Abstract
Objectives
To evaluate the diagnostic performance of 18F-choline PETCT in staging prostate cancer (PC) and whether the use of this imaging modality changes the therapeutic decision in patients previously staged by conventional imaging. The secondary aim was to determine the prognostic factors associated with positive choline PETCT findings in both detection of disseminated disease and in changes in the therapeutic indication.
Materials and methods
Multicentre, retrospective, observational study of 269 patients diagnosed with PC. Mean age was 69 ± 9.2 years. Of the 269 patients, 62 (23%) had high-risk localized PC (group 1), 118 (43.9%) biochemical failure after radical prostatectomy (group 2), and 89 (33.1%) biochemical failure after radiotherapy (group 3). None of the patients showed clear evidence of distant disease on computed tomography or bone scans. The following potential prognostic factors were assessed: PSA level at diagnosis; primary and secondary Gleason; Gleason score (GS); clinical and pathologic T and N stage; number of positive cylinders in the biopsy; presence of vascular or lymphatic invasion; status of surgical margins; androgen deprivation therapy (ADT); time to biochemical recurrence; and PSA, PSA doubling time (PSADT), and PSA velocity (PSAV) at failure. Univariate and multivariate analyses were performed, and receiver-operating curves calculated.
Results
The mean PSA by groups was, group 1: 31.22 ng/ml, group 2: 2.52 ng/ml and group 3: 5.85 ng/ml. The tumor detection rate with 18F-choline PETCT was 74% (group 1: 85.5%, group 2: 55.1% and group 3: 91%). Prognostic factors for positive 18F-choline PETCT were identified only in group 2: PSA at failure and PSADT. 18F-choline PETCT changed the therapeutic indication in 62.8% (group 1: 71%, group 2: 55.2% and group 3: 70.1%). The prognostic factors for a change in treatment were identified only in group 1: secondary Gleason ≤ 4 and GS ≤ 7 and in group 2: PSA at failure, PSA nadir after surgery and pathologic stage N0. 18F-choline PETCT identified lymph node and/or metastatic disease in 32.7% (group 1: 25.8%, group 2: 29.7% and group 3: 41.6%). Prognostic factors for detecting lymph node/metastasis were identified in the group 2: PSA failure ≥ 1.37 ng/ml and PSADT < 4 months and in the group 3: PSADT < 4.6 months and time to failure < 5 years.
Conclusion
These findings support the clinical use de 18F-choline PET-CT in staging high-risk patients with a secondary Gleason ≤ 4 and GS ≤ 7, in restaging patients with biochemical recurrence after RP if PSA at failure ≥ 1.37 ng/ml or PSADT ≤ 4 months and in patients with biochemical failure after RT, if PSADT ≤ 4.6 months and time to failure < 5 years, because it determines a change in the therapeutic indication.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PC) is the most common cancer and the second leading cause of cancer-related death in men [1]. Although close to 80% of men present with localized disease at diagnosis, the likelihood of developing metastatic disease depends on the initial risk group. Consequently, most clinical guidelines recommend performing computed tomography (CT) and bone scans (BS) as part of routine staging in patients with high-risk disease, in some intermediate-risk patients, and in biochemical failure. However, conventional staging (CT and BS) often fails to detect disseminated disease. For example, in cases with Gleason score (GS) < 8 or prostate-specific antigen (PSA) levels < 20 mg/ml, CT detects nodal involvement in less than 1% of patients. Similarly, the detection rate for bone metastases in patients with PSA < 10 ng/ml is only 2.3%.
Imaging modalities such as multiparametric ultrasound, multiparametric magnetic resonance imaging (MRI), and positron-emission tomography (PETCT) are now routinely used during all facets of PC management [2]. In patients with malignant solid tumors, perhaps the most widely used imaging technique is 18F-fluorodeoxyglucose (18F-FDG) PETCT. However, the sensitivity of this modality is lower in PC. PC cells are characterized by overexpression of choline kinase, which is responsible for the production of cell membrane components in which both acetate and choline are involved. Consequently, alternate radiotracers such as 11C-acetate, 11C- and 18F-choline have been developed. Several studies have found that choline PETCT has a greater sensitivity and specificity than 18F-FDG PETCT in PC [3, 4]. These alternative radiotracers have shown promising preliminary results in localizing recurrent disease [5].
