Abstract
Purpose
To evaluate 11C-choline PET/CT as a diagnostic tool for restaging prostate cancer (PCa), in a large, homogeneous and clinically relevant population of patients with biochemical recurrence (BCR) of PCa after primary therapy. The secondary aim was to assess the best timing for performing 11C-choline PET/CT during BCR.
Methods
We retrospectively analysed 9,632 11C-choline PET/CT scans performed in our institution for restaging PCa from January 2007 to June 2015. The inclusion criteria were: (1) proven PCa radically treated with radical prostatectomy (RP) or with primary external beam radiotherapy (EBRT); (2) PSA serum values available; (3) proven BCR (PSA >0.2 ng/mL after RP or PSA >2 ng/mL above the nadir after primary EBRT with rising PSA levels). Finally, 3,203 patients with recurrent PCa matching all the inclusion criteria were retrospectively enrolled and 4,426 scans were analysed.
Results
Overall, 52.8 % of the 11C-choline PET/CT scans (2,337/4,426) and 54.8 % of the patients (1,755/3,203) were positive. In 29.4 % of the scans, at least one distant finding was observed. The mean and median PSA values were, respectively, 4.9 and 2.1 ng/mL at the time of the scan (range 0.2 – 50 ng/mL). In our series, 995 scans were performed in patients with PSA levels between 1 and 2 ng/mL. In this subpopulation the positivity rate in the 995 scans was 44.7 %, with an incidence of distant findings of 19.2 % and an incidence of oligometastatic disease (one to three lesions) of 37.7 %. The absolute PSA value at the time of the scan and ongoing androgen deprivation therapy were associated with an increased probability of a positive 11C-choline PET/CT scan (p < 0.0001). In the ROC analysis, a PSA value of 1.16 ng/mL was the optimal cut-off value. In patients with a PSA value <1.16 ng/mL, 26.8 % of 1,426 11C-choline PET/CT scans were positive, with oligometastatic disease in 84.7 % of positive scans.
Conclusion
In a large cohort of patients, the feasibility of 11C-choline PET/CT for detecting the sites of metastatic disease in PCa patients with BCR was confirmed. The PSA level was the main predictor of a positive scan with 1.16 ng/mL as the optimal cut-off value. In the majority of positive scans oligometastatic disease, potentially treatable with salvage therapies, was observed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common solid neoplasm in men and the third leading cause of cancer-related death in men in Western Europe and the US [1, 2]. Although primary treatment of clinically localized PCa is associated with excellent oncological results, up to half the patients treated with radical prostatectomy (RP) or external beam radiotherapy (EBRT) experience biochemical recurrence (BCR) during follow-up [3–7]. Several tools evaluating numerous clinical and pathological parameters such as prostate-specific antigen (PSA) kinetics (such as doubling time and velocity), pathological Gleason score (GS), pathological T and N stage are now available and used by physicians to assess the probability of harbouring local or systemic recurrence after RP or EBRT [8–10]. These models are characterized by relatively good accuracy in distinguishing between local and distant relapse, but they are not able to provide precise and individual information about the site of relapse (e.g. visceral vs. bone metastases, pelvic vs. extrapelvic lesions) and/or the number of metastases. Therefore, clinicians are currently not able to target individualized salvage therapies according to the information provided by these tools only.
Conventional imaging, including CT, bone scintigraphy and MRI are characterized by low sensitivity in the detection of distant lesions of recurrent PCa [8]. Thus, such patients are generally referred for salvage radiotherapy to the prostate bed or systemic androgen deprivation therapy (ADT) when local or systemic relapse, respectively, is suspected [2]. Metastasis-targeted therapy might play a role in the management of these patients [11, 12] if an imaging modality able to accurately define site(s) of metastases is available. In the last decade, 11C-choline and/or 18F-choline PET/CT has been shown to perform better than conventional imaging in restaging patients with PCa after BCR [10, 13]. Nonetheless, choline PET/CT still has relatively low sensitivity, especially in patients with low PSA levels at the time of imaging [13–15]. Unfortunately, to obtain the best chance of cure in patients with PCa recurrence salvage treatment should be initiated when the PSA level is low [16–18]. Novel agents have been recently proposed to investigate PCa, including 68Ga-labelled PSMA analogues [19–21].
