Abstract
Purpose
The use of standalone cages (SAC) and anchored cages (AC) in anterior cervical discectomy and fusion surgery (ACDF) has shown advantage of reduced operative time and lower incidence of dysphagia. However, there is limited literature available comparing the clinical and radiological outcomes of SAC and AC.
Methods
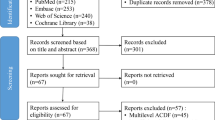
We conducted a prospective study for patients undergoing ACDF for cervical radiculopathy or myelopathy. Patient were classified based on the cage used into SAC group and the AC group. Clinical outcomes were assessed using the modified Japanese Orthopedic Association (mJOA) for myelopathy and Neck Disability Index (NDI) and Visual Analogue Scale (VAS) for radiculopathy. Dysphagia was graded as per Bazaz score. Radiologically, global cervical lordosis, segmental lordosis, cage subsidence, and migration were assessed.
Results
We analyzed 31 patients in each group with a minimum two year follow-up. The mean VAS improved from 7.9 to 4.56, mean NDI score improved from 27.6 to 19.8, and mean mJOA improved from 10.8 to 11.7 which were statistically significant (p < 0.05); however, no significant difference was noted between the SAC and AC groups. Mean global lordosis improved from 14.4 to 20.3° and mean segmental lordosis improved from 6 to 10.1° at six months and plateaued to 6.9° at final follow up without any significant difference between the groups. The subsidence was statistically more in 12.9% (4/31) in SAC than 6.4% (2/31) in AC.
Conclusion
AC showed of lower rates of subsidence while both SAC and AC had comparable clinical outcomes and radiological alignment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) is one of the most common spine surgical procedures performed for treating diverse cervical spine disorders since its first description by Smith and Robinson [1, 2]. The procedure encompasses an adequate decompression of the spinal cord and nerve roots followed by osseous fusion using an interbody spacer. Various interbody spacer constructs have been utilized including autologous bone graft, bone graft substitute, standalone interbody cages, anchored cages, and interbody spacers augmented by an anterior plates [1,2,3,4,5].
Anterior cervical plates with iliac crest bone grafts have been associated with higher rates of dysphagia and donor site morbidity [6,7,8]. To negate this, over the last couple of decades, two interbody implants, i.e., anchored cage (AC) and standalone cage (SAC), have become popular for ACDF surgeries. The evolution of ACDF with the use of SAC and AC provides restoration of height, immediate stability, and restoration of cervical lordosis [9,10,11]. The SAC and AC were able to reduce incidence of dysphagia that is associated with the use of anterior plate system with bone grafts or interbody cages. Interbody cages have been reported to cause complications like cage migration and subsidence [9, 12, 13]. This led to the introduction of AC designs incorporating fixing screw which theoretically provides a scaffold for bony fusion and stability [14,15,16]. However, there is a paucity of literature regarding clinical or radiological difference between the use of either SAC and AC designs. Hence, we attempted to assess the clinic-radiologic outcomes between two such subsets of patients undergoing ACDF, one treated with SAC and the other with AC.
Materials and methods
A prospective study was performed on patients undergoing single level ACDF for clinical symptoms of myelopathy, radiculopathy, or myeloradiculopathy between 2018 and 2020. The study was approved by the institute review board and ethics committee. Written informed consent was taken from all participants and all ethical standards in the Declaration of Helsinki were followed.
All the patients undergoing single level ACDF for degenerative cervical disc disease were included in the study. Patients who had an active infection, traumatic fracture, tumour, and revision surgical procedures were excluded from the study. The patients were divided into two groups: SAC group and AC group. The surgery was performed by three experienced spine surgeons at a tertiary care spine unit with the decision on use of cage design left to the discretion of the operating surgeon.
Clinical assessment
Demographic details were noted and clinical presenting symptoms including any neurological deficit were documented. Pain was assessed using the Visual Analogue Scale (VAS score) and Neck Disability Index (NDI score). Myelopathy was assessed using the modified Japanese Orthopaedic Association (mJOA) score. Clinical follow-up was performed pre-operatively, immediate post-operative, at six months, one year, and two years. Dysphagia was assessed using the Bazaz criteria for severity of difficulty swallowing [17].