Choline PETCT may provided valuable information in well-selected patients, including the following: patients with high-risk PC, patients with oligometastatic disease, and in patients who develop biochemical failure after local treatment [6].
In this context, the objectives of the present study were to evaluate the diagnostic performance of 18F-choline PETCT in staging prostate cancer and whether the use of this imaging modality changes the therapeutic decision in patients previously staged by conventional imaging. The secondary aim was to determine the prognostic factors associated with positive choline PETCT findings in both detection of disseminated disease and in changes in the therapeutic indication.
Material and methods
This was a multicentre, retrospective, observational study of 269 patients diagnosed and treated for PC. All patients underwent 18F-choline PETCT between January 2010 and November 2016. The mean patient age was 69 ± 9.2 years.
For the purposes of this study, the patients were classified into three distinct groups, as follows: group 1: 62 patients (23%) diagnosed with high-risk PC who underwent conventional staging, but without clear evidence of lymph node involvement or distant metastasis; group 2: 118 patients (43.9%) with biochemical failure after primary surgery (RP) ± radiotherapy (51 patients, 43.2% received RT post-surgery) defined by two consecutive PSA rises ≥ 0.2 ng/ml; and group 3: 89 patients (33.1%) with biochemical failure after primary radiotherapy (RT) defined by nadir of PSA + 2 ng/ml.
The following potential prognostic factors were obtained from the medical records: PSA level at diagnosis; primary and secondary Gleason; Gleason score (GS); clinical and pathologic T and N; number of positive cylinders in the biopsy; presence of vascular or lymphatic invasion; status of surgical margins; androgen deprivation therapy in the primary treatment (ADT); time to biochemical recurrence; and PSA, PSA doubling time (PSADT), and PSA velocity (PSAV) at failure.
Statistical analysis
A descriptive analysis was performed, including measures of central tendency and dispersion for the quantitative variables, and absolute and relative frequencies for the categorical variables. The Student’s t test and Chi-square test were used, respectively, to compare means and qualitative variables. Univariate and multivariate analyses were performed. Receiver-operating characteristic (ROC) curves were generated to analyze the quantitative variables found to be significant on the multivariate analysis. Statistical significance was set at p < 0.05. The SPSS statistical software package (v.22.0; IBM-SPSS; Chicago, IL; USA) was used for all statistical analyses.
The study was approved by the Clinical Research Ethics Committee at our institution and complies with all data protection regulations.
Results
The baseline characteristics of the study population are shown in Table 1.
Correlation between conventional staging and 18F-choline PET-CT
The mean PSA by groups, at the time of the PETCT, was: group 1: 31.22 ± 45.15 ng/ml, group 2: 2.52 ± 3.43 ng/ml and group 3: 5.85 ± 6.46 ng/ml. The tumor detection rate with 18F-choline PETCT by groups was, group 1: 85.5%, group 2: 55.1% and group 3: 91%.
The tumor detection rate with 18F-choline PETCT overall was 74% versus only 48.7% with conventional staging (p = 0.002). The findings of the 18F-choline PETCT study and conventional staging were only poorly well-correlated (Table 2), coinciding in only 107 cases (39.7%), a statistically significant difference (p = 0.004).
In conventional staging 16 patients (6%) had oligometastatic disease, but 18F-choline PETCT confirmed it only in 8 patients and identified previously undetected oligometastatic disease in 19 more patients (overall 27 patients (10.1%).
Only, in patients with biochemical failure after surgery several prognostic factors for positive 18F-choline PETCT were identified in univariate analysis: pathologic stage T3, perineural invasion, PSA at failure, PSADT and PSAV. On the multivariate analysis, the PSA at failure and PSADT maintained their significance (Table 3).
Change in the therapeutic indication
Overall, the 18F-choline PETCT finding changed the therapeutic indication in 169 patients (62.8%). By group, in 44 patients (71%) in group 1, 64 patients (55.2%) in group 2, and 61 patients (70.1%) in group 3.
On the univariate analysis, the significant prognostic factors for a change in the therapeutic indication based on the 18F-choline PETCT results are (Table 4): in high-risk: secondary Gleason ≤ 4 and GS ≤ 7, and in biochemical failure after surgery: pathologic stage N0, PSA nadir after surgery, and PSA at biochemical failure. On the multivariate analysis, the PSA at failure maintained their significance. In group 3 no prognostic factor was identified.
