Abstract
Purpose
The main drawback of 11C-choline PET/CT for restaging prostate cancer (PCa) patients with biochemical failure is the relatively low positive detection rate for prostate specific antigen (PSA) < 1 ng/ml. This study assessed whether 11C-choline PET/CT predicts survival in PCa patients with PSA < 1 ng/ml.
Methods
This retrospective study included 210 PCa patients treated with radical prostatectomy who underwent 11C-choline PET/CT from December 1, 2004 to July 31, 2007 due to biochemical failure. PCa-specific survival was estimated using Kaplan–Meier curves. Cox regression analysis was used to evaluate the association between clinicopathologic variables and PCa-specific survival. PCa-specific survival was computed as the interval from radical prostatectomy to PCa-specific death.
Results
Median follow-up after radical prostatectomy was 6.9 years (95% confidence interval, CI, 2.0–14.5 years). 11C-choline PET/CT was positive in 20.5% of patients. Median PCa-specific survival was 13.4 years (95% CI, 9.9–16.8 years) in patients with positive 11C-choline PET/CT, and it was not achieved in patients with negative 11C-choline PET/CT (log-rank, chi-square = 15.0, P < 0.001). Ten-year survival probabilities for patients with negative 11C-choline PET/CT and for patients with positive 11C-choline PET/CT were 86.0% (95% CI: 80.7%–91.3%) and 63.6% (95% CI: 54.5–72.7%). At multivariate analysis, only 11C-choline PET/CT significantly predicted PCa-specific survival (hazard ratio = 2.54, 95% CI, 1.05–6.13, P = 0.038). Patients with pathological 11C-choline uptake in the prostatic bed or in pelvic lymph nodes had longer PCa-specific survival in comparison to patients with pathological tracer uptake in the skeleton (log-rank: chi-square = 27.4, P < 0.001).
Conclusion
Despite the relatively low positive detection rate for PSA < 1 ng/ml, positive 11C-choline PET/CT predicts PCa-specific survival in this low PSA range. As long as more sensitive radiotracers, such as 68Ga-PSMA-11, do not become more widely available, these results might support a broader use of radiolabeled choline in restaging PCa for PSA < 1 ng/ml.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the last 20 years, many in-vitro and in-vivo studies have given strong support to the use of positron emission tomography and positron emission tomography/computed tomography (PET/CT) with radiolabeled choline (either 11C-choline or 18F-fluorocholine) in prostate cancer (PCa) patients. Over time, the technique has found robust application in restaging PCa patients with biochemical failure [1,2,3,4,5,6,7,8,9]. Additionally, promising results have been obtained in the initial staging of high-risk PCa patients [10, 11], to guide radiotherapy [12,13,14,15] and possibly in monitoring the response to second-line antiandrogenic therapy [16] or chemotherapy [17, 18].
In the setting of restaging, the major weak point of PET/CT with radiolabeled choline is represented by the relatively low positive detection rate for low PSA values, when the tumor burden is expected to be low and the therapeutic possibilities are expected to be maximal. Castellucci et al. reported a positive detection rate of 28% for PSA < 1.5 ng/ml [19]. Giovacchini et al. reported 26% for PSA between 0.8 ng/ml and 1.0 ng/ml [5]. Other studies reported similar or more distant values depending on the PSA threshold and on characteristics of the sample [4, 6, 7, 20,21,22,23]. For this reason, the European Association of Urology endorses the use of PET/CT with radiolabeled choline in the interval between 1 ng/ml and 2 ng/ml, but not for PSA < 1 ng/ml [24].
During the last few years, emphasis has been given to the potential role that might be played by the radiotracer class of the inhibitors of the prostate specific membrane antigen (PSMA) protein, the most frequently used being 68Ga-PSMA-11 [25,26,27]. Preliminary comparative data indicate that 68Ga-PSMA-11 could be more sensitive than radiolabeled choline for early detection of PCa recurrence, including in the interval of PSA ≤ 1 ng/ml [25,26,27,28,29].
