Abstract
Purpose
The purpose of the study was to explore the impact of Modic-2 changes on the clinical outcomes of single-level anterior cervical discectomy and fusion.
Methods
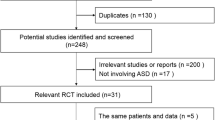
This study retrospectively reviewed the medical records of 35 ACDF patients with Modic-2 changes at adjacent level (Group A) and 213 patients without Modic-2 changes at adjacent level (Group B). Clinical and radiographic evaluations were performed preoperatively and repeated at 3, 6, 12, and 60 months after surgery.
Result
All patients were followed up for an average of 60 months. The clinical improvements in terms of NDI and JOA scores were achieved in both groups (P < 0.05), and no significant differences were found between the two groups (P > 0.05). The radiologic review demonstrated ASD was proven in 9 patients in Group A and 52 patients in Group B. A significant increase in ROM at the adjacent segments after surgery was observed in both groups (P < 0.05). No significant differences in adjacent segment ROM and DH were observed between two groups (P > 0.05). Comparing the outcome VAS of axial symptoms with Group A after surgery, patients in the Group B reported significantly lower VAS of axial symptoms at 1-year follow-up (P < 0.05). There were no significant differences between the two groups at the final follow-up (P > 0.05).
Conclusion
Modic-2 changes at adjacent level at baseline does not affect fusion rate or clinical outcome based on functional status but could negatively impact axial symptoms intensity and ASD, compared to patients without Modic-2 changes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) has been the gold standard of treatment for degenerative cervical spine disease, which may require a surgical fusion procedure if not improved by proper conservative treatment [1–3]. There were many studies that had reported good clinical and radiologic outcomes for ACDF, although it is associated with significant drawbacks such as postoperative dysphagia, hematoma, nonunion, axial symptoms, and adjacent-segment degeneration (ASD) [4–6].
In particular, ASD might lead to various pathologies ranging from degenerative changes in the adjacent segments (radiologic ASD) to recurrent or new onset symptoms in the low back and lower extremities (clinical ASD), which may require additional nonsurgical or surgical intervention. Axial symptoms were also an important issue which might be related to disk degeneration in adjacent segments or malalignment of the cervical spine [6, 7].
In 1988, Modic et al. proposed three types of degenerative changes affecting the vertebral endplate on magnetic resonance imaging (MRI): Type 1 changes demonstrated hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging; Type 2 changes have hyperintense signals on both T1- and T2-weighted MR images; and Type 3 changes demonstrated hypointense signals on both T1- and T2-weighted MR images. Type 1 changes demonstrated an inflammatory phase of the degenerative process; Type 2 changes represent fatty involution of the subchondral bone and marrow; and Type 3 changes demonstrated cicatrization phase of disk degeneration [8].
Several studies had reported Modic type 2 changes were the most common type. The most common level was the C5–C6, which was the most flexible level according to the Modic changes. Therefore, hyperactivity may be the main reason for cervical Modic changes [9–11]. In addition, it has been reported better clinical results were achieved in patients with Modic type 1 changes compared to the group of patients with Modic type 2 changes recently [12]. Based on this information, we hypothesized that Modic type 2 changes might impact on the clinical outcome or ASD after ACDF. The purpose of the study was to explore the impact of Modic-2 changes on the clinical outcomes of single-level ACDF.
Methods
This study was approved by the Institutional Review Board of No.3 hospital of Hebei medical university. All of the patients were informed that they were going to be in this study; those who did not wish to participate in this study were not enrolled.
This study was conducted using patients who met all of the following inclusion criteria: patients who suffered from symptoms of radiculopathy and/or myelopathy diagnosed on radiographs, CT, and MRI and that corresponded to clinical manifestations and physical examinations findings; (2) previous single-level ACDF; age between 40 and 65 years and a follow-up period of 5 years or more. We excluded patients who met any of the following criteria: fracture, deformity, infection, tumor of the cervical spine; medical history of fusion procedure at any level; or follow-up period less than 5 years.
