Abstract
Background
Good postoperative and excellent cosmetic results have been achieved with bilateral axillo-breast approach (BABA) robotic thyroidectomy (RoT). This study was performed to analyze the surgical outcomes and evaluate the surgical completeness and safety of BABA RoT.
Methods
Between February 2008 and February 2012, a total of 1026 cases of BABA RoT were performed. The clinicopathologic characteristics, operation types, and postoperative outcomes of patients were analyzed.
Results
Of the 1026 cases analyzed, 968 cases were a malignant tumor and 58 cases were benign thyroid disease. Mean operating times for BABA total RoT with central lymph node dissection included 38 ± 13 min (range 20–90 min) of working space creation and 75 ± 26 min (range 25–175) of console time. Among the 872 patients who underwent total thyroidectomy with central lymph node dissection, transient hypoparathyroidism occurred in 39.1 %, transient vocal cord palsy occurred in 14.2 %, and permanent hypoparathyroidism and permanent vocal cord palsy occurred in 1.5 % and 0.2 % of patients, respectively. The median stimulated thyroglobulin (Tg) level of patients after their first radioactive iodine therapy was 0.4 ng/mL, with 65.1 % of patients having a stimulated Tg level of <1.0 ng/mL. The median suppressed Tg level at 3 postoperative months of patients without radioactive iodine therapy was <0.1 ng/mL, with 99.4 % of patients showing a suppressed Tg level of< 1.0 ng/mL. There was no recurrence or mortality after a median follow-up of 23 months.
Conclusions
BABA RoT is a safe and effective method that provides good surgical completeness and has low rates of postoperative complications and recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Well-differentiated thyroid cancer has been the most prevalent cancer in Korea since 2009, and its incidence is increasing worldwide [1–3]. Most cases are papillary thyroid cancers, which most frequently occur in young woman. Because the prognosis and survival rate of thyroid cancer are excellent, cosmesis plays an important role in the surgical strategy of some thyroid cancer patients. Asian patients are at higher risk for hypertrophic scars [4, 5], and an incision at the anterior neck is considered cosmetically undesirable.
To address these concerns, in 2004, we developed the bilateral axillo-breast approach (BABA) for endoscopic thyroidectomy, which we combined with the da Vinci robotic system. The da Vinci system has several merits: EndoWrist, with a high degree of freedom of motion, allows the operator to perform more sophisticated and complex maneuvers, and high-definition three-dimensional (3D) imaging provides a good operative view with excellent depth perception [6]. We have reported the surgical clearance and safety of BABA robotic thyroidectomy (RoT) compared with open thyroidectomy [7, 8]. Over the past 5 years, we have performed more than 1000 cases of BABA RoT, and we have analyzed the surgical outcomes to assess the safety and effectiveness of this method.
Here we report the clinicopathologic characteristics, operation types and times, tumor, node, metastasis classification system (TNM) stage (based on the 7th edition of the American Joint Committee on Cancer/International Union against Cancer [AJCC/UICC]), results after radioactive ablation therapy, and disease recurrence rates of 1026 cases of thyroid disease treated by BABA RoT.
Patients and methods
Patients
Between February 2008 and February 2012, a total of 1026 individuals with thyroid disease underwent RoT by BABA at Seoul National University Hospital and affiliated hospitals. These operations were performed by five surgeons at three academic centers. Informed consent was obtained from all patients, and the protocols were approved by the institutional review boards of Seoul National University Hospital.