The aim of this retrospective analysis was to evaluate the role of 11C-choline PET/CT as a diagnostic tool for restaging PCa in a large, homogeneous and clinically relevant population of patients with recurrent PCa and BCR after radical therapy. The secondary aim was to determine the best timing for performing 11C-choline PET/CT during BCR.
Materials and methods
Population characteristics
The clinical records of PCa patients who had undergone a 11C-choline PET/CT scan in our institution for BCR were retrospectively analysed. Between January 2007 and June 2015 a total of 9,632 11C-choline PET/CT scans were performed. The inclusion criteria of the present retrospective analysis were: (1) proven PCa treated with RP (with or without adjuvant EBRT or adjuvant ADT) or with primary EBRT (with or without adjuvant ADT); (2) PSA serum values from the time of the scan; (3) proven BCR with rising PSA levels (PSA >0.2 ng/mL after RP and/or RP with adjuvant EBRT, PSA ≥2 ng/mL above the nadir after primary EBRT). According to these criteria, 3,203 consecutive patients with recurrent PCa were retrospectively enrolled and 4,426 11C-choline PET/CT scans were evaluated. In 590 of the 3,203 patients enrolled more than one 11C-choline PET/CT had been performed (range two to four scans per-patient). Scans in patients referred to our centre for other indications (e.g. staging) and/or scans in patients without PSA values at the time of the scan were excluded from the analysis; thus 5,206 scans were excluded. Population characteristics are summarized in detail in Table 1. Data concerning some of the enrolled patients have already been used in other published studies from the same institution. This was not considered an exclusion criterion.
Radiopharmaceuticals and imaging protocol
11C-Choline was synthesized according to the solid-phase method described by Pascali et al. [22], as previously described in other studies from the same institution [13].
11C-Choline PET/CT was performed according to local standard operating procedures. In Bologna, all scans were obtained using a hybrid PET/CT scanner (Discovery LS, Discovery STE or Discovery 690; GE Medical Systems, Waukesha, WI). CT parameters were 120 kVp, 60 mA, 0.8 s per tube rotation, slice thickness 5 mm, pitch 1.5, and table speed 30 mm per rotation. CT images were used both for image fusion and for attenuation correction of emission data. The patients fasted for at least 6 h before PET scanning and received an intravenous injection of 370 – 555 MBq of 11C-choline. The PET/CT scan was started 3 – 5 min after radiotracer injection. Emission data were acquired for five or six bed positions from the mid-thigh to the base of the skull, taking 3 – 4 min for each bed position (in relation to body weight and volume). Contrast-enhanced CT was not performed.
Image analysis
All 11C-choline PET/CT images were analysed using commercially available software packages (GE or Siemens). PET images were assessed visually, using transaxial, sagittal and coronal displays, and interpreted in consensus by two nuclear medicine physicians (P.C. and F.C.) with more than 5 years experience in 11C-choline PET/CT reading and aware of the clinical data. Visual interpretation was the main criterion to reach the final diagnosis. Any uptake higher than the surrounding background activity that did not correlate with physiological tracer uptake was considered pathological and suspicious of malignancy. Symmetrical or faint/moderate uptake in the inguinal lymph nodes (LNs) has never been regarded as suspicious of malignancy, nor has symmetrical or faint uptake in the mediastinal LNs. In addition, all pathological lesions were analysed semiquantitatively by calculating the maximum standardized uptake value (SUVmax). The SUVmax calculations did not influence the final diagnosis, because a cut-off to distinguish malignant from benign uptake has not yet been established. In the case of doubtful lesions a third nuclear medicine physician (S.F.) was consulted and a final diagnosis was reached in consensus.
In a patient-based analysis, PET-positive lesions were classified as local lesions (prostate/prostate bed relapse), pelvic LNs (iliac and/or pararectal), distant LNs (retroperitoneal and/or above the iliac bifurcation), bone lesions and other visceral lesions (thoracic LNs, lung, liver). In a lesion-based analysis, all lesions were assessed separately. The analysis of multiple lesions in terms of SUVmax was performed both considering the four lesions with the highest SUVmax and considering four representative randomly selected lesions. Oligometastatic disease was defined as the presence of one to three lesions regardless of site. Multimetastatic disease was defined as the presence of four or more lesions. 11C-Choline PET/CT-positive findings were reported as “positivity rate” since in the majority of patients histological confirmation was not available or feasible.
