Abstract
Purpose
To compare perioperative parameters, clinical outcomes, radiographic parameters, and complication rates of the new zero-profile, stand-alone Fidji cervical cage with those of the stand-alone cages with a titanium plate for anterior cervical discectomy and fusion (ACDF) for the surgical treatment of single- and multilevel cervical degenerative disc disease (DDD).
Methods
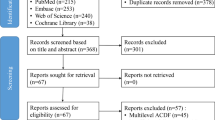
Between October 2009 and December 2013, 152 consecutive patients [86 males and 52 females; mean age 51.0 years (range 30–69 years)] with cervical DDD, who underwent surgery and were followed for more than 2 years, were enrolled in this study and divided into the cage group and plate group. The study compared perioperative parameters, surgery-related and implant-related complication rates, clinical outcomes, and radiologic parameters.
Results
The clinical and radiologic results in both groups were satisfactory after a minimum 2-year follow-up. No significant differences between the cage group and plate group in terms of improvement in the 36-Item Short Form Health Survey, visual analogue scale, Neck Disability Index, Japanese Orthopedic Association scores, disc height, mean fusion time, fusion rate, adjacent segment degeneration, and restoration of cervical lordosis, but the cage group was associated with a lower risk of postoperative dysphagia, shorter operation time, less blood loss, less cost of index surgery, and relatively greater simplicity than the plate group.
Conclusions
The zero-profile, stand-alone Fidji cervical cage for ACDF is an effective, reliable, and safe alternate to the conventional method for the treatment of cervical DDD. However, there is no definitive evidence that Fidji cervical cage has better intermediate-term outcomes than the stand-alone cages with a titanium plate for ACDF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The anterior approach to surgical treatment of cervical degenerative disease was first described by Smith and Robinson and popularized by Cloward in the 1950s [1]. Currently, anterior cervical discectomy and fusion (ACDF) is considered to be the definitive surgical treatment for symptomatic, single-, and multilevel, cervical degenerative disc disease (DDD). Many studies reported that ACDF is highly effective in terms of resolving symptoms, improving nerve function, and restoring the physiological curvature of the cervical spine [1–5]. Many surgeons prefer to add an anterior plating system in fusion procedures for increasing the immediate postoperative stability after bone grafting between vertebral bodies, as several studies suggest that this may enhance rigidity of fixation and decrease risk of nonunion, increase interbody fusion rates and stability, maintain or improve cervical lordosis, and prevent interbody graft dislocation or subsidence, particularly in multiple-level ACDFs [6–8].
Although the profile of the current anterior plating system is lower than that of earlier designs, they are still somewhat bulky and might pose a substantial risk of hardware-related complications, such as screws or plate dislodgement, soft-tissue injury, tracheoesophageal lesions, spinal cord or nerve injury, and dysphagia [9–13]. The reported rate of transient dysphagia after ACDF ranges from 2 to 67 % in the early postoperative period [14–25]. Mostly, these symptoms disappear during the first 3 months after surgery, but not all patients recover completely from swallowing problems [14, 17, 21, 23]. The incidence of chronic dysphagia-related symptoms after ACDF ranges from 3 to 21 % in the current literature [11, 22, 24, 25]. In addition, the screw–plate interface might lead to postoperative complications. Cases of migrating screws and subsequent soft-tissue damage are reported [26, 27]. Furthermore, Park et al. [28] demonstrated a higher incidence of adjacent segment degeneration (ASD) if an additional plate was used. The authors stated that this finding is consistent with inappropriate sized or misaligned plates interfering with the adjacent-level disc space. Yang et al. [29] supported this thesis, demonstrating lower rates of ASD performing ACDF without plates.
Limitations and problems with ACDF using a traditional plate method have led some investigators to explore a new device to potentially avoid these complications [23, 30–34]. In the past few years, a new zero-profile, stand-alone device (Fidji cervical cage, Abbott Spine, Bordeaux, France) for ACDF has attracted attention as a possible treatment for cervical DDD, with the aim to reduce the morbidity associated with the traditional cervical anterior plating system, while maintaining the benefits of interbody cages with anterior plating system [34]. Fidji cervical cages, made of PEEK material, are available in different shapes and sizes (Fig. 1). The anatomic shape fits with the vertebral endplate, and the implant cage has a lordotic angle. In sagittal section, it is trapezoid shaped to provide a degree of lordosis. A removable autostatic fin that juts out on top and bottom of the implant gives an immediate stability. Anti-backout teeth act also as additional stabilizers. Implants are available also with different heights, and interior surface allows placing bone graft or bone substitute. As a result, Fidji cervical cage has a hard frame that resists spinal loading and maintains spinal alignment.