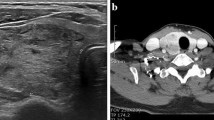
Indications for BABA RoT [9] included low-risk, well-differentiated thyroid carcinoma (<2 cm, no definite evidence of local invasion, cervical nodal metastasis by the preoperative pathologic and radiologic finding), Graves disease, or a benign thyroid nodule up to 8 cm in size. Preoperative diagnoses for thyroid nodules were made by ultrasound and ultrasound-guided fine-needle aspiration biopsy. All patients underwent computed tomography to evaluate tumor location and cervical lymph node metastasis. Patients with previous neck surgery, distant metastasis or multiple lateral neck node metastases, definite tumor invasion to an adjacent organ, or lesions located in the posterior part of the thyroid adjacent to the tracheoesophageal groove or Berry ligament were excluded. All patients also had a breast examination with mammography or ultrasound to detect breast lumps. Large body habitus, high body mass index, and thyroiditis were not considered factors in selection of patients for BABA RoT.
Patients with malignancy underwent total thyroidectomy. Thyroid lobectomy was considered in patients with small (<1 cm), low-risk, unifocal, intrathyroidal papillary carcinoma in the absence of radiologically or clinically involved cervical nodal metastases, and in patients who preferred to undergo thyroid lobectomy [10]. Most proven cases of malignant thyroid carcinoma underwent prophylactic ipsilateral central compartment lymph node dissection (LND). After lateral neck node metastases were excluded in preoperative fine needle aspiration, selective lateral LND was performed in occasional cases in which metastases were suspected in one or two lymph nodes on preoperative imaging.
Operative methods
The RoT procedure has been previously described [8, 9, 11]. Briefly, RoT involves four stages: creation of a working space, robot docking, console time (when the surgeon operates via the da Vinci system console), and closure.
The patient was given general anesthesia and placed in the supine position, extending the neck. After draping, the trajectory lines and working space were drawn on the chest and neck. Creation of a working space was started by hydrodissection. Epinephrine (1:200,000) in a 0.9 % NaCl solution was injected subcutaneously in the working space under the platysma in the neck.
Incisions were made bilaterally at the superomedial edge of the breast areolas and at the axillary folds. Bilateral axillary and circumareolar 8–12 mm ports were inserted after the working space was developed, by using a vascular tunneler through the port incision. The flap extended from the thyroid cartilage superiorly to 2 cm below the clavicle inferiorly and laterally from just beyond the medial border of the sternocleidomastoid muscle. The working space was made by low pressure (5–6 mm Hg) insufflations of CO2 gas.
The robot was docked, and a camera was inserted through the right breast. Monopolar electrocautery or ultrasonic shears were inserted through the left breast. Graspers (Prograsp and Maryland forceps, Intuitive Surgical Inc., Sunnyvale, CA) were inserted through the right and left axillary ports.
The midline of the strap muscle was identified and separated. After visualizing the cricothyroid membrane, isthmus, and trachea, the isthmus was divided with the ultrasonic shears, which facilitated dissection of the gland laterally and posteriorly, and allowed for optimal visualization of the superior thyroid pedicle. Thyroidectomy was performed while identifying and preserving the parathyroid glands and recurrent laryngeal nerve. The dissected thyroid lobe was extracted with an endoplastic bag. Lesion-side central compartment dissection was performed, with care taken to ensure that the recurrent laryngeal nerve was not damaged in patients with a concomitant malignancy or suspicious nodule. The contralateral lobe was dissected in the same manner.
After complete removal of the thyroid, the operative field was irrigated with saline, and meticulous hemostasis was achieved. The midline was closed by robotic endosuturing. In cases of selective lateral LND, a short segment of one double polydioxanone loop (PDS*II, Ethicon Inc., Cincinnati, OH) was used for traction of the sternocleidomastoid muscle.
Follow-up
All patients were followed-up at 2 weeks, 3 months, and 6 months postoperatively and then annually. In all patients, recurrent laryngeal nerve function was assessed from the vocal cord movement by using video laryngoscopy preoperatively, and at 2 postoperative weeks. Hypomotility, median fixation, or paramedian fixation of the vocal cords was recorded as vocal cord palsy. Laryngoscopy was repeated at each visit until vocal cord movement returned. In the case of transient vocal cord palsy, vocal cord movement returned within 6 postoperative months. In cases with a vocal cord abnormality that persisted at 6 postoperative months, permanent vocal cord palsy was diagnosed.
