Abstract
Background
Using the da Vinci® robotic system, surgeons can complete secure thyroidectomy without noticeable neck scarring. This study compared the surgical completeness of transaxillary robotic thyroidectomy (RT) with conventional open procedures (OT) in treating papillary thyroid carcinoma (PTC) patients.
Materials and methods
From April 2009 through February 2011, 94 PTC patients underwent total thyroidectomy with central compartment neck dissection (CCND) at Yonsei University College of Medicine. All patients received 1.1 GBq radioactive iodine (RAI) ablation, post-therapy whole-body scans (TxWBS), and diagnostic WBS (DxWBS) 1 year later. We prospectively compared patient clinicopathologic characteristics and surgical completeness between the two groups.
Results
Fifty-one patients underwent OT and 43 underwent RT. Mean age was significantly younger in the RT group. Tumor size, capsular-invasion frequency, multifocality, bilaterality, and central nodal metastasis were not different between the two groups. The number of retrieved nodes during CCND did not significantly differ between the groups. There was no significant difference between the OT and RT groups in stimulated thyroglobulin levels acquired during TxWBS and DxWBS. The RAI uptake ratios at TxWBS were significantly higher in the RT group compared with the OT group; however, follow-up DxWBS showed no difference in RAI uptake ratios. Also, the ablation success rate was similar between the two groups. There were no abnormal findings in follow-up neck ultrasonography in either group.
Conclusion
Remnant thyroid tissue ablation after transaxillary RT was successfully managed by 1.1 GBq RAI. RT showed similar surgical completeness versus conventional OT, and provides a safe and feasible surgical option for PTC patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Since Theodor Kocher established aseptic thyroidectomy, conventional open removal of the thyroid gland has been the universal treatment for papillary thyroid carcinoma (PTC). Open thyroidectomy (OT) was the standard procedure for more than a century because of its excellent surgical reliability, and low morbidity and mortality [1]. New surgical techniques have been introduced for treating PTC to improve patient satisfaction and well-being [2–8].
We introduced a novel gasless endoscopic thyroidectomy method using a transaxillary approach in 2001, and its oncologic outcomes were comparable with conventional open surgical approaches in low-risk PTC patients. Additionally, endoscopic thyroidectomy does not cause a noticeable neck scar [9–11]. With the application of the da Vinci® robot system to endoscopic thyroidectomy beginning in October 2007, our surgeons could complete secure thyroidectomy with more precision and accuracy than endoscopy alone [12–14]. The safety and benefits of transaxillary robotic thyroidectomy (RT) has already been reported worldwide; however, no definitive comparative study has been conducted to compare RT with conventional OT in terms of surgical radicality and oncologic safety [15–24]. Accordingly, this study compared the surgical completeness of transaxillary RT with conventional OT in PTC patients.
Patients and methods
Study population
From January 2011 through October 2012, we conducted a prospective, non-randomized, non-consecutive study in the Department of Surgery at Yonsei University College of Medicine. The study was approved by our Institutional Review Board. The study population included low-risk PTC patients who required low-dose radioactive iodine (RAI) ablation including T1–T3 and/or N0 and N1a. Eligibility criteria were (i) age >20 years; (ii) well-differentiated PTC; (iii) complete surgical resection without residual tumor; and (iv) no abnormal RAI uptake outside the thyroid bed during the first 1.1 GBq RAI ablation therapy Additionally, we confined the study subjects to regional residents to increase patient compliance for additional visits. All patients provided written informed consent to participate voluntarily in this study.