A few survival studies have already been performed in PCa patients with radiolabeled choline, and they have shown that PET/CT with radiolabeled choline can be used to predict survival in PCa patients [30,31,32]. However, the two studies performed by Giovacchini et al. [30, 31] were carried out in populations independently from the PSA values of the patients, and therefore mean PSA was higher than 1 ng/ml. Kwee et al. and Caroli et al. performed two studies with PET/CT in metastatic castration-resistant PCa patients [32, 33]. As such, it is still unexplored whether PET/CT with radiolabeled choline provides prognostic information for low PSA. Due to this relevant issue and the ongoing debate on the use of PET/CT with radiolabeled choline for PSA < 1 ng/ml, we designed this retrospective study to assess whether PET/CT with radiolabeled choline predicts PCa-specific survival for PSA < 1 ng/ml.
Patients and methods
Study population
This retrospective study included 210 PCa patients who underwent 11C-choline PET/CT for restaging of disease between December 1, 2004 and July 31, 2007. Inclusion criteria were: (1) histologically confirmed prostate adenocarcinoma, (2) primary treatment with radical prostatectomy, (3) biochemical failure, defined as PSA higher than 0.2 ng/ml and rising on at least two consecutive measurements performed 3 months apart, (4) clinical and pathological features of interest for multivariate Cox-regression analysis, (5) availability of follow-up information regarding the survival status, and (6) informed consent agreement.
Follow-up
Postoperative clinical surveillance included PSA determinations and rectal examinations every 3 to 12 months. During follow-up availability of imaging techniques, including 11C-choline PET/CT, computed tomography, ultrasonography, magnetic resonance, and bone scintigraphy was variable among patients.
Median follow-up after radical prostatectomy was 6.9 years (95% confidence interval, CI, 2.0–14.5 years). Median follow-up after 11C-choline PET/CT was 4.0 years (95% CI, 0.2–6.7 years). PCa-specific survival was chosen as primary endpoint. PCa-specific death was defined as death in any patient with metastasis who showed progression without another obvious cause of death [34]. PCa–specific survival was defined as the time between radical prostatectomy and PCa-specific death. At last follow-up, 29/210 patients (13.8%) had died and 24/210 patients (11.4%) had died of PCa. Survival times of patients who were alive at the last follow-up contact were censored.
This single-institution study was approved by the Ethical Committee of the San Raffaele Scientific Institute, Milan, Italy. An informed consent form for the execution of 11C-choline PET/CT scans and for anonymous publication of disease-related information according to the Declaration of Helsinki was signed by each patient.
PET/CT acquisition
After a low-dose CT scan, five 1-min frames centered on the pelvis were acquired immediately after the injection of 420 ± 62 MBq of 11C-choline. At the end of dynamic imaging, i.e., about 5 min post-injection, a whole-body PET scan was acquired [5].
Image interpretation
PET/CT images were visually interpreted. Images were analyzed by two nuclear medicine physicians with more than 8 years of experience in PET and PET/CT, and discrepancies were solved by consensus. Local recurrence was defined as focal 11C-choline uptake in the post-surgical prostatectomy loge. Lymph node and bone metastases were defined as focal 11C-choline uptake higher than background [5].
Statistical analysis
Comparisons of variables between two groups were performed using t-test and chi-square test as needed.
PCa-specific survival was estimated using Kaplan–Meier curves. Differences between survival curves of patients with positive 11C-choline PET/CT and negative 11C-choline PET/CT were evaluated using the log-rank test. Survival rates and their 95% confidence intervals were also derived from Kaplan–Meier curves. The association between 11C-choline PET/CT findings and PCa-specific survival was assessed using Cox proportional hazard regression models. Because of the very low number of fatal events and the moderately large sample size, only factors traditionally associated with PCa-survival [34, 35] were entered, so that convergence could be obtained. To minimize biases on survival times introduced by therapies started after 11C-choline PET/CT, patients that received any therapy (anti-androgenic therapy, radiotherapy or chemotherapy) after PET/CT were contrasted at multivariate analysis vs patients that did not receive any additional therapy. To verify that our results were independent by the definition of PCa–specific survival, an ancillary Cox-regression analysis was performed in which PCa–specific survival was computed as the interval between the date of 11C-choline PET/CT and the date of PCa-specific death or censoring. The proportional hazards assumption was formally tested using interaction terms between independent variables and time. All these interactions had P > 0.1.