During hospitalization, all patients underwent tests for serum total calcium, ionized calcium, phosphorus, and parathyroid hormone (PTH) to evaluate hypoparathyroidism. A serum total calcium level of <8 mg/dL with a hypocalcemic symptom during hospitalization was defined as transient hypoparathyroidism. Permanent hypoparathyroidism was defined as a serum PTH level of <5 pg/mL with an ongoing requirement for oral calcium supplementation beyond 6 months.
Indications for radioactive iodine (RAI) ablation were as follows: all patients with stage III or IV disease; all patients aged <45 years with stage II disease; most patients aged ≥ 45 with stage II disease; and selected patients with stage I disease, especially those with multifocal disease, nodal metastases, extrathyroid or vascular invasion, or aggressive histologies [9].
Patients for whom RAI ablation was indicated underwent therapy at 8–12 weeks after thyroidectomy. Before the administration of 131I, blood was drawn to measure TSH-stimulated serum thyroglobulin level (stimulated Tg). An 131I whole-body scan was performed on the second day after RAI ablation. In all patients with differentiated carcinoma who did not undergo RAI ablation, the TSH-suppressed serum thyroglobulin level (suppressed Tg) was checked at 3 postoperative months. All patients were examined by ultrasound at 1 postoperative year and annually thereafter.
Results
This study included 1026 consecutive cases (108 males and 918 females) with a mean age of 39.7 ± 9.8 years (range 13–70 years). According to postoperative pathology, the diagnoses of the cases were as follows: papillary thyroid carcinoma (n = 955), follicular thyroid carcinoma (n = 11), medullary thyroid carcinoma (n = 2), adenomatous goiter (n = 34), and follicular or Hürthle cell adenoma (n = 9). Nine cases were Graves disease without tumor in the final pathology report. One case was prophylactic thyroidectomy in a patient with MEN2A, with no neoplastic changes within the thyroid gland.
Of the eight cases that underwent completion thyroidectomy, five had no malignancy in the completion thyroidectomy specimen, and three had papillary thyroid carcinoma. Two cases were patients with newly diagnosed papillary thyroid carcinoma who had a history of previous endoscopic thyroidectomy. The mean malignant tumor size was 0.8 ± 0.49 cm (range 0.1–5.0 cm), and the mean benign tumor size was 1.9 ± 1.48 cm (range 0.2–6.0 cm). The operation types are summarized in Table 1.
The operating time of BABA total RoT with central LND included a mean of 38 ± 13 min (range 20–90 min) of working space creation and 75 ± 26 min (range 25–175 min) of console time. The mean postoperative hospital stay was 3.3 ± 0.7 days (range 2–10 days) (Table 1). The mean number of lymph nodes retrieved by central LND was 4.9 ± 3.74 nodes (range 1–24 nodes), and the number retrieved by selective lateral LND of levels II–IV was 13.2 ± 5.07 nodes (range 7–20 nodes).
Intraoperative bleeding occurred in two cases. The right internal jugular vein was torn during selective lateral LND and was repaired with a small incision on the neck area. Postoperative bleeding occurred in two cases. One case occurred on postoperative day 3 and stopped spontaneously and the other underwent decompression on postoperative day 6. One case of pneumothorax was found at postoperative day 2. Among the 872 patients who underwent BABA total RoT with central LND, transient hypoparathyroidism occurred in 341 patients (39.1 %) and transient vocal cord palsy occurred in 124 patients (14.2 %). Permanent hypoparathyroidism occurred in 13 patients (1.5 %), and permanent vocal cord palsy occurred in two patients (0.2 %).
