Abstract
Purpose
In this prospective study of 135 patients undergoing cementless total hip arthroplasty (THA) we asked whether six current definitions of combined anteversion prevent impingement and increase postoperative patient individual impingement-free range-of-motion (ROM).
Methods
Implant position was measured by an independent, external institute on 3D-CT performed six weeks post-operatively. Post-operative ROM was calculated using a CT-based algorithm detecting osseous and/or prosthetic impingement by virtual hip movement. Additionally, clinical ROM was evaluated pre-operatively and one-year post-operatively by a blinded observer.
Results
Combined component position of cup and stem according to the definitions of Ranawat, Widmer, Dorr, Hisatome and Yoshimine inhibited prosthetic impingement in over 90 %, while combined osseous and prosthetic impingement still occurred in over 40 % of the cases. The recommendations by Jolles, Widmer, Dorr, Yoshimine and Hisatome enabled higher flexion (p ≤ 0.001) and internal rotation (p ≤ 0.006). Clinically, anteversion rules of Widmer and Yoshimine provided one-year post-operatively statistically but not clinically relevant higher internal rotation (p ≤0.034).
Conclusion
Standard rules of combined anteversion detect prosthetic but fail to prevent combined osseous and prosthetic impingement in THA. Future models will have to account for the patient-individual anatomic situation to ensure impingement-free ROM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following the concept of combined anteversion during total hip arthroplasty (THA), the surgeon should consider cup version when deciding on the resulting stem in cemented THA and vice versa in cementless THA, respectively [1, 2]. Combined anteversion in THA has been shown to be associated with range of motion (ROM), impingement, dislocation, component wear and finally patient dissatisfaction [3, 4]. The intended combined anteversion is still a subject of debate. In 1970, the relation of cup and stem anteversion was first analysed in neonatal cadaveric hips regarding hip dysplasia [5]. Since then a variety of distinct definitions of combined anteversion have emerged suggesting target areas for combined cup and stem anteversion in THA [2, 6–9]. Historically, these combined anteversion guidelines have emerged from different scientific backgrounds ranging from intra-operative descriptions [10] and retrospective analysis [6] to navigation guided THA [2] and biomathematical models [7–9]. Ranawat and Maynard recommended an experienced based combined anteversion between 25° and 45° for women and between 25° and 35° for men [10]. Jolles et al. evaluated possible risk factors for hip dislocation after THA and found a 6.9-fold increase in patients with combined anteversion outside 40–60° [6]. In the 21st century, the technical progress opened a novel approach to biomathematical combined anteversion models calculating optimal ROM by virtual hip joint movement [7–9]. New operative concepts such as navigation-guided implantation harboured the possibility to control combined anteversion intra-operatively. Dorr et al. recommended combined anteversion of cup and stem between 25° and 50° [2]. Whereas these concepts provide recommendations based on experience [10], clinical data [6] or virtual mathematical calculations [7], none of the present combined anteversion rules has been created accounting for bony or soft tissue structures or functional aspects such as pelvic tilt [11].
We have recently demonstrated that component positioning according to combined anteversion rules does not result in better post-operative gait function [12]. We now focused on the six combined anteversion rules directly recommending safe zones in THA. With respect to the same acetabular reference [13], we analysed osseous and/or prosthetic impingement regarding these standard definitions of combined anteversion (Jolles et al. [6], Ranawat and Maynard [10], Dorr et al. [2], Widmer and Zurfluh [7], Yoshimine [9], Hisatome and Doi [8]) for THA using a three-dimensional computed tomography (3D-CT) ROM analysis and posed the following questions: (1) Do the six recommendations for combined anteversion prevent osseous and/or prosthetic impingement? (2) Are the differences in ROM relevant for activities of daily living (ADL)? (3) Is there any clinical difference in ROM one year post-operatively?
