Abstract
Every biological fluid, blood, interstitial fluid and lymph, urine, saliva, lacrimal fluid, nipple aspirate, and spinal fluid, contains a peptidome-degradome derived from the cellular secretome along with byproducts of the metabolic/catabolic activities of each parenchymal organ. Clement et al. (J Proteomics 78:172–187, 2013), Clement et al. (J Biol Chem 291:5576–5595, 2016), Clement et al. (PLoS One 5:e9863, 2010), Clement et al. (Trends Immunol 32:6–11, 2011), Clement et al. (Front Immunol 4:424, 2013), Geho et al. (Curr Opin Chem Biol 10, 50–55, 2006), Interewicz et al. (Lymphology 37:65‑72, 2004), Leak et al. (Proteomics 4:753‑765, 2004), Popova et al. (PLoS One 9:e110873, 2014), Zhou et al. (Electrophoresis 25:1289‑1298, 2004), D'Alessandro et al. (Shock 42:509‑517, 2014), Dzieciatkowska et al. (Shock 42:485‑498, 2014), Dzieciatkowska et al. (Shock 35:331‑338, 2011), Jordan et al. (J Surg Res 143:130‑135, 2007), Peltz et al. (Surgery 146:347‑357, 2009), Zurawel et al. (Clin Proteomics 8:1, 2011), Ling et al. (Clin Proteomics 6:175‑193, 2010), Sturm et al. (Nat Commun 4:1616, 2013). Over the last decade, qualitative and quantitative analysis of the biological fluids peptidome and degradome have provided a dynamic measurement of tissue homeostasis as well as the tissue response to pathological damage. Proteomic profiling has mapped several of the proteases and resulting degradation by-products derived from cell cycle progression, organ/tissue remodeling and cellular growth, physiological apoptosis, hemostasis, and angiogenesis. Currently, a growing interest lies in the degradome observed during pathological conditions such as cancer, autoimmune diseases, and immune responses to pathogens as a way to exploit biological fluids as liquid biopsies for biomarker discovery Dzieciatkowska et al. (Shock 42:485–498, 2014), Dzieciatkowska et al. (Shock 35:331–338, 2011), Ling et al. (Clin Proteomics 6:175–193, 2010), Ugalde et al. (Methods Mol Biol 622:3–29, 2010), Quesada et al. (Nucleic Acids Res 37:D239‑243, 2009), Cal et al. (Front Biosci 12, 4661–4669, 2007), Shen et al. (PLoS One 5:e13133, 2010a), Antwi et al. (Mol Immunol 46:2931–2937, 2009a), Antwi et al. (J Proteome Res 8:4722‑4731, 2009b), Bedin et al. (J Cell Physiol 231, 915‑925, 2016), Bery et al. (Clin Proteomics 11:13, 2014), Bhalla et al. (Sci Rep 7:1511, 2017), Fan et al. (Diagn Pathol 7:45, 2012a), Fang et al. (Shock 34:291‑298, 2010), Fiedler et al. (Clin Cancer Res 15:3812‑3819, 2009), Fredolini et al. (AAPS J 12:504‑518, 2010), Greening et al. (Enzymes 42:27‑64, 2017), He et al. (PLoS One 8:e63724, 2013), Huang et al. (Int J Gynecol Cancer 28:355‑362, 2018), Hashiguchi et al. (Med Hypotheses 73:760‑763, 2009), Liotta and Petricoin (J Clin Invest 116:26‑30, 2006), Petricoin et al. (Nat Rev Cancer 6:961‑967, 2006), Shen et al. (J Proteome Res 9:2339‑2346, 2010a), Shen et al. (J Proteome Res 5:3154‑3160, 2006), Smith (Clin Proteomics 11:23, 2014), Wang et al. (Oncotarget 8:59376‑59386, 2017), Yang et al. (Clin Exp Med 12:79‑87, 2012a), Yang et al. (J Clin Lab Anal 26:148‑154, 2012b), Yang et al. (Anat Rec (Hoboken) 293:2027‑2033, 2010), Zapico-Muniz et al. (Pancreas 39:1293‑1298, 2010), Villanueva et al. (Mol Cell Proteomics 5:1840‑1852, 2006), Robbins et al. (J Clin Oncol 23:4835‑4837, 2005), Klupczynska et al. (Int J Mol Sci 17:410, 2016). In this review, we focus on the current knowledge of the degradome/peptidome observed in two main biological fluids (plasma and lymph) during physiological and pathological conditions and its importance for immune surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Interstitial fluid and lymph
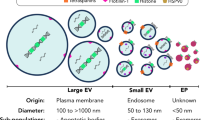