A total of 889 patients with papillary thyroid carcinoma underwent BABA total RoT. The mean age of these patients was 40.2 ± 9.5 years (range 13–66 years), and the male-to-female ratio was 1: 8.8 (91 male and 798 female subjects). The mean tumor size on histological analysis was 0.75 ± 0.39 cm (range 0.1–2.7 cm). In total, 81.4 % of patients had papillary thyroid microcarcinoma. Multifocality and bilaterality were observed in 286 (32.1 %) and 169 (19.0 %) cases, respectively. Extrathyroid extension occurred in 446 cases (50.2 %), and was microscopic in 417 cases (46.9 %) and gross in 29 cases (3.3 %). In terms of TNM stage according to the 7th edition of AJCC/UICC, 693 patients (77.9 %) had stage I disease, 191 patients (21.5 %) had stage III disease, and five patients (0.6 %) had stage IVa disease (Table 2).
In total, 500 patients (56.2 %) received RAI ablation. The median stimulated Tg level of patients at the first RAI ablation was 0.4 ng/mL (range <0.1–79.84 ng/mL), and 65.1 % of patients (295 of 453) had stimulated Tg levels <1.0 ng/mL. Forty-two patients were referred outside of the hospital after 2 postoperative weeks or delayed RAI ablation until after pregnancy and childbirth. In five cases, the Tg levels at the first RAI ablation were not measured.
For the RAI ablation-negative group, the median suppressed Tg level at 3 postoperative months was <0.1 ng/mL (range <0.1–7.0 ng/mL), and 99.4 % of patients (335 of 337) had a suppressed Tg level of <1.0 ng/mL. Fifty-two patients were referred outside of the hospital. One patient whose Tg level was 1.6 ng/mL at the first follow-up was recommended RAI ablation. This patient had no problem on ultrasound and he refused RAI ablation. His Tg level became <0.1 ng/mL at his second visit. Another patient with a Tg level of 7.0 ng/mL was checked by positron emission tomography and ultrasound, which revealed no evidence of disease.
After a median follow-up of 23 months, there was no locoregional recurrence in patients who underwent RoT. There was one case of lung metastasis, detected by the first 131I whole-body scan with stimulated Tg <1.0 ng/mL, and this patient underwent high-dose RAI ablation.
Discussion
Since Gagner [12] performed the first endoscopic neck surgery in 1996, various endoscopic thyroidectomy techniques have been proposed. Shimazu et al. [13] developed the axillo-bilateral breast approach to overcome the disadvantages of using one direction with lateral approaches and the disadvantages of instrument interference with the axillary approach. The axillo-bilateral breast approach provides excellent cosmetic results without neck scarring, but is limited by the difficulty in visualizing both lobes of the thyroid. Accordingly, in 2004, we developed BABA for optimal visualization during total thyroidectomy [14]. In our experience, BABA endoscopic thyroidectomy provides a good symmetrical surgical view of both thyroid lobes, a similar operative approach to conventional open thyroidectomy, and an excellent cosmetic outcome [14]. However, endoscopic operation has several limitations [15–18]. In particular, the use of a 2D visual representation and nonflexible endoscopic instruments may make surgical field visualization and instrument manipulation difficult. Also, endoscopy personnel must be experienced, and the learning curve is rather steep. To overcome some of the limitations of manual endoscopic operation, we combined the BABA technique with a robotic system.
Serum Tg levels may be used to detect recurrent or residual disease in most patients who undergo total thyroidectomy [10, 19–21]. Although the levels may be measured while TSH is suppressed, the test is more sensitive when TSH is stimulated [19, 20, 22, 23]. Stimulated Tg is directly correlated to the amount of residual thyroid tissue [20, 21, 24–26], and it may be used to predict persistent or recurrent disease by measurement of the thyroid bed 131I uptake after first RAI ablation [26–28]. A recent study of patients undergoing open thyroidectomy showed that 25.3 % of 438 patients with differentiated thyroid carcinoma showed a stimulated Tg <2.0 ng/mL after first RAI ablation [29]. In another report, 48.3 % of 729 patients with low-risk thyroid carcinoma showed a stimulated Tg level ≤1 ng/mL [24].
