Abstract
Purpose
Impingement is a major source for decreased range of motion (ROM) and dislocation in total hip arthroplasty (THA). In the current study we analyzed the impact of soft tissue impingement on ROM compared to bony and/or prosthetic impingement.
Methods
In the course of a prospective clinical trial 54 patients underwent cementless total hip arthroplasty in the lateral decubitus position using imageless navigation. The navigation device enabled intra-operative ROM measurements indicating soft tissue impingement. Post-operatively, all patients received postoperative 3D-CT. Absolute ROM without bony and/or prosthetic impingement was calculated with the help of a collision-detection-algorithm.
Results
Due to soft tissue impingement we found a reduced ROM of over 20° (p < 0.001) compared to bony and/or prosthetic impingement regarding flexion, extension, abduction and adduction and of over 10° regarding external rotation (p < 0.001). In contrast, soft tissue impingement showed less impact on internal rotation in 90° of flexion (p = 0.76). Multivariate analysis showed an association between BMI and flexion, whereas all other ROM directions were independent of BMI.
Conclusions
Soft tissue has a major impact on impingement-free ROM after THA. For the majority of movements, soft tissue restrictions are more important than bony and prosthetic impingement. Future models of patient individual joint replacement including pre-operative (CT) planning and intra-operative navigation should include algorithms additionally accounting for soft tissue impingement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Impingement in total hip arthroplasty (THA) is associated with reduced range of motion (ROM), higher risk of dislocation, component wear, and finally patient dissatisfaction [1–3]. In general impingement can occur between bony, prosthetic, and/or soft tissue structures [4, 5] (Fig. 1). Intra-operatively the orthopaedic surgeon aims to find an optimized implant position to guarantee an impingement free ROM post-operatively. Therefore, trial implants are used enabling intra-operative ROM testing. In case of impingement within ROM benchmarks required for activities of daily living (ADL) [6–8], different intra-operative options exist such as implant reorientation, offset increase or resection of osteophytes [9, 10]. However, intra-operative ROM estimation by eye harbors the risk of misinterpretation. Previous studies have shown the difficulty of intra-operatively preventing impingement by visual implant orientation [11]. In contrast, technical progress has developed biomathematical models to prevent impingement [12]. However, these algorithms focus on prosthetic impingement without accounting for soft tissue. Similarly, 3D-CT analysis offer information about prosthetic and bony impingement without considering soft tissue structures [13]. Although THA is one of the most common and successful orthopaedic procedures, there is nonetheless little published information concerning the impact of soft tissue on impingement free ROM compared to bony and/or prosthetic impingement.
In the current study we (1) aimed to investigate the intra-operative ROM, restricted by soft tissue, in minimally-invasive THA through an anterolateral approach in a lateral decubitus position compared to prosthetic and/or bony impingement. Furthermore, we (2) researched into correlations with anthropometric patient data (ASA, BMI, Kellgren-Lawrence index, incision length, treatment side, and sex) and implant geometries (cup size, stem size, stem geometry).
Patients and methods
Study flow and ethics
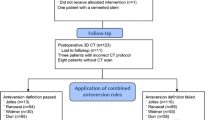
In the course of a registered, prospective controlled trial (DRKS00000739, German Clinical Trials Register) 54 patients underwent cementless THA using imageless navigation. Post-operatively, all patients received 3D-CT. This investigation was approved by the local Ethics Commission (10-121-0263). The current study is a subgroup analysis from a larger cohort [11]. Baseline characteristics of all patients included in this analysis are displayed in Table 1.
Patients
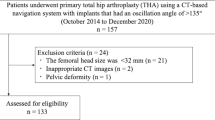
Patients admitted for primary cementless unilateral (minimal or no osteoarthritis of the contralateral hip) THA due to primary or secondary osteoarthritis between the ages of 50 and 75 with an ASA (American Society of Anesthesiologists) score ≤ 3 were recruited at our Department of Orthopaedic Surgery between December 2011 and February 2013. Exclusion criteria according to the criteria of the primary outcome were coxarthritis secondary to hip dysplasia, post-traumatic hip deformities, and prior hip surgery. In the navigated arm out of 66 patients, four did not receive the allocated intervention. In detail, two patients needed an offset liner (+4 mm) for a sufficient reconstruction of the acetabular offset, and one patient needed a cemented stem. These patients were excluded according to the study protocol. In one case the navigation system shut down during the procedure, and registration was lost. Three patients withdrew their informed consent, refused further participation in the study and were regarded as dropouts. For three patients CT data were not available. Navigated soft tissue measurements were not performed with two patients. The remaining 54 navigated cases were included for analysis. Anthropometric characteristics are shown in Table 1.