Lymph node involvement and/or metastatic disease
18F-choline PETCT identified lymph node and/or metastatic disease in a total of 88 patients (32.7%), distributed as follow: group 1: 16 patients (25.8%); group 2: 35 patients (29.7%); and group 3: 37 patients (41.6%).
In the group 1, no significant prognostic factors were found for the detection of nodal involvement or metastatic disease. In group 2, the following were significant prognostic factors on the univariate analysis (Table 5): pathologic stage ≥ pT3, ADT, PSA level at failure, PSADT and PSAV. On the multivariate analysis, the PSA at failure and PSADT remained significant.
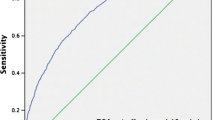
As Fig. 1 shows, the ROC curve for PSA failure—nodal/metastatic disease was significant. The sensitivity and specificity rates for the diagnosis of metastatic disease by 18F-choline PETCT were 65.5% and 73.6% for PSA at failure = 1.37 ng/ml.
The ROC curve for PSADT-nodal/metastatic disease was significant (AUC 0.763, typical error 0.056, p = 0.000). The sensitivity and specificity rates for diagnosing metastatic disease on the 18F choline PETCT were, respectively, 72.3% and 65.4% for PSADT = 4 months.
In group 3, the following variables were significant prognostic factors on the univariate analysis (Table 5): primary Gleason, GS, perineural invasion, ADT, PSADT, PSAV and time from completion of RT to failure. On the multivariate analysis, only PSADT remained statistically significant.
The ROC curve for PSADT-metastatic disease was significant (AUC 0.877, typical error 0.047, p = 0.000). The sensitivity and specificity for the diagnosis of metastases on choline PETCT were 87.1% and 64% for PSADT = 4.3 months.
The ROC curve for PSAV-metastatic disease was significant (AUC 0.886, typical error 0.055, p = 0.000). The sensitivity and specificity rates for detecting the presence of metastasis by choline PETCT according to the PSAV values were, respectively, 100% and 60% for PSAV = 0.22 ng/ml/month.
The ROC curve for time from completion of RT to failure-metastatic disease was significant (AUC 0.739, typical error 0.062, p = 0.001). The sensitivity and specificity for diagnosing metastatic disease on the choline PET-CT were, respectively, 78.1% and 60% in cases with a time to failure of 5 years.
Discussion
In the treatment of PC, correct staging is essential to select the most appropriate treatment. Conventional imaging scans are unable to detect metastatic disease in patients with low PSA levels. In addition, in patients with oligometastatic disease, these tests are insufficient to ensure that no additional lesions are present. In this context, we sought to determine if 18F-choline PETCT improves staging and changes the therapeutic indication. Our study has several limitations: retrospective design carried out in six centers with possible different interpretations of the PETCT findings. Our main findings showed that the results of the PETCT changed the therapeutic indication in 63% patients and identified lymph node and/or metastatic disease in 33% patients.
11C- or 18F-choline PETCT have only limited value in diagnosing primary PC due to their low sensitivity and specificity to differentiate between benign and malignant lesions in the prostate. MRI seems to be superior for the detection of primary PC [7]. For patients with intermediate or high-risk PC, commonly used imaging techniques such as CT and MRI have only a limited capacity to identify lymph node metastases because both modalities rely on lymph node size to identify metastases. Several meta-analyses [8, 9] have examined the detection rate of these imaging modalities for nodal metastases, but their use in routine clinical practice for N-staging of high-risk PC cannot be recommended because of limited sensitivity, especially for identifying small metastases and micrometastases [7].
The relative efficacy of 11C- or 18F-choline PETCT for M-staging in primary PC compared to other imaging modalities has been evaluated in several studies [10]. Both of these modalities can be recommended as alternatives to BS in patients with high-risk PC, especially given that studies have found that the results of choline PETCT imaging can change the management of these cases [6]. In our study, 18F-choline PETCT detected the presence of cancer in 85.5% of the high-risk patients; the detection rate for nodal and distant metastases was 25.8% leading to a change in therapeutic indication in 71% of these patients. We were unable to identify any prognostic factors for positive choline PETCT findings or nodal and metastasis detection. Probably, it is due to the small size of the sample. The high-risk group is only 62 patients and node/metastatic disease was detected in only 16 patients. However, in the high-risk group, the prognostic factors for a change in treatment were, secondary Gleason ≤ 4 and Gleason score ≤ 7, which could be the subgroup of patients in which PETCT would be indicated.