A group in Italy reported surgical completeness with minimally invasive video-assisted thyroidectomy (MIVAT) for papillary carcinoma [21]. MIVAT was carried out through a 15 mm incision between the sternal notch and the cricoid cartilage with needlescopic instruments and a 30 infinity 5 mm endoscope [21, 30]. The mean stimulated Tg after operation obtained with MIVAT (5.3 ± 5.8 ng/mL) was similar to that obtained with open thyroidectomy (7.6 ± 21.7 ng/mL). A separate report showed a mean stimulated Tg after video-assisted total thyroidectomy of 5.5 ± 6.2 ng/mL (range <0.1–25.3), with 21 % of 152 patients showing a stimulated Tg <0.1 ng/mL [30]. RoT using a transaxillary approach used a 5 to 6 cm vertical incision along the lateral border of the pectoralis major muscle in the axilla, created working space over the anterior surface of the pectoralis major muscle and between the sternal and the clavicular heads of the sternocleidomastoid muscle, and exposed thyroid under strap muscle with an external retractor [15]. Rather than reporting stimulated Tg levels, many studies of RoT using a transaxillary approach provide suppressed Tg levels at 4 postoperative months with or without RAI [15, 31–33]. Another group reported stimulated Tg levels at first RAI ablation after RoT by unilateral axillo-breast or axillary approach (mean: 12.70 ± 15.01 ng/mL, median: 8.8 ng/mL, range 0.1–62.6 ng/mL) or open thyroidectomy (mean: 4.90 ± 8.57 ng/mL, median: 1.9 ng/mL, range <0.1–65.8) [34].
In the case of BABA RoT, we previously reported the surgical outcomes of our initial experience of 109 patients [8]. The median stimulated Tg level of 57 patients who underwent RAI ablation was 0.2 ng/mL (range <0.1–36.4), and 74 % had a stimulated Tg level of <1.0 ng/mL [8]. We examined the mean stimulated Tg after first RAI ablation among patients who underwent BABA RoT compared to those who underwent open thyroidectomy, using the propensity score to show surgical completeness. The mean stimulated Tg levels and percentage with stimulated Tg level of <1.0 ng/mL were 1.4 ± 3.9 ng/mL (range <0.1–36.4) and 69.1 %, respectively, for the RoT group, compared to 1.2 ± 3.1 ng/mL (range <0.1–38.7) and 68.6 %, respectively, for the open thyroidectomy group. The surgical completeness of BABA RoT was not inferior to that of open thyroidectomy [7]. In the present study, the median stimulated Tg level of patients after first RAI ablation was 0.4 ng/mL (range <0.1–79.84), and 65.1 % (295 of 453) had a stimulated Tg level of <1.0 ng/mL. These results are similar to those of our previous study, and the stimulated Tg level achieved was lower than that obtained when using a different approach (Table 3).
Lee et al. [8] addressed some limitations of robotic thyroid surgery, which were a greater operative time and a smaller number of retrieved lymph node in robotic group than in open group. The operative time of robot surgery includes working space creation time, docking time, console time and closure time. The console time was 123 ± 29 min and retrieved lymph node was 2.5 ± 3.2 in previous RoT group. The console time was 75 ± 26 min in the present group and improved than previous group as surgeon’s experience expanded. The number of retrieved lymph node was also improved as surgeon’s experience expanded. The mean postoperative hospital stay of 3.3 days for RoT group was similar with that of 3.2 days for open thyroid surgery, which was reported previously [8, 14, 35].