Patients and methods
In the course of a registered, prospective controlled trial (DRKS00000739, German Clinical Trials Register), three dimensional computed tomography scans (3D-CT) were obtained after cementless THA. The main outcome of the study dealt with the comparison between conventional and navigation guided THA [14]. The present study is an independent secondary outcome analysis. A sovereign power calculation was performed for investigation of postoperative ROM in this analysis on a two-sided 5 % significance level. The clinically relevant difference in hip joint movement was set at 10 degrees including a standard deviation of 10 degrees according to literature [15]. Based on these considerations, a sample size of 23 in each group achieved a power of 90 % using two-sample t-tests (GPower 3.1, Düsseldorf, Germany). The investigation was approved by the local medical ethics committee (No.: 10-121-0263).
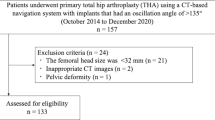
According to the study protocol eligible participants were patients between the ages of 50 and 75 with an American Society of Anaesthesiologists (ASA) score ≤ 3 who were admitted for primary cementless unilateral THA due to primary or secondary osteoarthritis at our institution. No patients had significant disease in the contralateral hip. Exclusion criteria were age < 50 (as a post-operative CT scan was required) and > 75 years (to ensure post-operative follow up was achieved), ASA score > 3, arthritis of the secondary to hip dysplasia, post-traumatic hip deformities, and previous hip surgery. Patients were recruited and informed consent was obtained by one of the clinical investigators. Figure 1 summarizes the data on the participants in the study. THA in all patients was performed in the lateral decubitus position using a minimally-invasive single-incision anterolateral approach [16]. Press-fit acetabular components with neutral liners and cement-free hydroxyapatite-coated stems (Pinnacle cup, Corail stem, DePuy, Warsaw, IN, USA) with metal heads of 32 mm were used except for one case with severe osteoporosis. Due to the elliptic neck design of the stem the head neck ratio is 3.50 for extension/flexion and 2.66 for abduction/adduction. Six weeks post-operatively, a pelvic/femoral 3D-CT was performed (Somatom Sensation 16; Siemens, Erlangen, Germany).
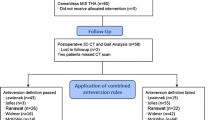
In total, 123 data sets were included for analysis. Anthropometric characteristics of the study group are shown in Table 1 [16]. Independent manual CT segmentation was performed on the pelvic bone and on the metal acetabular and femoral components by an independent external institute (Fraunhofer MEVIS, Bremen, Germany), blinded to individual patient data. Additionally, reference landmarks for providing the pelvic and femoral coordinate system were defined. This included both ASIS and pubic tubercle points to define the pelvic coordinate system and femoral head centre, mechanical axis and condyle axis to define the femoral coordinate system. Based on the manually segmented bone models, the post-operative ROM was calculated by a previously described algorithm (Fig. 2) which automatically determines both prosthetic and combined osseous and prosthetic impingement by virtually moving the leg until a collision between the 3D objects occurs [17, 18]. Neutral orientation for ROM calculations was defined according to the anterior pelvic plane (APP) with the femur along the APP and foot directed straight forward without rotation. For reproducibility, ROM calculations were performed twice and the mean of the two measurements was used for further analysis. Repeated measurements for 3D-CT impingement analysis showed a 95 % confidence interval of mean differences with 0.8–1.4 degrees for flexion, 1.3–3.2 degrees for extension, 0.2–1.0 degrees for external rotation, −0.6 to –0.1 for internal rotation at 90 degrees flexion, −1.7 to –1.3 degrees for abduction and 3.2–5.1 degrees for adduction. We then comparatively assessed the proportion of patients reaching the hip joint ROM configurations without impingement for activities of daily living (ADL) as given by Davis et al., Miki et al. and Turley et al. with at least 110 degrees of flexion, 30 degrees of extension, 50 degrees of abduction, 30 degrees of adduction, 45 degrees of external rotation during extension and 30 degrees of internal rotation during 90 degrees of hip flexion, respectively [4, 19, 20]. At the same time, we differentiated between exclusive prosthetic and combined osseous and prosthetic impingement, respectively. Moreover, cup inclination, anteversion, stem antetorsion and pelvic tilt were evaluated by the independent external institute on the