The interstitial fluid is a thin film of fluid that bathes all the cellular layers of each parenchymal organ (Guyton and Coleman 1968; Wiig and Swartz 2012; Zhang et al. 2006). In humans, 8–12 l of interstitial fluid are generated every day, which accounts for about one sixth of the body weight (Guyton and Coleman 1968; Wiig and Swartz 2012; Kramer et al. 1986). A fundamental function of the interstitial fluid is to provide nutrients, water, electrolytes, metabolites, and overall biomolecules to parenchymal cells (Wiig and Swartz 2012; Tran et al. 2018; Aukland et al. 1984; Zhang et al. 2017). Indeed, since the organ’s cellular layers are not in direct contact with the blood, nutrients, protein, and soluble molecules need to extravasate into the interstitial fluid to be taken up by parenchymal cells. The movement of proteins and biomolecules from the intravascular to the extravascular/interstitial compartment is associated with movement of water and electrolytes, which altogether forms the elementary composition of the interstitial fluid. Using radioactive tracer, it was originally shown that all the major categories of plasma proteins, such as albumin and α, β,and γ globulins were present in the interstitial fluid at a relatively smaller concentration (between 20 to 37%, depending on the anatomical district) than in the plasma (Wiig and Swartz 2012; Reed and Wiig 1983; Wiig and Noddeland 1983). These proteins, which are pivotal for the maintenance of the intravascular oncotic pressure, extravasate from the blood capillaries following the gradient of hydrostatic pressure present between the arterial and venule-end of the capillary bed (Michel 2004). The interstitial fluid will then be progressively enriched with the tissue proteome derived from the cellular secretome, products of metabolic cellular activities, extracellular matrix remodeling, and physiological apoptosis (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; D'Alessandro et al. 2014; Dzieciatkowska et al. 2014; Dzieciatkowska et al. 2011; Zurawel et al. 2011; D'Alessandro et al. 2011; Veenstra 2007; Veenstra et al. 2005). Indeed, although plasma albumin and serum globulins constitute the majority of the lymph proteins, tissue-specific proteins are also highly represented in the lymph proteome when compared to the plasma proteome (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; D'Alessandro et al. 2014; Dzieciatkowska et al. 2014; Dzieciatkowska et al. 2011; Zurawel et al. 2011; D'Alessandro et al. 2011; Veenstra 2007; Veenstra et al. 2005). Tissue specific proteins are present both as soluble proteins as well as in exosomes and extracellular vesicles, released from parenchymal cells and circulating in the lymph (Hood 2017; Kojima et al. 2018; Kojima et al. 2017; Srinivasan et al. 2016). Soluble proteins and their degradation products comprise different members of the extracellular matrix proteome, which is processed by the several Matrix Metalloproteinases (MMPs) involved in tissue growth and remodeling. Among these, MMPs generate collagens, laminins, versican, and lumican, among many other cleavage fragments, as a way to accommodate cell movement, division, and regulate cellular architecture or to generate specific collagen products that will act as integrin signaling (Clement et al. 2013; Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; Shi et al. 2010; Shi et al. 2009; Shi et al. 2011; Postawski et al. 1999; El Azreq et al. 2012; Garnotel et al. 1995; Kagami et al. 2001). Additionally, MMPs, ADAMs, Sheddase, and γ-Secretase products of cleaved growth factors (SDF1, VEGF) or other surface receptors (TNF, IL-1R, IL-11R, Notch1 IL-32) have also been mapped in the lymph, where soluble peptides are released following extracellular or intramembrane processing upon receptor ectodomain release (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; Osenkowski et al. 2004; Sabbota et al. 2010; Rizzo et al. 2013; Sanz et al. 2018; Terawaki et al. 2015; De Paiva et al. 2009; Levine 2008). By-products from plasminogen activators and thrombin, such as fibrin and PAR-1,3 and 4 cleaved products have also been found in the lymph (Clement et al. 2016; Clement et al. 2010). Degradation products from kallikreins, involved in blood and lymph flow regulation and electrolytes balance have also been mapped in the serum and lymph peptidome (Clement et al. 2016; Clement et al. 2010).