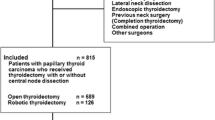
From April 2009 through February 2011, a total of 1,020 PTC patients underwent first-time total thyroidectomy with central compartment neck dissection (CCND) at the Department of Surgery at Yonsei University College of Medicine. The surgical extent was determined according to American Thyroid Association guidelines, and either therapeutic or prophylactic ipsilateral CCND was performed in all patients. Of these, 39 patients who underwent conventional endoscopic thyroidectomy were excluded in this study. We also excluded 177 patients who underwent combined selective neck node dissection for lateral neck node metastasis (N1b), 11 patients with T4 tumor and one with synchronous distant metastasis. Of a total of 792 patients, 471 patients (59.5 %) underwent conventional OT and 321 patients (40.5 %) underwent RT. All patients were offered both open and robotic procedures as options preoperatively, and the decision of surgical method was made according to the patient’s preference. A total of 585 patients (585/792, 73.9 %) received 1.1 GBq RAI ablation therapy after total thyroidectomy based on cancer stage and risk factors. Of these, 355 (60.7 %) were OT and 230 (39.3 %) were RT patients. Of these 585 patients, 102 patients voluntarily participated in this study; however, eight patients did not take the follow-up diagnostic whole-body scan (DxWBS) due to planned pregnancy or personal reasons. In the end, 94 patients (51 OT, 43 RT) were included in the statistical analysis of this study.
All patients received levothyroxine postoperatively to suppress thyroid-stimulating hormone (TSH). Patients received 1.1 GBq RAI ablation therapy after 6–12 weeks post-thyroidectomy. Post-therapy whole-body scans (TxWBS) were acquired 48 h after 131I administration. Diagnostic whole-body scanning with 74 MBq 131I was performed in all patients and thyroid bed uptake was measured 48 h after administration. Thyrotropin simulation was prepared with either levothyroxine withdrawal for 4 weeks, with 2 weeks on/2 weeks off of levotriiodothyronine or human recombinant TSH injection, for both 1.1 GBq RAI ablation and DxWBS. All patients were instructed to follow an iodine-restricted diet for 2 weeks before ablation and DxWBS. Serum thyroglobulin (Tg) levels were regularly measured by radioimmunoassay during follow-up. All patients were examined by neck ultrasonography at 1-year postoperatively and annually thereafter.
Operative methods
Conventional OT was performed using a 5–7 cm collar incision on the anterior neck. After dissecting an adequate subplatysmal flap, the midline of strap muscle was divided to expose the thyroid gland. Thyroidal vessels were individually ligated close to the thyroid gland to preserve the superior laryngeal nerve and parathyroid glands. The entire cervical course of the ipsilateral recurrent laryngeal nerve (RLN) was traced and preserved. Dissection of the contralateral thyroid gland proceeded using a subcapsular maneuver to preserve the RLN and parathyroid glands. Therapeutic or prophylactic ipsilateral CCND was performed in all patients.
The gasless transaxillary RT technique has been previously described [13, 14, 25, 26]. With the patient in the supine position with neck extended, the ipsilateral arm was raised. Via a 5–6 cm vertical incision made at the axilla area, a subcutaneous and subplatysmal flap was made from the anterior chest to the bifurcation of the sternocleidomastoid muscles. The dissection was performed through the avascular space between the two sternocleidomastoid muscle branches and proceeded beneath the strap muscles. After fully exposing the anterior surface of the contralateral thyroid gland, an external retractor was placed to maintain sufficient working space. In the two-incision procedure, an accessory port was inserted in the anterior chest area for placing the Prograsp™ forceps (Intuitive Surgical, Inc., Sunnyvale, CA, USA). The robotic docking procedure was performed as previously described [13, 14, 25, 26]. Thyroidectomy and CCND proceeded in the same manner as for the conventional OT method.
Outcome assessment
The surgical completeness of the RT versus OT method was compared by assessing the amount of remnant thyroid tissue, ablation success rate, extent of nodal dissection, and follow-up ultrasonography images. Remnant thyroid tissue was estimated by serum Tg level (both TSH-stimulated and TSH-suppressed) and by thyroid uptake count ratios on WBS (TxWBS and DxWBS). Stimulated serum Tg was measured before RAI administration in both TxWBS and DxWBS. Thyroid bed RAI uptake was evaluated both quantitatively and qualitatively (positive or negative) [27, 28]. A rectangular region of interest (ROI) was drawn at the thyroid bed area and the radioactivity in the thyroid bed was measured. As a reference value, radioactivity of whole body and another ROI with the same dimensions on the brain area were also measured. The count ratio of the thyroid bed-to-reference area quantitatively denoted the amount of remnant thyroid tissue (Fig. 1). Ablation was considered complete if the DxWBS was negative and/or the serum-stimulated Tg level was <2.0 ng/ml. The extent and radicality of nodal dissection was evaluated by the number of retrieved lymph nodes during CCND. One-year follow-up neck ultrasonography analyzed surgical completeness of the two operative methods. Normal ultrasonography result was defined as no suspicious finding at the thyroid bed or central and lateral lymph node regions.
