Abstract
Background
There are limited data on the effect of body mass index (BMI) on the actions of fixed-dose regadenoson. The purpose of this study was to determine the effect of BMI on the efficacy, side effects, and plasma concentration of regadenoson for Myocardial Perfusion Imaging (MPI).
Methods and Results
The study included 2,015 subjects from the ADVANCE MPI trials. Initial adenosine MPI was followed by randomization to regadenoson (400-μg bolus injection) or adenosine (6-minute infusion) MPI. Subjects were classified according to BMI into six categories from underweight (<20 kg/m2) to extremely obese (≥40 kg/m2). PK modeling was used to predict the effect of BMI on plasma regadenoson concentration (PRC). Adenosine-regadenoson agreement rates for the presence and extent of reversibility were similar across BMI categories (P > .05). The incidence of side effects was also similar across BMIs (P ≥ .06). Subjects were less likely to feel very or extremely uncomfortable after regadenoson vs adenosine in all groups with BMI ≥ 25 kg/m2, but this trend was not statistically significant in subjects with BMI 20-24 kg/m2 (P > .05). PRC was inversely related to BMI with 19% higher PRC in the underweight and 36% lower PRC in the extremely obese compared with a normal weight subject.
Conclusions
BMI does not alter the efficacy of regadenoson MPI despite lower PRC in high BMI subjects, or its side effect profile despite higher PRC in low BMI subjects. Regadenoson is better tolerated than adenosine but this benefit seems to lose statistical significance in subjects with BMI < 25 kg/m2.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary vasodilators are used as pharmacological stress agents in patients who are unable to exercise.1 Dipyridamole and adenosine are coronary vasodilators that in combination with myocardial perfusion imaging (MPI) provide valuable diagnostic and prognostic information for the assessment of patients with known or suspected coronary artery disease (CAD).2 Both agents are administered by continuous weight-adjusted infusion to increase coronary blood flow by stimulating adenosine receptors.3-5 Regadenoson, a chemical derivative of adenosine, is a selective A2A-adenosine receptor agonist that was recently approved as a pharmacological stress agent in the United States. Regadenoson is also administered intravenously but as a fixed-dose bolus (<10 seconds) injection. The magnitude of increase in coronary blood flow velocity by regadenoson is dose-dependent; at the clinically approved dose of 400 μg, the coronary hyperemic effect of regadenoson is similar to that of intracoronary adenosine.6 This effect lasts 2-5 minutes, which is adequate for the detection of inducible myocardial perfusion abnormality by stress MPI.6 In healthy volunteers, individual body weight had little effect on regadenoson pharmacokinetics or clearance, and this supported the use of non-weight adjusted dose injection.7 However, because of the small number of subjects studied, it was not possible to determine the effect of a wider range of body weights on regadenoson pharmacokinetics.
The ADVANCE-MPI 1 and 2 trials have shown that fixed-dose regadenoson MPI is comparable to adenosine MPI for the detection of reversible myocardial perfusion abnormality in patients with known or suspected CAD.8 The trials have also shown that regadenoson is better tolerated than adenosine. A previous study has already demonstrated that image comparability, incidence of side effects after regadenoson injection and test tolerability were not different between patients with body mass index (BMI) <30 vs >30 kg/m2.9 We extended previous observations by investigating the effect of a wider BMI range on the efficacy, side effect profile, and tolerability of regadenoson MPI. We also examined the effect of BMI on regadenoson pharmacokinetics (PK) with the use of population PK modeling and simulation.