Statistical analysis
The data are reported as means, standard deviations (SD), medians and ranges. The Mann-Whitney test was used to compare differences between continuous nonnormally distributed variables. The chi-squared test was used for categorical variables. Correlations between clinical and pathological features and 11C-choline PET/CT pathological findings were assessed using univariate and multivariate binary logistic regression analysis. The effective PSA level at the time of the scan (PSA-trigger) was coded as a continuous variable. According to EUA guidelines [2], other factors such as the type of primary intervention (PR vs. EBRT), GS (<7 vs. ≥7), T stage (<T3 vs. ≥T3), N stage (N0 vs. N1), M stage (M0 vs. M1), ongoing ADT (yes vs. no), age (<65 vs. ≥65 years), time from primary therapy to BCR (TTR, <12 vs. ≥12 months) were coded as categorical variables. Odds ratios (OR) computed by logistic regression, together with their 95 % confidence intervals (CIs), are reported. The regression coefficients of each variable are also provided. The Hosmer-Lemeshow test was used to assess the goodness of fit in the multivariate analysis. The performance of 11C-choline PET/CT in relation to the PSA levels at the time of the scans was assessed by receiver operating characteristic (ROC) curves generated by plotting sensitivity versus 1 − specificity. The best trigger PSA cut-off value for distinguishing between positive and negative 11C-choline PET/CT findings was determined using Youden’s index. All tests were two-sided. Statistical significance was assumed for p values less than 0.05. All statistical analyses were performed using SPSS statistical software package, version 21 (IBM Corp., Armonk, NY).
Results
Overall results
11C-Choline PET/CT was positive in 52.8 % of scans (2,337 of 4,426) and in 54.8 % of patients (1,755 of 3,203). The median PSA value at the time of the scan was 2.1 ng/mL (range 0.2 – 50 ng/mL). Table 2 shows the sites of positive findings detected on 11C-choline PET/CT. Of the positive scans, 57.1 % (29.4 % of all scans) showed at least one distant finding (extrapelvic LNs and/or bone lesions and/or other visceral lesion). 11C-choline PET/CT-positive patients showed significantly higher PSA levels (Mann-Whitney test) than 11C-choline PET/CT-negative patients (p < 0.0001); Table 3). No significant difference (p > 0.05) was observed in SUVmax between the different types of lesions in the analysis considering the four lesions with the highest SUVmax or in the analysis considering four representative lesions.
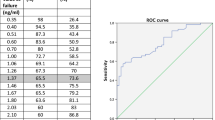
The analysis of the SUVmax values measured in this large patient series is summarized in Table 4. In both the univariate and the multivariate binary logistic regression analyses, PSA at the time of the scan and ongoing ADT were both associated with an increased probability of a positive 11C-choline PET/CT scan (PSA-trigger, OR 1.18, 95 % CI 1.15 – 1.20; p = 0.0001; ongoing ADT, OR 2.77, 95 % CI 2.21 – 3.48; p = 0.0001). Other factors included in the univariate and multivariate analyses (age, type of primary treatment, GS, TTR and TNM) were not significant predictors (p > 0.05). Univariate analysis demonstrated no change in the effect of the single variables. In the multivariate analysis, and the Hosmer-Lemeshow test showed no lack of fit in the model. In the ROC analysis (Fig. 1), a PSA value of 1.16 ng/mL was the optimal cut-off value for distinguishing between positive and negative 11C-choline PET/CT findings, with an area under the curve (AUC) of 0.739 (95 % CI 0.724 – 0.755).
Subpopulations
According to the indications proposed in the European Association of Urology (EAU) guidelines [2], 11C-choline PET/CT is suggested for restaging PCa patients with rising PSA levels between 1 and 2 ng/mL after primary therapy. In our patient series, 995 11C-choline PET/CT scans were performed in patients with a PSA value in this range at the time of the scan. The overall positivity rate in scans in patients with a PSA value in this range was 44.7 % (445 of 995), with an incidence of distant findings (extrapelvic LNs and/or bone lesions and/or visceral metastasis) of 19.2 % (42.9 % of positive scans). Oligometastatic disease (one to three lesions regardless of site) was observed in the 37.7 % of patients (84.3 % of positive scans).