Assessment of remnant thyroid tissue during whole-body scanning by measuring the RAI uptake ratio between the thyroid bed and reference regions. A Thyroid bed-to-brain ratio; the RAI activity of the thyroid bed (a) and the brain (b). B Thyroid bed-to-whole-body ratio; the RAI activity of the thyroid bed (c, d) and the RAI activity on anterior and posterior whole-body images. RAI radioactive iodine
Statistical analysis
Clinicopathologic characteristics and parameters of surgical completeness were compared between the RT and OT surgical methods. Continuous, quantitative data are expressed as mean ± standard deviation, and categorical, qualitative data as frequencies and percentages. Groups were compared using student’s t test, the Chi squared test, or Fisher’s exact test for quantitative and qualitative variables, as appropriate. Linear mixed model analyses were performed for repeated measures, including amounts of RAI uptake and stimulated serum Tg levels, with the unstructured covariance matrix and the data expressed as mean ± standard error. Post hoc analysis was conducted to adjust multiple comparisons, and an adjusted p value of <0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.1.3 software (SAS Institute Inc., Cary, NC, USA).
Results
The clinicopathologic characteristics of the two groups are shown in Table 1. The mean age of the RT group was significantly younger than the OT group (48.3 vs. 39.8 years, respectively; p < 0.001). In terms of histopathologic characteristics, the mean tumor size, incidence of capsular invasion, multiplicity, and bilaterality were not significantly different between the two groups. Regarding TNM classification, T and N stage were similar between the two groups (p = 0.245 and p = 0.219, for T and N stage, respectively). However, stage III was more frequent in the OT group due to the different age spectrum between the two groups (56.9 vs. 27.9 % in the RT and OT groups; p = 0.007). The incidence of postoperative complications including transient hypocalcemia and transient RLN injury were similar in both groups (transient hypocalcemia incidence 31.4 % in OT vs. 46.5 % in RT, p = 0.143; transient RLN injury incidence 0.0 % in OT vs. 2.3 % in RT, p = 0.457, data not shown).
Surgical completeness of the two groups was compared and data are presented in Tables 2 and 3. Table 2 represents the parameters of surgical completeness at the time of 1.1 GBq RAI ablation therapy. The number of retrieved nodes during CCND were not significantly different between the two groups (6.3 in OT vs. 4.9 in RT; p = 0.058). The stimulated serum Tg level at 1.1 GBq RAI ablation was also similar in the two groups (4.15 ng/ml in OT vs. 4.91 ng/ml in RT; p = 0.674). The RAI uptake ratio at TxWBS, including thyroid bed-to-brain and thyroid bed-to-whole-body ratios, were significantly higher in the RT group versus the OT group (p = 0.004 and p = 0.002 for respective ratios).
Table 3 denotes the completeness parameters after ablation therapy. The suppressed serum Tg levels evaluated 6 months after ablation were similar between the two groups (0.21 ng/ml in OT vs. 0.31 ng/ml in RT; p = 0.326). The DxWBS were performed at an average of 18.0 ± 4.3 months after ablation therapy (range 11–28 months). The stimulated serum Tg levels at DxWBS were also similar between the two groups (2.09 ng/ml in OT vs. 2.60 ng/ml in RT; p = 0.768). Both the thyroid bed-to-brain and thyroid bed-to-whole-body RAI uptake ratios decreased to similar values after ablation therapy in the two groups (p = 0.470 and p = 0.474 for respective ratios). The changes in stimulated serum Tg levels and RAI uptake before and after ablation are shown in Fig. 2.