Methods
Study Design and Population
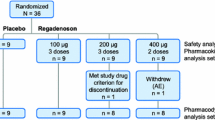
This was a sub-group analysis of the ADVANCE-MPI 1 and 2 trials, two identical double-blind, randomized, double-dummy, multicentre phase III trials evaluating the effectiveness of regadenoson MPI for the detection of reversible myocardial perfusion abnormality in patients with known or suspected CAD. These trials have been described in detail previously.8,9 In brief, eligible subjects underwent adenosine MPI for clinical purposes. Following initial open-label adenosine MPI, subjects were randomly assigned to either regadenoson or adenosine MPI in a 2:1 ratio. A total of 2,015 subjects underwent both initial and randomized MPI. The primary objective was to demonstrate that image agreements between two sequential adenosine-regadenoson images (regadenoson group) are not inferior to the strength of agreement between two sequential adenosine images (repeat adenosine group). Complete imaging data was available in 1,871 subjects for the purpose of efficacy (image comparability) analysis. Initial and randomized MPI were performed at a median interval of 7 days (25th to 75th percentile, 5 to 14 days). For the purpose of this analysis, subjects were classified according to BMI into the following categories: underweight (<20 kg/m2), normal (20-24 kg/m2), overweight (25-29 kg/m2), obese (30-34 kg/m2), very obese (35-39 kg/m2), or extremely obese (≥40 kg/m2).
Vasodilator Stress
For the initial adenosine MPI study, all subjects received adenosine at 140 μg/kg/min for 6 minutes without exercise. The tracer was injected 3 minutes after starting the adenosine infusion. For the randomized MPI study, subjects received either adenosine, which was administered in an identical way, or regadenoson, which was administered intravenously as a single non-weight adjusted injection of 400 μg over 10 seconds followed by a 5-mL saline solution flush. For the purposes of blinding, two intravenous lines were placed in each subject, one for the infusion of adenosine or placebo and the second for bolus injection of regadenoson or placebo. A bolus of regadenoson or placebo was injected 2.5 minutes after starting the infusion and the tracer was administered 10 to 20 seconds following a saline flush. Heart rate, blood pressure, and 12-lead ECG were measured at rest and over 45 minutes.
Image Processing and Interpretation
A full description of image processing and interpretation has been published.8 Briefly, the initial adenosine and randomized stress scans were acquired in identical ways and the images were analyzed in a single core laboratory. The left ventricular myocardium was divided into 17 segments and tracer uptake was scored using a 5-point scale from 0 = normal to 4 = absent by three experienced readers without knowledge of clinical status, BMI, or stress agent administered. Each scan was classified according to the number of reversible myocardial segments as 0 to 1 (no to minimal reversibility), 2 to 4 (small to moderate), or ≥5 (large). Each scan was classified further as reversible (2 or more reversible segments) or non-reversible (≤1 reversible segment) for the purpose of this analysis.
Side Effects and Tolerability
All side effects during and after pharmacological stress were recorded for both the initial and randomized MPI studies. The frequency of the each of the following pre-specified side effects (and any of these) was compared across BMI groups: chest pain, dyspnea, flushing, gastrointestinal (GI) discomfort, headache, light-headedness or dizziness, and throat, neck, or jaw discomfort. At the completion of the randomized study, test tolerability was assessed by requesting the subject to report how they felt during the randomized stress test (using a 4-point scale from 1 = comfortable to 4 = extremely uncomfortable) and by asking how the second randomized procedure compared to the initial adenosine study (using a 5-point scale from 1 = much better to 5 = much worse).
Population PK Modeling and Simulation of Regadenoson
Because of the limited number of samples obtained during the ADVANCE-MPI trials, the population PK analysis included regadenoson plasma concentrations data from another three clinical studies.6-10 The dataset therefore consisted of plasma regadenoson concentration values obtained from four to five samples taken from subjects enrolled in the two Phase III ADVANCE-MPI trials8,9 and from more than 10 plasma samples taken from subjects enrolled in three Phase I and II studies.6,7,10 Blood was sampled at various times from 1 minute to 12 hours post-dose, with the majority of samples collected within 4 hours of dosing. The final dataset comprised 6,531 values from 1,394 subjects. A number of linear compartmental PK models were evaluated to determine which model best described the regadenoson concentration-time data.7 The best population PK model included three compartments with an allometric relationship based on total body weight for all clearance, volume, and rate-constant parameters (appendix).