From October 2009 to December 2013, we performed ACDF using Fidji cervical cage in 68 patients. We report our experience on a retrospectively collected series of patients treated with the Fidji cervical cage, at single or multiple levels, and followed up to a minimum 2 year after surgery; indications, tips, and tricks related to such new device are described. To the best of our knowledge, this is the largest series of patients, with the longest available follow-up, reported in the literature. The objective of this study was to compare clinical and radiologic results of cervical spine procedures using the Fidji cervical cage with those using a traditional plate method for ACDF, and to assess the role and limitations of the new zero-profile, stand-alone device for the treatment of cervical DDD.
Materials and methods
Patient population
This was a retrospective clinical study. This study was approved by the ethics statement of our hospital (First Affiliated Hospital of PLA General Hospital, Beijing). Between October 2009 and December 2013, 152 consecutive patients who underwent ACDF for cervical DDD by a single surgeon in our spine surgery center took part in the study. Fourteen patients were excluded, because they had not completed their 1-year follow-up. Written informed consent was given by participants for their clinical records to be used in this study. All patients underwent X-ray, computed tomography (CT), and magnetic resonance imaging (MRI). Inclusion criteria were: (1) myelopathy or radiculopathy on the physical examination; (2) spinal cord or root compression visible on recent MRI at single- or multilevel; and (3) no response to at least 6 weeks of conservative treatment. Exclusion criteria were: (1) significant segmental instability and developmental stenosis; (2) a history of cervical spine surgery and other cervical diseases, including fracture, tumor, infection, or severe osteoporosis; and (3) a requirement for simultaneous anterior and posterior surgery.
Ultimately, 138 patients (86 males and 52 females) were deemed eligible for inclusion in the study. The mean age of patients was 51.0 years (range 30–69 years), and the mean duration of symptoms was 24.5 months (range 6–50 months). The average body mass index (BMI) was 28.7 (range 16.1–51.4). Sixty-eight patients who received the stand-alone Fidji cervical cage (cage group) between September 2011 and December 2013 were compared with 70 patients who received a conventional intervertebral spacer with anterior plating (plate group) between October 2009 and September 2011. The patients’ demographic data and number of treated segments are shown in Table 1. There were no statistically significant differences for patient sex, age, BMI, number of treated segments, symptom duration, follow-up time, or hospital stay among the two treatment groups. (p > 0.05, Table 1).
Surgical technique
Each patient received preoperative intravenous antibiotics. All procedures were performed through a transverse skin incision on the right side of the neck. Discectomy and decompression were performed using a surgical approach similar to that described by Smith and Robinson [1], with preservation of the uncovertebral joints to minimize soft-tissue damage and bleeding and to avoid damage to the bony endplates. To reduce new bone formation at bleeding sites, soft-tissue bleeding was meticulously controlled, and damaged bone was covered with bone wax. The posterior longitudinal ligaments were completely removed only when they were torn preoperatively. The cartilaginous endplate was removed completely to expose he cortical endplate. The bony endplate was preserved as such as possible to prevent cage subsidence.
The cage group: an appropriate-sized Fidji cervical cage was selected following the completion of discectomy and endplate preparation. The inner cavity of the cage was filled with autologous cancellous bone. The cage size was determined by both preoperative templating and intra-operative evaluation using a trial cage to confirm initial stability. The cage was inserted into the disc space using an impactor, and cage stability was confirmed after the distracter was removed. The plate group: the appropriate size for stand-alone cage was determined by both preoperative templating and intra-operative evaluation using a trial cage to confirm optimal implant size. A PEEK cage (DePuy Spine, Johnson & Johnson, New Brunswick, NJ, USA) was packed with autologous cancellous bone and inserted into the disc space as described above. After removal of the Caspar distractor, the self-tapping screws were used cranially and caudally to fix the SLIMLOC or SKYLINE anterior cervical plate (DePuy Spine, Johnson & Johnson, New Brunswick, NJ, USA). Operations were performed under fluoroscopic guidance. All patients were immobilized in a Philadelphia collar for 12 weeks postoperatively.
Data collection and outcome evaluations
The data collected included epidemiological data, operative segment, intra-operative blood loss, operation time, length of hospital stay, cost of index surgery, complications, and clinical and radiological parameters. Perioperative information was collected from the anesthesia records.
All outpatients visit at postoperative 1 week, 3, 6 months, and every 6 months thereafter. Follow-up clinical examinations were obtained by a physician unrelated to the surgical procedures. All patients were asked to complete questionnaires before surgery and at each follow-up examination. The self-reported measures used were the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) [35], Neck Disability Index (NDI) [36], and visual analogue scale (VAS) scores. Myelopathy was graded using the Japanese Orthopedic Association (JOA) score [37]. The incidence of dysphagia was recorded using the system defined by Bazaz [14]. Severity of dysphagia was graded as none, mild, moderate, or severe (Table 2). The presence of dysphagia was evaluated at 1 weeks postoperatively and at 3 months postoperatively.
