Abstract
Purpose
Regadenoson, an A2A adenosine receptor pharmacologic stress agent for radionuclide myocardial perfusion imaging (MPI), is administered as a single, fixed dose. We studied the side effect profile of regadenoson combined with two types of low-level exercise, according to body mass index (BMI).
Methods
Three hundred and fifty-six patients (46.1% men, mean age 67.7±10.7 years, range 31–90 years) underwent regadenoson stress testing combined with low-level exercise. Subjects were classified according to BMI as normal, overweight, or obese, and the type of low-level exercise performed as walking on the treadmill (TE group, n=190) or forcefully swinging legs while sitting (SS group, n=166). Patients’ demographics, medical history, clinical symptoms during stress, changes in ECG, oxygen saturation (SatO2), systolic blood pressure (SBP), and heart rate (HR) were evaluated.
Results
Groups were comparable (p=ns) with regard to cardiovascular risks factors. The incidence of side effects was similar across BMI (p=ns), although the TE patients showed improved profiles over those with SS exercise, with a significantly lower incidence of flushing, dizziness and nausea/gastrointestinal discomfort (12.9% vs. 28.4%; 19.9% vs. 33.4%; 11.4% vs. 19.2%, respectively; all p<0.05).
Regarding the hemodynamic response, we did not observe significant changes in SBP and HR after regadenoson administration across BMI categories. Comparing the TE and SS groups, no significant changes were observed in SBP, but there was a higher increase in HR in the TE group (p<0.05).
Conclusions
Regadenoson in combination with low-level exercise is safe and well tolerated over a wide range of BMI, with TE exercise showing a better side effect profile than SS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity and overweight are global problems with increasing prevalence in most countries. The worldwide prevalence of obesity has more than doubled between 1980 and 2014. According to recent World Health Organization (WHO) estimates about 13% of the world’s adult population (11% of men and 15% of women) were obese in 2014 and 39% of adults aged 18 years and over (38% of men and 40% of women) were overweight [1]. Overweight and obesity can be measured and classified by body mass index (BMI, weight in kg/m2). Overweight adults have a BMI of 25.0 to 29.9 kg/m2 and obese adults have a BMI ≥ 30.0 kg/m2 [2].
Because obesity is an important risk factor for early and accelerated atherosclerotic cardiovascular disease [3,4,5], non-invasive imaging techniques such as radionuclide myocardium perfusion imaging (MPI) are increasingly used in these types of patients. Dynamic exercise is the method of choice for producing coronary hyperemia in patients who can achieve adequate exercise endpoints [6]. Pharmacologic stress agents [adenosine, adenosine 5′-triphosphate (ATP), dipyridamole, or regadenoson] induce coronary artery hyperemia [7] and are indicated in patients unable to perform adequate exercise due to medical constraints or physical limitations, such as obesity.
Adenosine is a nonspecific agonist of adenosine receptor subtypes (A1, A2A, A2B , and A3), although coronary dilation is caused by interaction with the A2A receptor present in the vascular wall. ATP, the parent compound of adenosine especially used in Japan [8], has a vasodilator effect due to its degradation to adenosine and, on the other hand, by the direct stimulation of P2 purinergic receptors by ATP itself [9]. The vasodilation produced by dipyridamole is based on increased levels of intrinsic adenosine by means of adenosine-deaminase inhibition. Both adenosine and dipyridamole require weight-based dosing and administration as a continuous infusion.
Regadenoson is a selective A2A adenosine receptor pharmacologic stress agent indicated for radionuclide MPI [8, 9]. It is administered as a single, fixed-dose (0.4 mg/5 mL) intravenous (iv) bolus. As it has greater affinity for the A2A receptor and much lower affinity for the other adenosine receptor subtypes, regadenoson has fewer side effects and is better tolerated by patients compared with adenosine or dypiridamole [10, 11], and it can be used in patients with COPD or asthma [12,13,14,15,16,17]. In addition, because it does not require dose calculations or pump delivery, regadenoson is easier to use.
Given the high frequency of obesity in patients with symptoms of heart disease, the aim of this study was to investigate the side effect profile of regadenoson combined with low-level exercise in patients with a wide range of body sizes, with a special focus on obese patients. On the other hand, we compare the profiles according to the type of low level exercise performed: walking on the treadmill (TE group) or swinging legs while sitting on a stretcher, sit and swing (SS group).
Methods
We carried out a prospective study in 356 European patients (46.1% men) with a mean age of 67.7 ± 10.7 years (range 31–90 years). Table 1 lists the patients’ demographic characteristics. All patients underwent a clinically indicated pharmacologic stress test with regadenoson combined with low-level exercise. Ethical approval was provided by the local Institutional Review Board. All patients gave their signed written informed consent.
