Abstract
In ventral fusion after anterior cervical discectomy there is still a remarkable number of cage subsidence and segmental kyphosis seen. The aim of the present study is to assess whether the cage design influences the extent of correction loss during follow-up. Sixty patients with single-level cervical disc herniation were randomly treated with two different cervical inter-body cages (group1: Solis™ cage, Stryker Company and group2: Shell™ cage, AMT Company). Clinical and radiological follow-up was done before and after surgery, 3 and 6 months post-surgery. Clinical follow-up was done with the help of Odom’s criteria. Both groups were similar in the baseline parameters (age, sex, treated level). Statistically, the subsidence was significantly higher at 3 and 6-month follow-ups in group1 than in group2, however, clinical results showed no significant differences. In 67%, subsidence was seen in the anterior lower aspect of the treated segment. Segmental kyphosis was seen in seven patients of group1 and two patients of group2. A significant correlation is found between Odom’s criteria and subsidence. Although there was no significant difference in a short-term clinical result between the two treatment groups, we recommend the use of cages which preserve the determined segmental height and lordosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy is an effective procedure to treat compressive single-level radiculopathy. What to do once the decompression has been completed is yet unclear, and this uncertainty has existed since the anterior approach was popularized about 50 years ago [4, 22].
Performing anterior cervical discectomy (ACD) without fusion contends the risk that the empty disc space will collapse, often causing kyphosis. Loss of disc height associated with increased kyphosis can lead to a loss of neural foramen height and increased pain in the neck and scapular regions [2, 20].
Furthermore, studies show that increased segmental kyphosis promotes degeneration in adjacent segments [9].
As a consequence, anterior cervical discectomy and fusion (ACDF) is a common technique for treatment of cervical radiculopathy since many decades. For a long time, the traditional methods of Cloward and Robinson were the gold standard for ACDF [4, 6, and 26]. But this procedure has some disadvantages.
Autologous bone graft obtained from the anterior iliac crest is associated with significant donor-site morbidity [5, 8, 20, 21, and 26]. Also, there is a remarkable number of subsidence [1, 11, 17, 20, 26].
More recently, this operation has undergone changes involving synthetic inter-body cages and materials such as stainless steel, titanium, carbon fiber, poylmethyl-methacrylate (PMMA), and polyetheretherketone (PEEK). Cages were introduced because of their theoretical ability of restoration and preservation of disc height and lordosis and to prevent graft collapse.
Currently, in practice, there are a number of different inter-body cages for anterior cervical discectomy and fusion (ACDF). These implants differ in terms of material and shape. However, there is still a remarkable number of cage subsidence and segmental kyphosis while using these sophisticated implants [3, 7, 10, 13, 14, 17, 19, 20, 24–26].
The primary purpose of the present study is to evaluate, in a prospective randomized manner, whether the cage design influences the extent of correction loss during follow-up.
Secondary aims of the study are to evaluate the clinical course of both treatment groups and to correlate the radiological findings with the clinical follow-up.
Methods
Patients (inclusion and exclusion criteria)
For this study, only patients with a planned single-level discectomy and fusion (ACDF) for radiculopathy or cervical myelopathy were enrolled. The ethical committee of the hospital approved the study.
Patients with previous cervical disc surgery, metabolic bone disease, or systemic infection were excluded. Treatment of the segment C7-T1 was excluded because radiological follow-up with X-rays usually is not sufficient in this region.
After informed consent was obtained, 60 patients were enrolled for randomization. The method of randomization was based on a strictly alternating use of the two cage systems. This was not influenced by the indication for surgery or by the surgeon for itself. Using this method, the distribution of the three acting neurosurgeons is homogeneous in both treatment groups and is therefore no source of bias.
Fifty-two of 60 patients qualified against all criteria for evaluation. The reason for drop-out was lost to follow-up in six cases and refusal of participation in two cases.