The changing patterns of surgical completeness parameters before and after 1.1 GBq RAI ablation, according to the robotic or open surgical method. A The RAI uptake ratio between the thyroid bed-to-brain. B The RAI uptake ratio between the thyroid bed-to-whole-body. C TSH-stimulated serum Tg levels. RAI radioactive iodine, Tg thyroglobulin, DxWBS diagnostic whole-body scan
The success rates of 1.1 GBq RAI ablation were also compared between the two groups (Table 3). The ablation success rates based on DxWBSs, stimulated serum Tg levels at DxWBS, and combined WBS and stimulated Tg at DxWBS did not significantly differ between the two groups. The DxWBS was positive in 16 patients (nine OT patients and seven RT patients), and all observed uptake occurred at the thyroid bed. One OT case also showed an abnormal uptake in the lower neck area, which suggested a suspicious metastatic central node. There were no abnormal neck ultrasonography findings at the 1-year follow-up in either group.
Discussion
The incidence of thyroid cancer is increasing worldwide, and the proportion of papillary thyroid microcarcinoma is increasing explosively [29–31]. Early-stage small PTC has an excellent prognosis, allowing emphasis to be placed on patient postoperative quality of life [12, 19]. The transaxillary RT approach has received much attention due to associated improvement in patient postoperative well-being. The early surgical outcomes of RT were comparable with the conventional OT. In addition, translocation of the anterior neck scar to the axilla in RT improved patient cosmesis, satisfaction, and self-consciousness [16, 17, 19, 21]. Preservation of the anterior neck area during flap dissection reduced swallowing difficulty and sensory discomfort, including neck hyperesthesia and paresthesia [15, 19]. Furthermore, less postoperative adhesion formation with RT results in less laryngotracheal fixation, and improves subjective voice function and some objective voice functions, including the mean highest frequency and the frequency range during the early postoperative period versus OT [15].
The application of new techniques in cancer therapy should assure oncologic safety. In this regard, until now the RT approach lacked definitive evidence about recurrence and survival rates. Some surgeons are concerned about the feasibility of performing radical operations with this technique. Short-term follow-up data (mean 29.1 months) of the robotic procedure showed similar results than the conventional open method [17]. However, longer-term follow-up data were previously unavailable because the first adoption of robotic techniques for treating PTC occurred in 2007 [14, 17, 25]. Therefore, we conducted this prospective study to assess the oncologic effectiveness of RT in terms of surgical completeness.
Surgical completeness was assessed by comparing multiple parameters. The serum Tg concentration, especially the TSH-stimulated serum Tg level, is a reliable surrogate marker for assessing remnant thyroid tissue after total thyroidectomy [27, 28, 32–34]. Increased radioactivity in the neck during 131I WBS also provides evidence of remnant thyroid tissue [27, 28, 32–34]. In this study, we compared the RAI uptake of the thyroid bed with two reference regions. The RAI uptake ratios provide a relative quantification of the amount of remnant thyroid tissue [27, 28]. The brain was used as reference background because it is an RAI-poor area due to the blood–brain barrier [28]. Furthermore, the RAI uptake of anterior and posterior whole-body images were also measured because the absorption and excretion of iodine is correlated with patient body surface area. The success rate of 1.1 GBq RAI ablation and follow-up neck ultrasonography were also used to compare the completeness of the two surgical methods [35].
According to American Thyroid Association guidelines, thyroid lobectomy is sufficient for treating low-risk, unifocal, and intrathyroidal PTCs <1 cm in diameter [31]. In PTCs >1 cm, a near-total or total thyroidectomy is recommended, and RAI administration is recommended for all patients with gross extrathyroidal extension of the tumor regardless of tumor size, and in patients with higher risk features based on the combination of age, tumor size, lymph node status, and tumor histology [31]. The goal of RAI administration after total thyroidectomy is (i) normal thyroid remnant ablation to facilitate initial staging and detection of recurrence; (ii) as adjuvant therapy to destroy unproven metastasis to decrease recurrence risk; and (iii) to treat persistent disease [31]. The recurrence rate is reported at approximately 1 % in patients with ablation success [36, 37].