To assess the robustness of our results, we also assessed survival as a function of the TNM classification of the American Joint Committee on Cancer (AJCC), assuming 11C-choline PET/CT as gold standard for identification of disease. For the analysis, three groups of patients were defined on the basis of five PET/CT anatomical findings, i.e.: (1) patients with pathological 11C-choline uptake in the skeleton (M1b) and in retroperitoneal lymph nodes (M1a), (2) patients with pathological 11C-choline uptake in pelvic lymph nodes (N1 M0) or in the prostate bed (N0) (grouped together to increase the statistical power), 3) patients with negative 11C-choline PET/CT.
PET/CT results were also related to standard of care imaging studies and biopsies.
Statistical significance was defined as P < 0.05. Survival analysis was performed using the SPSS v 18 statistical software package (SPSS Inc., Chicago, IL, USA).
Results
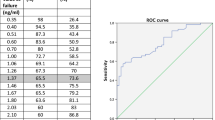
The clinical and pathological characteristics of the sample are reported in Table 1. Median PSA in the whole sample was 0.54 ng/ml. 11C-choline PET/CT was positive in 43/210 patients (20.5%). Patients with positive 11C-choline PET/CT had, in comparison to patients with negative 11C-choline PET/CT, higher PSA, more advanced pathological stage, and received therapy after PET/CT more frequently. On an anatomical basis, pathological 11C-choline uptake was observed in either pelvic (23/210, 11.0%) or in retroperitoneal lymph nodes (6/210, 2.9%), in the skeleton (8/210, 3.8%) and in the post-surgical prostate bed (17/210, 8.1%).
In patients with positive 11C-choline PET/CT, median survival was 13.4 years (95% CI: 9.9–16.8 years). In patients with negative PET/CT, median survival was not achieved owing to the low frequency of fatal events in this group: the difference between the two groups was statistically significant (log-rank, chi-square = 15.0, P < 0.001; Fig. 1). Survival probabilities for the whole group, for patients with negative 11C-choline PET/CT and for patients with positive 11C-choline PET/CT are reported in Table 2. Survival probabilities were always higher for patients with negative 11C-choline PET/CT than for patients with positive 11C-choline PET/CT. For example, 10-year survival probabilities for patients with negative 11C-choline PET/CT and for patients with positive 11C-choline PET/CT were 86.0% (95% CI: 80.7%–91.3%) and 63.6% (95% CI: 54.5–72.7%).
Results of the Cox regression analysis are shown in Table 3. At univariate analysis, statistical significance was attained by 11C-choline PET/CT (P < 0.001), pathological stage (P = 0.045), and Gleason score (P = 0.017). However, at multivariate analysis statistical significance was maintained only by 11C-choline PET/CT (hazard ratio, HR = 2.54, 95% CI, 1.05–6.13, P = 0.038). As expected, patients with higher risk of death were also those that received additional therapy more frequently because of pathological 11C-choline PET/CT. Neglecting this term highly increases the statistical significance of 11C-choline PET/CT (HR = 3.59, 95% CI, 1.50–8.59, P = 0.004).
Using the follow-up interval from 11C-choline PET/CT to the date of PCa-specific death or censoring as time variable did not change the results. Kaplan–Meier analysis showed that median PCa-specific survival was significantly shorter in patients with positive 11C-choline PET/CT (5.9 years) than in patients with negative 11C-choline PET/CT (7.9 years) (log-rank, chi-square = 19.5, P < 0.001, Fig. 2). At Cox regression, statistical significance was reached at univariate analysis by 11C-choline PET/CT (P < 0.001), pathological stage (P = 0.018), and Gleason score (P = 0.013). However, at multivariate analysis the statistical significance was maintained only by 11C-choline PET/CT (HR = 2.96, 95% CI, 1.24–7.08, P = 0.014).