Radiological assessment
Plain lateral projection radiographs were studied for global lordosis, segmental lordosis, cage migration, cage subsidence, and radiological fusion using standard definitions reported by previous authors [18,19,20]. MRI findings including level of pathology and Pfirrmann grade of degeneration for the disk were noted [21]. Radiological follow-up was performed preo-peratively, immediate post-operative, at six months, one year, and two years.
Illustrative example of measurement of radiological parameters on the lateral radiograph is shown in Fig. 1. The global lordosis was measured by Cobb’s angle between the end plates of the C2 and C7 vertebrae. The segmental lordosis was measured by Cobb’s angle between superior end plate of cranial vertebrae and inferior end plate of caudal vertebrae of the operated segment. Subsidence was defined as > 2-mm decrease in the anterior or posterior disk height (Fig. 2) and cage migration was the change in distance between the anterior tip of the vertebral body and the anterior tip of the cage [22]. Fusion was assessed as the presence of trabeculae bridging bone formation at the anterior and/or posterior cortex of the involved vertebral bodies and absence of radiolucency through fusion levels.
Showing measurements of global lordosis, segmental lordosis, and disc height at index level for a patient with standalone cage a pre-operative radiograph and b post-operative radiograph. The cobb angle is measured between inferior end plate of C2 and the inferior end plate of C7. The global lordosis is measured at 14.4° pre-operatively and 17.6° post-operatively
Showing a 32-year-old male patient with C56 collapsed disc space with radiculopathy. a Pre-operative radiographs show a collapsed and kyphotic C56 disc space. b The immediate postop radiograph with satisfactory cage placement and restoration of disc height. c The final follow-up radiograph showing cage subsidence; however, the patient continued to remain asymptomatic with good functional outcomes
Surgical procedure
The surgery was performed in the supine position, with the neck and head kept in a slight extension position with a towel roll placed below the shoulders. The standard right-sided Smith-Robinson approach was used to access the anterior vertebral body with intervening discs. Level is confirmed using intra-operative fluoroscopy. Discectomy was done at the desired level, followed by disc space preparation and insertion of the cage, i.e., SAC or AC. Care was taken to prevent breaching the subchondral bone to reduce the risk of subsidence. Cage position was confirmed on intra-operative image intensifier and wound was closed in layers. The patient was given a soft cervical collar to immobilize the spine. Patients were allowed bedside sitting and standing on day one. By day two, patients could be mobilized with support, as per tolerance.
Statistical analysis
Statistical analysis was done using SPSS 27.0 software. Clinical and radiological changes were analyzed using paired t, unpaired t test, and ANOVA test. The statistical significance was defined as p < 0.05.
Results
We analyzed 62 (SAC: n = 31 and AC: n = 31) patients who fulfilled the inclusion criteria and underwent ACDF surgery in this study. Out of 62, 47 were male, and 15 females. The most commonly involved level was C5-6, with the mean age at the time of surgery being 47.8 years (range 17–83). The mean duration of symptoms was 11 ± 3 months (range 8–16 months).
The preop mean VAS, NDI, and mJOA score pre-operatively and post-operatively was comparable for both groups (p > 0.05) (Table 1). The mean VAS improved from 7.9 to 4.56, mean NDI score improved from 27.6 to 19.8, and mean mJOA improved from 10.8 to 11.7 which were statistically significant (p < 0.05); however, no significant difference was noted between the SAC and AC groups for the clinical outcomes and the pain status (Table 2).
There was no significant difference in mean surgical time between SAC (94 ± 12 min) and AC (98 ± 8 min). The amount of blood loss in SAC (80 ± 10 ml) and AC (88 ± 8 ml) was comparable. There was no significant difference in incidence of dysphagia and Bazaz grade of dysphagia between both groups.