According to the ROC analysis, the overall population was divided in two subpopulations with PSA levels lower and higher than the cut-off value. In the subpopulation of patients with PSA <1.16 ng/mL the overall detection rate calculated from 1,426 scans was 26.8 % (382 of 1,426 scans), with an incidence of distant findings of 12 % (44.7 % of positive scans). Oligometastatic disease was observed in the 22.7 % of patients (84.7 % of positive scans). In the subpopulation of patients with PSA >1.16 ng/mL the overall detection rate calculated from 3,000 scans was 65.1 % (1,954 of 3,000 scans), with an incidence of 32 % (49.1 % of positive scans). Oligometastatic disease was observed in the 37.5 % of patients (57.6 % of positive scans).
According to the statistical analysis, ongoing ADT was a significant predictor associated with an increased probability of a positive scan. In the 1,766 scans performed in patients with rising PSA values during ADT, the overall detection rate was 66.1 % (1,168 of 1,766 scans), with an incidence of distant findings of 43.7 % (66.1 % of positive scans). Oligometastatic disease was observed in the 45 % of patients (68.7 % of positive scans). These results are summarized in Table 5 and Fig. 2. PET/CT imaging in two example patients is presented In Figs. 3 and 4.
A 61-year-old patient with PCa treated in March 2009 with RP + pelvic lymph node dissection (GS 4 + 4, pT3N0Mx with initial PSA 8 ng/mL, PSA nadir after therapy 0.2 ng/mL). No adjuvant ADT was administrated. BCR occurred 19 months after RP. PSA at the time of the investigation was 5.2 ng/mL. 11C-Choline PET/CT images show focal intense uptake in the sixth hepatic segment. An ultrasound-guided biopsy was subsequently performed to confirm the presence of a metastatic lesion from PCa. a MIP image (arrow SUVmax 19.0); b PET, CT and fused images of the hepatic lesion
A 63-year-old patient with PCa treated in 2012 with RP + pelvic LN dissection (GS 5 + 4, T3N1Mx;,initial PSA 12 ng/mL). BCR occurred 12 months after RP. The patients was referred for ADT. Despite ADT during the previous 3 months, PSA increased to 1.9 ng/mL. The patient was referred for restaging with 11C-choline PET/CT. 11C-Choline PET/CT images show two osteolytic lesions with intense tracer uptake in L2 and in C3. a MIP image (dotted arrow L2 uptake, SUVmax 4.3; solid arrow C3 uptake, SUVmax 11.0); b PET, CT and fused images of the lesion in L2; c PET, CT and fused images of the lesion in L2
Discussion
During the last decade choline PET/CT has been widely used to restage PCa patients who experience BCR [23, 24]. EAU guidelines [2] suggest the use of choline PET/CT in patients with BCR and rising PSA levels between 1 and 2 ng/mL. This indication was proposed on the basis that to obtain the best chance of cure in patients with PCa recurrence salvage treatment should be initiated when the PSA level is low [25, 26] and that choline PET/CT shows relatively low sensitivity in patients with low PSA levels at the time of imaging [13–15]. Furthermore, metastasis-directed therapies with salvage radiotherapy or salvage pelvic LN dissection has shown promising results in terms of BCR-free survival and ADT-free survival [11, 12]. In this context, the availability of a diagnostic test capable of differentiating single metastatic, oligometastatic and multimetastatic disease at recurrence could be crucial and would substantially affect the clinical decision-making process. In our patient series, 995 11C-choline PET/CT scans were performed in patients with a PSA value in the range proposed by the EAU guidelines (1 – 2 ng/mL), with an overall positivity rate of 44.7 % of the 995 scans. In this large subpopulation, 11C-choline PET/CT showed the presence of oligometastatic disease eligible for treatment with salvage therapy, in 37.7.% of all the scans (375 of 995) and 84.3 % of the positive scans.