In patients with biochemically recurrent PC, both 11C- and 18F-choline PETCT are highly accurate in identifying nodal and distant metastases. The main advantage of PETCT is that it is a single, whole-body examination; however, its accuracy in detecting local recurrence is limited [11]. Evangelista et al. [6] demonstrated that 18F-choline PETCT was more sensitive and specific than BS and CT in the restaging setting. Those authors also found that MRI was more sensitive than choline PETCT, particularly in identifying local recurrences. MRI can detect local recurrence in prostatic bed, but its sensitivity in patients with PSA level < 0.5 ng/ml remains controversial, local recurrence was seen in 37% of men with PSA > 0.3 ng/ml vs 13% if PSA ≤ 0.3 ng/ml [12]. Couñago et al. [13] evaluated tumor recurrences after RP in 38 patients using both 18F-choline PETCT and MRI, finding no differences in the detection rates for local recurrence, nodal recurrence, or bone metastases. A systematic review and meta-analysis included 10 studies (1031 patients) evaluating the diagnostic performance of MRI for the detection of bone metastasis in patients with prostate cancer, newly diagnosed and treated, the median PSA were 2.7–31 ng/ml. The sensitivity and specificity of all studies were 96% and 98%, respectively [14].
A meta-analysis of choline PETCT for the management of PC concluded that choline PETCT changed the treatment indication in 41% of patients [9], in our study this happened in 62.8%. In most patients with PC, the goal of treatment is to administer a risk-adjusted, patient-specific treatment to maximize cancer control while minimizing adverse effects. Modern radiation techniques such as intensity-modulated radiotherapy and image-guide radiotherapy enable the application of high-dose radiation to the primary intraprostatic lesion, to a nodal recurrence isolated after RP, or to loco-regional nodal metastases. They also require more accurate imaging tools to reliably identify not only the primary lesion and potential nodal involvement, but more importantly, to reliably detect or rule out the presence of distant disease [15]. In this sense, choline PETCT can help to distinguish between localized, regional, and distant recurrence to better inform decision-making for improved disease management. Small areas of local recurrence may be amenable to salvage radiotherapy, while early detection of distant disease would enable the timely administration of ADT [16]. 18F-choline PETCT has a limited role in evaluating prostatic gland/fossa recurrence due to the physiological biodistribution of the radiopharmaceutical agent. However, in 70–90% of patients with PSA levels > 2 ng/ml (regardless of the GS), focal uptake is compatible with a true local recurrence [17]. In our study, 18F-choline PETCT confirmed local and loco-regional disease in 22.7% and 13.4% of patients, respectively.
The advent of 18F-choline PETCT has led to the identification of a new subgroup of metastatic PC patients: oligometastatic disease [18]. This subgroup could eventually be managed by treating all active lesions with local therapy, either surgery or ablative stereotactic body radiotherapy [19]. We found that choline PETCT identified oligometastatic disease in 10% in our sample, a finding that implied a change in the treatment indication.
One study involving 1000 patients who underwent 18F-choline PETCT after biochemical failure found that 645 of the PETCT were positive for recurrent disease. In addition, the choline PETCT findings were positive in 81% of patients with PSA ≥ 2 ng/mL, 43% with PSA from 1 to 2 ng/mL, and 31% with PSA ≤ 1 ng/mL while 78.8% of patients with positive PETCT findings had a GS > 7 [20]. In contrast, we found no correlation between GS and positive choline PETCT; however, we did find a highly significant correlation between the detection rate and PSA failure after surgery.
In our sample, findings from the 18F-choline PETCT study were positive in 55% and 91%, respectively, of patients with biochemical failure after RP or RT. Kwee et al. [21] evaluated 50 patients treated with RP or RT, with rising PSA levels at follow-up, finding that the 18F-choline PETCT was positive in 62% of patients overall. In that study, the sensitivity rate in patients with a PSA ≥ 1.1 ng/mL was 88%.
Fuccio et al. [22] retrospectively evaluated 123 consecutive-treated patients with biochemically recurrent PC after RP, finding that 11C-choline PETCT was positive in 34.1%. The mean PSA value in the 11C-choline PETCT negative patients was 2.7 ng/ml versus 3.8 ng/ml in those with a positive result. In our sample, the mean PSA value in the post-RP biochemical failure group was 0.94 ng/ml for those with a negative choline PETCT versus 3.72 ng/ml in those with a positive PETCT.