Of the 52 qualified patients, 29 were male and 23 female. The mean age was 50.2 years at time of surgery. Indication for surgery was compressive single-level radiculopathy in 46 cases and one level myelopathy in six cases.
Treated levels were C3–C4 in four, C4–C5 in three, C5–C6 in 20 and C6–C7 in 25 patients.
Surgical technique
Cervical spine was exposed by a standard antero-lateral approach and this followed by microsurgical anterior cervical discectomy. Cartilage was removed from the vertebral endplates using curettes. The posterior longitudinal ligament was opened and dural sac and nerve root were decompressed using a high-speed drill. Then, the optimum cage size was determined with help of lateral fluoroscopy. The aim was, here, to restore disc height and cervical lordosis. All cages were implanted empty. In all cases of predominant cervical myelopathy an additional instrumentation with a cervical titanium plate was performed (Osmium™ plate, Ulrich Co., Ulm, Germany, Fig. 1a). This was performed in three patients of group1 and three patients of group2.
Post-operatively, no patient received a collar.
Cage systems
There were two different cage systems used: in group1, the Solis™ cage (Stryker Company, Kalamazoo, USA) was used and in group2, the Shell™ cage, (AMT Company, Nonnweiler, Germany). Both cages are made of polyetheretherketone (PEEK), a benzene ring polymer, which is radiolucent.
The Solis cage is ring-shaped with a thickness of about 2 mm. There are different implant heights available ranging from 4 to 8 mm in steps of 1 mm. Furthermore, there are two different implant diameters: 12 and 14 mm. For preventing dislocation, the implant has bilaterally 1-mm titanium spikes. These spikes are also markers to aid in identification of position on plain X-rays or fluoroscopy. The upper and lower aspect of the implant is covered with small teeth. The contact surface area of the 12-mm implant is 60 mm2 and of the 14 mm implant is 80 mm2 (Fig. 1b).
The Shell cage is a trapezoid-shaped box with a thickness varying from 1 to 4 mm. At the lateral and anterior aspect, the wall is increased to 3 mm, the anterior lower aspect to 4 mm thickness. This feature is planned to prevent subsidence in the anterior implant area.
The lateral wall of the implant is oblique shaped, fitting to the uncinate process of the lower vertebra.
The implant is available in four different steps of width, ranging from 14 mm to 20 mm. So, if the correct implant size is selected, the implant should have contact bilaterally to the uncinate processes. The implant height is varying from 4 to 7 mm in steps of 1 mm. To prevent dislocation, the upper and lower surface is covered with teeth. At each corner of the cage, there is a titanium spike on the one hand, also to prevent dislocation and on the other hand, as a marker for implant identification by fluoroscopy or plain X-rays (Fig. 1c).
In contrast to the Solis cage the Shell cage has different footprints between lower and upper surface. Therefore, for calculating the contact surface area, the average of the lower and upper surface is used. The Shell cage with a width of 14 mm has a contact surface area of 109 mm2, the 16-mm implant, 119 mm2, the 18-mm implant, 129 mm2, and the 20-mm implant, 139 mm2.
Radiological outcome measures
Radiological and clinical follow-up was done before surgery. Post-surgical follow-ups were performed on 3 and 6 months. All patients underwent pre-surgical MRI scans of the cervical spine. At follow-ups, radiological assessment involved plain X-ray in AP (anterior–posterior) and lateral projections, centered to the operated segment. If there were abnormalities discovered, additional lateral flexion–extension radiographs were done. An independent interpreter assessed the radiographs in order to eliminate bias. Analysis of the radiographs included measurements of the segmental height ratio, the absolute segmental height, the inter-body angle, and the grading of fusion.
The inter-body height ratio is measured as the total vertical height of the two vertebral bodies which form the movement segment, divided by the anterior–posterior (AP) diameter of the upper vertebral body on a lateral radiograph (Fig. 2b). This eliminates the magnification variation in the measurements taken from radiographs. With help of the pre-operative MRI scan, it is possible to measure the absolute AP diameter of the upper vertebral body (Fig. 2a). Using this value, in all radiographs, the absolute segmental height can be calculated.