Surgical technique
All operations were performed using the same surgical technique. The surgical approach for the ACDF was through the Smith-Robinson approach. After the exposure, the diseased disk was excised, along with the posterior longitudinal ligament followed by decompression of the spinal cord and nerve roots. The endplates were prepared with a high-speed burr, and then the appropriately sized tricortical iliac crest graft or polyetheretherketone (PEEK) cage (Medtronic Sofamor Danek, Memphis, TN, USA) filled with bone was placed in the interspace. Then the anterior plate system was applied (Medtronic Sofamor Danek, Memphis, TN, USA).
Diagnostic criteria for Modic-2
Modic-2 changes have hyperintense signal on both T1- and T2-weighted MR images (Fig. 1). One reviewer had assessed the MR images twice for evaluation of intraobserver reliability. The other reviewer assessed the MR images once.
Evaluation criteria
We compared the preoperative value before and after surgery and at 3, 6, 12, and 60 months postoperatively. Radiographic evaluation included static and dynamic flexion/extension lateral images which was used to assess fusion and ASD by two independent doctors who evaluated the radiographs without knowledge of the clinical outcomes. ASD was defined as following: calcification of the anterior longitudinal ligament; a narrowing of the disk space with or without posterior osteophytes; new anterior or enlarging osteophyte formation. Disk height (DH) was defined as an average value of the anterior DH and the posterior DH. The range of movement (ROM) of the operated and adjacent levels was defined by shell angle (Fig. 2).
Clinical outcome was evaluated using a visual analog scale (VAS) to determine axial symptoms and the Neck Disability Index (NDI), and values were obtained before each treatment and again at 1 month, 3 months, 6 months, 1 year, and 5 years after surgery. The modified Japanese Orthopedic Association (JOA) scoring system was used to determine functional status before surgery and at the final follow-up visit. The recovery rate (%) at the final follow-up visit was calculated by using the Hirabayashi method: (postoperative JOA score-preoperative score)/(17-preoperative score) × 100 %.Normal score of JOA present 17.
Statistical analysis
Statistical analysis was performed using SPSS software (Version 17.0, Chicago, IL, USA) and two-tailed P values <0.05 were considered statistically significant. The independent Student’s t test, paired t test, and the Fisher’s exact test were used for variables such as demographic data, VAS, NDI, JOA, and ASD. Results were presented as mean ± standard deviation.
Result
We retrospectively reviewed the medical records of 35 ACDF patients with Modic-2 changes at adjacent level (Group A) and 213 patients without Modic-2 changes at adjacent level (Group B) that met the inclusion criteria for this study. The groups were comparable with regard to demographics, and there were no statistically significant differences between the two groups (Table 1). No vertebral artery injury and implant subsidence were found in this study. Modic-2 changes were most frequently found at C6/7, where they were observed in 12 cases (34.3 %). The second-most common level to show MC was C5/6 with 10 cases (28.6 %).The interobserver agreement of Modic-2 changes at adjacent level was substantial with a value of 0.79. The intraobserver agreement of Modic-2 changes at adjacent level was also substantial with a value of 0.72. Dysphagia was present in three patients postoperatively.
ROM at the adjacent levels increased from 8.8 ± 2.1 to for 9.6 ± 2.3 for the Group A and from 9.2 ± 1.8 to 10.8 ± 1.6 for the Group B (P < 0.05). No significant differences were found between the two groups(P > 0.05). The mean preoperative and final DH were 4.7 ± 1.3 mm and 4.6 ± 1.6 mm in Group A. The mean preoperative DH was 5.3 ± 1.5 mm. The final DH was 5.1 ± 1.3 mm. There was no difference in ROM and DH changes at the adjacent levels between the two groups (P > 0.05). The radiologic review demonstrated ASD was proven in nine patients, and three were diagnosed with symptomatic ASD in Group A. In Group B, ASD was proven in 52 patients, and three were diagnosed with symptomatic ASD.