In daily clinical practice, choline PET/CT has been shown to be of value in patient management, leading to a change in the management decision in approximately 50 % of patients [27–29]. However, despite a wide bibliography [23, 26], there is still no consensus as to the proper indication for choline PET/CT in patients with BCR. Considering our results, we also determined the optimal cut-off value for predicting positive and negative scans in a statistically relevant ROC analysis performed on 4,426 scans. A PSA value of 1.16 ng/mL was found to be the optimal cut-off value. In patients with a PSA value lower than 1.16 ng/mL (1,426 scans), 11C-choline PET/CT showed the presence of oligometastatic disease in the 84.7 % of positive scans. On the contrary, in patients with a PSA value higher than 1.16 ng/mL (3,000 scans) limited disease (one to three lesions) was observed in the 57.6 % of positive scans. According to our results obtained in a large, homogeneous and clinically relevant population, 11C-choline PET/CT could have a role even in patients with low PSA levels during BCR, detecting the presence of a limited number of lesions treatable with salvage therapy in approximately one third of patients (Fig. 2). 11C-choline PET/CT could be suggested to select patients suitable for salvage therapy (according to the good performance for detecting oligometastatic disease in patients with low PSA levels observed in this study) since the best chance of cure in in patients with PCa recurrence is when the cancer burden is low.
Finally, we confirmed in our patient series previous results already presented in the literature [30, 31], confirming the high positivity rate of 11C-choline PET/CT in patients in whom the scan was performed for rising PSA values during ADT. 11C-Choline PET/CT was positive in 66 % of the enrolled patients during ADT. Moreover, 68 % of the positive scans showed oligometastatic disease. Although it was not an aim of our study, we suggest that using a metabolic radiopharmaceutical, such as choline in castrate-resistant patients could have a role as a predictor of therapy response [32, 33]. Indeed, despite the advent of new receptor radiotracers such as 68Ga-PSMA [34], it seems from a theoretical perspective more appropriate to use a metabolic tracer in the assessment of response to therapy.
The main limitation of the study was the lack of histological confirmation for the majority of lesions found. This approach was not always feasible in patients with recurrence. This is a limitation in many retrospective studies designed with similar aims. Accordingly, we report the results of our study only in terms of positivity rate. Finally, we note that in 18 % of our patient population more than one 11C-choline PET/CT scan had been performed, and this may have caused a selection bias. However, the objective of the analysis was to assess different parameters (including PSA at the time of the scan and ongoing ADT) and their association with the extension of the disease assessed by 11C-choline PET/CT. In this context, a scan-based analysis should be more appropriate and complete, and include a greater amount of data.
Conclusion
To the best of our knowledge, this study included the largest series of consecutive PCa patients with BCR (median PSA 2.1 ng/mL) investigated with 11C-choline PET/CT yet reported. The overall positivity rate of 11C-choline PET/CT calculated from 4,426 scans was 52.8 % and PSA was the main predictor of a positive scan with an optimal cut-off value of 1.16 ng/mL. In patients with a PSA value between 1 and 2 ng/mL, the positivity rate among the 995 scans was 44.7 %. In 84.3 % of the positive scans oligometastatic disease potentially treatable with salvage therapies was observed. According to our results, 11C-choline PET/CT could also be suggested in patients with low PSA levels since there is a reasonably high probability of detecting oligometastatic disease.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi:10.3322/caac.21332.
Mottet N, Bellmunt J, Briers E, van den Bergh RCN, Bolla M, van Casteren NJ, et al., Guidelines on prostate cancer. European Association of Urology; 2015.
Briganti A, Karnes RJ, Gandaglia G, Spahn M, Gontero P, Tosco L, et al. Natural history of surgically treated high-risk prostate cancer. Urol Oncol. 2015;33(4):163.e7–13.
Punnen S, Cooperberg MR, D’Amico AV, Karakiewicz PI, Moul JW, Scher HI, et al. Management of biochemical recurrence after primary treatment of prostate cancer: a systematic review of the literature. Eur Urol. 2013;64(6):905–15.
Freedland SJ, Presti Jr JC, Amling CL, Kane CJ, Aronson WJ, Dorey F, et al. Time trends in biochemical recurrence after radical prostatectomy: results of the SEARCH database. Urology. 2003;61(4):736–41.
Boorjian SA, Eastham JA, Graefen M, Guillonneau B, Karnes RJ, Moul JW. A critical analysis of the long-term impact of radical prostatectomy on cancer control and function outcomes. Eur Urol. 2012;61(4):664–75.