Apoptotic cells, which have been detected in the lymph (Olszewski 2001), have also been shown to release intracellular proteins such as cytosolic enzymes (carboxypeptidase, enolase-3, LDH, GAPDH, different kinases), cytoskeletal proteins (α-actinin-4, filamin-α), chaperones (14–3-3, hsc-70 and hsp-90), and mitochondrial and nuclear proteins (histones HMGB1) (Bournazou et al. 2009; Lauber et al. 2003; Osman et al. 2017; Piacentini et al. 1999; Weigert et al. 2010). Degradation products due to caspase activity have also been mapped in the lymphatic fluid (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013).
During pathological conditions, including acute and chronic inflammation, cancer, and autoimmune and degenerative diseases, several proteomic analyses have shown that the interstitial fluid and the lymph are further enriched with by-products of tissue injury, necrosis, apoptosis, and overall cellular damage (D'Alessandro et al. 2014; Zurawel et al. 2011; Fang et al. 2010; Goldfinch et al. 2008; Meng and Veenstra 2007; Meng and Veenstra 2011; Mittal et al. 2008; Mittal et al. 2009; Nguyen et al. 2010; Olszewski et al. 2001). Following trauma changes in the lymph proteome could be observed within the first 30 min including triggering of coagulation and pro-inflammatory responses, changes in proteases/antiproteases homeostasis, and release of products from cellular damage (D'Alessandro et al. 2014). Similarly, changes in the lymphatic fluid were observed following acute pancreatitis with release of pancreatic enzymes and a necrosis-related degradome (Mittal et al. 2009). In patients with rheumatoid arthritis, the inflammatory process could be clearly mapped in the lymph draining the affected joints. Finally, lymph analysis in different models of cancer has shown the potential of exploiting interstitial and lymphatic fluid for early detection of metastasis. Indeed, one of the main goals of cancer research is the ability to detect and possibly prevent metastasis formation, and liquid biopsy is considered the key to monitor disease progression. We recently performed a comparative proteomic analysis between lymph and plasma in several patients with melanoma, as compared to healthy controls. We determined that the lymph was significantly enriched in melanoma biomarkers such as Melan-A, S100B, and S100A8 (Buchbinder and Flaherty 2016; Huang and Hoon 2016), whereas the same proteins were undetectable in blood (manuscript in preparation). Additionally, factors known to strongly correlate with metastatic potential in melanoma, including colony stimulating factor-1 (CSF-1), Galectin-3, and matrix metalloproteinases (MMP)-2 and -9 (Egeblad and Werb 2002), were also orders of magnitude higher in lymph compared to plasma (manuscript in preparation). When melanoma patients without metastasis were compared with those with metastasis, as well as with healthy patients, a distinct protein signature in the lymph, that was absent in the plasma, and that characterized the lymph of metastatic melanoma patients was found. Highly expressed were proteins related to cytoskeletal rearrangement and adhesion (myosin, actin, tropomyosin, troponin, integrins), matrix remodeling (vimentin, enolases, cathepsins), histone variants, and glycolytic enzymes (triosephosphate isomerase). Most of these proteins were previously shown to be differently regulated in tumor progression and metastasis (Wilson et al. 2010) (Hsiao et al. 2013).
Overall, during the last 20 years, several proteomic analyses performed on bovine, ovine, rodent, and human lymph sampled in physiological and pathological conditions have determined that the lymphatic fluid is not a simple ultrafiltrate of the plasma but collects the “omic signature” of the organ from which it drains (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; D'Alessandro et al. 2014; Dzieciatkowska et al. 2014; Dzieciatkowska et al. 2011; Zurawel et al. 2011; D'Alessandro et al. 2011; Veenstra 2007; Veenstra et al. 2005).