Inclusion and exclusion criteria
Regadenoson was prescribed by the physician in charge of the patient’s myocardial test, without regard to this study. The exclusion criteria were as follows: (a) history of recent acute myocardial infarction, unstable angina or decompensated or inadequately controlled congestive heart failure; (b) history of sick sinus syndrome or greater than first degree AV block, except in patients with functional artificial pacemaker; (c) long QT syndrome; (d) current use of dipyridamole, aminophylline, or theophylline; (e) intake of methylxantine-containing foods and beverages prior to study; (f) patients with COPD or asthma were included in the study except if any of the following was present: active bronchoconstriction, wheezing, or requiring systemic corticosteroid therapy for control of bronchoconstrictive disease.
Study design
This was an observational, comparative study designed to reflect routine clinical practice. Evaluations were carried out by monitoring the patient during the day of drug administration following the standard clinical practice of our department. Detailed clinical and procedure data were collected prospectively and stored in a database. BMI was calculated using weight and height values recorded immediately before the test. Patients were categorized into the following three BMI classes according to World Health Organization standards: 1) normal weight (<25.0 kg/m2); 2) overweight (25.0–29.9 kg/m2); and 3) obese (≥30.0 kg/m2). BMI was treated as a categorical variable for all analyses.
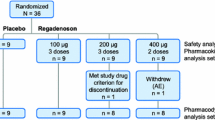
Patients were instructed to eat a light breakfast before the test. They underwent a 2-day pharmacologic stress combined with low-level exercise/rest protocol. Two types of low-level exercise were performed by patients: One set of patients (n = 190) walked on the treadmill (TE) at 2.7–3.5 km/h and 0° incline (2.3–2.7 METs), and the remaining patients (n = 166) who were unable to walk adequately on the treadmill due to lower extremity problems (claudication, hip, or knee prosthesis) performed an alternative type of low-level exercise such as forcefully swinging their legs while sitting on a stretcher (SS) [18].
Regadenoson was administered as a peripheral intravenous bolus (10 s) after 1.5 min of exercise immediately followed by a 5-mL saline flush. MPI radiopharmaceutical, 99mTc-sestamibi (n = 249) or 99mTc-tetrofosmin (n = 107), was injected approximately 30 s after starting regadenoson into the same catheter. The test ended after 4 min of exercise (Fig. 1).
Patients’ demographics, medical history, side effects, ECG, pulsioxymeter oxygen arterial saturation (SatO2), systolic blood pressure (SBP), and heart rate (HR) were evaluated. ECG monitoring continued during the procedure and for at least 10 min into recovery following regadenoson administration. Horizontal or down-sloping ST segment depression ≥1 mm was considered abnormal.
Symptoms during the stress procedure were recorded as reported by the patient, except flushing that was assessed by the nurse. We considered side effects all those effects appearing during stress and up to 2 h later. Patients’ SBP and HR were recorded as baseline (measures obtained immediately before starting the test) and maximum change (over the duration of the test) following regadenoson administration.
Data analysis
Continuous data were expressed as mean ± standard deviation (SD), and categorical variables were displayed with observed frequency and percentage. In the contrast between groups, categorical variables were compared using the Mantel-Haenszel Chi-square test, and continuous variables were compared with Kruskal-Wallis test, whereas the Wilcoxon-Z test was used to compare changes in SatO2. In all cases using two-side p-values with alpha < 0.05 level of significance; however, a Bonferroni correction was applied for multiple categorical comparisons.
Results
The baseline clinical characteristics of the study population have been described in the Table 1. There was a high prevalence of co-morbidities such as hypertension (80.2%), dyslipidemia (43.6%), diabetes (43.7%), smoking (15.6%), and known coronary artery disease (14.6%).
The presence of known coronary artery disease was not significantly different across BMI categories (15.4% in obese patients, 9.9% in overweight patients, 22.4% in normal weight patients; p = 0.19) neither between types of low-level exercise (16.5% in TE group vs. 12.2% in SS group; p = 0.26).
The study included 328 patients with pulmonary diseases, such as asthma and COPD (92.1%). Of these, 167 had COPD and 161 had asthma, 50.9% and 49.1%, respectively, and 11 of those patients had stable severe COPD, and one had severe persistent asthma (3.7%).
The largest proportion of patients were classified as obese (58.7%), followed by overweight (30.3%) and normal weight (10.9%). We observed a direct association between the increase in BMI and higher rates of co-morbidities, including hypertension, diabetes mellitus, and dyslipidemia.