Choline PETCT identified nodal and/or metastatic involvement in 30% of the patients with biochemical failure after RP and the significant prognostic factors were: PSA failure ≥ 1.37 ng/ml and PSADT ≤ 4 months. Schillaci et al. [23] evaluated the influence of PSA, PSAV, and PSADT on 18F-choline PETCT in restaging patients with rising PSA after RP. The author to conclude that 18F-choline PETCT is recommended in patients with PSA > 2 ng/ml, PSADT ≤ 6 months and PSAV > 2 ng/ml per year.
Chiaravalloti et al. [24] investigated the performance of 18F-choline PETCT in 79 patients with biochemical failure after RP. Findings on the 18F-choline PETCT were positive in 55%. In patients with a PSADT ≤ 6 months the detection rate was 65%, and in patients with PSAV > 1 ng/ml/yr the rate was 67%.
Jadvar, conducted a study to summarize the findings of systematic reviews and meta-analyses, finding that the overall pooled detection rate for choline PETCT in restaging PC was 58%, increasing to 65% when PSADT was ≤ 6 months and to 71% and 77% when the PSAV was > 1 or > 2 ng/ml/yr, respectively [25].
In another study, Chondrogiannis et al. [26] performed 18F-choline PETCT to evaluate 46 patients with biochemical failure after RT, finding a positive detection rate in 80.4% of the sample, which increased in line with increase in the trigger PSA. The detection rate was 54.5% in patients with PSA levels between 1.0 and 2.0 ng/ml; 81% between 2.0 and 4.0 ng/ml; and 89% between 4–6 ng/ml, and 100% in patients with PSA > 6.0 ng/ml. In the overall series, patients with a negative PETCT had a mean PSA of 2.3 ng/ml vs 7.5 ng/ml in the positive PETCT group. Of the PETCT positive patients, 59% had local relapse confined to the prostatic bed while 22% presented lymph node and distant metastases. In contrast, in our study, the detection rate was 91% in patients with biochemical failure after RT, and the detection rate for nodal and distant metastases was 41.6%. The PSA level was not a prognostic factor; the only prognostic factors were: PSADT ≤ 4.6 months, PSAV 0.22 ng/ml/month, and time to failure < 5 years.
The 68 Ga-prostate-specific membrane antigen (68 Ga-PSMA) has been recently developed as a ligand in PETCT to detect the presence of PC. This technique is more effective in detecting metastases, nodal involvement, and recurrent PC than 18F-choline PETCT and CT. It is effective in patients with low PSA levels and is positively associated with rising PSA levels and tumor size [27]. Bluemel et al. [28] investigated the value of 68 Ga-PSMA PETCT in patients with biochemical recurrence but negative finding on 18F-choline PETCT, finding that this imaging modality detected recurrent disease in 43.8% of those patients. Detection rates were 28.6, 45.5, and 71.4%, respectively, for PSA levels ≥ 0.2 to < 1 ng/mL, 1 to 2 ng/mL, and > 2 ng/mL. Table 6 summarizes prostate specific antigen cut-off and detection rates of choline and 68 Ga-PSMA PETCT in the restaging setting [6]. The 68 Ga-PSMA is recommended for evaluating biochemical relapse after prostatectomy for the superiority over choline for PSA levels < 1 ng/ml, however, at this time in Spain we do not have availability to perform PSMA [29].
Conclusions
The tumor detection rate with 18F-choline PET-CT was 74%, detecting oligometastatic disease in 10.1%, lymph node/metastatic disease in 33%, and changed the therapeutic indication in 62.8% of the sample. Our findings support the clinical use de 18F-choline PET-CT in staging high-risk patients with a secondary Gleason ≤ 4 and GS ≤ 7, in restaging patients with biochemical recurrence after RP if PSA at failure ≥ 1.37 ng/ml or PSADT ≤ 4 months and in patients with biochemical failure after RT if PSADT ≤ 4.6 months and time to failure < 5 years, because it determines a change in the therapeutic indication.
References
Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014: cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29.