Preoperative imaging included anterior–posterior (AP) and lateral X-rays, with flexion–extension views, CT and MRI. The cervical spine static and dynamic X-rays were obtained at each follow-up. Cervical lordosis was assessed using the of C2–C7 Cobb angle, the angle formed by the two lines drawn perpendicular to the inferior endplates of the C2 and C7 vertebral bodies in a neutral position. The disc height (DHI) was measured on the lateral X-ray as the distance from the highest portion of the lower endplate of the cephalad vertebra to the closest portion of the upper endplate of the caudal vertebra [31]. The occurrence of subsidence was investigated. Subsidence is defined as loss of height of more than 2 mm at any of the two measured disc heights [38]. A solid fusion was considered present if the following features were observed: (1) no motion across the fusion site on flexion–extension X-rays, (2) trabeculae across the fusion site, or (3) no lucency across the fusion site or around any of the screw sites. If the fusion was questionable, sagittal reconstructive CT scans were performed. Degenerative changes in the adjacent segments were evaluated on MRI at the final follow-up. Disc degeneration was graded on T2-weighted sagittal and axial images using the five-point scale as described by Miyazaki [39]. To correct for intra-observer and inter-observer differences in radiological measurements, three experienced observers independently evaluated radiological outcomes.
Statistical analyses
All analyses were performed using the Statistical Package for the Social Sciences for Windows, version 22.0 (SPSS Inc., Chicago, IL, USA). Quantitative data were expressed as the mean ± standard deviation. Inter-group comparisons were performed using the t test or Wilcoxon signed-rank test. Clinical and radiological data before and after surgery were compared using the mixed effect model. Qualitative data were expressed as rate or proportion. Inter-group comparisons were performed using Pearson’s Chi-square test or Fisher’s exact test. Any value of p < 0.05 was considered to indicate statistical significance.
Results
Surgical outcomes
All cases were followed up for more than 2 years postoperatively (median 26 months, range 24–48 months). The Fidji cervical cages were implanted in 68 patients (123 segments). The plate group consisted of 70 patients (122 segments) treated with stand-alone cages and a titanium plate. The surgical outcomes of these patients are summarized in Table 3. Operation time and blood loss were significantly less in the cage group compared with the plate group (73.2 ± 22.3 vs 81.2 ± 19.5 min, 54.6 ± 33.3 vs 75.7 ± 46.8 mL, p < 0.05). There was significantly less cost of index surgery including implant cost in the cage group compared with the plate group (US $6478.2 ± 836.6 vs 7510.8 ± 899.9, p < 0.05).
Clinical outcomes
The clinical outcomes of these patients are summarized in Table 4. The SF-36, VAS, NDI, and JOA scores of all patients, including both the cage and plate group, were improved significantly after surgery at any time point (all p < 0.05). There were no significant differences between the two groups in the SF-36, VAS, NDI, and JOA scores at any time point (all p > 0.05).
Radiological outcomes
The radiological outcomes of these patients are summarized in Table 5. In the cage group, the C2–C7 Cobb angle was 10.78° ± 2.30° before surgery, 14.22° ± 1.48° 1 week after surgery, 14.15° ± 1.49° 3 months after surgery, and 14.01° ± 1.47° at the final follow-up. In the plate group, the C2–C7 Cobb angle was 10.62° ± 2.24° before surgery, 14.63° ± 1.51° 1 week after surgery, 14.59° ± 1.38° 3 months after surgery, and 14.49° ± 1.70° at the final follow-up. The C2–C7 Cobb angle of all patients, including both the cage and plate groups, were improved significantly after surgery at any time point (all p < 0.05, Table 5). The C2–C7 Cobb angle showed different degrees of reduction at the 3 months after surgery and the final follow-up comparing 1 week after surgery in both two groups. However, no significant difference was noticed between the postoperative period and the last follow-up (all p > 0.05). There were no significant differences between the two groups in the C2–C7 Cobb angle at any time point (all p > 0.05).
In the cage group, the DHI was 6.13 ± 1.75 mm before surgery, 7.26 ± 1.17 mm 1 week after surgery, 6.85 ± 0.85 mm 3 months after surgery, and 6.63 ± 0.79 mm at the final follow-up. In the plate group, the DHI was 6.06 ± 1.58 mm before surgery, 7.33 ± 1.21 mm 1 week after surgery, 7.11 ± 1.04 mm 3 months after surgery, and 7.09 ± 1.02 mm at the final follow-up. The DHI of all patients in both two groups was restored significantly after surgery at any time point (all p < 0.05). However, from 3 months after surgery to final follow-up, the DHI in both two groups showed a significant reduction comparing 1 week after surgery (all p < 0.05). There was significant difference in the change in DHI at the final follow-up between the cage and plate groups (p = 0.0041).