Side effects
Comparison between types of low-level exercise (regardless of BMI)
Onset of side effects of both types of low-level exercise was immediately after dosage and reversal shortly after (5–10 min.).
Patients who performed TE exercise demonstrated an improved side effect profile over those with SS exercise (Table 2). We observed that flushing, dizziness, nausea and GI discomfort were more frequent in the SS group when compared to the TE group (p < 0.05). The rest of side effects were comparable between the TE and SS groups.
In a similar fashion, the number of patients with no side effects at all after regadenoson administration was higher in those who underwent a TE exercise.
Comparison across BMI categories
The frequency of each side effect after regadenoson administration in the TE patients (Fig. 2) was similar across BMI subgroups (p = ns), although linear trends were observed in some effects, such as a higher frequency of fatigue, chest pain, dizziness, and dry mouth in obese patients, and throat tightness, and headache in normal weight patients.
As in the TE group, the frequency of each side effect following regadenoson administration combined with SS exercise (Fig. 3) was similar across BMI classes (p = ns). However, the previous linear trends were not observed in this group.
Changes in ECG monitoring
No significant changes in ECG monitoring were observed across BMI categories (p = ns). Thus, one normal weight patient (0.03%), four overweight (0.04%), and four obese patients (0.02%) showed horizontal or down-sloping ST depression ≥1 mm in multiple leads.
Changes in SatO2
No decreases in SatO2 occurred following regadenoson administration for each BMI category (96.7% ± 0.2 vs. 97.4% ± 0.2 in obese patients; 96.7% ± 0.3 vs. 97.6 ± 0.3 in overweight patients; 97.3% ± 0.4 vs. 97.7% ± 0.6 in normal weight patients).
Hemodynamic response
When we studied the influence of the type of low-level exercise (regardless of the BMI category) (Table 3), no significant changes were observed in SBP between the TE and SS groups (5.2 ± 21 mmHg vs. 1.7 ± 22 mmHg, p = ns). However, HR changes between baseline and maximum value after dosing were significantly different between the TE and SS groups, with a higher increase in the TE group (36 ± 21 b.p.m. vs. 26 ± 19 b.p.m., p < 0.05).
According to the BMI categories, mean resting SBP of patients was significantly higher in obese patients when compared to overweight and normal weight patients (151.5 ± 24.7 mmHg vs. 140.0 ± 24.7 mmHg vs. 143.3 ± 24.1 mmHg, respectively; p < 0.05), while no difference in resting HR among the three categories was observed (80 ± 17 b.p.m. vs. 78 ± 19 b.p.m. vs. 77 ± 14 b.p.m., respectively; p = ns).
We did not observe significant differences in hemodynamic parameters after dosing across BMI categories, except a higher SBP baseline and maximum values in obese patients who performed the TE protocol (Table 4).
Discussion
This study assesses the side effect profile of regadenoson combined with low-level exercise across a wide range of BMI, with special attention to obesity, which is an important risk factor for cardiovascular disease. To the best of our knowledge, this is the first study comparing the side effect profile of patients undergoing these two types of low-level exercise: walking on the TE or SS in patients who lack sufficient ambulatory function.
As other studies have reported [19,20,21,22,23], the combination of low-level exercise during regadenoson administration is safe and produces a significant reduction in the side effect profile. Moreover, our data show that TE exercise produces a better side effect profile than SS exercise, most probably due to its higher level of exercise performance, as no significant differences with regard to other factors such as obesity or comorbidities (hypertension, diabetes, smoking, or known coronary artery disease) were seen between patients undergoing either type of exercise.
No differences were observed in the side effects of each type of low-level exercise among BMI categories, although linear trends in the TE group were observed. A possible explanation for the higher trend of headache and throat tightness in normal weight patients is the inverse relation between body weight and plasmatic concentrations of regadenoson [24].
Although no differences in SPECT results between regadenoson and nonspecific agonists of adenosine have been demonstrated [25], the latter require a weight-based dosing and, therefore, high doses are needed in obese patients, whereas regadenoson is administered as a fixed-dose because neither its central volume of distribution nor the clearance is significantly affected by body weight [8]. A comparison of side effects between regadenoson and adenosine both combined with low-level exercise in 207 patients with obesity [26] showed a similar side effect profile for both groups. However, the lack of data about a minimal toxic dose of adenosine makes the fixed-dose of regadenoson safer. Moreover, recent ASNC guidelines [27] describe that the correct weight-base dose for the obese patients is unclear for adenosine, and it is customary to use the upper limit of 250 lbs. (113.5 kg) for adenosine dosing. In this way, regadenoson would be the only available option for patients with higher weights [23]. An example of MPI SPECT in an obese female patient is shown in Fig. 4.