Blood
The blood peptidome-degradome was the first, among all other biological fluids, to be investigated. Over the years, several mass spec analyses have provided a comprehensive mapping of blood peptides in physiological and pathological conditions. Overall, over 10,000 peptides deriving from both intracellular and extracellular sources have been identified using bottom up and top down mass spectrometry. Most of these peptides derive from proteolytic processing performed by a variety of peptidases involved in several cellular processes including tissue remodeling, membrane receptor editing, cellular secretion, and cellular apoptosis. The amount and complexity of the extracellular degradome/proteome is further increased during inflammatory and degenerative conditions as well as cancer, all conditions associated with increased protease activity. As such, the blood peptidome-degradome has been considered a valuable source of biological information, as a liquid biopsy for identifying plasma-based markers of disease. Notably, quantification of insulin peptides in serum is used as a biomarker for diabetes (Wan et al. 2018), collagen fragments as well as peptides from cartilage proteins, as a marker of osteoporosis and degenerative joint conditions, β-amyloid and TAU peptides for Alzheimer’s disease (Tapiola et al. 2009), and angiotensin II for hypertension (Zuo et al. 2005), to name a few. For cancer peptides, a comprehensive database (http://crdd.osdd.net/raghava/cancerpdf/) has recently been generated that reports peptides mapped in serum and plasma from ~ 30 forms of cancers. The reported degradome/peptidome highlights protein processing and degradation in the tissue environment as biomarkers of cancer-associated activities. An automated technology platform has also been developed at Memorial Sloan-Kettering Cancer Center (MSKCC) to extract and map peptides from patients’ serum. Using robotic automation on a MALDI-TOF target plate, around 600 peptides were identified in a cohort of 27 patients with metastatic thyroid cancer and 32 controls. A statistically significant diverse peptidome could be mapped between the two groups (Villanueva et al. 2006). Similar analyses have mapped degradome/peptidomes in patients with oral, breast, ovarian, colon-rectal cancer as well as metastasis from different malignancies (Antwi et al. 2009b; Bedin et al. 2016; Bery et al. 2014; Fan et al. 2012a; Fredolini et al. 2010; Greening et al. 2017; Liotta and Petricoin 2006; Petricoin et al. 2006; Smith et al. 2014; Yang et al. 2012b; Armandola 2003; Bassani-Sternberg 2018; Fan et al. 2012b). All these analyses point to the importance of the peptidome/degradome, present in biological fluid, as an important tool for biomarker discovery (Petricoin et al. 2006).
Lymph and blood circulation in spleen and lymph nodes
In the paragraphs below, the anatomical structures of spleen and lymph nodes are described. Our goal is to illustrate how lymph and blood flows through these secondary lymphatic organs and how the anatomical structure facilitates the process of clearance and sampling of the blood and lymph proteome/peptidome for immunosurveillance. The variety, complexity, and functionality of the different immune cell populations present in these organs are beyond the goal of this review.
Blood clearance in the spleen
Anatomically the spleen is divided into the red and white pulp (Mebius and Kraal 2005). Since a major role of the spleen is to clear/filtrate the incoming blood, the splenic circulation differs from the classical pattern of arterioles, capillaries, and venules, as present in all the other parenchymal organs (Mebius and Kraal 2005). The red pulp is divided into anatomical regions by connective tissue called the “cords of Billroth.” The cords are formed by a meshwork of fibroblast-like reticular cells supported by extracellular matrix and reticulin fibers without endothelial lining (Mebius and Kraal 2005). The anatomical cavernous spaces of the cords directly receive arterial blood from terminal arterioles and arterial capillaries (Mebius and Kraal 2005). Several macrophages and dendritic cells are present within the cords attached to the extracellular matrix components, whose job it is to filtrate pathogens, abnormal/old/damaged red blood cells from the blood and to sample the overall circulating proteome (Mebius and Kraal 2005; Steiniger and Barth 2000; Qi et al. 2014). From the cords, the blood flows into the venous sinuses, which represent a second system of filters, before entering the venule-end of the splenic circulatory system (Mebius and Kraal 2005). The venous sinusoidal system consists of a network of contractile reticular fibers, composed of actin and myosin-like filaments, known as stress fibers, which run both circumferentially and longitudinally forming a filtration lattice. Elongated endothelial cells, on top of this fenestrated basal membrane, as well as a population of macrophages known as metallophilic macrophages, form this additional filter to ensure no pathogens or damaged red blood cells re-enter the general circulation (Mebius and Kraal 2005; Qi et al. 2014).