The tendency of subsidence is recorded in a semi-quantitative way. Results are scored in three levels: no obvious subsidence, minor subsidence, and major subsidence. Minor subsidence was defined as a state when the cage entered the endplate with a maximum of 2 mm, and major subsidence was defined as more than 2 mm. In cases with subsidence, the direction of subsidence is recorded.
The segmental angle is that between the lower endplate of the upper vertebral body and the upper endplate of the lower vertebral body, as measured on a lateral radiograph (Fig. 2c). Recorded is the course of the segmental angle. The results are categorized in three groups: no loss of segmental correction, minor kyphotic change (less then 2°), and major kyphotic deterioration (2° or more at last follow-up).
Correction loss is defined as a combination of the semi-quantitative parameters subsidence and segmental kyphosis. No subsidence means 0 point, major subsidence, 2 points, and no kyphosis, again, 0 point, and, finally, major kyphosis, 2 points. Correction loss is defined as the sum of points for both parameters, which means the sum has a range from 0 points for excellent radiological results and 4 points for worst results. The reason for creating on more radiological parameter is to combine the two partial independent variables subsidence and segmental kyphosis to one parameter.
The radiological assessment is done digitally using PACS Software system (Impax DS 3000, Agfa-Gevaert, Mortsel, Belgium).
The bone fusion is graded in four categories: Obvious fusion, when the trabeculae crossing the disc space or a bridging bone is seen around the implant, probable fusion, when there is an obvious densification in the cage, fusion in question, when there is only minor change of density in and around the cage, and no fusion, when all of these is absent.
Clinical outcome measures
Clinical follow-up was done with the help of Odom’s criteria with a grading from excellent to poor in four groups: Excellent (Odom I) was given for patients with no cervical spine symptoms and not impaired daily activities. Good (Odom II) means patients with intermittent discomfort, but with no significant interference with work. Fair (Odom III) was graded in cases with subjective improvement, but significant limitation of physical activities and finally poor (Odom IV) for patients with no improvement or worse compared with the condition before surgery [15, 23].
Statistical analysis
The Winstat Ver 3.10 statistical software package in combination with a Microsoft Access database was used for statistical analysis of the data. We applied exclusively non-parametric statistical tests such as chi-square, the Fisher exact, t, and Mann–Whitney U tests, if appropriate. A P value of 0.05 was assumed sufficient to indicate statistical significance. Non-parametric correlation analyses were performed using the Spearman-rho rank-ordered correlation coefficient and the Kendall-tau coefficient for exploring the statistical association of categorical variables.
Results
Baseline parameter
Both treatment groups were similar relating to sex and age. Also, the treated level and the relation between radiculopathy and myelopathy were well comparable.
In group 1 (Solis cage), ten patients received an implant with 5 mm height and 16 with an implant of 6 mm height. In group 2 (Shell cage), six patients received an implant with 4 mm, 14 with 5 mm height and six patients, an implant with 6 mm height. In group 1, four times an implant with a diameter of 12 mm and 20 times an implant with a diameter of 14 mm were used. In group 2, an implant with a width of 16 mm was used in five patients, with a width of 18 mm in 14 patients and an implant with a width of 20 mm was used in seven patients. In no case of group 2, an implant width of 14 mm was used.