To determine the influence of BMI on regadenoson PK, the plasma regadenoson concentration at 1 minute after a 400-μg injection of regadenoson in a typical 65-year-old subject with preserved renal function (i.e., creatinine clearance = 100 mL/min) and BMI of 17.5, 22.5, 27.5, 32.5, 37.5, or 42.5 kg/m2 was simulated using parameter estimates of the population PK model.11 Weight for each BMI value was extrapolated using the relationship between weight and BMI established in the population model.
Statistical Analysis
Results were summarized as mean ± SD or SEM or median (interquartile range). Spearman rank correlation was used to examine the relationship between BMI and hemodynamic parameters at baseline and after vasodilator stress. Cochran-Mantel-Haenszel tests were used to assess equality of simple agreement rates for the presence of reversibility and for the size of reversible perfusion abnormality between initial adenosine and randomized scans across BMI groups. The reversibility average agreement rate was estimated as the equally weighted average of the agreement rates for subjects with initial adenosine scan category 0-1 or ≥2 reversible myocardial segments. The reversibility size category average agreement rate was calculated as the equally weighted average of the agreement rates for subjects with initial adenosine scan category 0-1, 2-4 or ≥5 reversible segments. For all comparisons, values of P < .05 were considered statistically significant. Statistical analyses were performed using SAS/STAT® versions 9.1 and 9.2. Simulation analysis was conducted using NONMEM VI.12
Results
Clinical characteristics of subjects who underwent regadenoson MPI are summarized in Table 1. There were fewer male subjects in the underweight and extremely obese categories (P < .001). Obese subjects were younger than non-obese (P < .001). The incidence of hypertension and diabetes increased with increasing BMI (P < .001).
Mean (SD) resting heart rate tended to increase with BMI from 64 ± 11 bpm in subjects with BMI < 20 kg/m2 to 70 ± 11 bpm in subjects with BMI ≥ 40 kg/m2. Similarly, mean (SD) systolic and diastolic blood pressure increased slightly with BMI from 135 ± 18 and 74 ± 9 mm Hg in subjects with BMI < 20 kg/m2 to 140 ± 20 and 80 ± 11 mm Hg in subjects with BMI ≥ 40 kg/m2, respectively. After regadenoson stress, there was a weak trend of smaller heart rate increases with increasing BMI, with median increases ranging from 21 (14 to 30) bpm in underweight subjects to 18 (14 to 28) bpm in extremely obese subjects (r = −0.13, P < .001). There was also a weak trend of smaller median systolic blood pressure decreases with increasing BMI ranging from −14 (−21 to −3) mm Hg in underweight subjects to −10 (−17 to −3) mm Hg in extremely obese subjects (r = 0.06, P = .02). There was no significant relationship between BMI and diastolic blood pressure changes after regadenoson injection (r = 0.02, P = .54).
Efficacy
Average agreement rates for the presence or absence of reversible perfusion abnormality are shown in Table 2. For subjects randomized to regadenoson, the average agreement rates did not differ significantly between initial adenosine and regadenoson MPI across BMI categories (P = .06) but for subjects randomized to repeat adenosine, average agreement rates decreased with increasing BMI (trend test, P = .009). For both the randomized groups, the observed average agreement rate was lowest in the extremely obese. Average agreement rates for the size of reversible perfusion abnormality were also similar across BMI categories for subjects randomized to regadenoson (P = .13) and for those randomized to repeat adenosine (P = .64) (Table 3).
Side Effects and Tolerability
The frequency of each of the pre-specified side effects and of any side effects after regadenoson injection was similar across BMI categories (P ≥ .06). The frequency of the five commonest side effects according to BMI is shown in Figure 1. The incidence of any regadenoson-related side effects in subjects with BMI < 20 kg/m2 was similar to that in normal weight subjects (15 (65%) vs 188 (75%), respectively; P = .33). With regard to test tolerability, the proportion of subjects reporting discomfort after regadenoson vs adenosine was 22% vs 0% in the <20 kg/m2 BMI category; 12% vs 17% in the 20-24 kg/m2 category; 8% vs 18% in the 25-29 kg/m2; 5% vs 19% in the 30-34 kg/m2; 9% vs 27% in the 35-39 kg/m2; and 8% vs 31% in the ≥40 kg/m2 BMI category, respectively. Subjects with BMI < 25 kg/m2 were more likely to report feeling very or extremely uncomfortable during regadenoson than subjects with BMI ≥ 25 kg/m2. The estimated ratios of the odds of feeling very or extremely uncomfortable after regadenoson to the odds of feeling very or extremely uncomfortable after repeat adenosine are shown in Figure 2.