Radiological outcome
The mean values for the global lordosis and the segmental lordosis pre-operatively and post-operatively were comparable between the SAC and AC group (p > 0.05) (Table 3). The mean global lordosis improved from 14.4 to 20.3° and mean segmental lordosis improved from 6 to 10.1° at six months and plateaued to 6.9° at final follow-up without any significant difference between the SAC and AC groups (Tables 3 and 4).
Global cervical spine lordosis showed a statistically significant increase at six months postop, from 14.45 to 23.4 ± 1.17, followed by a decrease and plateau to 20.3 ± 1.08 at 2 years. The segmental cervical spine lordosis, for the operated vertebrae, showed a statistically significant increase at six months postop, from 6.1 to 10.1, followed by a drop to 6.9 ± 1.2 at two years follow-up. There was no statistically significant difference between the type of implant used, in either global lordosis or segmental lordosis.
The incidence subsidence as assessed using the anterior/posterior disk space height was seen in six patients out of a total of 62. A total of 13.7% (4/31) in standalone and 6.8% (2/31) in anchored cages were statistically significant. There was cage migration observed in four cases, two in each group as evaluated by a change in the anterior cage distance when compared to the anterior tip of the vertebral body. However, none of the patients with cage migration had clinical symptoms resulting from the same. There were no cases of surgical site infection or radiological nonunion at final follow-up.
Discussion
Traditionally, anterior cervical discectomy and fusion has been carried out using iliac crest grafts as interbody spacers; however, it was associated with donor site morbidity and complications of graft migration, collapse, or expulsion [1]. This was later complemented by the addition of anterior cervical plates to reduce the complications previously mentioned [1, 4]. Anterior plates were associated with higher rates of hoarseness of voice, dysphagia, and oesophageal irritation which led to the introduction of the SAC [7, 9]. Being a lower profile implant, rates of dysphagia encountered were reduced [7, 9]. Evolution in the cage design has seen previous carbon fiber and titanium cages being replaced by PEEK cages (poly ether ether ketone) which are radiolucent and have a young’s modulus closer to bone thereby theoretically reducing the risk of subsidence [1, 2, 18].
Cervical radiculopathy and myelopathy treated with ACDF have provided satisfactory outcomes [5, 7, 13, 18]. A review of the preexisting literature yielded comparative studies between the cage + anterior plate and SAC or AC. However, we found limited literature comparing outcomes of SAC with AC [23].
Cho et al. published the only report on comparison on PEEK cages (SAC) and AC cages and noted that the clinical outcomes assessed using NDI and VAS score showed no statistically significant difference between the two groups [24]. However, there was improved segmental lordosis and disc height and reduced subsidence in the AC group. These findings were comparable to our results for the clinical outcomes and subsidence. However, the segmental lordosis and global lordosis in our series did not show a significant difference between the SAC and AC groups.
Dysphagia is recognized as a common complication following ACFD and rates with the use of anterior cervical plates are reported to be more than SAC and AC [7, 25, 26]. Wang et al. [25] reviewed multicentric retrospective data and reported a 20% dysphagia in the immediate post-operative period which reduced to 1.1% at 1-year follow-up. Li et al. [27] reported an incidence of 5.9% postoperative dysphagia in the SAC group and 12.9% in the cage and plate group which reduced to 1.5% and 4.5%, respectively, at the three month follow-up. They concluded that the SAC had an advantage in lowering dysphagia. We observed an incidence of 9% transient dysphagia in the postoperative period with none of the patients reporting dysphagia at one year follow-up. In our study, the dysphagia was only of mild grade as per Bazaz score and the rates did not differ significantly in the two groups.
We assessed radiological outcomes using the segmental and global cervical lordosis, subsidence, and cage migration. The occurrence of poorer clinical outcomes in ACDF surgeries is correlated with the occurrence of subsidence and local kyphosis at the index level [10, 11]. Our study reported improvement in the segmental lordosis and global lordosis for both groups, which were well-maintained at final follow-up without difference between the groups. Cho et al. [24] noted that the segmental lordosis in their series declined for SAC and AC over time; however, the decline in the anchored group was lower favouring better lordosis maintenance with the AC group.