In this study, surgical completeness of both surgical methods was assessed consecutively, before and after 1.1 GBq RAI ablation. Complete thyroid removal was assessed by serum Tg level, RAI activity, and neck ultrasonography [33, 34]. Despite intended radical surgery, thyroid gland removal is often incomplete [29]. Salvatori et al. [38] reported that most patients (93.1 %) had normal thyroid remnants after conventional open total thyroidectomy in both the ipsilateral and contralateral sides relative to the tumor site. The OT approach provides excellent exposure of the thyroid gland and a symmetric operating view, a very small amount of thyroid tissue left during functional preservation of superior laryngeal nerve, parathyroid glands, and RLN [38].
In this study, RAI uptake in the thyroid bed was higher in the RT versus OT group, as assessed in post-therapy WBS, suggesting larger amounts of remnant thyroid parenchyma. In the unilateral approach of transaxillary RT, complete removal of the contralateral thyroid gland is more difficult, especially in patients with a deeply-seated Berry ligament or a prominent Zuckerkandl’s tubercle due to thyroiditis. Furthermore, dissection with the Harmonic curved shears during the robotic procedure requires leaving a very small amount of remnant thyroid tissue at the contralateral Berry ligament area to avoid RLN thermal injury. However, we have also shown that despite the higher thyroid ratios in post-treatment WBS in RT patients, there was no difference in ablation failure rates between RT and OT patients. This indicates that although there might be larger remnant thyroid tissue in RT patients, a routine low-dose RAI (1.1 MBq) dosage is sufficient to successfully ablate remnant thyroid tissue.
The stimulated serum Tg levels after both surgical methods were not significantly different at the time of 131I ablation. Furthermore, they declined after ablation in both groups and were similar between the two groups. Yi et al. [35] also reported that the serum stimulated Tg of RT was similar to OT at and after ablation. Moreover, the ablation success rate, defined by the combination of stimulated serum Tg <2 ng/ml and/or normal DxWBS, was not significantly different between the two surgical methods, and the 1-year follow-up neck ultrasonography revealed no abnormal finding in either groups. In other words, the RT approach leaves more thyroid remnant than OT; however, it is minimal and effectively ablated by low-dose (1.1 GBq) RAI administration.
Regarding nodal dissection, RT can effectively perform clean CCND that is comparable to results obtained with OT. The number of retrieved central lymph nodes during therapeutic and/or prophylactic CCND was not significantly different between the RT and OT approaches, and both groups had similar postoperative complication rates. The lateral RT approach can fully expose the ipsilateral level VI node area. In RT, the pretracheal node was detached from cervical thymic tissues and dissected to the sternal notch inferiorly. The paraesophageal node was fully exposed from the medial side of carotid artery and removed by preserving the RLN until the inferior thyroidal artery was exposed. The prelaryngeal node was also easily dissected with clearance of the pyramidal lobe [13]. Additionally, the contralateral CCND can be successfully performed during RT in the same maneuver after identifying the contralateral RLN [12, 35].
This study has several limitations. First, the mean age was significantly younger in the RT group. Due to higher body image concerns, younger patients prefer a more aesthetic procedure. This different age spectrum was mainly attributable to the discrepancy of TNM stage in this study. Second, our sample size was relatively small and is the experience of RT experts in a single institution. Therefore, a large multicenter trial is needed for defining the practical safety and universal feasibility of RT. Third, we used several parameters instead of patient survival and recurrence to evaluate the completeness of RT. Longer follow-up evaluation may be required to determine the real oncologic safety of RT.
Conclusion
In conclusion, remnant thyroid tissue ablation after transaxillary RT was successfully managed by 1.1 GBq RAI. RT showed similar surgical completeness versus conventional OT, and provides a safe and feasible surgical option for PTC patients.