Sarkar S, Das S. A review of imaging methods for prostate cancer detection: supplementary issue: image and video acquisition and processing for clinical applications. Biomed Eng Comput Biol. 2016;7(s1):BECB.S34255.
García JR, Soler M, Blanch MA, Ramírez I, Riera E, Lozano P, et al. PET/TAC con 11C-colina y 18F-FDG en pacientes con elevación de PSA tras tratamiento radical de un cáncer de próstata. Rev Esp Med Nucl. 2009;28(3):95–100.
Zuazu JR, Rodríguez M, Mayans AR, Sansi AS, Bergera JJZ, Martínez-Monge R, et al. Valor de la PET en la recurrencia del cáncer de próstata con PSA 5 ng/ml. Actas Urol Esp. 2009;33(8):844–52.
Mottet N, Bellmunt J, Briers E, Bolla M, Bourke L, Cornford P, De Santis M, Henry AM, Joniau S, Lam TB, Mason MD, van der Poel HG, van der Kwast TH, Rouvière O, Wiegel T. Guidelines Associates: Arfi N, van den Bergh RCN, van den Broeck T, Cumberbatch M, Fossati N, Gross T, Lardas M, Liew M, Moldovan P, Schoots IG, Willemse PM. Prostate Cancer guidelines EAU 2017. http://uroweb.org/guideline/prostate-cancer/.
Evangelista L, Briganti A, Fanti S, Joniau S, Reske S, Schiavina R, et al. New clinical indications for 18 F/11 C-choline, new tracers for positron emission tomography and a promising hybrid device for prostate cancer staging: a systematic review of the literature. Eur Urol. 2016;70(1):161–75.
Nitsch S, Hakenberg OW, Heuschkel M, Drager D, Hildebrandt G, Krause BJ, et al. Evaluation of prostate cancer with 11C- and 18F-choline PET/CT: diagnosis and initial staging. J Nucl Med. 2016;57(Supplement_3):38S–42S.
Umbehr MH, Müntener M, Hany T, Sulser T, Bachmann LM. The role of 11C-choline and 18F-fluorocholine positron emission tomography (PET) and PET/CT in prostate cancer: a systematic review and meta-analysis. Eur Urol. 2013;64(1):106–17.
von Eyben FE, Kairemo K. Meta-analysis of 11C-choline and 18F-choline PET/CT for management of patients with prostate cancer. Nucl Med Commun. 2014;35(3):221–30.
Beheshti M, Rezaee A, Geinitz H, Loidl W, Pirich C, Langsteger W. Evaluation of prostate cancer bone metastases with 18F-NaF and 18F-fluorocholine PET/CT. J Nucl Med Off Publ Soc Nucl Med. 2016;57(Suppl 3):55S–60S.
Mapelli P, Incerti E, Ceci F, Castellucci P, Fanti S, Picchio M. 11C- or 18F-Choline PET/CT for imaging evaluation of biochemical recurrence of prostate cancer. J Nucl Med. 2016;57(Supplement_3):43S–8S.
Liauw SL, Pitroda SP, Eggener SE, Stadler WM, Pelizzari CA, Vannier MW, et al. Evaluation of the prostate bed for local recurrence after radical prostatectomy using endorectal magnetic resonance imaging. Int J Radiat Oncol. 2013;85(2):378–84.
Couñago F, Recio M, Maldonado A, Del Cerro E, Díaz-Gavela AA, Thuissard IJ, et al. Evaluation of tumor recurrences after radical prostatectomy using 18F-Choline PET/CT and 3T multiparametric MRI without endorectal coil: a single center experience. Cancer Imaging Off Publ Int Cancer Imaging Soc. 2016;16(1):42.
Woo S, Suh CH, Kim SY, Cho JY, Kim SH. Diagnostic performance of magnetic resonance imaging for the detection of bone metastasis in prostate cancer: a systematic review and meta-analysis. Eur Urol. 2018;73(1):81–91.
Rischke HC, Grosu AL. PET/CT imaging in prostate cancer: indications and perspectives for radiation therapy. In: Geinitz H, Roach III M, van As N, editors. Radiotherapy in prostate cancer. Berlin: Springer; 2014. p. 15–31. http://springerlink.bibliotecabuap.elogim.com/10.1007/174_2014_1007.
Leiblich A, Stevens D, Sooriakumaran P. The utility of molecular imaging in prostate cancer. Curr Urol Rep. 2016 Mar; 17(3). http://springerlink.bibliotecabuap.elogim.com/10.1007/s11934-015-0573-z.