Khuntia D, Reddy CA, Mahadevan A, Klein EA, Kupelian PA. Recurrence-free survival rates after external-beam radiotherapy for patients with clinical T1-T3 prostate carcinoma in the prostate-specific antigen era: what should we expect? Cancer. 2004;100(6):1283–92.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014;65(2):467–79.
Kattan MW, Wheeler TM, Scardino PT. Postoperative nomogram for disease recurrence after radical prostatectomy for prostate cancer. J Clin Oncol. 1999;17(5):1499–507.
Choueiri TK, Dreicer R, Paciorek A, Carroll PR, Konety B. A model that predicts the probability of positive imaging in prostate cancer cases with biochemical failure after initial definitive local therapy. J Urol. 2008;179(3):906–10.
Suardi N, Gandaglia G, Gallina A, Di Trapani E, Scattoni V, Vizziello D. Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single institution series with a minimum follow-up of 5 years. Eur Urol. 2015;67(2):299–309.
Ost P, Bossi A, Decaestecker K, De Meerleer G, Giannarini G, Karnes RJ. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol. 2015;67(5):852–63.
Castellucci P, Fuccio C, Rubello D, Schiavina R, Santi I, Nanni C, et al. Is there a role for 11C-choline PET/CT in the early detection of metastatic disease in surgically treated prostate cancer patients with a mild PSA increase <1.5 ng/ml? Eur J Nucl Med Mol Imaging. 2011;38(1):55–63.
Picchio M, Mapelli P, Panebianco V, Castellucci P, Incerti E, Briganti A, et al. Imaging biomarkers in prostate cancer: role of PET/CT and MRI. Eur J Nucl Med Mol Imaging. 2015;42(4):644–55.
Mamede M, Ceci F, Castellucci P, Schiavina R, Fuccio C, Nanni C, et al. The role of 11C choline PET imaging in the early detection of recurrence in surgically treated prostate cancer patients with very low PSA level <0.5 ng/mL. Clin Nucl Med. 2013;38(9):e342–5.
Briganti A, Karnes RJ, Joniau S, Boorjian SA, Cozzarini C, Gandaglia G, et al. Prediction of outcome following early salvage radiotherapy among patients with biochemical recurrence after radical prostatectomy. Eur Urol. 2014;66(3):479–86.
Fossati N, Karnes RJ, Cozzarini C, Fiorino C, Gandaglia G, Joniau S, et al. Assessing the optimal timing for early salvage radiation therapy in patients with prostate-specific antigen rise after radical prostatectomy. Eur Urol. 2016;69(4):728–33.
Stephenson AJ, Scardino PT, Kattan MW, Pisansky TM, Slawin KM, Klein EA, et al. Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol. 2007;25(15):2035–41. Erratum in: J Clin Oncol. 2007;25(26):4153.
Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart HG, Hadaschik BA, et al. PET imaging with a [68Ga]gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40(4):486–95.
Morigi JJ, Stricker PD, van Leeuwen PJ, Tang R, Ho B, Nguyen Q, et al. Prospective comparison of 18F-fluoromethylcholine versus 68Ga-PSMA PET/CT in prostate cancer patients who have rising PSA after curative treatment and are being considered for targeted therapy. J Nucl Med. 2015;56(8):1185–90.
Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, et al. (68)Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging. 2015;42(8):1284–94.
Pascali C, Bogni A, Iwata R, Cambie M, Bombardieri E. 11C-Methylation on C18 Sep-Pak cartridge: a convenient way to produce [N-methyl-11C]choline. J Labelled Comp Radiopharm. 2000;49:195–203.
Fanti S, Minozzi S, Castellucci P, Balduzzi S, Herrmann K, Krause BJ, et al. PET/CT with (11)C-choline for evaluation of prostate cancer patients with biochemical recurrence: meta-analysis and critical review of available data. Eur J Nucl Med Mol Imaging. 2016;43(1):55–69.
Castellucci P, Fanti S. Prostate cancer: identifying sites of recurrence with choline-PET-CT imaging. Nat Rev Urol. 2015;12(3):134–5.