We also assessed survival according to the TNM classification of the AJCC, as defined by 11C-choline PET/CT. Kaplan–Meier analysis showed that 11C-choline PET/CT could successfully distinguish the three groups of patients defined in their stage according to the 11C-choline uptake, i.e.: (1) patients with pathological 11C-choline uptake in the skeleton (M1b) or in retroperitoneal lymph nodes (M1a), (2) patients with pathological 11C-choline uptake in pelvic lymph nodes (N1 M0) or in the prostate bed (N0), and (3) patients with negative 11C-choline PET/CT (log-rank, chi-square = 27.4; P < 0.001) (Fig. 3). Median survival was achieved only in M1b/M1a patients (6.2 years, 95% CI, 2.6–9.8 years). In the multivariate analysis, statistical significance was obtained only by 11C-choline PET/CT coded according to the three AJCC-based groups (P = 0.010).
Kaplan–Meier PCa-specific survival probability curves in patients with negative 11C-choline PET/CT (PET/CT-), in patients with positive 11C-choline PET/CT suggestive of local recurrence or pelvic lymph node disease (PET/CT+, N0 and N1 M0, respectively) and in patients with positive 11C-choline PET/CT suggestive of retroperitoneal lymph node disease or bone metastases (PET/CT+, M1a and M1b, respectively)
At least one standard of care procedure was available in 139/210 patients (66%). Specifically, 5/136 patients (4%) had positive bone scintigraphy, 5/136 patients (4%) had positive abdominal-pelvic contrast-enhanced CT, 22/117 patients (19%) had positive abdominal-pelvic multiparametric magnetic resonance, and 12/127 (9%) patients had positive ultrasonography-guided prostate bed or lymph node biopsy. Since some patients had lesions in different anatomical sites, standard of care procedures were positive in 31/139 patients (22%). Among patients with negative standard of care procedures (n = 108), Kaplan–Meier analysis showed that median PCa-specific survival was 4.6 years (95% CI 2.4–20.6) in patients with positive 11C-choline PET/CT (n = 12), while median PCa-specific survival was not achieved in patients with negative 11C-choline PET/CT (n = 96) (log-rank, chi-square = 6.6, P = 0.010).
Since PCa patients treated with anti-androgenic therapy (ADT) were combined to patients not treated with ADT to increase the statistical power, another Cox regression analysis was performed where the variables 11C-choline PET/CT, treatment with ADT at the time of PET/CT, and their interaction were entered. Statistical significance was obtained for the first two variables (P = 0.003 and P = 0.040), but not for their interaction (P = 0.203), indicating that the results were not significantly biased by the mixture of the two clinically different populations. The association between ADT and positive PET/CT (see also Table 1) is a well-replicated finding attributed to the higher number of risk factors or to the more aggressive disease in patients receiving ADT [5, 36, 37].
Discussion
PET/CT with radiolabeled choline has drastically improved imaging of PCa in the last 20 years [37, 38]. This technique has been shown to be useful in different clinical contexts, primarily for restaging patients with biochemical failure [1,2,3,4,5,6,7,8,9], for initial staging of newly diagnosed high-risk PCa patients [10, 11], and to guide salvage radiotherapy [12,13,14,15]. In patients with biochemical failure after radical prostatectomy, PET/CT with radioactive choline predicts PCa-specific survival, and its prognostic power is greater than any other traditional biochemical or pathological risk factor [30, 31].
In spite of these multiple favorable features, during these years it became evident that PET/CT with radiolabeled choline was affected by an important limit, i.e., the positive detection rate in patients with biochemical failure after radical prostatectomy is relatively low for low PSA values, either PSA < 1 ng/ml or PSA < 1.5 ng/ml, according to the study design. Most studies in these intervals reported positive detection rates ranging between about 20% and an optimistic 45% [1, 4, 6, 19, 21,22,23, 39, 40]. Studies reported even lower detection rates (11%) in cases of particular inclusion criteria, such as absence of macroscopic disease on conventional imaging [4]. Studies agreed that, also in this low PSA interval, the positive detection rate of PET/CT can be increased by preferably selecting patients with either short PSA doubling time or high PSA velocity [4, 19, 22, 39, 40]; this is, however, impractical for some physicians. This weakness of PET/CT with radiolabeled choline is particularly dismaying considering that it is for low PSA values that the disease burden is expected to be less and the interest of clinicians is highest. Indeed, the European Association of Urology endorses the use of PET/CT with radiolabeled choline for PSA between 1 ng/ml and 2 ng/ml, but not for PSA < 1 ng/ml [41].