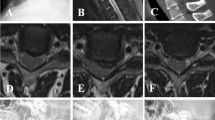
At final follow-up, the fusion rates were 91.2 % (62/68) in the cage group, and 92.9 % (65/70) in the plate group, which was not a significant difference between groups (p = 0.7155). The radiologic mean fusion time was 9.7 ± 3.9 months in the cage group, and 9.0 ± 3.6 months in the plate group. Although the radiologic mean fusion time slightly prolonged in the cage group comparing the plate group, no significant difference (p = 0.248) was noted. Radiological evidence of ASD was observed in 4/41 patients (9.8 %) in the cage group and 8/49 patients (16.3 %) in the plate group, which was not a significant difference between groups (p = 0.3611). A typical case is shown in Fig. 2.
A 53-year-old male had experienced numbness in both hands and weakness in all four extremities for 2 years. Preoperative cervical lateral X-rays (a) and sagittal T2-weighted MRI (b) showed degenerative disc disease and spinal cord compression at C3–C4, C4–C5, and C5–C6. The patient underwent 3-level ACDF with the new zero-profile, stand-alone Fidji cervical cage. Postoperatively, the patient was satisfied and showed an excellent clinical result. Postoperative AP and lateral X-rays (d, e) showed that the relatively good alignment of C2–C7 was identified, and Fidji cervical cages were in good position. Postoperative sagittal T2-weighted MRI (e) showed decompression of the spinal cord at C3–C4, C4–C5, and C5–C6. CT sagittal reconstruction (f) 1 year after surgery showed sound bone fusion mass was noted. At final follow-up, flexion–extension lateral X-rays (g, h) showed satisfactory stability in the fusion segments
Complications
The complications of these patients are summarized in Table 6. In the cage group, postoperative complications included epidural hematoma (1 case), hoarseness (1 case), dysphagia (5 cases), axial neck pain (2 cases), and subsidence (12 segments). In the plate group, postoperative complications included cerebral fluid leakage (1 case), epidural hematoma (2 cases), hoarseness (3 cases), dysphagia (13 cases), axial neck pain (1 case), infection (1 case), new neurological deficit (1 case), implant dislodgement (1 case), implant malposition (2 cases), hardware breakage (2 cases), and subsidence (9 segments).
Although postoperative complications were similar in both surgical groups, we found a marked difference in postoperative dysphagia. Transient postoperative dysphagia (<3 months) was found in 5.9 % of patients in the cage group and 12.9 % of patients in the plate group. Although complaints of dysphagia persisted beyond 3 months in only one patient in the cage group, they were recorded in four patients in the plate group. Thus, dysphagia was significantly more frequent in patients with ACDF using an additional anterior plate compared with patients who receive the stand-alone Fidji cervical cage (p = 0.049). The severity of dysphagia lasting >3 months was in the vast majority of patients mild. One patient in the cage group and two patients in the plate group experienced mild dysphagia lasting >3 months after the surgery. Another patient had moderate dysphagia with difficulties swallowing liquid. One patient in the plate group suffered from severe dysphagia with frequent swallowing difficulties eating solid food. He underwent a swallow evaluation that revealed partial aspiration of food.
Discussion
ACDF is an effective and safe procedure for the surgical treatment of patients with radiculopathy and myelopathy. However, the use of an additional anterior plate is associated with various intra-operative and postoperative complications. Several complications have been described, for example, screw loosening and soft-tissue damage by migrated screws, chronic dysphagia, and ASD [2, 9–13, 27–29, 40–42]. In this study, we described the clinical and radiographic results of a new ACDF technique using the cage with a new zero-profile, stand-alone device. We asked whether this new implant would be associated with a low rate of dysphagia and other complications in patients having this ACDF procedure would be able to achieve solid fusion and maintain postoperative clinical outcomes.
Solid bony fusion constitutes a goal of ACDF, because nonunion has been linked to poor outcomes [7]. Only stable bony fusion prevents delayed kyphotic deformity with concomitant foraminal stenosis causing root compression and neck pain [41, 43]. In a literature review of 25 studies with overall 2682 patients, Fraser et al. [44]. were able to document a significantly increased rate of fusion if an additional anterior plate has been used for either single-level or multilevel ACDF procedures (92.1 %). A similar rate of bony fusion was detected in our study who underwent ACDF with anterior plating (92.9 %). Importantly, we found that the new zero-profile, stand-alone device was associated with a comparable rate of bony fusion (91.2 %). In addition, the SF-36, VAS, NDI, and JOA scores of all patients in both two groups were improved significantly after surgery at any time point. There were no significant differences in surgical and clinical outcomes between the two groups during the follow-up period. However, Fidji cervical cage was associated with shorter operation time, less blood loss, less cost of index surgery, and relatively greater simplicity than the stand-alone cages with a titanium plate for ACDF.
