis followed patients beyond 3 months. Typically with scar formation, at the 3-month time point, the scar width is generally wider than the original incision, and erythema is still present past the boundaries of the incision [16]. Since scar maturation tends to occur over a period of 1 year, longer follow-up could reveal the long-term advantage of the TA approach. Our study with a follow-up of 1 year showed that the differences at a late postoperative period of 1 year were not statistically significant between the two groups, although the satisfaction score was somewhat higher in the TA group. A scar in the axilla can be more acceptable to patients, where it can be hidden with usual clothing or when the shoulder is in a neutral position. This may be a great advantage, especially during the postoperative period within 6 months, but may not be advantageous after 1 year.
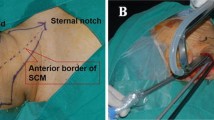
The total operation time, including flap elevation, is one disadvantage of this technique, although this can be reduced with greater surgical experience [17, 18]. In our study, an additional 90 min was needed in the TA group compared with the conventional group. This longer operation time may be associated with not only possible increased morbidity from general anesthesia, but also postoperative complications. Because the TA approach includes flap elevation in the upper chest and traction of sternal head of SCM and strap muscles, these could all affect postoperative functional parameters [19].
As in previous studies, our study showed no differences in changes in GRBAS scores, fundamental frequency, or maximal vocal pitch [20]. Tae et al. [21] used a 5-item questionnaire to investigate symptoms of vocal fatigue, hoarseness, pitch limitation, breathiness or weakness, and difficulty singing, with patients rating the severity of each symptom on a 5-point scale (0 = none to 4 = very severe). Preoperatively, the open cohort and the robotic cohort were similar in their reporting of vocal impairment. Postoperatively, the open cohort had a higher severity of voice symptoms at postoperative 1 day (p = 0.008), 1 month (p = 0.049), and 3 months (p = 0.043), but not at 6 months. In contrast, VHI in our study was significantly aggravated in the early postoperative period, especially within 1 month, which demonstrated that patients are subjectively more unsatisfied regarding voice after TA thyroidectomy in the early postoperative period. This change was minimized at postoperative month 6 and at 1 year. This discrepancy with previous studies may have resulted from differences in the study cohorts. However, based on the results of our study, we think that voice discomfort during the early postoperative period should be a consideration, especially for younger patients who want to undergo the TA approach, although the enrollment of younger patients with a more active social life in the TA group could have affected the results.
Previous data regarding pain, paresthesia, and swallowing relied on a short follow-up period and different numbers of cohorts in each follow-up period [22–24]. Follow-up periods of previous studies have primarily been 3 months, which seems to be too short for sufficient analysis of long-term postoperative outcomes. Pain severity in our study was in accordance with the previous studies in that no significant difference was observed between the TA and conventional groups. Pain in the TA group did show a relatively slower recovery, although the difference between the groups did not reach statistical significance. In addition, paresthesias in the neck and chest were more aggravated in the TA group. We do not think that this difference resulted from the surgeon’s experience, because the primary surgeon in our study had over 3 years of experience with robotic surgery before initiating this prospective study. Rather, we believe that dissatisfaction in paresthesia is innate weakness of TA thyroidectomy, where the flap elevation of the chest and neck and traction injury during the longer operation may have an effect. Although paresthesias decreased and were about the same after postoperative 3 months, we think that discomfort in the neck and chest may be more severe in the early postoperative period with TA thyroidectomy than with conventional thyroidectomy. Results regarding subjective swallowing function were similar. DHI scores were higher in the TA group than in the conventional group, and we believe that wider flap elevation and injury to the neck muscle can affect this result.
Our results should be viewed in the context of potential limitations. The cohorts being compared in this study were significantly different in many aspects. Patients in the TA group were younger and there were more females than in the conventional group. This bias has been seen in most studies. We think that further study with randomization or an age- and sex-matched prospective study is needed to elucidate the role of TA thyroidectomy on postoperative functional outcomes. Before such research is available, our 1-year prospective study can provide good evidence that TA thyroidectomy is not always beneficial in regard to functional outcomes.
Thyroid cancer is associated with a relatively long survival rate and a long recurrence-free survival. For this reason, oncologic outcomes are not established in TA thyroidectomy because of the short duration of the introduction of the surgical skill. Most previous studies have demonstrated that the complication rate and functional outcomes of TA thyroidectomy are comparable to or better than those with conventional open thyroidectomy. However, as previously mentioned, most of the studies have potential biases from a retrospective design, along with varying age and male-to-female ratios and a short follow-up period. Our study found negative findings in that functional outcomes could be aggravated in the early postoperative period in TA total thyroidectomy. These negative results should be a consideration when counseling patients regarding the procedure and in the decision-making on the surgical approach of total thyroidectomy. We suggest that TA total thyroidectomy should not be thoughtlessly recommended without reviewing all possible aspects of postoperative changes until a higher level of evidence is available to elucidate the role of TA thyroidectomy.