Operative procedures
THAs were performed by four experienced orthopaedic surgeons (JG, TR, ES, MW) from Regensburg University Medical Center. All operations were performed with the patient in lateral decubitus position through a minimally invasive anterolateral approach to the hip after an intermuscular and interneural tissue plane between the tensor muscle and the gluteus medius muscle [14]. During the procedure the patient was secured by two stiff patient positioners on the proximal part of the sacrum and on the symphysis. Press fit components (Pinnacle; DePuy, Warsaw, IN, USA) and cement-free hydroxyapatite-coated stems (Corail; DePuy Warsaw, IN, USA) were used. The tribologic pairing consisted of polyethylene liners and metal heads with a diameter of 32 mm. Operations were performed in hemispinal anesthesia with additional sedatives providing a maximum of relaxation.
An imageless navigation system (Hip 6.0 prototype, Brainlab, Feldkirchen, Germany) was used for all procedures. Imageless navigation provides accurate and reproducible intra-operative measurement of ROM independently of patient/pelvic positioning. In literature it has been shown that the mean difference in ROM analyses between 3D-CT and imageless navigation technology lies under 5° [15]. The registration process for navigated THA in a lateral decubitus position has been described previously [16–18]. Reference pins (two Kirschner wires of 3.2 mm diameter) were fixed into the anterior iliac crest and into the ventrolateral third of the distal femur. The four points defining the anterior pelvic plane (APP, anterior superior iliac spines, and pubic tubercles) were registered using a reference pointer positioned on the skin’s surface. On the femoral side, the medial and lateral aspects of the epicondyles and ankle points were registered [11].
Intra-operative ROM analysis
Investigation of ROM with computer navigation measurements was performed immediately after insertion of the final implants. Flexion, extension, abduction, adduction, external rotation, and internal rotation in 90° flexion were measured through passive movement of the operated leg by the operating surgeon to ROM limits (Fig. 2). The patient’s thorax, pelvis, and lower extremities including the mechanical axis of the femur (estimated by the femoral head centre and the centre of both femoral epicondyles) were in line with the boundaries of the operation table. The basic position was the leg held straight horizontally in relation to the floor. This basic position was comparable for navigation and 3D-CT measurements as the movements were performed in relation to the APP, the reference plane for both navigation and 3D-CT measurements, combined with the femoral mechanical axis. Automatic detection of motion by the navigation system was visible on the screen (Fig. 3).
Post-operative ROM analysis
For CT based analysis (Somatom Sensation 16; Siemens, Erlangen, Germany) six weeks post-operatively the pelvic bone, the femur, and the metal acetabular and femoral components were segmented separately by an independent external institute (MeVis Medical Solutions, Bremen, Germany). The ROM analysis by virtual movement was generated by means of these segmented bone models with the help of an already described algorithm with automatic detection of bony/prosthetic impingement [11]. Directions of movements were defined according to the recommendations of the International Society of Biomechanics (ISB) [19]. For every direction (flexion/extension, abduction/adduction, internal rotation in 90° of flexion/external rotation in 0° of flexion) the absolute ROM, i.e., the ROM until a collision occured, was measured by using the collision-detection-algorithm [15].
Outcomes and data analysis
IBM SPSS Statistics 22 (SPSS Inc, Chicago, IL, USA) was used for analysis. The navigation measurements were compared with the analysis for prosthetic and bony impingement. We performed a descriptive analysis and the Wilcoxon test on a 5 % significance level reporting means, standard deviation and range to show differences between measurements of soft tissue impingement and analysis for prosthetic and bony impingement. For illustration of method comparison corresponding box plots are presented.
The correlations between the mean ROM restricted by soft tissues and age, BMI, ASA, Kellgren score, sex, cup size, and stem size were analyzed with a binary logistic regression model.
Results
Mean implant positions were 42.6° ± 5.2° for cup inclination, 18.3° ± 6.6° for cup anteversion and 9.0° ± 10.5° for stem torsion. We found a reduced ROM due to soft tissue impingement. The differences between measurements of soft tissue impingement and ROM restricted by prosthetic/bony impingement were over 20° for flexion, extension, abduction, and adduction (p < 0.001) and over 10° for external rotation (p < 0.001) (Table 2). Soft tissue impingement appeared to have less impact in internal rotation at 90° of flexion (p = 0.76). Comparison of combined prosthetic/bony with isolated prosthetic impingement revealed a decreased ROM of more than 20° for adduction and external rotation (p < 0.001). For all other ROM directions the differences between combined prosthetic/bony and isolated prosthetic impingement were less than 10°. Differences in ROM (imageless navigation) measurements between soft tissue, combined prosthetic/bony and prosthetic impingement are displayed in Table 2. Box plots of the measurements of prosthetic, combined prosthetic/bony and soft tissue impingement for all ROM directions are presented in Fig. 4.