Radiological results
The mean segmental height before treatment was 29.38 mm. After treatment, there was an obvious increase in segmental height in both treatment groups. At 3 months follow-up, the mean segmental height in the Solis group was lower than pre-surgery, but not in the Shell group. From 3 to 6 months follow-up, there is still a slight decrease of segmental height in both treatment groups (Table 1). If pre-surgical segmental height is standardized to 100%, then the succession of the segmental height during treatment and follow-ups in both treatment groups would be better compared (Fig. 3). After surgery, the Solis group showed a 4.5% increase in segmental height comparing to 3% in the Shell group. After 3 months, the Solis group had a 2.2% loss of height in contrast to the Shell group, who had still an increase of about 1.6%. This difference is statistically significant with a P value of 0.036. After another 3 months, both treatment groups had lost a further 0.6% of segmental height. So, the major height loss was seen from the post-operative control to 3 months follow-up with a loss of 6.8% in the Solis group and 1.4% in the Shell group.
Subsidence was recorded in 15 of 52 patients (29%). Subsidence occurred statistically significantly more in group1 (42%) than in group2 (15%) with a P value of 0.014 at last follow-up. Age and sex showed no influence to subsidence (Table 2). No subsidence occurred in the six patients treated additionally with a titanium plate.
Subsidence occurred at different locations of the adjacent vertebral bodies. A symmetrical slight subsidence was recorded in three patients of group1 and one patient of group2. Subsidence in the anterior upper aspect of the cage happened in one case of each group. Most frequent was subsidence in the anterior lower aspect of the implant: This happened in nine patients of the Solis group and in one of the Shell group (Fig. 4). Furthermore, subsidence in the posterior upper aspect was recorded in one patient of the Shell group. Sometimes, there were combinations, like subsidence in the anterior and posterior lower aspect. So, the sum of all is more than the recorded 15 cases of subsidence.
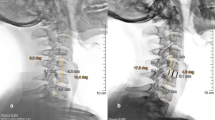
Worst case illustration. A 42-year-old woman with severe correction loss during follow-up and Odom grade III at last follow-up. a MRI scan before surgery in the sagittal plane. b Plain X-ray 3 months after surgery: Typical cage subsidence in the anterior lower aspect of the implant (major subsidence) and also major segmental kyphosis. c After another 3 months, segmental kyphosis is slightly progressive
Segmental kyphosis was recorded in 10 of 52 patients (19%). There was significantly more kyphosis in the Solis group with a P value of 0.032 at last follow-up. Age and sex showed no influence to segmental kyphosis. No segmental kyphosis occurred in the six patients treated additionally with a titanium plate (Table 2).
The bone fusion was graded in four categories, ranging from obvious fusion to no fusion. On their last follow-ups, 30% of the patients showed an obvious fusion, 46% a probable fusion, and 12% a fusion in question, and a further 12% with no bone fusion. There are no obvious differences in both treatment groups. Furthermore, there is no correlation neither between bone fusion and clinical course nor between bone fusion and correction loss.
No anterior or posterior cage dislocation was seen on follow-ups. There was no implant breakage or screw loosening recorded.
Clinical results
Clinical follow-up was done with help of Odom’s criteria with a grading in four steps from excellent (Odom I) to poor (Odom IV) [15]. On the last follow-ups, 94% of patients showed an excellent or good result of treatment. Six percent of patients had only a minimal improvement of signs and symptoms. There was no clinical deterioration recorded. Comparing both treatment groups, there was a tendency towards better clinical results in the Shell group without significance (Table 3). Age and sex showed no obvious influence on the clinical course.
A clear correlation is found between Odom’s criteria and subsidence with a P value of 0.039 (Spearman-rho rank-ordered correlation, Table 4). Increased segmental kyphosis showed a tendency toward worse clinical outcome without significance (P = 0.082). The above-defined parameter correction loss, a combination of subsidence and segmental kyphosis, is also correlating significantly with the clinical course at last follow-up (P = 0.042).
During inpatient stay, there was only one surgery-related complication recorded. One patient suffered of transient recurrent nerve palsy after surgery with a complete regression 6 months later. There was no case of wound infection and no neurological deterioration. No patient required a recurrent operation of the cervical spine during follow-up.