Concerning BMI subgroups, our results confirm other studies [24, 28, 29] showing that the side effect profile of regadenoson is similar across a wide range of body weights.
Regarding the hemodynamic response, several studies have shown a transient decrease in BP [10, 22]. Our results show no significant differences in SBP after regadenoson administration, confirming the RegEx trial results [20], where exercise was thought to counteract the SBP lowering effect of regadenoson. We observed higher values of resting and maximum SBP in obese patients, but no differences were found in the increase of SBP after dosing.
Regadenoson increases HR more than adenosine [30,31,32]. Although the adenosine-induced tachycardia had been attributed to a baroreflex-mediated activation, other authors [32] concluded that the selective activation of the A2A receptors of regadenoson in the carotid body produces direct activation of the sympathetic nervous system and, therefore, a more exaggerated increase of HR. In our study, significant higher HR values after regadenoson injection were observed in the TE group, again probably in relation to the higher level of exercise.
Limitations of the study
Patients did not perform a questionnaire of the intensity of symptoms and, therefore, the possible grading of effects is not reflected in this study. However, no patient required theophylline administration for reversal of severe effects, thus we consider all symptoms mild to moderate.
Conclusion
Regadenoson is safe, with a similar side effect profile across a wide range of body weights. The TE exercise shows a better profile than the SS exercise, but the latter is preferable to no exercise at all. A reasonable amount of exercise improves the tolerability and the image quality when compared to pharmacologic stress alone in patients who cannot walk on a treadmill. In this sense, it appears to be an attractive choice for this growing population.
Given that obesity increases hypoventilation and decreases the exercise capacity and that the most recent ASNC guidelines do not recommend adenosine administration in patients with weight higher than 113.5 kg, regadenoson represents the only safe vasodilator stress agent at this moment.
References
Media centre. Obesity and overweight. Fact sheet N°311 (updated January 2015). http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 29 July 2016.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. WHO technical report series 894. Geneva: World Health Organization; 2000.
Wilson PW, D’Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162(16):1867–72.
Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation. 2006;113:898–918.
Madala MC, Franklin BA, Chen AY, Berman AD, Roe MT, Peterson ED, Ohman EM, Smith SC Jr, Gibler WB, McCullough PA. Obesity and age of first non-st-segment elevation myocardial infarction. J Am Coll Cardiol. 2008;52:979–85.
Verbene HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40.
McGeoch RJ, Oldroyd KG. Pharmacological options for inducing maximal hyperemia during studies of coronary physiology. Catherter Cardiovasc Interv. 2008;71:198–204.
Rapiscan: EPAR – Product Information – European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001176/WC500097100.pdf
Al Jaroudi W, Iskandrian AE. Regadenoson: a new myocardial stress agent. J Am Coll Cardiol. 2009;54:1123–30.
Iskandrian AE, Bateman T, Belardinelli L, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol. 2007;14:645–58.
Jager PL, Buiting M, Mouden M, Oostkijk AH, Timmer J, Knollema S. Regadenoson as a new stress agent in myocardial perfusion imaging. Initial experience in The Netherlands. Rev Esp Med Nucl Imagen Mol. 2014;33:346–51.
Thomas GS, Tammelin BR, Schiffman GL, Marquez R, Rice DL, Milikien D, et al. Safety of regadenoson, a selective adenosine A2A agonist, in patients with chronic obstructive pulmonary disease: a randomized, double-blind, placebo-controlled trial (RegCOPD trial). J Nucl Cardiol. 2008;15:319–28.
Leaker BR, O’Connor B, Hansel TT, Barnes PJ, Meng L, Mathur VS, Lieu HD. Safety of regadenoson, an adenosine A2A receptor agonist for myocardial perfusion imaging, in mild asthma and moderate asthma patients: a randomized, double-blind, placebo-controlled trial. J Nucl Cardiol. 2008;15:329–36.
Prenner BM, Bukofzer S, Behm S, Feaheny K, McNutt BE. A randomized, double-blind, placebo-controlled study assessing the safety and tolerability of regadenoson in subjects with asthma or chronic obstructive pulmonary disease. J Nucl Cardiol. 2012;19:681–92.
Salgado-Garcia C, Jimenez-Heffernan A, Sanchez de Mora E, Ramos-Font C, Lopez-Martin J, Rivera de los Santos F, Ynfante-Mila I. Comparative study of the safety of regadenoson between patients with mild/moderate chronic obstructive pulmonary disease and asthma. Eur J Nucl Med Mol Imaging. 2014;41:119–25.