The spleen white pulp contains around 30% of the total lymphocyte population which are structured around a central arteriole as “periarteriolar lymphocyte sheaths” (PALS). Most of the T cells are in the inner part of the PALS whereas B cells and plasma cells are in the outer PALS. In the periarteriolar areas, T cells interact with dendritic cells and B cells. Next to the PALS, bona fide B cell follicles are present where clonal expansion of B cells, isotype switching, and somatic hypermutation occurs (Mebius and Kraal 2005). Anatomical integrity of these areas is controlled by a complex of chemokine gradients (CXCL13, CCL19, CCL21) and their respective receptors which guide T and B cell trafficking and localization (Mebius and Kraal 2005). Altogether PALS and B cell follicles are surrounded by a corona-like structure, called the marginal zone, which also contains B cells, the marginal zone macrophages, and different dendritic cell subsets (Mebius and Kraal 2005). The marginal zone is located between the white and red pulp and is an important transit area for cells entering the PALS from the blood stream.
PALS and B cell follicles resemble the anatomical structures present in the lymph node albeit an important difference is that the spleen is void of afferent lymphatics. As such, the lymph does not circulate in the splenic parenchyma and blood filtration is the primary immunological function of the spleen. On the other hand, structures similar to efferent lymphatics have been described in the spleen as an exit way for T, B, and dendritic cells to leave the white pulp and re-circulate into the lymphatic system (Guyton and Coleman 1968). These lymphatic vessels, present in the T and B areas of the white pulp, have been described flowing from the outer to the inner PALS, running in parallel to the arteriole and draining into the pancreatic-splenic lymph nodes (Guyton and Coleman 1968). From there, the lymph flows into the intestinal lymph trunk, which then enters the cisterna chyli and finally drains into the thoracic duct.
Lymph clearance in the lymph nodes
During the past few years, new research has elucidated how the interstitial fluid enters the initial lymphatics to form lymph. It was originally proposed, and recently experimentally proven, that tissue movement transiently increases interstitial pressure, generating a suction force that facilitates drainage into the open-ended lymphatics (Guyton and Coleman 1968). These initial lymphatics do not contract whereas the downstream collecting lymphatics propel the lymph forward through a Ca++-initiated contraction of smooth muscle present in the vessel wall. Additionally, the presence of a one-way valve separating anatomical segments of the vessels at equal distance (each segment is called a lymphangion) synergizes with the vessel pumping activity favoring lymph movement towards the lymph node (Santambrogio 2013).
Several studies have indicated that subcutaneously injected fluorochrome-labeled proteins or particles reach the draining node within minutes after injection, signifying the efficiency of the lymphatic circulation in transporting soluble and particulate material to the regional lymph nodes (Santambrogio 2013). Additionally, subsets of dendritic cells that patrol peripheral organs also enter the lymphatics, following a CCR7- CCL21 gradient into the lymph node (Russo et al. 2016). These afferent lymphatic vessels, draining well-defined anatomical regions, enter through the lymph nodal capsule into the sub-capsular sinuses, which are pool-like areas where the lymph flows and is filtrated by the macrophages and dendritic cells lining the walls of the sinuses (Clement et al. 2011). CD11b+CD169+MHCII+ macrophages and dendritic cells have been characterized on the floor of the sub-capsular and medullary sinuses, that act as “flypaper” to capture incoming pathogens for T and B cell presentation. These cells function as pivotal gatekeepers, which prevent pathogen dissemination (Junt et al. 2007). From the sinuses, the lymph travels along two possible routes; particulate material and proteins with a molecular weight above 80 kDa flow from the sub-cortical and medullary sinuses into the efferent lymphatic to the next lymph node, whereas proteins and small molecules below 80 kDa enter the conduit system. The conduit system comprises a series of 100–200 nm diameter channels, within the nodal T cell areas, formed by a central pillar of collagens I and V and peripheral walls formed by perlecan, fibronectin and laminins (Drumea-Mirancea et al. 2006; Gretz et al. 2000; Moussion and Sixt 2013; Roozendaal et al. 2009; Sixt et al. 2005). These channels physically connect the sub-cortical and para-cortical regions of the node with the medullary spaces and the high endothelial venule. Low molecular weight proteins and small molecules passing through the conduit will encounter dendritic cells, scattered throughout the T cell areas, whose dendrites directly penetrate the conduit system (Drumea-Mirancea et al. 2006; Gretz et al. 2000; Moussion and Sixt 2013; Roozendaal et al. 2009; Sixt et al. 2005).