The incidence rates of postoperative hypoparathyroidism and vocal cord palsy vary depending on the assessment modality and extent of surgery [36–38]. In the present group, 39.1 % of patients experienced transient hypoparathyroidism and 14.2 % of patients experienced transient vocal cord palsy, compared with rates of 17.7 % and 2.5 %, respectively, for open thyroidectomy in our institution [35]. For open thyroidectomy, the rates of transient hypoparathyroidism were reported range from 14.0 % to 39.6 % [36–42]. In the present study, transient hypoparathyroidism rate is within acceptable rate compared with previous reports but higher than those of open thyroidectomy in our institution [35]. Transient vocal cord palsy rates are high. It is thought that any of vocal cord movement abnormality such as hypomotility without hoarseness is also considered as transient vocal cord palsy in our institution. After conventional open thyroidectomy, reported rates of permanent hypoparathyroidism range from 0 to 4.9 % and rates of permanent vocal cord palsy range from 0 to 3.6 % [36–42]. In the present study, the rates of permanent hypoparathyroidism (1.5 %) and permanent vocal cord palsy (0.2 %) were similar or better than those previously reported for conventional open thyroidectomy [35]. One of the two patients with permanent vocal cord palsy recovered from vocal cord hypomotility by 18 months after operation. We had experience of bleeding control after BABA endoscopic surgery [18], which took endoscopic approach using the same incision sites. We had not experienced immediate postoperative bleeding among the cases of BABA RoT. However, we assume that endoscopic decompression and bleeding control in BABA RoT could be done in the same way as in BABA endoscopic operation.
We previously reported that BABA was associated with a higher degree of patient cosmetic satisfaction and BABA induced some sensory impairment in the anterior chest area including on the breasts and nipples but it improved significantly 3 months after surgery [14, 43]. And the operative scars are almost invisible [8, 14]. This cosmetic outcome is the main drive for oncoplastic thyroid surgery. The results of our study show that RoT using BABA can result in an oncologically safe operation using oncoplastic principles [44, 45]. Additional research is needed to compare the recurrence rate between open thyroidectomy and BABA RoT because of relatively short follow-up periods.
The present data includes 174 patients of our initial BABA robotic total thyroidectomy which we previously reported [7, 8]. All of these 174 operations were performed by one expert operator with the same team. To assess the oncologically safety and completeness of BABA RoT, we investigated 1026 cases of BABA RoT performed by several surgeons with or without technical expertise of BABA in our institution and affiliated hospitals. Although the study involved five surgeons with varying RoT experience at three centers, the results were similar to those obtained in our previous study. In BABA, the docking of the robot was designed to optimize visualization of the midline of the strap muscle by using the right breast port for the camera. This symmetrical view allowed both thyroid lobes to be dissected with a similar view and with a medial approach rather than open surgery. With this advantage, the surgeon can perform total thyroidectomy both completely and safety.
Conclusions
BABA RoT is an oncologically safe and effective method that provides good surgical completeness as well as low rates of postoperative complications and recurrence for lower-risk patients with differentiated thyroid cancer.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) GLOBOCAN 2008 v2.0. Cancer incidence and mortality worldwide. IARC Cancer Base No. 10. International Agency for Research on Cancer, Lyon, France. Available at: http://globocan.iarc.fr. Accessed July 1, 2012
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295(18):2164–2167
Lee JS (2012) Cancer facts and figures. National Cancer Control Institute http://ncc.re.kr. Accessed July 1, 2012