References
Bae DS, Koo DH, Choi JY, Kim E, Lee KE, Youn YK (2014) Current status of robotic thyroid surgery in South Korea: a web-based survey. World J Surg 38(10):2632–2639
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2011) Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg 253(6):1060–1066
Kang SW, Jeong JJ, Nam KH, Chang HS, Chung WY, Park CS (2009) Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg 209(2):1–7
Lee J, Nah KY, Kim RM, Ahn YH, Soh EY, Chung WY (2010) Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc 24(12):3186–3194
Lewis CM, Chung WY, Holsinger FC (2010) Feasibility and surgical approach of transaxillary robotic thyroidectomy without CO(2) insufflation. Head Neck 32(1):121–126
Perrier ND, Randolph GW, Inabnet WB, Marple BF, VanHeerden J, Kuppersmith RB (2010) Robotic thyroidectomy: a framework for new technology assessment and safe implementation. Thyroid 20(12):1327–1332
Davis SF, Abdel Khalek M, Giles J, Fox C, Lirette L, Kandil E (2011) Detection and prevention of impending brachial plexus injury secondary to arm positioning using ulnar nerve somatosensory evoked potentials during transaxillary approach for thyroid lobectomy. Am J Electroneurodiagnostic Technol 51(4):274–279
Cha W, Kong IG, Kim H, Hah JH, Sung MW (2014) Desmoid tumor arising from omohyoid muscle: the first report for unusual complication after transaxillary robotic thyroidectomy. Head Neck 36(5):48–51
Cabot JC, Lee CR, Brunaud L, Kleiman DA, Chung WY, Fahey TJ 3rd, Zarnegar R (2012) Robotic and endoscopic transaxillary thyroidectomies may be cost prohibitive when compared to standard cervical thyroidectomy: a cost analysis. Surgery 152(6):1016–1024
Lee J, Kwon IS, Bae EH, Chung WY (2013) Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endoscrinol Metab 98(7):2701–2708
Chung WY (2012) Pros of robotic transaxillary thyroid surgery: its impact on cancer control and surgical quality. Thyroid 22(10):986–987
Rosen CA, Lee AS, Osborne J, Zullo T, Murry T (2004) Development and validation of the voice handicap index-10. Laryngoscope 114(9):1549–1556
Silbergleit AK, Schultz L, Jacobson BH, Beardsley T, Johnson AF (2012) The Dysphagia handicap index: development and validation. Dysphagia 27(1):46–52
Kang SW, Park JH, Jeong JS, Lee CR, Park S, Lee SH, Jeong JJ, Nam KH, Chung WY, Park CS (2011) Prospects of robotic thyroidectomy using a gasless, transaxillary approach for the management of thyroid carcinoma. Surg Laparosc Endosc Percutan Tech 21(4):223–229
Kandil EH, Noureldine SI, Yao L, Slakey DP (2012) Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 214(4):558–564
Bond JS, Duncan JA, Sattar A, Boanas A, Mason T, O’Kane S, Ferguson MW (2008) Maturation of the human scar: an observational study. Plast Reconstr Surg 121(5):1650–1658
Lee J, Yun JH, Nam KH, Soh EY, Chung WY (2011) The learning curve for robotic thyroidectomy: a multicenter study. Ann Surg Oncol 18(1):226–232
Park JH, Lee J, Hakim NA, Kim HY, Kang SW, Jeong JJ, Nam KH, Bae KS, Kang SJ, Chung WY (2014) Robotic thyroidectomy learning curve for beginning surgeons with little or no experience of endoscopic surgery. Head Neck. doi:10.1002/hed.23824
Sun GH, Peress L, Pynnonen MA (2014) Systematic review and meta-analysis of robotic vs conventional thyroidectomy approaches for thyroid disease. Otolaryngol Head Neck Surg 150(4):520–532
Lee J, Na KY, Kim RM, Oh Y, Lee JH, Lee J, Lee JS, Kim CH, Soh EY, Chung WY (2012) Postoperative functional voice changes after conventional open or robotic thyroidectomy: a prospective trial. Ann Surg Oncol 19(9):2963–2970
Tae K, Kim KY, Yun BR, Ji YB, Park CW, Kim DS, Kim TW (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26(7):1871–1877
Tae K, Ji YB, Cho SH, Lee SH, Kim DS, Kim TW (2012) Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years’ experience. Head Neck 34(5):617–625
Lee J, Yun JH, Choi UJ, Kang SW, Jeong JJ, Chung WY (2012) Robotic versus endoscopic thyroidectomy for thyroid cancers: a multi-institutional analysis of early postoperative outcomes and surgical learning curves. J Oncol 2012:734541
Foley CS, Agcaoglu O, Siperstein AE, Berber E (2012) Robotic transaxillary endocrine surgery: a comparison with conventional open technique. Surg Endosc 26(8):2259–2266
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Doh Young Lee, Saehee Lim, Sung Hoon Kang, Kyoung Ho Oh, Jae-Gu Cho, Seung-Kuk Baek, Jeong-Soo Woo, Soon-Young Kwon, and Kwang-Yoon Jung have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lee, D.Y., Lim, S., Kang, S.H. et al. A prospective 1-year comparative study of transaxillary total thyroidectomy regarding functional outcomes: Is it really promising?. Surg Endosc 30, 1599–1606 (2016). https://doi.org/10.1007/s00464-015-4386-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4386-4