Castellucci P, Ceci F, Graziani T, Schiavina R, Brunocilla E, Mazzarotto R, et al. Early biochemical relapse after radical prostatectomy: which prostate cancer patients may benefit from a restaging 11C-Choline PET/CT scan before salvage radiation therapy? J Nucl Med. 2014;55(9):1424–9.
Evangelista L, Briganti A, Fanti S, Joniau S, Reske S, Schiavina R, et al. New clinical indications for 18F/11C-choline, new tracers for positron emission tomography and a promising hybrid device for prostate cancer staging: a systematic review of the literature. Eur Urol. 2016. doi:10.1016/j.eururo.2016.01.029
Ceci F, Herrmann K, Castellucci P, Graziani T, Bluemel C, Schiavina R, et al. Impact of 11C-choline PET/CT on clinical decision making in recurrent prostate cancer: results from a retrospective two-centre trial. Eur J Nucl Med Mol Imaging. 2014;41(12):2222–31.
Soyka JD, Muster MA, Schmid DT, Seifert B, Schick U, Miralbell R, et al. Clinical impact of 18F-choline PET/CT in patients with recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2012;39(6):936–43.
Goldstein J, Even-Sapir E, Ben-Haim S, Saad A, Spieler B, Davidson T, et al. Does choline PET/CT change the management of prostate cancer patients with biochemical failure? Am J Clin Oncol. 2014. doi:10.1097/COC.0000000000000139
Ceci F, Castellucci P, Mamede M, Schiavina R, Rubello D, Fuccio C, et al. (11)C-Choline PET/CT in patients with hormone-resistant prostate cancer showing biochemical relapse after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2013;40(2):149–55.
Ceci F, Castellucci P, Graziani T, Schiavina R, Renzi R, Borghesi M, et al. 11C-Choline PET/CT in castration-resistant prostate cancer patients treated with docetaxel. Eur J Nucl Med Mol Imaging. 2016;43(1):84–91.
Maines F, Caffo O, Donner D, Sperduti I, Bria E, Veccia A, et al. Serial (18)F-choline-PET imaging in patients receiving enzalutamide for metastatic castration-resistant prostate cancer: response assessment and imaging biomarkers. Future Oncol. 2016;12(3):333–42.
De Giorgi U, Caroli P, Burgio SL, Menna C, Conteduca V, Bianchi E, et al. Early outcome prediction on 18F-fluorocholine PET/CT in metastatic castration-resistant prostate cancer patients treated with abiraterone. Oncotarget. 2014;5(23):12448–58.
Meller B, Bremmer F, Sahlmann CO, Hijazi S, Bouter C, Trojan L, et al. Alterations in androgen deprivation enhanced prostate-specific membrane antigen (PSMA) expression in prostate cancer cells as a target for diagnostics and therapy. EJNMMI Res. 2015;5(1):66.
Acknowledgments
The authors thank the whole Nuclear Medicine Team for their invaluable collaboration and their daily contribution over recent years. The authors thank Dr. Joshua James Morigi (Nuclear Medicine, University of Bologna) for language revision.
Author contributions
Tiziano Graziani and Francesco Ceci contributed equally.
Data collection: Tiziano Graziani, Giulia Polverari and Giacomo Maria Lima.
Data analysis: Francesco Ceci and Tiziano Graziani.
Statistical analysis: Francesco Ceci.
Manuscript writing and editing: Francesco Ceci and Paolo Castellucci.
Final manuscript revision: Alessio Giuseppe Morganti, Andrea Ardizzoni, Riccardo Schiavina and Stefano Fanti.
Project supervision: Paolo Castellucci and Stefano Fanti.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Ethical approval
This study was performed according to the principles of the Declaration of Helsinki and its subsequent amendments.
Informed consent
Considering the retrospective design of the study, formal consent was not required.
Additional information
Tiziano Graziani and Francesco Ceci contributed equally to this work.
Rights and permissions
About this article
Cite this article
Graziani, T., Ceci, F., Castellucci, P. et al. 11C-Choline PET/CT for restaging prostate cancer. Results from 4,426 scans in a single-centre patient series. Eur J Nucl Med Mol Imaging 43, 1971–1979 (2016). https://doi.org/10.1007/s00259-016-3428-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-016-3428-z