manually segmented reconstruction of pelvis and femur using image-processing software (based on MeVisLab, MeVis) as previously described [18, 21]. In short, the normal vector of the sagittal plane is identical to the vector between both ASIS landmarks. To construct the transversal plane the centre point of the pubic tubercle landmarks was calculated and projected onto the vector between both ASIS landmarks. The vector from the centre point to its projection was used to determine the normal vector of the transversal plane. The normal vector of the coronal plane was calculated as the cross product of the sagittal and transversal normal vectors. Subsequently a plane parallel to the implant aperture was constructed with its normal vector representing the implant axis. Using the radiographic definition in relation to the APP anteversion and inclination angles of the acetabular implant were calculated. For evaluation of stem torsion the condylar axis of the femur was calculated and the mechanical axis of the femur defined by the centre of the caudal contact points of the femoral condyles and the centre of the femoral head. A reference point on the prosthesis was defined so that the vector towards the centre of the femoral head represented the neck of the prosthesis. The normal vector of the plane created from this reference point and both points of the mechanical axis were projected onto a plane orthogonal to the mechanical axis. We calculated the angle between this vector and the orthogonal projected condylar axis and subtracted 90°, thereby defining the degree of femoral stem torsion. Cup coverage was determined with a special coverage algorithm that calculates the bony overlap ratio based on the manually segmented bone models as previously described to ensure sufficient cup coverage [18]. Besides, further impingement-related parameters such as femoral offset and neck length were evaluated (Table 2). Clinical goniometric ROM evaluation was performed by an experienced blinded examiner prior to THA and one year post-operatively. One year after THA, out of 123 patients, 115 were available for clinical ROM analysis.
Impingement-free ROM was calculated based on 3D-CT models of the bony and prosthetic structures. Impingement was determined by virtually moving the leg until a collision between the 3D objects occurred. The maximum achievable ROM in the specified motion directions was measured for all ROM directions (a Extension, b Flexion, c External Rotation, d Internal Rotation, e Abduction, f Adduction)
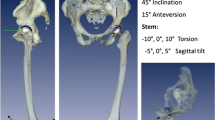
Six common definitions for combined cup and stem anteversion directly associated with recommendations for THA were chosen [2, 6–10]. We then assessed the rate of osseous and/or prosthetic impingement in relation to the six corresponding definitions of combined cup and stem anteversion. For comparability the six combined anteversion definitions were referred to the APP using the formula published by Wan et al. [13]. An overview of the six definitions of combined anteversion is shown in Table 3. Neck length and femoral offset potentially influencing impingement were comparable within the combined anteversion definitions.
For statistical analysis, normally and nonnormally distributed continuous data are presented as mean (standard deviation) or median (interquartile range), respectively. Accordingly, group comparisons were performed by two-sided t-tests or Mann–Whitney U-tests on a 5 % significance level. Absolute and relative frequencies were given for categorical data and compared between groups by chi-square tests on a 5 % significance level. IBM SPSS Statistics 22 (SPSS Inc, Chicago, IL, USA) was used for analysis.
Results
Combined cup and stem anteversion within the recommendations of Ranawat and Maynard [10], Widmer and Zurfluh [7], Dorr et al. [2], Hisatome and Doi [8] and Yoshimine [9] prevented prosthetic impingement in over 90 % of cases for all ROM directions of ADL, whereas combined anteversion according to the rule of Jolles et al. [6] inhibited prosthetic impingement in 76.9 % (Fig. 3a). In contrast, for combined osseous and prosthetic impingement, cup and stem anteversion within Widmer’s and Zurfluh’s definition [7] inhibited impingement regarding ADL in 56.7 % of the cases. For all other definitions of combined anteversion combined osseous and prosthetic impingement occurred in over 50 % of patients although combined anteversion was inside benchmarks of the corresponding definition (Fig. 3b). The reason for impingement was predominantly an insufficient external rotation below 45 degrees and abduction under 50 degrees according to limits for required ROM for ADL (supplementary material 1).