Dysphagia is a well-known complication after ACDF using an additional anterior plate. Previous studies have demonstrated that the incidence of postoperative dysphagia can reach up to 71 %, and persistent dysphagia can reach 35.1 % even at 7.2 years after ACDF with an anterior cervical plate [14, 17, 21, 23]. Several studies, based on analysis of a small sample size, have reported the application of the zero-profile implant system (Zero-P, Synthes GmbH, Switzerland). However, the incidence of postoperative dysphagia ranges from 0 to 76 % [23, 30, 32, 45, 46]. For the early postoperative period, the rate of dysphagia in our study is similar to that in the current literature [14, 17, 21, 23]. However, in comparison with the published data [11, 22, 24, 25], the incidence of chronic dysphagia in our patients was low after implantation of the Fidji cervical cage (1.5 %). Although the exact pathophysiologic mechanism of dysphagia after ACDF procedures is not well understood, many hypotheses have been proposed [16, 17, 20, 24, 25, 47]. According to Fountas et al. [11], postoperative soft-tissue edema, esophageal injury, postoperative hematoma, and adhesive formations around implanted cervical plates might be possible explanations for dysphagia-related symptoms. The anterior cervical locking plate is placed directly posterior to the esophagus and may impinge or irritate the esophagus. It has been demonstrated that design and thickness of anterior locking plates correlate with postoperative dysphagia. According to Lee et al. [21], there is a correlation between plate thickness and dysphagia rate, with decreased dysphagia incidence when thinner plates were used. The zero-profile Fidji cervical cage is not placed across the anterior vertebral body, and can be completely contained in the decompressed intervertebral space, avoiding the mechanical stimulus to the esophagus and other pre-vertebral soft tissues, preserving as many normal anatomical tissues as possible. This may explain the lower postoperative dysphagia incidence in the cage group in our study. Another possible mechanism for postoperative dysphagia after ACDF with anterior plating may be additional traction required to place an anterior locking plate. Increased pressure on the esophagus during implantation of an anterior plate has also been suggested to contribute to dysphagia in patients who undergo ACDF with anterior plating [47]. Future randomized controlled multicenter studies focusing on the mechanisms of dysphagia and methods to reduce the incidence of dysphagia are needed.
The exact pathophysiologic mechanism of ASD remains unknown [28, 29, 40, 48–51]. ACDF has a high rate of clinical success for the treatment of cervical DDD, but the rigid fixation may result in ASD, which could eventually lead to a need for additional treatment [28, 29, 51]. The presence of a plate is also likely to accelerate degenerative changes in adjacent segments, which increased motion and increased intra-discal pressure have been reported in the untreated levels adjacent to fused levels [49–53]. Hilibrand et al. [52] reported that approximately 25 % of patients who underwent single-level ACDF developed ASD within 10 years. The Fidji cervical cage minimizes such risk of inducing adjacent disc level degeneration and spondylotic changes as it remains within the index disc space, far from adjacent-level disc spaces; and correct plate position (i.e., not reaching the adjacent disc space) has been shown to be associated with a lower incidence of ASD. Nonetheless, Miao et al. [54] pointed out that a longer observation is necessary to determine whether or not these devices can also reduce the rate of ASD.
The stand-alone cage has been used widely in clinical practice, and successful clinical results have been reported in more than one study, although the reliability of this technique remains controversial [4, 55–59]. One of the major concerns about stand-alone cage used for ACDF is the cage subsidence [38, 57, 58, 60]. During the process of bone remodeling, settlement of the cage of less than 2 mm into the vertebral bodies until fusion is to be expected [38]. If the cage subsides into the vertebral body, however, with disc collapse, foraminal height and the cervical alignment would fail to restore, thus influencing the clinical outcome. The incidence of cage subsidence and its consequences among the literatures were quite different [38, 57, 58, 60]. Gercek et al. [38] reported that 5 of 8 patients (9 levels, 62.5 %) had radiological signs of cage subsidence, and recommended additional stabilization is necessary to avoid this problem, though cage subsidence did not correlate with clinical symptoms. In a prospective study [60], subsidence was present in 30 of the 67 (44.8 %) fused segments of ACDF using a titanium cage, but the height of the foramen was well maintained among the subsidence cases. In our study, the incidence of cage subsidence was 9.8 % in the cage group and less than that by the majority of other authors. In addition, we found an interesting phenomenon. All cases with cage subsidence were noted at a 3-month follow-up, indicating that the subsidence did not progress during that time, probably because of fusion. For the subsidence cases, the disc height of the treated level at the final follow-up remained significantly greater than that before surgery. Despite cage subsidence, the long-term clinical outcome of patients of subsidence remained satisfactory. In our opinion, risk factors for progressive cage subsidence include instability created by discectomy, postoperative cervical motion, cage design, oversized cage insertion with excessive distraction to obtain immediate stability, endplate preparation (excessive resection), and low bone mineral density.