Kelly AP (2009) Update on the management of keloids. Semin Cutan Med Surg 28(2):71–76
Soltani AM, Francis CS, Motamed A, Karatsonyi AL, Hammoudeh JA, Sanchez-Lara PA, Reinisch JF, Urata MM (2012) Hypertrophic scarring in cleft lip repair: a comparison of incidence among ethnic groups. Clin Epidemiol 4:187–191
Dionigi G (2009) Robotic thyroid surgery: need for initial stricter patient selection criteria. Surg Laparosc Endosc Percutan Tech 19(6):518
Lee KE, Koo DH, Im HJ, Park SK, Choi JY, Paeng JC, Chung JK, Oh SK, Youn YK (2011) Surgical completeness of bilateral axillo-breast approach robotic thyroidectomy: comparison with conventional open thyroidectomy after propensity score matching. Surgery 150(6):1266–1274
Lee KE, Koo DH, Kim SJ, Lee J, Park KS, Oh SK, Youn YK (2010) Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery 148(6):1207–1213
Lee KE, Choi JY, Youn YK (2011) Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech 21(4):230–236
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, Mciver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
Lee KE, Rao J, Youn YK (2009) Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech 19(3):e71–e75
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83(6):875
Shimazu K, Shiba E, Tamaki Y, Takiguchi S, Taniguchi E, Ohashi S, Noguchi S (2003) Endoscopic thyroid surgery through the axillo-bilateral-breast approach. Surg Laparosc Endosc Percutan Tech 13(3):196–201
Choe JH, Kim SW, Chung KW, Park KS, Han WS, Noh DY, Oh SK, Youn YK (2007) Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 31(3):601–606
Kang SW, Jeong JJ, Nam KH, Chang HS, Chung WY, Park CS (2009) Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg 209(2):e1–e7
Tan CTK, Cheah WK, Delbridge L (2008) “Scarless” (in the neck) endoscopic thyroidectomy (SET): an evidence-based review of published techniques. World J Surg 32(7):1349–1357
Slotema ET, Sebag F, Henry JF (2008) What is the evidence for endoscopic thyroidectomy in the management of benign thyroid disease? World J Surg 32(7):1325–1332
Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo DH, Kim SJ, Lee J, Chung YS, Oh SK, Youn YK (2012) Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc 26(4):948–955
Tuttle RM, Ball DW, Byrd D, Dilawari RA, Doherty GM, Duh QY, Ehya H, Farrar WB, Haddad RI, Kandeel F, Kloos RT, Kopp P, Lamonica DM, Loree TR, Lydiatt WM, Mccaffrey JC, Olson JA, Parks L, Ridge JA, Shah JP, Sherman SI, Sturgeon C, Waguespack SG, Wang TN, Wirth LJ (2010) Thyroid carcinoma. J Natl Compr Canc Netw 8(11):1228–1274
Torrens JI, Burch HB (2001) Serum thyroglobulin measurement. Utility in clinical practice. Endocrinol Metab Clin North Am 30(2):429–467
Miccoli P, Elisei R, Materazzi G, Capezzone M, Galleri D, Pacini F, Berti P, Pinchera A (2002) Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery 132(6):1070–1073
Pacini F, Lari R, Mazzeo S, Grasso L, Taddei D, Pinchera A (1985) Diagnostic-value of a single serum thyroglobulin determination on and off thyroid suppressive therapy in the follow-up of patients with differentiated thyroid-cancer. Clin Endocrinol (Oxf) 23(4):405–411
Mazzaferri EL, Kloos RT (2002) Is diagnostic iodine-131 scanning with recombinant human TSH useful in the follow-up of differentiated thyroid cancer after thyroid ablation? J Clin Endocrinol Metab 87(4):1490–1498
Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, Bardet S, Leenhardt L, Bastie D, Schvartz C, Vera P, Morel O, Benisvy D, Bournaud C, Bonichon F, Dejax C, Toubert ME, Leboulleux S, Ricard M, Benhamou E, Refractaires TT (2012) Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 366(18):1663–1673
Wartofsky L (2002) Editorial: using baseline and recombinant human TSH-stimulated Tg measurements to manage thyroid cancer without diagnostic (131)I scanning. J Clin Endocrinol Metab 87(4):1486–1489
Cailleux AF, Baudin E, Travagli JP, Ricard M, Schlumberger M (2000) Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? J Clin Endocrinol Metab 85(1):175–178