In a search for variables influencing ROM we found in a multivariate analysis ROM restriction of >20° in flexion due to soft tissue impingement to be associated with BMI (HR = 1.2, p = 0.05, table XY) whereas we found no other correlation between soft tissue restrictions for flexion and patient specific characteristics or implant data such as sex, ASA, age, Kellgren score, cup size, and stem size (Table 3). Furthermore, no correlations were found for all other ROM directions and BMI as well other patient characteristics (data not shown).
Discussion
In the current study we showed that the soft tissue situation is the limiting component for most directions of movement after cementless THA. Only for internal rotation, there is no significant difference between soft tissue ROM and prosthetic/osseous ROM. Increased BMI is an important parameter regarding soft tissue impingement as demonstrated in the multivariate analysis for flexion.
In literature ROM testing during THA is discussed controversially. Widmer et al. [12] focused on the relative orientation of the acetabular and femoral prosthetic component to each other and its influence on the overall ROM with the help of biomathematical calculations and theoretical assumptions. The aim was to position both components in such a way that the normal hip joint ROM [19] was contained within the prosthetic ROM.
In addition to impingement between prosthetic components impingement can also occur between bony structures. However, additionally soft tissues can reduce ROM. Whereas the latest studies succeeded in analyzing and preventing impingement between osseous and/or prosthetic structures [11], there is only little data about reduction of ROM through soft tissues. Nonetheless soft tissue impingement is commonly accepted as one reason for reduced ROM and dislocation [20–22]. Elkins et al. performed a biomechanical analysis of soft tissue impingement of the thigh and showed an increased risk for dislocation for BMIs of 40 or greater [23].
There are several limitations of our study. First, mechanical and muscular limitations, e.g., contractures, neuro muscular activity, and muscular strength also have the potential to reduce ROM in active patients. Furthermore, soft tissue tension under real life conditions may modify ROM. Moreover, it has to be considered, that intra-operative passive hip ROM can be affected by different types of anesthesia, surgical approach, sterile drapes, soft tissue interventions, orientation of prosthetic components, and implant design [9, 10]. Wound healing and scar formation could similarly alter post-operative ROM. Therefore, the registered intra-operative ROM may vary from post-operative ROM during activities of daily living. However, we did not intend to investigate post-operative ROM but to focus on the general impact of soft tissue on ROM without potential confounders as mentioned above. Second, we only performed a passive ROM analysis under anesthesia. No active muscular contributions were considered. Biomechanical studies with gait analysis and further studies to explore soft tissue impingement have to be performed to answer these ambiguous items. Third, we did not account for pelvic tilt in our ROM analysis. Under walking conditions the pelvic position may be different. We believe that the issue of dynamic pelvic tilt is yet to be resolved [24–26]. Theoretically, navigation offers the chance to measure the pelvic tilt on the operating table [27]. Fourth, with 3D-CT analysis and computer navigation we compared two different ROM measurement methods. However, previous studies have shown that imageless navigation provides accurate and reproducible intra-operative measurement of ROM independently of patient/pelvic positioning. The mean difference in ROM analyses between 3D-CT analysis and imageless navigation technology has been reported to be under 5° [15].
Soft tissue impingement after THA has a major impact on impingement free ROM for flexion, extension, abduction, adduction, and external rotation whereas internal rotation in 90° of flexion is less susceptible to soft tissue impingement. Although a high BMI is regarded as the major risk factor for soft tissue impingement, it occurs for most ROM directions independently of BMI. Therefore, future algorithms for patient individual improvement of post-operative ROM are encouraged to account for soft tissue structures.