Through this highly regulated size exclusion mechanism, two fundamentally important functions of the lymph node are achieved: fluid homeostasis and pathogen immunosurveillance. Indeed, the vast majority of water/fluid from the interstitial fluid and pre-nodal lymph will pass through the conduit and flow directly into the high endothelial venule as a mechanism to control body fluid homeostasis (Jamalian et al. 2017). On the other hand, particulate materials and pathogens are excluded from the conduit as a safeguard mechanism to avoid bacteria/viruses entering the bloodstream. Pathogens that will not be phagocytized by the dendritic cells and macrophages present in the sub-cortical and medullary sinuses will exit through the efferent lymphatic into another lymph node (Clement et al. 2011). Indeed in humans, the 600–800 lymph nodes present throughout the body are organized in chains of 6–8 nodes to ensure proper pathogen clearance. As such, the lymph nodes act as a sieve that uses size exclusion as a mechanism to capture the self and non-self proteome for immunosurveillance.
A recent quantitative analysis of the nodal clearance capacity, which utilized state-of-the-art, label-free quantitative (LFQ) proteomics complemented by tandem mass tag isotope labeling, was used to identify proteomic changes in the pre- and post-nodal mesenteric lymph (Clement et al. 2018). The proteomic data were supplemented with analysis of lymphatic transport of fluorochrome-labeled proteins, bacteria, and beads, by direct cannulation of pre-nodal lymphatics followed by post-nodal collection and quantification. The picture that emerged is that lymph nodes act as very efficient filtration organs, with concentration-dependent filtration efficiency across molecular sizes (Clement et al. 2018). Indeed, by direct lymphatic cannulation with injection of titrated amounts of fluorophore-labeled proteins, at a physiological flow pressure, it was determined that for protein concentrations up to 5 μg/ml, corresponding to the concentrations of all tissue-specific antigens, the efficiency of protein clearance upon nodal passage was up to 80–90%. For much higher protein concentrations, corresponding to the ones normally observed for proteins involved in the maintenance of oncotic pressure, efficiency of protein clearance upon nodal passage was lower (Clement et al. 2018). Similarly, the lymph node could efficiently clear a pathogen load up to a million bacteria, but when ten million bacteria were injected into the pre-nodal lymph, around 30% of the pathogen load could be observed in the post-nodal lymph (Clement et al. 2018).
Proteases generating the blood and lymph peptidome
Protease genes comprise 1.7% of the human expressed genome but despite their relevance in a variety of biological activities, many of the proteases, their substrates, activators, and inhibitors are yet to be fully characterized. Proteases can be divided into five catalytic classes including metallo, serine, cysteine, threonine, and aspartic proteases. Each class is further divided into different families, mostly based on primary amino acid sequence and three-dimensional structure (MEROPS database). During the last few years, there has been a keen interest in the analysis of the proteases, their inhibitors, and degradation substrates in serum and lymph. The overall goal of these liquid biopsies is to map changes during physiological and pathological conditions, which can help identify early stage of disease and monitor its progression. Indeed, albeit a degradome can be mapped in both fluids under physiological conditions, its composition changes both qualitatively and quantitatively in pathological conditions generating degradomic maps, and peptide hot-spots as potential disease biomarkers. In the paragraphs below, we review current literature on the known family of proteases generating the degradome/peptidome in the blood and lymph in physiological and pathological conditions. Although all the below mentioned enzymes are involved in several pathological processes, our analysis will only report on enzymatic processing in relationship to the blood and lymph peptidome.
MMPs and ADAMs
During physiological conditions, the lymphatic fluid degradome is highly represented in byproducts derived from the action of collagenolytic matrix metalloproteinase (MMPs) and disintegrin metalloproteinases (ADAMs), which are involved in extracellular matrix remodeling in parenchymal organs.