Cervical lordosis is considered to play an important role in the maintenance of surgical results [5, 61–64]. Sagittal malalignment will cause an increased distribution of stress on internal fixation devices and the adjacent segments, which will increase the incidence of failure of internal fixation and disease in adjacent segments [63, 64]. Inadequate recovery of cervical lordosis after ACDF has a strong and consistent influence on to the cervical instability, postoperative axial pain, and the deterioration of neurological deficit, and may influence the functional recovery [62–64]. In our study, cervical lordosis significantly improved in both the cage and plate group at final follow-up. The SF-36, VAS, NDI, and JOA scores of all patients in both two groups were improved significantly after surgery at final follow-up, and postoperative clinical outcomes was well maintained.
The use of all generations of cervical anterior plates is associated with various intra-operative and postoperative complications [3, 9–11, 22, 27, 42, 56]. In their review of the literature, Vaccaro et al. [42] reported an incidence of screw and plate loosening reaching 15.4 %, screw and plate breakage rates, respectively, up to 13.3 and 6.7 %, a plate and graft displacement (with or without graft fracture) rate scaling up to 21.4 % and an incidence of implant malposition (screws in discs, plating of unfused segments, etc.) from 0 to 12.5 % for long-segment plates. Many newer implants are designed with different screw-locking mechanisms to avoid these mechanical complications. It should be noted that balancing between preferably small plate dimensions (low profile) and the necessity of thicker plates to have a secure constrained screw fixation is challenging from an engineering standpoint. Nevertheless, the problem of screw and plate malposition during surgery still exists. Specifically, the lack of implant migration or screw loosening might be related to the design of the locking plate–screw interface. In this study, regardless of the number of operated levels, we did not encounter these implant-related complications in cage group during follow-up.
This study is limited by the relatively small number of patients. In addition, the mean follow-up period was too short to evaluate the long-term efficacy of the new zero-profile, stand-alone Fidji cervical cage for the treatment of cervical DDD. However, we feel that this study provides useful information regarding the surgical treatment of cervical DDD, because there are currently a few reports describing outcomes after Fidji cervical cage for ACDF. Further large-scale, prospective, randomized studies with long-term follow-up periods are needed to overcome these limitations and definitively determine whether the new zero-profile, stand-alone Fidji cervical cage has advantages over the stand-alone cages with a titanium plate for ACDF.
Conclusions
In summary, the clinical and radiological outcome of the new zero-profile, stand-alone Fidji cervical cage for the surgical treatment of single- and multilevel degenerative cervical disc disease was satisfactory after a minimum 2-year follow-up. The results do not show significant differences between the zero-profile, stand-alone Fidji cervical cage and the stand-alone cages with a titanium plate in terms of improvement in the SF-36, VAS, NDI, JOA scores, DHI, mean fusion time, fusion rate, ASD, and restoration of cervical lordosis, but Fidji cervical cage was associated with a lower risk of postoperative dysphagia, shorter operation time, less blood loss, less cost of index surgery, and relatively greater simplicity than the stand-alone cages with a titanium plate for ACDF. Overall, the results show that the zero-profile, stand-alone Fidji cervical cage for ACDF is an effective, reliable, and safe alternate to the conventional method for the treatment of cervical DDD. However, there is no definitive evidence that the zero-profile, stand-alone Fidji cervical cage has better intermediate-term outcomes than the stand-alone cages with a titanium plate for ACDF.