In regards to absolute single ROM directions without osseous or prosthetic impingement, we found a higher flexion of about 10 degrees (p ≤ 0.006) and higher internal rotation at 90 degrees flexion of about 15 degrees (p ≤ 0.001, Fig. 4) for combined anteversion according to Jolles et al. [6], Widmer and Zurfluh [7], Dorr et al. [2], Yoshimine [9] and Hisatome and Doi [8]. In contrast, extension was decreased with a mean difference of about 10 degrees using these five definitions (p ≤ 0.032), but outside a clinically relevant area, since extension was still above limits for ADL. A similar clinically irrelevant trend for decreased ROM was observed for external rotation and adduction with mean differences below 10 degrees (Table 4).
Impingement-free ROM for (a) flexion and (b) internal rotation at 90° flexion is demonstrated for cup and stem version according to the current available definitions of combined anteversion. Significance levels are given above. The transition between grey and white areas marks the area necessary for ROM in ADL
Evaluation of clinical outcome showed one year after THA higher internal rotation at 90 degrees flexion (Fig. 5) for patients with combined cup and stem anteversion according to the definitions of Widmer and Zurfluh [7] (p = 0.019) and Yoshimine [9] (p = 0.034). For all other ROM directions, no differences were observed regarding combined anteversion rules one year after THA. Similarly, in the pre-operative situation there was no difference in clinical ROM for all combined anteversion rules (supplementary material 2).
Discussion
The concept of combined anteversion defines cup anteversion as a function of prosthetic stem version [18]. If the orthopaedic surgeon relied on one of the numerous recommendations for optimal combined cup and stem version, an optimum ROM without impingement should be realised for ADL. We therefore posed three questions: (1) Do the six recommendations for combined anteversion prevent osseous and/or prosthetic impingement? (2) Are the differences in ROM relevant for activities of daily living (ADL)? (3) Is there any clinical difference in ROM one year post-operatively?
There are five limitations of this study. First, the six common definitions of combined anteversion in THA used in this study are of different origin. Ranawat and Maynard [10] provided recommendations for successful cemented THA using an intra-operative assessment for stem version with the tibia vertical as a reference [10], whereas Jolles et al. [6] researched into the prevalence of complications after THA. Novel approaches to combined anteversion were introduced using new intra-operative techniques such as navigation [2]. In addition, computerized models were generated to evaluate ROM in relation to cup and stem position [7–9]. Therefore, the comparability of these definitions of combined anteversion is limited. Besides, several of those standard rules for THA use different references for acetabular orientation as described by Murray [22] and either refer to the coronal plane or APP [13]. Thus, we had to adjust the six recommendations for combined anteversion to the radiographic APP plane to ensure comparability. Second, our 3D-CT based assessment of cup inclination and version was performed in the APP, although pelvic tilt has an impact on clinical function. However, pelvic tilt differs during gait and thus is a dynamic process, which according to the authors’ opinion has not been sufficiently resolved yet [11]. Third, regarding combined anteversion rules according to Jolles et al. [6] and Hisatome and Doi [8] our analysis was underpowered, reducing the possibility to assess precisely these two combined anteversion rules. Despite the high number of cases, we had few cases fulfilling combined anteversion according to Jolles et al. [6] and Hisatome. This might be due to the high benchmarks for combined anteversion within 40° and 60° for Jolles et al. [6]. The mean combined anteversion of 25.9° in our study group through an anterolateral approach was comparable with literature using a modified Hardinge approach with a mean combined anteversion of cup and stem of 29.1° [23]. However, in posterior approaches higher combined anteversion values are reported due to the increased risk of posterior dislocation [2]. For Hisatome and Doi [8] extraordinary strict ROM criteria were postulated. Fourth, the 3D-CT impingement detection algorithm assessed osseous and prosthetic impingement. However, we were not able to look for soft tissue related impingement. In obese patients, soft tissue may limit ROM before hardware impingement occurs [24, 25]. Besides, iliopsoas impingement is a further parameter influencing ROM [26]. Fifth, we performed only cementless THA through a minimally invasive anterolateral approach using non-modular components of one manufacturer (CCD 135°, cone 12/14, head 32 mm diameter, head neck ratio 3.50 for extension/flexion and 2.66 for abduction/adduction). However, the investigated definitions of combined anteversion rely on different prosthetic designs and head diameters restricting their comparability [27].