References
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F (2002) Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty 17:359–364
Dorr LD, Malik A, Wan Z, Long WT, Harris M (2007) Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res 465:92–99
Craiovan B, Grifka J, Keshmiri A, Moser B, Wörner M, Renkawitz T (2015) Bone defect adjusted strategy in revision arthroplasty of the hip: wich implant in wich situation? Innovations and approved methods. Orthopade 44(5):366–374
Trousdale RT, Cabanela ME, Berry DJ (1995) Anterior iliopsoas impingement after total hip arthroplasty. J Arthroplasty 10:546–549
Yoshimine F (2006) The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech 39:1315–1323
D’Lima DD, Urquhart AG, Buehler KO et al (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am 82:315
Miki H, Yamanashi W, Nishii T et al (2007) Anatomic hip range of motion after implantation during total hip arthroplasty as measured by a navigation system. J Arthroplasty 7:946–952
Seki M, Yuasa N, Ohkuni K (1998) Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res 16:513
Shoji T, Yamasaki T, Izumi S, Hachisuka S, Ochi M (2016) The influence of stem offset and neck shaft angles on the range of motion in total hip arthroplasty. Int Orthop 40(2):245–253
Hirata M, Nakashima Y, Hara D, Kanazawa M, Kohno Y, Yoshimoto K, Iwamoto Y (2015) Optimal anterior femoral offset for functional range of motion in total hip arthroplasty--a computer simulation study. Int Orthop 39(4):645–651
Renkawitz T, Weber M, Springorum R, Sendtner E, Woerner M, Ulm K, Weber T, Grifka J (2015) Impingement-free range of movement, acetabular component cover and early clinical results comparing 'femur-first' navigation and 'conventional' minimally invasive total hip arthroplasty: a randomised controlled trial. Bone Joint J 97(7):890–898
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815
Shoji T, Yasunaga Y, Yamasaki T, Mori R, Hamanishi M, Ochi M (2013) Bony impingement depends on the bone morphology of the hip after total hip arthroplasty. Int Orthop 37(10):1897–1903
Michel M, Witschger P (2007) MicroHip: a minimally invasive procedure for total hip replacement surgery using a modified Smith-Peterson approach. Ortop Traumatol Rehabil 9:46–51
Renkawitz T, Haimerl M, Dohmen L, Woerner M, Springorum HR, Sendtner E, Heers G, Weber M, Grifka J (2012) Development and evaluation of an image-free computer-assisted impingement detection technique for total hip arthroplasty. Proc Inst Mech Eng H 226(12):911–918
Renkawitz T, Haimerl M, Dohmen L, Gneiting S, Wegner M, Ehret N, Buchele C, Schubert M, Lechler P, Woerner M, Sendtner E, Schuster T, Ulm K, Springorum R, Grifka J (2011) Minimally invasive computer-navigated total hip arthroplasty, following the concept of femur first and combined anteversion: design of a blinded randomized controlled trial. BMC Musculoskelet Disord 12:192
Sendtner E, Tibor S, Winkler R et al (2010) Stem torsion in total hip replacement. Acta Orthop 81:579–582
Turley GA, Ahmed SM, Williams MA, Griffin DR (2011) Establishing a range of motion boundary for total hip arthroplasty. Proc Inst Mech Eng H 225:769–782
Wu G, Siegler S, Allard P et al (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech 35:543–548
Brooks PJ (2013) Dislocation following total hip replacement: causes and cures. Bone Joint J 95-B:67–69
Preininger B, Haschke F, Perka C (2014) Diagnostics and therapy of luxation after total hip arthroplasty. Orthopade 43(1):54–63
Hayashi S, Nishiyama T, Fujishiro T, Hashimoto S, Kanzaki N, Nishida K, Kurosaka M (2012) Obese patients may have more soft tissue impingement following primary total hip arthroplasty. Int Orthop 36(12):2419–2423
Elkins JM, Daniel M, Pedersen DR, Singh B, Yack HJ, Callaghan JJ, Brown TD (2013) Morbid obesity may increase dislocation in total hip patients: a biomechanical analysis. Clin Orthop Relat Res 471(3):971–980
Malik A, Maheshwari A, Dorr LD (2007) Impingement with total hip replacement. J Bone Joint Surg Am 89-A:1832–1842
McCollum DE, Gray WJ (1990) Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res 261:159–170
Parratte S, Pagnano MW, Coleman-Wood K, Kaufman KR, Berry DJ (2009) The 2008 Frank Stinchfield award: variation in postoperative pelvic tilt may confound the accuracy of hip navigation systems. Clin Orthop Relat Res 467:43–49
Babisch JW, Layher F, Amiot LP (2008) The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am 90-A:357–365
Acknowledgments
The help of Ms. S. Kling, Ms. C. Jendrewski, Ms. M. Riedl, Mr. M. Schubert, Mr. A. Hapfelmeier, Mr. B. Messmer, Mr. L. Dohmen, and Dr. M. Haimerl in this project is appreciated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval and informed consent
All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
No author’s financial or any other conflicts of interest are related directly or indirectly to the subject of this article. Funding for this clinical trial was provided by the German Federal Ministry of Education and Research (BMBF; grant number 01EZ0915). No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Rights and permissions
About this article
Cite this article
Woerner, M., Weber, M., Sendtner, E. et al. Soft tissue restricts impingement-free mobility in total hip arthroplasty. International Orthopaedics (SICOT) 41, 277–282 (2017). https://doi.org/10.1007/s00264-016-3216-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3216-1