References
Welbourn RB (1996) Highlights from endocrine surgical history. World J Surg 20(5):603–612
Duncan TD, Ejeh IA, Speights F, Rashid QN, Ideis M (2006) Endoscopic transaxillary near total thyroidectomy. JSLS 10(2):206–211
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83(6):875
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S (2002) Comparative study of thyroidectomies: endoscopic surgery versus conventional open surgery. Surg Endosc 16(12):1741–1745
Lombardi CP, Raffaelli M, de Crea C, Princi P, Castaldi P, Spaventa A, Salvatori M, Bellantone R (2007) Report on 8 years of experience with video-assisted thyroidectomy for papillary thyroid carcinoma. Surgery 142(6):944–951 discussion 944–951
Miccoli P, Berti P, Raffaelli M, Conte M, Materazzi G, Galleri D (2001) Minimally invasive video-assisted thyroidectomy. Am J Surg 181(6):567–570
Miccoli P, Elisei R, Materazzi G, Capezzone M, Galleri D, Pacini F, Berti P, Pinchera A (2002) Minimally invasive video-assisted thyroidectomy for papillary carcinoma: a prospective study of its completeness. Surgery 132(6):1070–1073 discussion 1073–1074
Shimizu K, Akira S, Jasmi AY, Kitamura Y, Kitagawa W, Akasu H, Tanaka S (1999) Video-assisted neck surgery: endoscopic resection of thyroid tumors with a very minimal neck wound. J Am Coll Surg 188(6):697–703
Yoon JH, Park CH, Chung WY (2006) Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 16(4):226–231
Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 100(6):477–480
Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Gasless endoscopic thyroidectomy using trans-axillary approach; surgical outcome of 581 patients. Endocr J 56(3):361–369
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2011) Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg 253(6):1060–1066
Kang SW, Lee SC, Lee SH, Lee KY, Jeong JJ, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 146(6):1048–1055
Kang SW, Jeong JJ, Nam KH, Chang HS, Chung WY, Park CS (2009) Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg 209(2):e1–e7
Tae K, Kim KY, Yun BR, Ji YB, Park CW, Kim DS, Kim TW (2012) Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc 26(7):1871–1877
Tae K, Ji YB, Cho SH, Lee SH, Kim DS, Kim TW (2012) Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years’ experience. Head Neck 34(5):617–625
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2012) Early surgical outcomes comparison between robotic and conventional open thyroid surgery for papillary thyroid microcarcinoma. Surgery 151(5):724–730
Lee J, Yun JH, Nam KH, Choi UJ, Chung WY, Soh EY (2011) Perioperative clinical outcomes after robotic thyroidectomy for thyroid carcinoma: a multicenter study. Surg Endosc 25(3):906–912
Lee J, Nah KY, Kim RM, Ahn YH, Soh EY, Chung WY (2010) Differences in postoperative outcomes, function, and cosmesis: open versus robotic thyroidectomy. Surg Endosc 24(12):3186–3194
Lee J, Na KY, Kim RM, Oh Y, Lee JH, Lee JS, Kim CH, Soh EY, Chung WY (2012) Postoperative functional voice changes after conventional open or robotic thyroidectomy: a prospective trial. Ann Surg Oncol 19(9):2963–2970
Kandil EH, Noureldine SI, Yao L, Slakey DP (2012) Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 214(4):558–564
Landry CS, Grubbs EG, Morris GS, Turner NS, Holsinger FC, Lee JE, Perrier ND (2011) Robot assisted transaxillary surgery (RATS) for the removal of thyroid and parathyroid glands. Surgery 149(4):549–555
Ciabatti PG, Burali G, D’Ascanio L (2012) Single-incision robot-assisted transaxillary surgery for early-stage papillary thyroid cancer. Ann Otol Rhinol Laryngol 121(12):811–815
Aliyev S, Taskin HE, Agcaoglu O, Aksoy E, Milas M, Siperstein A, Berber E (2013) Robotic transaxillary total thyroidectomy through a single axillary incision. Surgery 153(5):705–710
Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc 23(11):2399–2406
Ryu HR, Kang SW, Lee SH, Rhee KY, Jeong JJ, Nam KH, Chung WY, Park CS (2010) Feasibility and safety of a new robotic thyroidectomy through a gasless, transaxillary single-incision approach. J Am Coll Surg 211(3):e13–e19
Lee KE, do Koo H, Im HJ, Park SK, Choi JY, Paeng JC, Chung JK, Oh SK, Youn YK (2011) Surgical completeness of bilateral axillo-breast approach robotic thyroidectomy: comparison with conventional open thyroidectomy after propensity score matching. Surgery 150(6):1266–1274
Im HJ, do Koo H, Paeng JC, Lee KE, Chung YS, Lim I, Lee DS, Chung JK, Youn YK (2012) Evaluation of surgical completeness in endoscopic thyroidectomy compared with open thyroidectomy with regard to remnant ablation. Clin Nucl Med 37(2):148–151
Fratkin MJ, Newsome HH Jr, Sharpe AR Jr, Tatum JL (1983) Cervical distribution of iodine 131 following total thyroidectomy for thyroid cancer. Arch Surg 118(7):864–867
Leger FA, Izembart M, Dagousset F, Barritault L, Baillet G, Chevalier A, Clerc J (1998) Decreased uptake of therapeutic doses of iodine-131 after 185 MBq iodine-131 diagnostic imaging for thyroid remnants in differentiated thyroid carcinoma. Eur J Nucl Med 25(3):242–246
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
Lee KE, Kim E, Koo DH, Choi JY, Kim KH, Youn YK (2013) Robotic thyroidectomy by bilateral axillo-breast approach: review of 1026 cases and surgical completeness. Surg Endosc 27(8):2955–2962
Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, Bardet S, Leenhardt L, Bastie D, Schvartz C, Vera P, Morel O, Benisvy D, Bournaud C, Bonichon F, Dejax C, Toubert ME, Leboulleux S, Ricard M, Benhamou E (2012) Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 366(18):1663–1673
Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L, Nicol A, Clark PM, Farnell K, McCready R, Smellie J, Franklyn JA, John R, Nutting CM, Newbold K, Lemon C, Gerrard G, Abdel-Hamid A, Hardman J, Macias E, Roques T, Whitaker S, Vijayan R, Alvarez P, Beare S, Forsyth S, Kadalayil L, Hackshaw A (2012) Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med 366(18):1674–1685
Yi O, Yoon JH, Lee YM, Sung TY, Chung KW, Kim TY, Kim WB, Shong YK, Ryu JS, Hong SJ (2013) Technical and oncologic safety of robotic thyroid surgery. Ann Surg Oncol 20(6):1927–1933
Cailleux AF, Baudin E, Travagli JP, Ricard M, Schlumberger M (2000) Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? J Clin Endocrinol Metab 85(1):175–178
Pacini F, Capezzone M, Elisei R, Ceccarelli C, Taddei D, Pinchera A (2002) Diagnostic 131-iodine whole-body scan may be avoided in thyroid cancer patients who have undetectable stimulated serum Tg levels after initial treatment. J Clin Endocrinol Metab 87(4):1499–1501
Salvatori M, Raffaelli M, Castaldi P, Treglia G, Rufini V, Perotti G, Lombardi CP, Rubello D, Ardito G, Bellantone R (2007) Evaluation of the surgical completeness after total thyroidectomy for differentiated thyroid carcinoma. Eur J Surg Oncol 33(5):648–654
Acknowledgments
The authors are grateful to Dong-Su Jang (Medical Illustrator, Medical Research Support Section, Yonsei University College of Medicine, Seoul, Republic of Korea) for his help with the figures.
Disclosures
Drs. Sohee Lee, Cho Rok Lee, Seung Chul Lee, Seulkee Park, Haiyoung Son, Sang-Wook Kang, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Cheong Soo Park, Arthur Cho, and Ha Yan Kim have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, S., Lee, C.R., Lee, S.C. et al. Surgical completeness of robotic thyroidectomy: a prospective comparison with conventional open thyroidectomy in papillary thyroid carcinoma patients. Surg Endosc 28, 1068–1075 (2014). https://doi.org/10.1007/s00464-013-3303-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3303-y