There are over 20 MMPs and over 40 ADAMs family members in the human genome. MMP proteolysis forms space for cell migration by cleaving intercellular junctions or the basement membrane, regulate tissue morphology through proteolysis of cell-cell junctions, and by cleavage can activate/deactivate signaling molecules (Sternlicht and Werb 2001). For example, MMP9 cleavage of collagen IV α3 chain has been shown to generate an anti-angiogenic peptide which binds to the αvβ3 integrin (Hamano 2003). As such, the majority of the generated peptidome/degradome consists of collagens, laminins, elastins, fbronectins, proteoglycans, and surface molecules, such as cadherins, and integrins. Indeed, cleavage products from all these proteins have been extensively mapped in the lymph and plasma (Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; Shen et al. 2010b; Clement et al. 2018; Farrah et al. 2011).
In pathological conditions, MMPs and ADAMs have been closely associated with cancer growth, invasion, and metastasis. Advancement in activity-based profiling of protease function has enabled tracking MMPs and ADAMs tissue proteolytic activities in different stages of cancer (Kato et al. 2005). Additionally, transgenic mice harboring gene deletion of individual MMPs have shown how these proteases facilitate neoplastic progression by degrading the extracellular matrix structure, processing cell-cell and cell-matrix adhesion molecules. Indeed, MMP2, MMP13, and 14 have all been implicated in pericellular tumor proteolysis (Affara et al. 2009). Collagens, laminins, growth factors, and cytokine processing have all been linked to MMP3, 7, 8, and 11 in different cancer models spanning ovarian, liver cancer, intestinal adenomas, and squamous cell carcinoma (Affara et al. 2009; Rudensky et al. 1991). Besides aiding tumor invasion, MMPs also contribute to tumor growth by VEGF cleavage that alters tissue neo-angiogenesis (Affara et al. 2009).
Increased levels of active MMP9 and MMP2 have also been found in the CSF and sera of patients with multiple sclerosis (MS) prior to a relapse albeit their specific substrates in the disease have not yet been characterized (Scarisbrick 2008). Similarly, active ADAMs such as ADAM-17 and its processing substrates (TNF-α and CX3CL1) have been found in the serum of patients with relapsing MS (Scarisbrick 2008).
Cleavage products following regulated-proteolysis of membrane receptors have also been found released in the interstitial fluid/lymph (Clement et al. 2013; Clement et al. 2016; Clement et al. 2010; Clement et al. 2011; Clement and Santambrogio 2013; Clement et al. 2018), including products derived from IL-6R and IL-11R proteolysis by ADAM10 and ADAM17, which releases peptide fragments of around 20 amino acids (Goth et al. 2015), similarly an 11 amino acid fragment is released from proteolysis of the TNF-R (Mukaro et al. 2018), or fragments released following proteolysis by α-β and γ secretases of the IL-1R and IL-2R, EGFR, TLR-superfamily, and other chemokines or cytokines (Levine 2008; Blobel 2005; Huovila et al. 2005; Garton et al. 2006).
Serine proteases
Serine proteases are a large family of proteases whose most notable members include chymotrypsin, trypsin, elastase, clotting factors (Xa, XI, thrombin, plasmin, plasminogen activators), kallikreins, granzymes, cathepsin G, and factors from the complement cascade (C1r, C1s, and C3 convertases). Although the degradome of some of these proteases is only present in biological fluids in pathological conditions, other enzymes of this family are active in a wide variety of physiological functions. For example, a degradome derived from the activity of clotting factors is physiologically present in both serum and lymph (Clement et al. 2013; Clement et al. 2016; Clement et al. 2010; Meng and Veenstra 2007; Farrah et al. 2011; Anderson et al. 2004; Omenn et al. 2005). Similarly, kallikrein-related degradomes, due to their involvement in fluid and electrolytes regulation, have also been mapped in the lymph (Clement et al. 2016).