Evangelista L, Cimitan M, Hodolič M, Baseric T, Fettich J, Borsatti E. The ability of 18F-choline PET/CT to identify local recurrence of prostate cancer. Abdom Imaging. 2015;40(8):3230–7.
Supiot S, Rio E, Pacteau V, Mauboussin M-H, Campion L, Pein F. OLIGOPELVIS—GETUG P07: a multicentre phase II trial of combined salvage radiotherapy and hormone therapy in oligometastatic pelvic node relapses of prostate cancer. BMC Cancer. 2015 Dec;15(1). http://bmccancer.biomedcentral.com/articles/10.1186/s12885-015-1579-0.
Pasqualetti F, Panichi M, Sainato A, Matteucci F, Galli L, Cocuzza P, et al. [18F]Choline PET/CT and stereotactic body radiotherapy on treatment decision making of oligometastatic prostate cancer patients: preliminary results. Radiat Oncol. 2016 Dec;11(1). http://www.ro-journal.com/content/11/1/9.
Cimitan M, Evangelista L, Hodolič M, Mariani G, Baseric T, Bodanza V, et al. Gleason score at diagnosis predicts the rate of detection of 18F-choline PET/CT performed when biochemical evidence indicates recurrence of prostate cancer: experience with 1,000 patients. J Nucl Med Off Publ Soc Nucl Med. 2015;56(2):209–15.
Kwee SA, Coel MN, Lim J. Detection of recurrent prostate cancer with 18F-fluorocholine PET/CT in relation to PSA level at the time of imaging. Ann Nucl Med. 2012;26(6):501–7.
Fuccio C, Castellucci P, Schiavina R, Guidalotti PL, Gavaruzzi G, Montini GC, et al. Role of 11C-choline PET/CT in the re-staging of prostate cancer patients with biochemical relapse and negative results at bone scintigraphy. Eur J Radiol. 2012;81(8):e893–6.
Schillaci O, Calabria F, Tavolozza M, Caracciolo CR, Agrò EF, Miano R, et al. Influence of PSA, PSA velocity and PSA doubling time on contrast-enhanced 18F-choline PET/CT detection rate in patients with rising PSA after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2012;39(4):589–96.
Chiaravalloti A, Di Biagio D, Tavolozza M, Calabria F, Schillaci O. PET/CT with 18F-choline after radical prostatectomy in patients with PSA ≤ 2 ng/ml. Can PSA velocity and PSA doubling time help in patient selection? Eur J Nucl Med Mol Imaging. 2016;43(8):1418–24.
Jadvar. Positron emission tomography in prostate cancer: summary of systematic reviews and meta-analyses. Tomography. 2015;1(1):18–22.
Chondrogiannis S, Marzola MC, Ferretti A, Maffione AM, Rampin L, Grassetto G, et al. Role of 18F-choline PET/CT in suspicion of relapse following definitive radiotherapy for prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40(9):1356–64.
Oliveira J, Gomes C, Faria D, Vieira T, Silva F, Vale J, et al. 68Ga-prostate-specific membrane antigen positron emission tomography/computed tomography for prostate cancer imaging: a narrative literature review. World J Nucl Med. 2017;16(1):3.
Bluemel C, Krebs M, Polat B, Linke F, Eiber M, Samnick S, et al. 68 Ga-PSMA-PET/CT in patients with biochemical prostate cancer recurrence and negative 18F-choline-PET/CT. Clin Nucl Med. 2016;41(7):515–21.
Couñago F, Artigas C, Sancho G, Gómez-Iturriaga A, Gómez-Caamaño A, Maldonado A, et al. PET/TC con 68 Ga-PSMA, importancia en la práctica hospitalaria. Visión del oncólogo radioterápico. Rev Esp Med Nucl E Imagen Mol. 2018 Aug. https://linkinghub.elsevier.com/retrieve/pii/S2253654X18301501.
Acknowledgements
The authors would also like to thank Bradley Londres for translating and editing the present document.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Samper Ots, P., Luis Cardo, A., Vallejo Ocaña, C. et al. Diagnostic performance of 18F-choline PET-CT in prostate cancer. Clin Transl Oncol 21, 766–773 (2019). https://doi.org/10.1007/s12094-018-1985-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-1985-2