Grunwald F, Menzel C, Fimmers R, Zamora PO, Biersack HJ (1996) Prognostic value of thyroglobulin after thyroidectomy before ablative radioiodine therapy in thyroid cancer. J Nucl Med 37(12):1962–1964
Kim TY, Kim WB, Kim ES, Ryu JS, Yeo JS, Kim SC, Hong SJ, Shong YK (2005) Serum thyroglobulin levels at the time of 131I remnant ablation just after thyroidectomy are useful for early prediction of clinical recurrence in low-risk patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab 90(3):1440–1445
Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L, Nicol A, Clark PM, Farnell K, Mccready R, Smellie J, Franklyn JA, John R, Nutting CM, Newbold K, Lemon C, Gerrard G, Abdel-Hamid A, Hardman J, Macias E, Roques T, Whitaker S, Vijayan R, Alvarez P, Beare S, Forsyth S, Kadalayil L, Hackshaw A (2012) Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med 366(18):1674–1685
Lombardi CP, Raffaelli M, De Crea C, Princi P, Castaldi P, Spaventa A, Salvatori M, Bellantone R (2007) Report on 8 years of experience with video-assisted thyroidectomy for papillary thyroid carcinoma. Surgery 142(6):944–951
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2011) Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg 253(6):1060–1066
Kang SW, Lee SC, Lee SH, Lee KY, Jeong JJ, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 146(6):1048–1055
Kang SW, Lee SH, Ryu HR, Lee KY, Jeong JJ, Nam KH, Chung WY, Park CS (2010) Initial experience with robot-assisted modified radical neck dissection for the management of thyroid carcinoma with lateral neck node metastasis. Surgery 148(6):1214–1221
Tae K, Ji YB, Cho SH, Lee SH, Kim DS, Kim TW (2012) Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years’ experience. Head Neck 34(5):617–625
Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK (2007) Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 31(12):2302–2308
Lee YS, Kim SW, Kim SW, Kim SK, Kang HS, Lee ES, Chung KW (2007) Extent of routine central lymph node dissection with small papillary thyroid carcinoma. World J Surg 31(10):1954–1959
Roh JL, Park JY, Il Park C (2007) Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 245(4):604–610
Palestini N, Borasi A, Cestino L, Freddi M, Odasso C, Robecchi A (2008) Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbecks Arch Surg 393(5):693–698
Henry JF, Gramatica L, Denizot A, Kvachenyuk A, Puccini M, Defechereux T (1998) Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg 383(2):167–169
Sywak M, Comford L, Roach P, Stalberg P, Sidhu S, Delbridge L (2006) Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 140(6):1000–1005
Steinmuller T, Klupp J, Wenking S, Neuhaus P (1999) Complications associated with different surgical approaches to differentiated thyroid carcinoma. Langenbecks Arch Surg 384(1):50–53
Lee YS, Nam KH, Chung WY, Chang HS, Park CS (2010) Postoperative complications of thyroid cancer in a single center experience. J Korean Med Sci 25(4):541–545
Kim SJ, Lee KE, Myong JP, Kwon MR, Youn YK (2011) Recovery of sensation in the anterior chest area after bilateral axillo-breast approach endoscopic/robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech 21(5):366–371
Masetti R, Di Leone A, Franceschini G, Magno S, Terribile D, Fabbri MC, Chiesa F (2006) Oncoplastic techniques in the conservative surgical treatment of breast cancer: an overview. Breast J 12(5):S174–S180
Baildam AD (2002) Oncoplastic surgery of the breast. Br J Surg 89(5):532–533
Disclosures
Kyu Eun Lee, Eunyoung Kim, June Young Choi, Do Hoon Koo, Kyu Hyung Kim, and Yeo-Kyu Youn have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding authors
Additional information
The Kyu Eun Lee and Eunyoung Kim authors contributed equally to this work, and both should be considered first author.
Rights and permissions
About this article
Cite this article
Lee, K.E., Kim, E., Koo, D.H. et al. Robotic thyroidectomy by bilateral axillo-breast approach: review of 1026 cases and surgical completeness. Surg Endosc 27, 2955–2962 (2013). https://doi.org/10.1007/s00464-013-2863-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2863-1