Authors have reported that post ACDF procedure, the kyphotic malalignment promotes degenerative changes in adjoining vertebrae and adjacent segment degeneration [2, 20, 28]. The presence of pre-operative segmental kyphosis has been reported to correlate with higher chance of cage subsidence [24, 29]. In our series, the patients with subsidence did not show any features of adjacent segment degeneration at two years follow-up and the pre-operative segmental alignment was kyphotic in one patient out of six as seen in Fig. 2. Suggesting other factors such as age, bone mineral density may have an impact on subsidence [28].
Post fusion surgery, the bone remodeling process is associated with the settlement of the cage into the vertebral body [12]. Previous authors have defined subsidence of cage as sinking of the cage and loss of disc height by more than 2 mm which has been associated with poorer clinical outcomes and recurrence of symptoms [2, 13]. Bartels et al. noted that subsidence is a coupled process of bone resorption and formation, which takes place over several months [12]. We observed subsidence rates of 6.8% (2 out of 31) in anchored cages and 13.7% (4 out of 31) in patients with standalone cages. Comparatively, other studies have reported subsidence rates ranging from 7% in a study by Hida et al. [30] of 146 patients to 82% in a study of 96 patients by Kim et al. [29] with the use of cylindrical cages. The study by Kim et al. reported no impact on clinical outcome even with significant rates of subsidence [29]. Similarly, on our series, the six patients with subsidence did not show worse or poorer clinical outcomes at two year interval.
Previous studies have shown subsidence to be related to numerous factors such as disk space over distraction, end plate damage during curettage, or forceful implantation of the cage [4, 29,30,31]. There are several factors that can reduce the incidence of cage subsidence which include end plate preservation, large contact surface, and increased bone mineral density [29]. Although the AC group had lower subsidence, numerous confounding factors such as age, bone mineral density, and surgical technique may contribute to subsidence. Subsidence was more frequently observed over the superior end plate of the inferior vertebral body in five out of the six cases. This may be attributed to lower mineralization at the superior end plate when compared to the inferior end plate. The limitation of our study includes the fact that these confounding factors for subsidence have not been studied and the sample size in each of the groups is small. The use of the AC or the SAC was left to the discretion of the operating surgeon and this can be source of selection bias. However, both cage designs were used in comparable numbers during the course of the study. Since the clinical and radiological results were comparable, it appears that the cage design does not impact the clinical outcomes at the 2 years follow-up. No randomized control trial has been performed to compare outcomes for SAC and AC and this could be area for future potential research.
In conclusion, both anchored cages and standalone cages have comparable clinical outcomes. The radiological outcomes for cervical lordosis and sagittal alignment are comparable at two years follow-up. However, anchored cages may have a lower rate for subsidence. The addition of anchoring screws however does not completely negate the risk of subsidence and cage migration.
Data availability
Data is not a part of a public repository.
References
Chong E, Pelletier MH, Mobbs RJ, Walsh WR (2015) The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord 16:1–11
Korinth MC (2008) Treatment of cervical degenerative disc disease–current status and trends. Cen Eur Neurosurg 69:113–124
Iwasaki K, Ikedo T, Hashikata H, Toda H (2014) Autologous clavicle bone graft for anterior cervical discectomy and fusion with titanium interbody cage. J Neurosurg Spine 21:761–768
Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34:2886–2892
Anderson DG, Albert TJ (2002) Bone grafting, implants, and plating options for anterior cervical fusions. Orthopedic Clinics 33:317–328
He S, Zhou Z, Lv N, Shao X, Zhou X, Wang Y et al (2021) Comparison of clinical outcomes following anterior cervical discectomy and fusion with zero-profile anchored spacer-ROI-C-fixation and combined intervertebral cage and anterior cervical discectomy and fusion: a retrospective study from a single center. Med Sci Monit: Int Med J Exp Clin Res 27:e931050–e931051