Regadenoson:adenosine odds ratio (95% confidence interval). Estimated ratios of the odds of feeling very or extremely uncomfortable after regadenoson to the odds of feeling very or extremely uncomfortable after repeat adenosine according to BMI category. There was no data point for repeat adenosine in the BMI category ≤20 kg/m2
Effect of BMI on Regadenoson Pharmacokinetics
Simulated plasma regadenoson concentration 1 minute after dosing (C 1) was inversely related to BMI (Figure 3). The simulated plasma concentration of a normal weight subject (BMI 22.5 kg/m2) was 26.7 ng/mL (Table 4). According to the model, plasma regadenoson concentration was approximately 34% lower (17.7 ng/mL) for an extremely obese subject (BMI 42.5 kg/m2) and approximately 17% higher (31.2 ng/mL) for an underweight subject (BMI 17.5 kg/m2) compared with a normal weight subject.
Discussion
The results of this study demonstrate that BMI influences the pharmacokinetics of fixed-dose regadenoson but this does not translate into clinically significant changes in regadenoson efficacy or side effect profile across various BMI categories. PK modeling and simulation indicated lower plasma regadenoson concentrations with increasing BMI after a rapid injection of 400 μg of regadenoson. However, the presence and extent of reversible perfusion abnormality by regadenoson was similar across all BMI categories suggesting that the coronary hyperemia induced by 400 μg of regadenoson is not modified by subject body weight. Importantly, BMI had no significant effect on the side effect profile of regadenoson. Furthermore, regadenoson was better tolerated than adenosine although this trend was not statistically significant in subjects with BMI < 25 kg/m2. Our results confirm early observations7,9 and demonstrate that regadenoson at a fixed dose of 400 μg is an effective stress agent that allows the detection of inducible ischemia in subjects irrespective of their BMI.
There was a trend of smaller changes in heart rate and systolic blood pressure with increasing BMI after regadenoson injection. Such trend is unlikely to represent a blunted response to regadenoson in larger subjects and might be partly or entirely explained by the observed increase in baseline heart rate and blood pressure with increasing BMI.
Unlike adenosine and dipyridamole, regadenoson is administered as a fixed-dose injection. Previous dose-escalation and safety studies demonstrated that single-dose regadenoson causes maximal or near-maximal coronary hyperemia with minimal side effects.6 These studies, however, were too small to rule out the effect of a wide range of body weights on regadenoson actions. This study shows similar efficacy of regadenoson for the detection of reversible perfusion abnormality across a wide range of BMIs suggesting that the ability of single-dose regadenoson to induce adequate hyperemia and hence myocardial blood flow heterogeneity is independent of body weight.
Image agreement rates between initial adenosine and regadenoson for the presence and extent of reversible perfusion abnormality were lowest in subjects with BMI ≥ 40 kg/m2. Similar low agreement rates were found in the repeat adenosine group. Large body habitus is likely to result in lower image quality and soft-tissue attenuation-related defects and hence less certainty and greater reader variability in the visual interpretation of serial MPI studies. A recent study by Mahmarian et al13 has demonstrated that quantitative image analysis significantly improves agreement between sequential MPI studies for the severity and extent of perfusion abnormality. By comparing individual myocardial count profile with that of a normal database, quantitative analysis might have resulted in better agreement between sequential adenosine and regadenoson MPI among the obese. Also, the addition of low-level exercise might have increased agreement rates in the extremely obese by improving image quality.14,15 Supplemental exercise during vasodilator stress enhances image quality by provoking splanchnic vasoconstriction and decreasing background to heart activities ratio.14,15
According to this study, the vasodilator action of regadenoson is not modified by BMI and this might partly be explained by the initial volume of distribution of a rapid injection of regadenoson after its administration into a peripheral vein. The effect of regadenoson on the coronary circulation is determined by its concentration during its first pass through the heart. In turn, first pass concentration of regadenoson is primarily determined by the volume of blood between the injection site and the heart. We hypothesize that the volume of blood diluting a bolus dose of regadenoson as it travels from the injection site to the heart is likely to be independent of and less variable than individual body weight.