For both the groups, the patients had significant functional activity improvement and pain relief after surgery. Substantial improvement in JOA and NDI occurred in both groups compared with the preoperative values, and there were no significant differences between the two groups. At the last follow-up, the mean recovery rates were 61.1 and 64.7 %, respectively (P > 0.05).
The preoperative VAS of axial symptoms was 7.5 ± 2.1 and 7.3 ± 1.9, respectively. There were no significant differences in axial symptoms between the two groups before surgery. At 1-year follow-up, the VAS of axial symptoms significantly decreased to 2.8 ± 1.6 and 2.1 ± 1.2 respectively, representing a statistically significant difference (P < 0.05). Comparing the outcome VAS of axial symptoms with Group A after ACDF, patients in the Group B reported significantly lower VAS of axial symptoms (P < 0.05). There were no significant differences between the two groups at the final follow-up (Table 2).
Discussion
Degenerative cervical spine disease is a common disease and can be managed conservatively in many cases. However, despite proper conservative management, some patients eventually require surgical management with ACDF. Although ACDF has been widely performed with favorable clinical and radiologic outcomes, some drawbacks of this approach have also been noted including persistent axial symptoms and ASD. Furthermore, some patients might have to undergo additional surgery at the adjacent level.
Previous studies of Modic changes have focused on lumbar spine, which suggested strong relationship with pain and disk degeneration. However, in contrast to the lumbar spine, few studies have reported the Modic changes in the cervical spine which was highly mobile and prone to degeneration and pain. Repetitive loading or recurrent disk injury led to minor injury of the endplate [9–11]. Modic changes in the cervical spine was a dynamic phenomenon similar to the lumbar spine, which was known to be related to axial symptoms and accelerated disk degeneration of the cervical segments. It has been reported there was a significantly higher prevalence of Modic changes in patients with axial symptoms. Mann et al. demonstrated that patients with MC are more likely to have a disk herniation at the same level [9]. Hayashi et al. also reported Modic changes were observed in 84 (19.2 %) in 437 patients. Diskdegeneration grades and spinal cord compression grades of segments were significantly higher than those without Modic changes [13].
In this study, we retrospectively analyzed the medical records of 213 patients with single-level ACDF who were followed for at least 5 years postoperatively according to the presence or absence of Modic-2 changes. There were no differences in preoperative JOA, NDI, and VAS scores on axial symptoms between the two groups, which were significantly improved compared to the preoperative scores in both groups. However, the Group B showed significant differences in VAS for axial symptoms compared to that of the group A at the 1-year follow-up. No differences were found between thetwo groups at the last follow-up. The Modic changes in the spine are dynamic, which suggested that they were inreversible. It has concerning the usefulness of these MRI changes as an indicator of clinical symptoms or surgical outcomes. Thus the natural history of MC might explain the change of the axial symptoms after 1-year follow-up.
Increasing cervical segment motion is known to be related to axial symptoms and accelerated disk degeneration of the cervical segments. In addition, several authors have reported that excessive motion of the cervical spine negatively impacts outcomes for surgical treatment of cervical spine pathologies such as ACDF. Biomechanical studies also suggested that the arthrodesis influenced mechanical properties of intervertebral disks in the adjacent segments [14, 15]. In a recently study, it had reported patients with Modic-2 changes were more likely to have spinal canal stenosis and disk degeneration at the level compared to patients without Modic changes [13].
This study retrospectively analyzed the medical records of 256 patients with single-level ACDF who were followed for at least 5 years postoperatively according to the presence or the absence of Modic-2. No patient needed additional surgery for recurrent symptoms.
In group A, ASD was radiographically proven in 28 (24.1 %) patients, and three were diagnosed with symptomatic ASD. No statistically significant differences were found between the two groups.