Vaishnav AS, Saville P, McAnany S, Haws B, Khechen B, Singh K et al (2019) Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine 44:E400–E407
Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK (2010) Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc 48:342
Nemoto O, Kitada A, Naitou S, Tachibana A, Ito Y, Fujikawa A (2015) Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol 25:127–134
Fujibayashi S, Neo M, Nakamura T (2008) Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci 15:1017–1022
Oh JK, Kim TY, Lee HS, You NK, Choi GH, Yi S et al (2013) Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. Clin Spine Surg 26:415–420
Bartels RH, Donk RD, Feuth T (2006) Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 58:502–508
Kast E, Derakhshani S, Bothmann M, Oberle J (2009) Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 32:207–214
Wang Z, Jiang W, Li X, Wang H, Shi J, Chen J et al (2015) The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J 24:148–154
Hofstetter CP, Kesavabhotla K, Boockvar JA (2015) Zero-profile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating. J Spinal Disord Tech 28:E284–E290
Dufour T, Huppert J, Louis C, Beaurain J, Stecken J, Aubourg L, Vila T (2010) Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one year follow-up. Br J Neurosurg 24:633–640
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458
Li J, Lei T, Shen Y (2015) The impact of Modic-2 changes on the clinical outcomes of single-level anterior cervical discectomy and fusion. Eur Spine J 24:2936–2940
Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS (2014) Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg Soc 56:103
Oh K, Lee CK, You NK, Kim SH, Cho KH (2013) Radiologic changes of anterior cervical discectomy and fusion using allograft and plate augmentation: comparison of using fixed and variable type screw. Korean J Spine 10:160
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516
Han SY, Kim HW, Lee CY, Kim HR, Park DH (2016) Stand-alone cages for anterior cervical fusion: are there no problems? Korean J Spine 13:13
Cho HJ, Hur JW, Lee JB, Han JS, Cho TH, Park JY (2015) Cervical Stand-alone polyetheretherketone cage versus zero-profile anchored spacer in single-level anterior cervical discectomy and fusion: minimum 2-year assessment of radiographic and clinical outcome. J Korean Neurosurg Soc 58:119
Wang T, Ma L, Yang DL, Wang H, Bai ZL, Zhang LJ, Ding WY (2017) Factors predicting dysphagia after anterior cervical surgery: a multicenter retrospective study for 2 years of follow-up. Medicine 96:34
Tervonen H, Niemelä M, Lauri ER, Bäck L, Juvas A, Räsänen P et al (2007) Dysphonia and dysphagia after anterior cervical decompression. J Neurosurg Spine 7:124–130
Li Z, Zhao Y, Tang J, Ren D, Guo J, Wang H, Li L, Hou S (2017) A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J 26:1129–1139. https://doi.org/10.1007/s00586-016-4739-2
Lee YS, Kim YB, Park SW (2014) Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine 39:1280–1287
Kim S, Chun HJ, Yi HJ, Bak KH, Kim DW, Lee YK (2012) Long-term follow-up radiologic and clinical evaluation of cylindrical cage for anterior interbody fusion in degenerative cervical disc disease. J Korean Neurosurg Soc 52:107
Hida K, Iwasaki Y, Yano S, Akino M, Seki T (2008) Long-term follow-up results in patients with cervical disk disease treated by cervical anterior fusion using titanium cage implants. Neurol Med Chir (Tokyo) 48(10):440–446. https://doi.org/10.2176/nmc.48.440
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4:447–453
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr Siddharth Aiyer, Dr Shailesh Hadgaonkar, and Dr Ajay Kothari. The first draft of the manuscript was written by Dr Niharika Virkar and Dr Pramod Bhilare and critical revision was done by Dr Siddharth Aiyer. Project administration was carried out by Dr Parag Sancheti. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Sancheti Institute for Orthopaedics and Rehabilitation Institute Ethics Committee (Date: 2/11/2019 /No:IEC-SIOR/Agenda 058).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publications
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1 and 2.
Conflict of interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Virkar, N., Bhilare, P., Hadgaonkar, S. et al. Standalone cage versus anchored cage for anterior cervical discectomy and fusion: a comparative analysis of clinical and radiological outcomes. International Orthopaedics (SICOT) 46, 2339–2345 (2022). https://doi.org/10.1007/s00264-022-05493-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05493-z