In answer to the first question of our study, prosthetic impingement was inhibited in over 90 %, when cup/stem anteversion were within the combined anteversion definitions as published by Ranawat and Maynard [10], Widmer and Zurfluh [7], Dorr et al. [2], Hisatome and Doi [8] or Yoshimine [9]. This indicates that the current combined anteversion models enable detection of prosthetic impingement and therefore serve the purpose of their original design. In contrast, none of the current available definitions of combined anteversion could entirely prevent combined bony and/or prosthetic impingement. Although combined anteversion of cup and stem was within the target zone of combined anteversion, combined osseous and prosthetic impingement still occurred in over 40 % of cases for all six rules of combined anteversion. This is further confirmed by one post-operative dislocation we experienced in our study group. Our analysis revealed an impingement between an unusually prominent inferior iliac spine and the greater trochanter in 90° of flexion and 20° internal rotation. When we analysed this case we identified the fact that cup and stem were within the safe zones. One cause of the failure of combined anteversion rules in detecting combined bony and/or prosthetic impingement might be the absence of integrating functional aspects of hip joint movement. The pelvic tilt might have a major influence on the functional outcome after THA [28]. The combined anteversion concepts do not consider this properly. However, since pelvic tilt is a dynamic variable during gait it is especially challenging to control the impact of this parameter on functional outcome [11]. Furthermore, the sagittal stem alignment is a further parameter influencing impingement-free ROM [29, 30].
Responding to the second question, we found higher flexion and internal rotation at 90 degrees flexion of 10 degrees and even more for five of the six investigated definitions of combined anteversion and therefore regard this as clinically relevant. This means that anterior impingement and consecutively posterior dislocation might be reduced if cup and stem anteversion are inside the limits of recommended combined anteversion. In contrast, extension and external rotation in extension were reduced compared to cup and stem version outside the benchmarks of these combined anteversion definitions. This could lead to posterior impingement and therefore anterior dislocation could appear more frequently. Since posterior impingement was observed in extreme ROM with over 50 degrees extension and 40 degrees of external rotation, we do valuate this as clinically irrelevant.
In terms of our third question, we measured a higher internal rotation at 90 degrees flexion for combined cup and stem version according to Yoshimine [9] and Widmer and Zurfluh [7]. However, the mean differences were between three and four degrees and thus must be regarded as clinically irrelevant. For all other ROM directions, clinical ROM was comparable independently of combined cup and stem version according to current anteversion rules. These findings underline that combined osseous, prosthetic and moreover soft tissue impingement are patient-individual. Actually, impingement is even more complicated since dynamic alterations of pelvic tilt further influence ROM during ADL [11]. No current standard combined anteversion rule reflects this complex situation sufficiently. Therefore, intraoperative control tools such as imageless navigation have to be developed to enable intra-operative combined cup and stem orientation according to the patient’s individual anatomic situation. Meanwhile, out of the current available definitions of combined anteversion the recommendations according to Widmer and Zurfluh [7] and Yoshimine [9] should be favoured since they were best able to detect prosthetic impingement and enable higher ROM.