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Jt Surg Am 40-A:607–624
Yue WM, Brodner W, Highland TR (2005) Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 30:2138–2144
Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J (2004) Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 17:79–85
Park HW, Lee JK, Moon SJ, Seo SK, Lee JH, Kim SH (2009) The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976) 34:E591–E595. doi:10.1097/BRS.0b013e3181ab8b9a
Li Z, Huang J, Zhang Z, Li F, Hou T, Hou S (2014) A comparison of multilevel anterior cervical discectomy and corpectomy in patients with 4-level cervical spondylotic myelopathy: a minimum 2-year follow-up study. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000212
Bohler J, Gaudernak T (1980) Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma 20:203–205
Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50:229–236 (discussion 236–228)
Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976) 34:2886–2892. doi:10.1097/BRS.0b013e3181b64f2c
Fujibayashi S, Shikata J, Kamiya N, Tanaka C (2000) Missing anterior cervical plate and screws: a case report. Spine (Phila Pa 1976) 25:2258–2261
Lowery GL, McDonough RF (1998) The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine (Phila Pa 1976) 23:181–186 (discussion 186–187)
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS Jr (2007) Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 32:2310–2317. doi:10.1097/BRS.0b013e318154c57e
Jung A, Schramm J (2010) How to reduce recurrent laryngeal nerve palsy in anterior cervical spine surgery: a prospective observational study. Neurosurgery 67:10–15. doi:10.1227/01.NEU.0000370203.26164.24 (discussion 15)
Jung A, Schramm J, Lehnerdt K, Herberhold C (2005) Recurrent laryngeal nerve palsy during anterior cervical spine surgery: a prospective study. J Neurosurg Spine 2:123–127. doi:10.3171/spi.2005.2.2.0123
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 27:2453–2458. doi:10.1097/01.BRS.0000031407.52778.4B
Smith-Hammond CA, New KC, Pietrobon R, Curtis DJ, Scharver CH, Turner DA (2004) Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine (Phila Pa 1976) 29:1441–1446
Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD, Le Roux PD (2002) Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech 15:362–368
Min Y, Kim WS, Kang SS, Choi JM, Yeom JS, Paik NJ (2013) Incidence of dysphagia and serial videofluoroscopic swallow study findings after anterior cervical discectomy and fusion: a prospective study. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000060
Fengbin Y, Xinwei W, Haisong Y, Yu C, Xiaowei L, Deyu C (2013) Dysphagia after anterior cervical discectomy and fusion: a prospective study comparing two anterior surgical approaches. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:1147–1151. doi:10.1007/s00586-012-2620-5
Jeyamohan SB, Kenning TJ, Petronis KA, Feustel PJ, Drazin D, DiRisio DJ (2015) Effect of steroid use in anterior cervical discectomy and fusion: a randomized controlled trial. J Neurosurg Spine 23:137–143. doi:10.3171/2014.12.SPINE14477
Olsson EC, Jobson M, Lim MR (2015) Risk factors for persistent dysphagia after anterior cervical spine surgery. Orthopedics 38:e319–e323. doi:10.3928/01477447-20150402-61
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18:406–409
Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E (2009) Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg 111:18–27. doi:10.1016/j.clineuro.2008.07.009
Wang Z, Jiang W, Li X, Wang H, Shi J, Chen J, Meng B, Yang H (2015) The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 24:148–154. doi:10.1007/s00586-014-3628-9
Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976) 30:2564–2569
Yue WM, Brodner W, Highland TR (2005) Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 14:677–682. doi:10.1007/s00586-004-0849-3
Cagli S, Isik HS, Zileli M (2009) Cervical screw missing secondary to delayed esophageal fistula: case report. Turk Neurosurg 19:437–440
Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI (2009) Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine (Phila Pa 1976) 34:641–646. doi:10.1097/BRS.0b013e318198ce10
Park JB, Cho YS, Riew KD (2005) Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Jt Surg Am 87:558–563. doi:10.2106/JBJS.C.01555
Yang JY, Song HS, Lee M, Bohlman HH, Riew KD (2009) Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine (Phila Pa 1976) 34:30–33. doi:10.1097/BRS.0b013e318190d833
Shao H, Chen J, Ru B, Yan F, Zhang J, Xu S, Huang Y (2015) Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res 10:148. doi:10.1186/s13018-015-0290-9
Li Z, Yu S, Zhao Y, Hou S, Fu Q, Li F, Hou T, Zhong H (2014) Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci Off J Neurosurg Soc Australas 21:942–948. doi:10.1016/j.jocn.2013.09.007
Hofstetter CP, Kesavabhotla K, Boockvar JA (2015) Zero-profile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating. J Spinal Disord Tech 28:E284–E290. doi:10.1097/BSD.0b013e31828873ed
Scholz M, Schleicher P, Pabst S, Kandziora F (2015) A zero-profile anchored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine (Phila Pa 1976) 40:E375–E380. doi:10.1097/BRS.0000000000000768
Huang SL, Yan HW, Wang KZ (2013) Use of Fidji cervical cage in the treatment of cervical spinal cord injury without radiographic abnormality. BioMed Res Int 2013:810172. doi:10.1155/2013/810172
King JT Jr, Roberts MS (2002) Validity and reliability of the Short Form-36 in cervical spondylotic myelopathy. J Neurosurg 97:180–185
Vernon H, Mior S (1991) The Neck Disability Index: a study of reliability and validity. J Manip Physiol Ther 14:409–415
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K (2001) Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 26:1890–1894 (discussion 1895)
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 12:513–516. doi:10.1007/s00586-003-0539-6
Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC (2008) Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 21:288–292. doi:10.1097/BSD.0b013e31813c0e59
Song KJ, Choi BW, Jeon TS, Lee KB, Chang H (2011) Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 20:1940–1945. doi:10.1007/s00586-011-1864-9
Thorell W, Cooper J, Hellbusch L, Leibrock L (1998) The long-term clinical outcome of patients undergoing anterior cervical discectomy with and without intervertebral bone graft placement. Neurosurgery 43:268–273 (discussion 273–264)
Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11:410–415
Murphy MA, Trimble MB, Piedmonte MR, Kalfas IH (1994) Changes in the cervical foraminal area after anterior discectomy with and without a graft. Neurosurgery 34:93–96
Fraser JF, Hartl R (2007) Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine 6:298–303. doi:10.3171/spi.2007.6.4.2
Yang Y, Ma L, Liu H, Xu M (2016) A meta-analysis of the incidence of patient-reported dysphagia after anterior cervical decompression and fusion with the zero-profile implant system. Dysphagia 31:134–145. doi:10.1007/s00455-015-9681-7
Barbagallo GM, Romano D, Certo F, Milone P, Albanese V (2013) Zero-P: a new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(Suppl 6):S868–S878. doi:10.1007/s00586-013-3005-0
Tortolani PJ, Cunningham BW, Vigna F, Hu N, Zorn CM, McAfee PC (2006) A comparison of retraction pressure during anterior cervical plate surgery and cervical disc replacement: a cadaveric study. J Spinal Disord Tech 19:312–317. doi:10.1097/01.bsd.0000210117.01897.ca
Mobbs RJ, Rao P, Chandran NK (2007) Anterior cervical discectomy and fusion: analysis of surgical outcome with and without plating. J Clin Neurosci Off J Neurosurg Soc Australas 14:639–642. doi:10.1016/j.jocn.2006.04.003
Xia XP, Chen HL, Cheng HB (2013) Prevalence of adjacent segment degeneration after spine surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 38:597–608. doi:10.1097/BRS.0b013e318273a2ea
Litrico S, Lonjon N, Riouallon G, Cogniet A, Launay O, Beaurain J, Blamoutier A, Pascal-Mousselard H, French Society of Spine S (2014) Adjacent segment disease after anterior cervical interbody fusion: a multicenter retrospective study of 288 patients with long-term follow-up. Orthop Traumatol Surg Res OTSR 100:S305–S309. doi:10.1016/j.otsr.2014.07.004
Chung JY, Kim SK, Jung ST, Lee KB (2014) Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J Off J N Am Spine Soc 14:2290–2298. doi:10.1016/j.spinee.2014.01.027
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J Off J N Am Spine Soc 4:190S–194S. doi:10.1016/j.spinee.2004.07.007
Hussain M, Natarajan RN, Fayyazi AH, Braaksma BR, Andersson GB, An HS (2009) Screw angulation affects bone-screw stresses and bone graft load sharing in anterior cervical corpectomy fusion with a rigid screw-plate construct: a finite element model study. Spine J Off J N Am Spine Soc 9:1016–1023. doi:10.1016/j.spinee.2009.08.461
Miao J, Shen Y, Kuang Y, Yang L, Wang X, Chen Y, Chen D (2013) Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech 26:E193–E197. doi:10.1097/BSD.0b013e31827a2812
Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC (2002) Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 51:1343–1349 (discussion 1349–1350)
Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL (2000) A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine (Phila Pa 1976) 25:2646–2654 (discussion 2655)
Fujibayashi S, Neo M, Nakamura T (2008) Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci Off J Neurosurg Soc Australas 15:1017–1022. doi:10.1016/j.jocn.2007.05.011
Wu WJ, Jiang LS, Liang Y, Dai LY (2012) Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 21:1374–1382. doi:10.1007/s00586-011-2131-9
Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, Marciano FF, Crawford NR (2009) A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976) 34:156–160. doi:10.1097/BRS.0b013e31818ff9c4
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4:447–453. doi:10.3171/spi.2006.4.6.447
Li Z, Guo Z, Hou S, Zhao Y, Zhong H, Yu S, Hou T (2014) Segmental anterior cervical corpectomy and fusion with preservation of middle vertebrae in the surgical management of 4-level cervical spondylotic myelopathy. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23:1472–1479. doi:10.1007/s00586-014-3208-z
Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, Mason A, Burneikiene S (2011) Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 68:1309–1316. doi:10.1227/NEU.0b013e31820b51f3 (discussion 1316)
Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ (2004) Anterior correction of cervical kyphotic deformity: effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg 100:13–19
Harrison DD, Harrison DE, Janik TJ, Cailliet R, Ferrantelli JR, Haas JW, Holland B (2004) Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine (Phila Pa 1976) 29:2485–2492
Acknowledgments
Kindly thanks for the support of a Special Financial Grant from China Postdoctoral Science Foundation 2015T81101.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors state that there is no actual or potential of conflicts of interest in relation to this article. All authors declare that there are no any financial and personal relationships with other people or organisations that could inappropriately influence (bias) our work.
Funding
Kindly thanks for the support of the Special Financial Grant from China Postdoctoral Science Foundation 2015T81101. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional information
Z. Li, Y. Zhao and J. Tang contributed equally to the manuscript and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Li, Z., Zhao, Y., Tang, J. et al. A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J 26, 1129–1139 (2017). https://doi.org/10.1007/s00586-016-4739-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4739-2