Discussion
Several techniques have been used for surgical treatment of cervical radiculopathy and myelopathy. The primary goal of all techniques is the decompression of the affected nerve root and restoration of cervical alignment. For long-lasting maintenance of cervical alignment, it is important to prevent subsidence and segmental kyphosis.
Methods and baseline parameter
The present study has a focus on the radiological course of ACDF. For precise measurement of segmental height, a ratio of the total vertical height of both fused vertebra to the AP diameter of the upper vertebrae was measured. Using an MRI scan, the absolute AP diameter was measured. By this way, absolute values without any influence by magnification can be calculated. To our knowledge, this analysis method is not yet published before.
Using the above-mentioned measuring method for segmental height, we were able to determine the course of segmental height during treatment and follow-up. The method is accurate enough to show plausible values by using median scores in patient groups of more than five patients. Looking at smaller numbers, this method is, according to our experience, not precise enough. The reason for this is, mainly, that in plain X-rays, segments sometimes are partly obliquely projected. This implies a remarkable error for this measurement method. For solving this problem, either a CT or MRI scan would be necessary or the use of conventional tomography would help. But, all of these solutions would cause an inadequate increase of effort and partly additional radiation exposure for the patient.
That is the reason why we added a second semi-quantitative measurement for segmental subsidence with a scaling in three levels. Here, the examiner looks mainly at the configuration of the endplates. Subsidence always implies an impression of the endplates and the depth of this impression gives hints for the extent of subsidence. To our experience, this method is often more precise than the absolute measurement method mentioned above.
More unproblematic is the measurement of segmental kyphosis. We think that a classification in three degrees is, here, precise enough.
Because of the limited budget we had for performing this study, we were not able to do expensive examinations like CT scan at follow-up for proving bone fusion. Therefore, our results concerning to this are of limited value.
It is very important for all these radiological measurements to do them by an independent examiner. Otherwise, the risk of bias is considerable.
For clinical follow-ups, Odom’s criteria were used. This scale is mainly developed for cervical radiculopathy. We used this scale also for our six patents with predominant myelopathy; on the one hand, because all cases showed only mild signs of myelopathy and on the other hand, to make evaluation easier and comparable.
The baseline parameters of both groups are very similar. Here, we found no hints for any bias.
Radiological results
After cage implanting, the segmental height increased in both treatment groups remarkably. The increase in the Solis group was more pronounced than in the Shell group. The reason, therefore, could be that the titanium pins of the Solis cage jut out more than the pins of the Shell cage. This could also partly explain why the Solis group showed a marked height loss up to the first follow-up. Another reason for frequent subsidence in the Solis group is probably not a large-enough contact surface area. This fact was also pointed out by Kemmesies and Meier in a retrospective comparison of five different intervertebral disc spacers for cervical spondylodesis [10]. Remarkable is the frequent subsidence of the Solis implant in the anterior lower aspect of the segment: This happened in nine patients of the Solis group and only in one patient of the Shell group. Here, it is very likely that the increased contact surface area of the Shell cage at the anterior lower aspect of the implant prevents this cage form subsidence at this site.
The tendency of the Solis implant to subside in the anterior lower aspect of the segment is probably the reason for the frequent segmental kyphosis in this treatment group.
Overall subsidence rate of 29% is well comparable to other series: Schmieder et al. [18] had a subsidence rate of 45% using a titanium cage.
In contrast are the results of an Italian study using also a Solis cage in 36 patients: the subsidence rate was, here, 0% after 18 months [13].
In our series, the fusion rate (obvious and probable fusion) was 76%. This is comparable to other series, like 61% fusion rate after 6 months in the study of Mastronardi et al. [13].
Clinical results
Our clinical results are altogether comparable to that of other authors [1, 7]. Comparing both treatment groups, there was a tendency towards better clinical results in the Shell group without statistical significance. In contrast to other investigations in our patients, age and gender showed no obvious influence on the clinical course [16].