The failure of radiolabeled choline to completely satisfy this clinical demand prompted the search for new tracers. Among these, 68Ga-PSMA-11 (also known as 68Ga-HBED-CC, Glu-urea-Lys(Ahx)-HBED-CC, or 68Ga-PSMA-HBED-CC), often abbreviated as 68Ga-PSMA, represents the most promising tracer for PCa imaging [28, 29]. Comparative studies have consistently reported higher positive detection rate of PET/CT with 68Ga-PSMA compared to PET/CT with radiolabeled choline and differences were noteworthy for PSA < 1 ng/ml [25, 26]. However, there is currently no PET PSMA tracer with FDA/EMA approval, and in many countries the use of 68Ga-PSMA is still restricted by national legislatory rules so that, until formal approval is granted, 68Ga-PSMA can only be used only in experimental clinical trials. Therefore, while on one hand is reasonable to expect that in the very short term radiolabeled choline will still be the main tracer for PCa imaging in many centers, on the other hand PSMA PET agents are expected to replace radiolabeled choline as soon as FDA/EMA approval is obtained.
The results of our current study appear therefore particularly important: even though the positive detection rate of PET/CT with radioactive choline for PSA < 1 ng/ml is low (20.5% in our study), PET/CT findings do have prognostic value also in this narrow PSA interval, and therefore they require proper clinical management. In two retrospective studies with median PSA of 3.4 ng/ml [42] and 2.3 ng/ml [43], PET/CT with radiolabeled choline significantly influenced the clinical management of PCa patients in almost 50% of the cases. Therefore, use of PET/CT with radiolabeled choline for low PSA values requires some trade-off between high rate of false negative scans and good clinical management of positive patients. Moreover, we have shown that the prognostic information of 11C-choline PET/CT is maintained also in patients that have no evidence of disease in standard of care diagnostic procedures. These patients are definitely a subgroup of patients in whom 11C-choline PET/CT plays a critical role for imaging the site of relapse of disease and guiding further therapeutic options [4].
In the two survival studies that our group had previously carried out in two PCa populations not selected on the basis of their PSA value, median PSA was up to 1.82 ng/ml and highest PSA was up to 48.6 ng/ml [30, 31]. In the present study, median and maximum PSA were 0.54 ng/ml and 0.99 ng/ml respectively. Similarly to what we found in the two cited studies, also in the present investigation 11C-choline PET/CT was the only variable that reached statistical significance at multivariate analysis. To the best of our knowledge, the current study represents the first investigation assessing PCa-specific survival with 11C-choline PET/CT in PCa patients treated with radical prostatectomy and experiencing biochemical failure restricted to patients with PSA < 1 ng/ml.
To assess the robustness of our results, we also assessed survival according to the TNM classification of the AJCC, assuming 11C-choline PET/CT as gold standard for identification of disease. Kaplan–Meier analysis showed that 11C-choline PET/CT could successfully distinguish three groups of patients defined in their stage according to the 11C-choline uptake: (1) patients with pathological 11C-choline uptake in the skeleton (M1b) or in retroperitoneal lymph nodes (M1a), (2) patients with pathological 11C-choline uptake in pelvic lymph nodes (N1 M0) or in the prostate bed (N0), and (3) patients with negative 11C-choline PET/CT. The group including patients with skeletal metastases had shorter survival in comparison to patients with PET/CT findings suggestive of pelvic lymph node metastases or local recurrence, consistent with the fact that skeletal metastases represent the primary source of morbidity and mortality in PCa-patients. Overall, these results indirectly support an acceptable clinical accuracy of the technique [37, 44]. Results also were not sensitive to the definition of survival time, because very similar findings were obtained using the interval from prostatectomy and the interval from PET/CT.