According to the radiologic measurements, postoperatively, no significant increase in adjacent segment motion in the Group A occurred compared with the minimal ROM changes in adjacent-level motion observed in the group B. No significant decrease in adjacent segment motion in the Group A occurred compared with the minimal DH changes in adjacent level observed in the group B. These findings indicated that adjacent segments with Modic-2 changes did not increase the incidence of disk degeneration at these levels.
Limitation
The changes of ASD were only shown by plain radiographic images, which was cost-effectiveness and simplicity as a follow-up method. It still provided limited information compared with CT or MRI. Whether the ACDF would accelerate the Modic changes at the adjacent level was unknown. The prospective and large-scale studies should be performed to define the relationship between Modic-2 changes and ACDF outcome. In the future study, we can explore the correlation between different types of Modic changes and curvature on cervical spine.
Conclusion
Based on our data, it is found that Modic-2 changes at adjacent level at baseline do not affect fusion rate or clinical outcome based on functional status but could negatively impact the axial symptoms intensity and ASD compared to patients without Modic-2 changes.
References
Cho SK, Riew KD (2013) Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg 21(1):3–11
Njoku I Jr, Alimi M, Leng LZ et al (2014) Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: Clinical article. J Neurosurg Spine 21(4):529–537
Matz PG, Holly LT, Mummaneni PV et al (2009) Anterior cervical surgery for the treatment of cervical degenerative myelopathy. J Neurosurg Spine 11(2):170–173
Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al (2007) Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 32(21):2310–2317
Li GL, Hu JZ, Lu HB et al (2015) Anterior cervical discectomy with arthroplasty versus anterior cervical discectomy and fusion for cervical spondylosis. J Clin Neurosci 22(3):460–467
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S–194S
Hilibrand AS, Carlson GD, Palumbo MA et al (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Modic MT, Steinberg PM, Ross JS et al (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199
Mann E, Peterson CK, Hodler J (2011) Degenerative marrow (modic) changes on cervical spine magnetic resonance imaging scans: prevalence, inter- and intra-examiner reliability and link to disc herniation. Spine 36:1081–1085
Matsumoto M, Okada E, Ichihara D et al (2012) Modic changes in the cervical spine: prospective 10-year follow-up study in asymptomatic subjects. J Bone Joint Surg Br 94(5):678–683
Sheng-Yun L, Letu S, Jian C, et al (2014) Comparison of Modic Changes in the Lumbar and Cervical Spine, in 3167 Patients with and without spinal pain. PLoS One 9(12):e114993
Li J, Li Y, Wei J, et al (2015)A study on the cervical spondylotic myelopathy treated by anterior cervical diskectomy and fusion in accordance with Modic changes with a 2-year minimum follow-up. J Orthop Surg Res 10(1):11 [Epub ahead of print]
Hayashi T, Daubs MD, Suzuki A et al (2014) Effect of Modic changes on spinal canal stenosis and segmental motion in cervical spine. Eur Spine J 23(8):1737–1742
Dang AB, Hu SS, Tay BK. (2008) Biomechanics of the anterior longitudinal ligament during 8 g whiplash simulation following single- and contiguous two-level fusion: A finite element study. Spine (Phila Pa 1976) 33(6):607–611
Bydon M, Xu R, Macki M et al (2014) Adjacent segment disease after anterior cervical discectomy and fusion in a large series. Neurosurgery 74(2):139–146
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have read and contributed to the submitted manuscript and there is no conflict of interest among the authors.
Ethical Board Review statement
This material has not been published and is not under consideration elsewhere. This study receives no financial support. The Impact of Modic-2 changes on the clinical outcomes of single-level anterior cervical discectomy and fusion.
Rights and permissions
About this article
Cite this article
Li, J., Lei, T. & Shen, Y. The Impact of Modic-2 changes on the clinical outcomes of single-level anterior cervical discectomy and fusion. Eur Spine J 24, 2936–2940 (2015). https://doi.org/10.1007/s00586-015-4161-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4161-1