Very interesting and a little bit surprising was the clear correlation between clinical results and subsidence. The parameter correction loss is also significant correlating with Odom’s criteria. A clear tendency without significance was seen in the change of absolute segmental height and the course of segmental kyphosis compared to clinical course. Reviewing literature to this question gives us different answers. There are hints for increased degeneration of adjacent segments, when segmental kyphosis occurred [9]. It is still under discussion whether there is a correlation between correction loss and clinical results or not.
A number of papers saw no obvious correlation concerning this question [6, 16, 18].
Some others saw correlations: Kwon et al. [11] followed-up 34 patients after ACDF using an allograft for fusion. Despite the relative small numbers of patients, they saw a correlation between neck pain, disc height, and kyphosis. Laing et al. [12] compared, in 55 patients, clinical results and segmental kyphosis following ACDF: there was a tendency to more neck pain and higher values in the Neck Disability Index without significance. Vavruch et al. [26] looked at 103 patients after ACDF using autograft or a carbon-fiber cage with a follow-up of 2 years. The authors found a significant correlation between segmental kyphosis and the Cervical Spine Functional Score.
Our results with a significant correlation of clinical and radiological results support the above-mentioned results strongly. Maybe there are further studies necessary, including more patients to confirm or contradict our results concerning this question.
Limitations of the study
We used a mean follow-up of 6 months. This is an obvious weakness of this study. So, the presented results can be interpreted as early results. We think that major radiological changes in the fused segment will occur during the included follow-up time. A longer follow-up would have meant much more effort and costs of the study.
Conclusions
In the current study, there was a significant difference in subsidence and segmental kyphosis between both treatment groups. Furthermore, there is a significant correlation between some radiological and clinical results. Although there was no significant difference in short-term clinical results between the two treatment groups, the aim should be to preserve the determined segmental height and lordosis. Therefore, we recommend using cages with a large-enough contact surface area, increased at the anterior lower aspect of the implant.
References
Barlocher CB, Barth A, Krauss JK, Binggeli R, Seiler RW (2002) Comparative evaluation of microdiscectomy only, autograft fusion, polymethylmethacrylate interposition, and threaded titanium cage fusion for treatment of single-level cervical disc disease: a prospective randomized study in 125 patients. Neurosurg Focus 12(1):E4
Bertalanffy H, Eggert HR (1988) Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir 90:127–135
Bruneau M, Nisolle JF, Gilliard C, Gustin T (2001) Anterior cervical interbody fusion with hydroxyapatite graft and plate system. Neurosurg Focus 10(4):E8
Cloward RB (1958) The anterior approach for removal of ruptured cervical discs. J Neurosurg 15:602–617
Frederic S, Benedict R, Payer M (2006) Implantation of an empty carbon fiber cage or a tricortical iliac crest autograft after cervical discectomy for single-level disc herniation: a prospective comparative study. J Neurosurg Spine 4:292–299
Haden N, Latimer M, Seeley HM, Laing RJ (2005) Loss of inter-vertebral disc height after anterior cervical discectomy. Br J Neurosurg 19:469–474
Hamburger C, Festenberg FV, Uhl E (2001) Ventral discectomy with PMMA interbody fusion for cervical disc disease: long-term results in 249 patients. Spine 26:249–255
Heary RF, Schlenk RP, Sacchieri TA, Barone D, Brotea C (2002) Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery 50:510–517
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324
Kemmesies D, Meier U (2005) Experience with five different intervertebral disc spacers for cervical spondylodesis. Zentralbl Neurochir 66:24–33
Kwon B, Kim DH, Marvin A, Jenis LG (2005) Outcomes following anterior cervical discectomy and fusion: the role of interbody disc height, angulation, and spinous process distance. J Spinal Disord Tech 18:304–308
Laing RJ, Ng I, Seeley HM, Hutchinson PJ (2001) Prospective study of clinical and radiological outcome after anterior cervical discectomy. Br J Neurosurg 15:319–323
Mastronardi L, Ducati A, Ferrante L (2006) Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease. Preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir 148:307–312
Meier U, Kemmesies D (2004) [Experiences with six different intervertebral disc spacers for spondylodesis of the cervical spine]. Orthopade 33:1290–1299 (German)