Conclusions
In summary, in this group of PCa patients with biochemical failure after radical prostatectomy and PSA < 1 ng/ml, 11C-choline PET/CT has a positive detection rate of 20.5% and predicts PCa-specific survival. Tracers with higher positive detection rate are desirable for the clinical routine. However, until such tracers become more widely available, PET/CT with radiolabeled choline might be more broadly used in this low PSA range for clinical studies.
References
Castellucci P, Fuccio C, Nanni C, Santi I, Rizzello A, Lodi F, et al. Influence of trigger PSA and PSA kinetics on 11C-Choline PET/CT detection rate in patients with biochemical relapse after radical prostatectomy. J Nucl Med. 2009;50:1394–400.
Evangelista L, Zattoni F, Guttilla A, Saladini G, Colletti PM, Rubello D. Choline PET or PET/CT and biochemical relapse of prostate cancer: a systematic review and meta-analysis. Clin Nucl Med. 2013;38:305–14.
Fanti S, Minozzi S, Castellucci P, Balduzzi S, Herrmann K, Krause BJ, et al. PET/CT with (11)C-choline for evaluation of prostate cancer patients with biochemical recurrence: meta-analysis and critical review of available data. Eur J Nucl Med Mol Imaging. 2016;43:55–69.
Giovacchini G, Picchio M, Briganti A, Cozzarini C, Scattoni V, Salonia A, et al. [11C]Choline positron emission tomography/computerized tomography to restage prostate cancer cases with biochemical failure after radical prostatectomy and no disease evidence on conventional imaging. J Urol. 2010;184:938–43.
Giovacchini G, Picchio M, Coradeschi E, Bettinardi V, Gianolli L, Scattoni V, et al. Predictive factors of [(11)C]choline PET/CT in patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2010;37:301–9.
Krause BJ, Souvatzoglou M, Tuncel M, Herrmann K, Buck AK, Praus C, et al. The detection rate of [11C]choline-PET/CT depends on the serum PSA-value in patients with biochemical recurrence of prostate cancer. Eur J Nucl Med Mol Imaging. 2008;35:18–23.
Mapelli P, Incerti E, Ceci F, Castellucci P, Fanti S, Picchio M. 11C- or 18F-choline PET/CT for imaging evaluation of biochemical recurrence of prostate cancer. J Nucl Med. 2016;57:43S–8S.
Picchio M, Messa C, Landoni C, Gianolli L, Sironi S, Brioschi M, et al. Value of [11C]choline-positron emission tomography for re-staging prostate cancer: a comparison with [18F]fluorodeoxyglucose-positron emission tomography. J Urol. 2003;169:1337–40.
Umbehr MH, Muntener M, Hany T, Sulser T, Bachmann LM. The role of 11C-choline and 18F-fluorocholine positron emission tomography (PET) and PET/CT in prostate cancer: a systematic review and meta-analysis. Eur Urol. 2013;64:106–17.
Beheshti M, Imamovic L, Broinger G, Vali R, Waldenberger P, Stoiber F, et al. 18F choline PET/CT in the preoperative staging of prostate cancer in patients with intermediate or high risk of extracapsular disease: a prospective study of 130 patients. Radiology. 2010;254:925–33.
Evangelista L, Guttilla A, Zattoni F, Muzzio PC. Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate- to high-risk prostate cancer: a systematic literature review and meta-analysis. Eur Urol. 2013;63:1040–8.
Grosu AL, Weirich G, Wendl C, Prokic V, Kirste S, Geinitz H, et al. 11C-choline PET/pathology image coregistration in primary localized prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:2242–8.
Incerti E, Fodor A, Mapelli P, Fiorino C, Alongi P, Kirienko M, et al. Radiation treatment of lymph node recurrence from prostate cancer: is 11C-choline PET/CT predictive of survival outcomes? J Nucl Med. 2015;56:1836–42.