To the best of our knowledge, this is the first study comparing present definitions of combined anteversion among each other regarding their impact on post-operative ROM after THA based upon data from a clinical trial with 3D-CT analysis. In summary, standard combined anteversion rules for THA appear suitable to prevent prosthetic impingement during THA but fail to prevent combined osseous and prosthetic impingement. Future models within the concept of combined anteversion for THA will therefore have to account for both the component position as well as the patient’s individual anatomic situation including functional aspects such as pelvic tilt to ensure impingement-free ROM.
References
Widmer KH (2004) A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty 19:387–390
Dorr LD, Malik A, Dastane M, Wan Z (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467:119–127. doi:10.1007/s11999-008-0598-4
Malik A, Maheshwari A, Dorr LD (2007) Impingement with total hip replacement. J Bone Joint Surg Am 89:1832–1842. doi:10.2106/JBJS.F.01313
Miki H, Yamanashi W, Nishii T, Sato Y, Yoshikawa H, Sugano N (2007) Anatomic hip range of motion after implantation during total hip arthroplasty as measured by a navigation system. J Arthroplasty 22:946–952. doi:10.1016/j.arth.2007.02.004
McKibbin B (1970) Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg (Br) 52:148–159
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 17:282–288
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821. doi:10.1016/j.orthres.2003.11.001
Hisatome T, Doi H (2011) Theoretically optimum position of the prosthesis in total hip arthroplasty to fulfill the severe range of motion criteria due to neck impingement. J Orthop Sci 16:229–237. doi:10.1007/s00776-011-0039-1
Yoshimine F (2006) The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech 39:1315–1323. doi:10.1016/j.jbiomech.2005.03.008
Ranawat CS, Maynard MJ (1991) Modern technique of cemented total hip arthroplasty. Tech Orthop 6:17–2510. doi:10.1054/arth.2001.24442
Parratte S, Pagnano MW, Coleman-Wood K, Kaufman KR, Berry DJ (2009) The 2008 Frank Stinchfield award: variation in postoperative pelvic tilt may confound the accuracy of hip navigation systems. Clin Orthop Relat Res 467:43–49. doi:10.1007/s11999-008-0521-z
Weber M, Weber T, Woerner M, Craiovan B, Worlicek M, Winkler S, Grifka J, Renkawitz T (2015) The impact of standard combined anteversion definitions on gait and clinical outcome within one year after total hip arthroplasty. Int Orthop 39(12):2323–33. doi:10.1007/s00264-015-2777-8
Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD (2009) Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res 467:32–42. doi:10.1007/s11999-008-0597-5
Renkawitz T, Haimerl M, Dohmen L, Gneiting S, Wegner M, Ehret N, Buchele C, Schubert M, Lechler P, Woerner M, Sendtner E, Schuster T, Ulm K, Springorum R, Grifka J (2011) Minimally invasive computer-navigated total hip arthroplasty, following the concept of femur first and combined anteversion: design of a blinded randomized controlled trial. BMC Musculoskelet Disord 12:192. doi:10.1186/1471-2474-12-192
Pijls BG, Dekkers OM, Middeldorp S, Valstar ER, van der Heide HJ, Van der Linden-Van der Zwaag HM, Nelissen RG (2011) AQUILA: assessment of quality in lower limb arthroplasty. An expert Delphi consensus for total knee and total hip arthroplasty. BMC Musculoskelet Disord 12:173. doi:10.1186/1471-2474-12-173
Michel MC, Witschger P (2007) MicroHip: a minimally invasive procedure for total hip replacement surgery using a modified Smith-Peterson approach. Ortop Traumatol Rehabil 9:46–51
Renkawitz T, Haimerl M, Dohmen L, Woerner M, Springorum HR, Sendtner E, Heers G, Weber M, Grifka J (2012) Development and evaluation of an image-free computer-assisted impingement detection technique for total hip arthroplasty. Proc Inst Mech Eng H 226:911–918. doi:10.1177/0954411912460815