As suggested by the PK model in this study, plasma regadenoson concentration varies according to BMI. However, all predicted concentrations after a rapid injection of 400 µg of regadenoson were consistently above the EC80 value or concentration of regadenoson at 80% of maximal effect (i.e., 12 ng/mL), a concentration that is known to yield adequate coronary vasodilation for the purpose of perfusion imaging.16 Moreover, further increases in regadenoson concentration above this value would not lead to a significant increase in response.16 Therefore, injection of a single 400-μg dose of regadenoson results in plasma concentrations exceeding the minimum required for an adequate hyperemic effect across a wide range of BMIs. This observation supports the lack of a significant effect of BMI on the efficacy of regadenoson MPI.
Finally, the incidence of side effects after regadenoson injection was similar across BMIs. This study also shows that regadenoson is better tolerated than adenosine although this appears to be less apparent in underweight and normal weight subjects as opposed to obese subjects, and is correlated with a 17% higher predicted plasma concentration of regadenoson in the underweight. Therefore, the reduced tolerability in these subjects might be explained by a higher plasma concentration of regadenoson that is not associated with an increased risk of side effects.
Limitations
This is a retrospective study and, therefore, it is not powered to detect smaller differences in efficacy, side effect profile, or tolerability in the extreme BMI groups, particularly in the underweight group. BMI is confounded to some extent by other subject characteristics that may affect efficacy, side effect profile, and tolerability such as age, gender, and ethnicity, but the study did not control for these characteristics.
For the purpose of efficacy analysis, the extent of myocardial perfusion abnormality induced by regadenoson was compared with that caused by adenosine, the reference procedure. We cannot draw a conclusion regarding the effect of BMI on the diagnostic accuracy of regadenoson MPI for the detection of angiographic coronary artery stenosis. However, based on the current results, it is unlikely that BMI would modify the sensitivity of regadenoson MPI for the detection of hemodynamically significant coronary stenosis.
In conclusion, the efficacy of fixed-dose regadenoson for the detection of inducible myocardial ischemia is not influenced by BMI. This phenomenon can be explained by the mechanism of action of regadenoson and its concentration-response relationship characteristics. Regadenoson is better tolerated than adenosine but this benefit seems to disappear in subjects with BMI < 25 kg/m2. The current results support the use of a single dose of 400 μg of regadenoson for stress MPI.
References
Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging—executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). J Am Coll Cardiol 2003;42:1318–33.
Loong CY, Anagnostopoulos C. Diagnosis of coronary artery disease by radionuclide myocardial perfusion imaging. Heart 2004;90:v2–9.
Botvinick EH, Dae MW. Dipyridamole perfusion scintigraphy. Semin Nucl Med 1991;21:242–65.
Cerqueira MD, Verani MS, Schwaiger M, Heo J, Iskandrian AS. Safety profile of adenosine stress perfusion imaging: Results from the Adenoscan Multicenter Trial Registry. J Am Coll Cardiol 1994;23:384–9.
Sato A, Terata K, Miura H, Toyama K, Loberiza FR Jr, Hatoum OA, et al. Mechanism of vasodilation to adenosine in coronary arterioles from patients with heart disease. Am J Physiol Heart Circ Physiol 2005;288:H1633–40.
Lieu HD, Shryock JC, von Mering GO, Gordi T, Blackburn B, Olmsted AW, et al. Regadenoson, a selective A2A adenosine receptor agonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol 2007;14:514–20.