Picchio M, Berardi G, Fodor A, Busnardo E, Crivellaro C, Giovacchini G, et al. (11)C-Choline PET/CT as a guide to radiation treatment planning of lymph-node relapses in prostate cancer patients. Eur J Nucl Med Mol Imaging. 2014;41:1270–9.
Schwarzenbock SM, Kurth J, Gocke C, Kuhnt T, Hildebrandt G. Krause BJ role of choline PET/CT in guiding target volume delineation for irradiation of prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40(Suppl 1):S28–35.
De Giorgi U, Caroli P, Scarpi E, Conteduca V, Burgio SL, Menna C, et al. (18)F-Fluorocholine PET/CT for early response assessment in patients with metastatic castration-resistant prostate cancer treated with enzalutamide. Eur J Nucl Med Mol Imaging. 2015;42:1276–83.
Ceci F, Castellucci P, Graziani T, Schiavina R, Renzi R, Borghesi M, et al. (11)C-Choline PET/CT in castration-resistant prostate cancer patients treated with docetaxel. Eur J Nucl Med Mol Imaging. 2016;43:84–91.
Schwarzenbock SM, Eiber M, Kundt G, Retz M, Sakretz M, Kurth J, et al. Prospective evaluation of [(11)C]Choline PET/CT in therapy response assessment of standardized docetaxel first-line chemotherapy in patients with advanced castration refractory prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43:2105–13.
Castellucci P, Fuccio C, Rubello D, Schiavina R, Santi I, Nanni C, et al. Is there a role for (11)C-choline PET/CT in the early detection of metastatic disease in surgically treated prostate cancer patients with a mild PSA increase < 1.5 ng/ml? Eur J Nucl Med Mol Imaging. 2011;38:55–63.
Chiaravalloti A, Di Biagio D, Tavolozza M, Calabria F, Schillaci O. PET/CT with (18)F-choline after radical prostatectomy in patients with PSA ≤ 2 ng/ml. Can PSA velocity and PSA doubling time help in patient selection? Eur J Nucl Med Mol Imaging. 2016;43:1418–24.
Graziani T, Ceci F, Castellucci P, Polverari G, Lima GM, Lodi F, et al. (11)C-Choline PET/CT for restaging prostate cancer. Results from 4,426 scans in a single-centre patient series. Eur J Nucl Med Mol Imaging. 2016;43:1971–9.
Schillaci O, Calabria F, Tavolozza M, Caracciolo CR, Finazzi Agro E, Miano R, et al. Influence of PSA, PSA velocity and PSA doubling time on contrast-enhanced 18F-choline PET/CT detection rate in patients with rising PSA after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2012;39:589–96.
Vees H, Buchegger F, Albrecht S, Khan H, Husarik D, Zaidi H, et al. 18F-choline and/or 11C-acetate positron emission tomography: detection of residual or progressive subclinical disease at very low prostate-specific antigen values (< 1 ng/ml) after radical prostatectomy. BJU Int. 2007;99:1415–20.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent—update 2013. Eur Urol. 2014;65:124–37.
Afshar-Oromieh A, Zechmann CM, Malcher A, Eder M, Eisenhut M, Linhart HG, et al. Comparison of PET imaging with a (68)Ga-labelled PSMA ligand and (18)F-choline-based PET/CT for the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2014;41:11–20.
Morigi JJ, Stricker PD, van Leeuwen PJ, Tang R, Ho B, Nguyen Q, et al. Prospective comparison of 18F-Fluoromethylcholine versus 68Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J Nucl Med. 2015;56:1185–90.
Schwenck J, Rempp H, Reischl G, Kruck S, Stenzl A, Nikolaou K, et al. Comparison of 68Ga-labelled PSMA-11 and 11C-choline in the detection of prostate cancer metastases by PET/CT. Eur J Nucl Med Mol Imaging. 2017;44:92–101.
Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, et al. Sensitivity, specificity, and predictors of positive 68Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;70:926–37.
von Eyben FE, Picchio M, von Eyben R, Rhee H. Bauman G (68)Ga-labeled prostate-specific membrane antigen ligand positron emission tomography/computed tomography for prostate cancer: a systematic review and meta-analysis. Eur Urol Focus. 2018;4:686–93.