Odom GL, Finney W, Woodhall B (1958) Cervical disc lesions. JAMA 166:23–28
Peolsson A, Hedlund R, Vavruch L, Oberg B (2003) Predictive factors for the outcome of anterior cervical decompression and fusion. Eur Spine J 12:274–280
Ryu SI, Mitchell M, Kim DH (2006) A prospective randomized study comparing a cervical carbon fiber cage to the Smith–Robinson technique with allograft and plating: up to 24 months follow-up. Eur Spine J 15:157–164
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4:447–453
Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA (2005) Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine 2:116–122
Siddiqui AA, Jackowski A (2003) Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. J Bone Joint Surg Br 85:1019–1025
Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS et al (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 28:134–139
Smith AW, Robinson RA (1958) The treatment of certain spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40:607–624
Singh A, Crockard HA (2001) Comparison of seven different scales used to quantify severity of cervical spondylotic myelopathy and post-operative improvement. J Outcome Meas 5:798–818
Tureyen K (2003) Disc height loss after anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir 145:565–569
van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW (2005) Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J 5:645–649
Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine 27:1694–701
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Peter Ulrich, Offenbach, Germany
The authors deal in their prospective study with a typical complication of anterior cervical discectomy, the loss of disc height and increasing kyphosis. Despite recent advances in spacer technology, the problem is far from being solved. Furthermore, the variety of solutions extolled by the industry makes it more difficult to make the right choice. The purpose of the study was to evaluate, in a randomized controlled protocol, whether the cage design influences the extent of correction loss and the clinical results. At 6 months after mono-segmental discectomy, the cage with the greater contact surface area increased at the anterior lower aspect (Shell™ cage, AMT Company, Nonnweiler, Germany) yielded significantly better results in the radiologic outcome than its counterpart (Solis™ cage, Stryker Company, Kalamazoo, USA). The correlation between radiologic criteria and clinic was less compelling. The authors present an innovative method of measuring segmental height, which seems quite valuable. The conclusion that a careful choice of the proper cage is crucial for obtaining good radiological and clinical results confirms a widespread experience. Despite a limited number of patients enrolled in the study and a relatively short follow-up, the paper presents a remarkable contribution to the ongoing discussion about the best technique in ventral fusion after anterior cervical discectomy.
Hiroshi Nakagawa, Nagoya, Japan
This is a randomized prospective clinical study on subsidence following anterior cervical inter-body fusion using two different cages made of PEEK.
It demonstrated a well-analyzed data which recommended usage of cages with a large-enough contact surface area to preserve the segmental height and lordosis, although this study is of limited value because of a relatively small number of cases, rather short follow-ups, and no CT follow-ups.
For the last decade, we have had some experience of more than 400 cases with cervical myelopathy and radiculopathy which were treated by anterior inter-body cage fixation using cyrindrical titanium cages. In cervical discs and spondylosis, two cages were inserted side by side in a locked fashion and with the anterior cage surface placed along the anterior cortex of the vertebrae in order to minimize the subsidence of the cages.
One thing I can not understand is that the authors used anterior plating in addition to inter-body cages in cases with cervical myelopathy. Is there any rationale for this? In our series, about 70% of the cases have myelopathy and have been treated mostly by cages only without much problem.
With more experience and cases, I hope they will come up with a lesser invasive method in the future.
Disclaimer
None of the authors has received any financial support from any company cited in this study, and none of the authors has any financial or other interest in a company involved in this study.
Rights and permissions
About this article
Cite this article
Kast, E., Derakhshani, S., Bothmann, M. et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 32, 207–214 (2009). https://doi.org/10.1007/s10143-008-0168-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-008-0168-y