Gordi T, Frohna P, Sun HL, Wolff A, Belardinelli L, Lieu H. A population pharmacokinetic/pharmacodynamic analysis of regadenoson, an adenosine A2A-receptor agonist, in healthy male volunteers. Clin Pharmacokinet 2006;45:1201–12.
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 2007;14:645–58.
Cerqueira MD, Nguyen P, Staehr P, Underwood SR, Iskandrian AE, ADVANCE-MPI Trial Investigators. Effects of age, gender, obesity, and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging: Integrated ADVANCE-MPI trial results. JACC Cardiovasc Imaging 2008;1:307–16.
Gordi T, Blackburn B, Lieu H. Regadenoson pharmacokinetics and tolerability in subjects with impaired renal function. J Clin Pharmacol 2007;47:825–33.
Food and Drug Administration. Population pharmacokinetics. US Department of Health and Human Services Guidance for Industry 1999;1-31.
Beal S, Sheiner L, Oeckmann AJE. Icon Development Solutions. NONMEM Users Guides 2006.
Mahmarian JJ, Cerqueira MD, Iskandrian AE, Bateman TM, Thomas GS, Hendel RC, et al. Regadenoson induces comparable left ventricular perfusion defects as adenosine: A quantitative analysis from the ADVANCE MPI 2 trial. JACC Cardiovasc Imaging 2009;8:959-68.
Thomas GS, Prill NV, Majmundar H, Fabrizi RR, Thomas JJ, Hayashida C, et al. Treadmill exercise during adenosine infusion is safe, results in fewer adverse reactions, and improves myocardial perfusion image quality. J Nucl Cardiol 2000;7:439–46.
Thomas GS, Thompson RC, Miyamoto MI, Ip TK, Rice DL, Milikien D, et al. The RegEx trial: A randomized, double-blind, placebo- and active-controlled pilot study combining regadenoson, a selective A(2A) adenosine agonist, with low-level exercise, in patients undergoing myocardial perfusion imaging. J Nucl Cardiol 2009;16:63–72.
Gao Z, Li Z, Baker SP, Lasley RD, Meyer S, Elzein E, et al. Novel short-acting A2A adenosine receptor agonists for coronary vasodilation: Inverse relationship between affinity and duration of action of A2A agonists. J Pharmacol Exp Ther 2001;298:209–18.
Acknowledgments
Authors would like to thank Dr Jerling, a former employee of CV Therapeutics, Inc., Justus Bingham and the Metrum Research Group for conducting the population PK modeling and simulation of regadenoson.
Conflict of interest
Drs Staehr, Olmsted, Zeng, and Blackburn are current employees of Gilead Sciences, Inc/CV Therapeutics, which provided funding for this study. Dr Cerqueira has served as Consultant and on the Speakers Bureau for CV Therapeutics, Inc, and currently serves as Consultant and on the Speakers Bureau for Astellas Pharma US. Professor Underwood has served as member of the publications committee of ADVANCE MPI trials, which were sponsored by CV Therapeutics, Inc. The other authors report no conflicts.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by CV Therapeutics/Gilead Sciences, Inc (Palo Alto, California) and Astellas Pharma US (Deerfield, Illinois).
Appendix
Appendix
Three-compartment model:
where CL i is the clearance, \( {\text{CL}}_{{i}_{{\text{CR}}_{\text{norm}}}} \) is the normalized creatinine clearance, WT i is the weight, BMI i is the body mass index, V 1i is the volume of the central compartment, K 12i is the rate constant from central compartment to distribution compartment 1, K 21i is the rate constant from distribution compartment to central compartment, K 13i is the rate constant from central compartment to distributional compartment 2, K 31i is the rate constant from distributional compartment 2 to central compartment.
Rights and permissions
About this article
Cite this article
Reyes, E., Staehr, P., Olmsted, A. et al. Effect of body mass index on the efficacy, side effect profile, and plasma concentration of fixed-dose regadenoson for myocardial perfusion imaging. J. Nucl. Cardiol. 18, 620–627 (2011). https://doi.org/10.1007/s12350-011-9377-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9377-9