Giovacchini G, Incerti E, Mapelli P, Kirienko M, Briganti A, Gandaglia G, et al. [11C]Choline PET/CT predicts survival in hormone-naive prostate cancer patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2015;42:877–84.
Giovacchini G, Picchio M, Garcia-Parra R, Briganti A, Abdollah F, Gianolli L, et al. 11C-Choline PET/CT predicts prostate cancer-specific survival in patients with biochemical failure during androgen-deprivation therapy. J Nucl Med. 2014;55:233–41.
Kwee SA, Lim J, Watanabe A, Kromer-Baker K, Coel MN. Prognosis related to metastatic burden measured by (18)F-Fluorocholine PET/CT in castration-resistant prostate cancer. J Nucl Med. 2014;55:905–10.
Caroli P, De Giorgi U, Scarpi E, Fantini L, Moretti A, Galassi R, et al. Prognostic value of 18F-choline PET/CT metabolic parameters in patients with metastatic castration-resistant prostate cancer treated with abiraterone or enzalutamide. Eur J Nucl Med Mol Imaging. 2018;45:348–54.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Death in patients with recurrent prostate cancer after radical prostatectomy: prostate-specific antigen doubling time subgroups and their associated contributions to all-cause mortality. J Clin Oncol. 2007;25:1765–71.
Zhou P, Chen MH, McLeod D, Carroll PR, Moul JW, D’Amico AV. Predictors of prostate cancer-specific mortality after radical prostatectomy or radiation therapy. J Clin Oncol. 2005;23:6992–8.
Ceci F, Castellucci P, Mamede M, Schiavina R, Rubello D, Fuccio C, et al. (11)C-Choline PET/CT in patients with hormone-resistant prostate cancer showing biochemical relapse after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2013;40:149–55.
Giovacchini G, Giovannini E, Leoncini R, Riondato M, Ciarmiello A. PET and PET/CT with radiolabeled choline in prostate cancer: a critical reappraisal of 20 years of clinical studies. Eur J Nucl Med Mol Imaging. 2017;44:1751–76.
Chiti A, Picchio M. The rising PET: the increasing use of choline PET/CT in prostate cancer. Eur J Nucl Med Mol Imaging. 2011;38:53–4.
Giovacchini G, Picchio M, Garcia-Parra R, Mapelli P, Briganti A, Montorsi F, et al. [11C]choline positron emission tomography/computerized tomography for early detection of prostate cancer recurrence in patients with low increasing prostate specific antigen. J Urol. 2013;189:105–10.
Giovacchini G, Picchio M, Scattoni V, Garcia Parra R, Briganti A, Gianolli L, et al. PSA doubling time for prediction of [(11)C]choline PET/CT findings in prostate cancer patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2010;37:1106–16.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014;65:467–79.
Soyka JD, Muster MA, Schmid DT, Seifert B, Schick U, Miralbell R, et al. Clinical impact of 18F-choline PET/CT in patients with recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2012;39:936–43.
Ceci F, Herrmann K, Castellucci P, Graziani T, Bluemel C, Schiavina R, et al. Impact of 11C-choline PET/CT on clinical decision making in recurrent prostate cancer: results from a retrospective two-centre trial. Eur J Nucl Med Mol Imaging. 2014;41:2222–31.
Fanti S, Lalumera E. Of standard of reference and accuracy: the problem of truth in imaging. Eur J Nucl Med Mol Imaging. 2016;43:52–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest and no research support from funding agencies or industry.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea Ciarmiello and Maria Picchio are Co-Last Author
Rights and permissions
About this article
Cite this article
Giovacchini, G., Guglielmo, P., Mapelli, P. et al. 11C-choline PET/CT predicts survival in prostate cancer patients with PSA < 1 NG/ml. Eur J Nucl Med Mol Imaging 46, 921–929 (2019). https://doi.org/10.1007/s00259-018-4253-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4253-3