Golzar Y, Doukky R. Regadenoson use in patients with chronic obstructive pulmonary disease: the state of current knowledge. Int J Chron Obstruct Pulmon Dis. 2014;9:129–37.
Salgado-Garcia C, Jimenez-Heffernan A, Ramos-Font C, Lopez-Martin J, Sanchez de Mora E, Aroui T, Lopez-Aguilar R, Rivera de los Santos F, Ruiz-Frutos C. Safety of regadenoson in patients with severe chronic obstructive pulmonary disease. Rev Esp Med Nucl Imagen Mol. 2016;35:283–6.
Stratmann HG, Mark AL, Williams GA. Thallium-201 perfusion imaging with atrial pacing or dypiridamole stress testing for evaluation of cardiac risk prior to nonvascular surgery. Clin Cardiol. 1990;13:611–6.
Thomas GS, Prill NV, Majmundar H, Fabrizi RR, Thomas JJ, Hayasida C, et al. Treadmill exercise during adenosine infusion is safe, results in fewer adverse reactions, and improves myocardial perfusion image quality. J Nucl Cardiol. 2000;7(5):439–46.
Kwon DH, Cerqueira MD, Young R, Houghtaling P, Lieber E, Menon V, et al. Lessons from regadenoson and low-level tredmill/regadenoson myocardial perfusion imaging: initial clinical experience in 1263 patients. J Nucl Cardiol. 2010;17(5):853–7.
Thomas GS, Thompson RC, Miyamoto MI, et al. The RegEx trial: a randomized, double-blind, placebo- and active-controlled pilot study combining regadenoson, a selective A2A adenosine agonist, with low-level exercise, in patients undergoing myocardial perfusion imaging. J Nucl Cardiol. 2009;16(1):63–72.
Elliot MD, Holly TA, Leonard SM, Hendel RC. Impact of an abbreviated adenosine protocol incorporating adjunctive treadmill exercise on adverse effects and image quality in patients undergoing stress myocardial perfusion imaging. J Nucl Cardiol. 2000;7(6):584–9.
Janvier L, Pinaquy J, Douard H, Karcher G, Bordenave L. A useful and easy to develop combined stress test for myocardial perfusion imaging: Regadenoson and isometric exercise, preliminary results. J Nucl Cardiol. 2017;24(1):34–40.
Reyes E, Staerh P, Olmsted A, et al. Effect of body mass index on the efficacy, side effect profile, and plasma concentration of fixed-dose regadenoson for myocardial perfusion imaging. J Nucl Cardiol. 2011;18(4):620–7.
Mahmarian JJ, Peterson LE, Xu J, Cerqueira MD, et al. Regadenoson provides perfusion results comparable to adenosine in heterogeneous patient population: a quantitative analysis from de ADVANCE MPI trials. J Nucl Cardiol. 2015;22(2):248–61.
Salgado C, Jimenez-Heffernan A, Ramos-Font C, Lopez-Martin J, Sanchez de Mora E, Lopez-Aguilar R, et al. Comparison of adverse events between regadenoson and adenosine both combined with low-level exercise in patients with obesity. Eur Heart J Cardiovasc Imaging. 2015;16(suppl 1):i38–55.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verbene HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: stress, protocols, and tracers. J Nucl Cardiol. 2016;23:606–39.
Cerqueira MD, Nguyen P, Staehr P, Underwood SR, Iskandrian AE. Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging. 2008;1:307–16.
Gordi T, Frohna P, Hai-Ling S, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet. 2006;45(12):1201–12.
Clarke B, Conradson TB, Dixon CM, et al. Reproducibility of heart rate changes following adenosine infusion in man. Eur J Clin Pharmacol. 1988;35:309–11.
Mahmarian JJ, Cerqueira MD, Iskandrian AE, et al. Regadenoson induces comparable left ventricular perfusion defects as adenosine: a quantitative analysis from the ADVANCE MPI 2 trial. JACC Cardiovasc Imaging. 2009;2:959–68.
Dhalla AK, Wong MY, Wang WQ, Biaggioni I, Belardinelli L. Tachycardia caused by A2A adenosine receptor agonist is mediated by direct sympathoexcitation in awake rats. J Pharmacol Exp Ther. 2006;316:695–702.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosures
The authors declare that there is no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Salgado-Garcia, C., Jimenez-Heffernan, A., Lopez-Martin, J. et al. Influence of body mass index and type of low-level exercise on the side effect profile of regadenoson. Eur J Nucl Med Mol Imaging 44, 1906–1914 (2017). https://doi.org/10.1007/s00259-017-3717-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3717-1