Renkawitz T, Weber M, Springorum HR, Sendtner E, Woerner M, Ulm K, Weber T, Grifka J (2015) Impingement-free range of movement, acetabular component cover and early clinical results comparing 'femur-first' navigation and 'conventional' minimally invasive total hip arthroplasty: a randomised controlled trial. Bone Joint J 97-B:890–898. doi:10.1302/0301-620X.97B7.34729
Davis KE, Ritter MA, Berend ME, Meding JB (2007) The importance of range of motion after total hip arthroplasty. Clin Orthop Relat Res 465:180–184. doi:10.1097/BLO.0b013e31815c5a64
Turley GA, Ahmed SM, Williams MA, Griffin DR (2011) Establishing a range of motion boundary for total hip arthroplasty. Proc Inst Mech Eng H 225:769–782
Weber M, Lechler P, von Kunow F, Vollner F, Keshmiri A, Hapfelmeier A, Grifka J, Renkawitz T (2015) The validity of a novel radiological method for measuring femoral stem version on anteroposterior radiographs of the hip after total hip arthroplasty. Bone Joint J 97-B:306–311. doi:10.1302/0301-620X.97B3.34618
Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Joint Surg (Br) 75:228–232
Wines AP, McNicol D (2006) Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty 21:696–701. doi:10.1016/j.arth.2005.11.008
Hube R, Dienst M, von Roth P (2014) Complications after minimally invasive total hip arthroplasty. Orthopade 43:47–53. doi:10.1007/s00132-013-2123-z
Preininger B, Haschke F, Perka C (2014) Diagnostics and therapy of luxation after total hip arthroplasty. Orthopade 43:54–63. doi:10.1007/s00132-013-2125-x
Park KK, Tsai TY, Dimitriou D, Kwon YM (2016) Three-dimensional in vivo difference between native acetabular version and acetabular component version influences iliopsoas impingement after total hip arthroplasty. Int Orthop. doi:10.1007/s00264-015-3055-5
Tsuda K, Haraguchi K, Koyanagi J, Takahashi S, Sugama R, Fujiwara K (2016) A forty millimetre head significantly improves range of motion compared with a twenty eight millimetre head in total hip arthroplasty using a computed tomography-based navigation system. Int Orthop. doi:10.1007/s00264-015-3095-x
Babisch JW, Layher F, Amiot LP (2008) The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am 90:357–365. doi:10.2106/JBJS.F.00628
Renkawitz T, Haimerl M, Dohmen L, Gneiting S, Lechler P, Woerner M, Springorum HR, Weber M, Sussmann P, Sendtner E, Grifka J (2012) The association between Femoral Tilt and impingement-free range-of-motion in total hip arthroplasty. BMC Musculoskelet Disord 13:65. doi:10.1186/1471-2474-13-65
Müller M, Duda G, Perka C, Tohtz S (2016) The sagittal stem alignment and the stem version clearly influence the impingement-free range of motion in total hip arthroplasty: a computer model-based analysis. Int Orthop 40(3):473–80. doi:10.1007/s00264-015-2845-0
Acknowledgments
We thank Dipl-Ing. Mario Schubert for his support in calculations of biomathematical combined anteversion models.
MW and TR originated the idea for the study and led on its design. TR and JG supervised the project. TR, MW, MWOE, BC, MWOR, FV and JG participated in the design of the study. MW, TR, MWOE, BC, MWOR and HS coordinated the experiment and were responsible for data acquisition. HS performed the clinical follow up. MWOR, MWOE, BC and FV were responsible for CT data collection. MW computed implant positions according to the different definitions. MW performed the statistical testing. All authors read and corrected draft versions of the manuscript and approved the final manuscript.
The project upon which this publication is based was funded by the German Federal Ministry of Education and Research (BMBF) under Project Number 01EZ0915.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Weber, M., Woerner, M., Craiovan, B. et al. Current standard rules of combined anteversion prevent prosthetic impingement but ignore osseous contact in total hip arthroplasty. International Orthopaedics (SICOT) 40, 2495–2504 (2016). https://doi.org/10.1007/s00264-016-3171-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3171-x