On the other hand, serine proteases, which are essential mediators of gastrointestinal physiology, serving digestive purposes as well as mucosal tissue homeostasis (Denadai-Souza et al. 2018), are only found in serum and plasma during pathological conditions. Increased plasma serine protease activity has been observed in inflammatory bowel disease, Ulcerative Colitis, and Crohn’s disease (Denadai-Souza et al. 2018). The pathological relevance of these enzymes is highlighted by the finding that re-establishment of proteolytic homeostasis, using protease inhibitors, reduces the severity of these conditions (Denadai-Souza et al. 2018). Degradation products from trypsin, chymotrypsin, elastase, and other serine proteases have been mapped in the lymph collected from patients or mice models of bowel disease (D'Alessandro et al. 2014; Dzieciatkowska et al. 2011; Benoit and Zawieja 1992).
Three main pathways characterize the complement system: classical, lectin, and alternative. Although the classical and lectin pathways generally are activated following recognition of exogenous/pathogenic materials, the alternative pathway is constitutively active at low levels in physiological conditions (Noris and Remuzzi 2013). This is often referred to as the tickover mechanism and allows the system to stay primed for rapid activation (Noris and Remuzzi 2013). Indeed, a degradome for the alternative pathway has been mapped in lymph and plasma collected from healthy individuals (Clement et al. 2013; Clement et al. 2016; Clement et al. 2010; Meng and Veenstra 2007; Farrah et al. 2011; Anderson et al. 2004; Omenn et al. 2005). On the other hand the activity of the complement cascade is highly increased in acute and chronic inflammatory conditions as well as degenerative pathologies in every parenchymal organ (Antwi et al. 2009b; Bedin et al. 2016; Bery et al. 2014; Fredolini et al. 2010; Greening et al. 2017; Liotta and Petricoin 2006; Petricoin et al. 2006; Armandola 2003; Affara et al. 2009).
The serine proteases subfamily of elastase, tryptase, proteinase 3, and Cathepsin G are mostly active during inflammation when they are released from mast cells and granulocytes and rapidly degrade connective tissue proteins (Korkmaz et al. 2010).
Cysteine proteases
Cysteine proteases include some of the Cathepsin family members, Caspases and Calpains. Cathepsins (F,K,L,O,S,V,X and W) are endopeptidases, whereas cathepsins B, H, X, and C possess exopeptidase activity. They are mostly found in endolysosomal compartments and at least some members are secreted extracellularly. Under physiological conditions, an extracellular degradome has been associated with the role of cathepsins L in skin and hair follicle morphogenesis (Roth et al. 2000) and cardiac remodeling (Stypmann et al. 2002) and a cathepsin K role in bone resorption (Saftig et al. 1998). Cathepsins are up-regulated and secreted in almost every form of cancer, where they are generally associated with poor prognosis. The degradome associated with their functional activity relates to neoangiogenesis (laminin, collagen IV, fibronectin proteolysis, processing of angiogenic inhibitors, or proangiogenic factors), cell proliferation and invasiveness (ECM degradation, activation of MMPs, processing of cell-cell adhesion) (Rudensky et al. 1991; Dabrosin et al. 2004; Frosch et al. 1999; Ito et al. 2000; Keppler et al. 1994). Additionally, during acute and chronic inflammatory conditions, macrophages, dendritic cells, and also non-immune cells secrete active Cathepsins, which contribute to the tissue degradome (Caglic et al. 2013; Poole et al. 1976; Moon et al. 2016; Mohamed et al. 2010; Yan et al. 2016).
A Caspase-generated degradome/peptidome is also observed following physiological tissue apoptosis and presence of apoptotic cells in the lymph (Olszewski 2001). Apoptosis occurs physiologically, as a homeostatic mechanism to maintain cell populations in tissues and it is estimated that around 10 billion cells are made each day to balance the ones dying by apoptosis (Renehan et al. 2001). Peptides derived from Caspase 3 processing have been mapped to several intracellular proteins as detailed in the paragraph above (Clement et al. 2016; Clement et al. 2010). Both inflammatory (Caspases 1-4-5 in humans and 1-11 and 12 in mice) and apoptotic Caspases (initiators 2-8-9-10 and executioners 3-6-7) are critically active in inflammatory responses where they participate in maturing pro-inflammatory cytokines (IL-1β and IL-18), and as the major executioners of cell death. As such, a Caspase degradome has been mapped in the plasma during acute and chronic inflammatory conditions such as myocardial infarction, chronic hepatitis C, and nonalcoholic Fatty liver disease, COPD and hemorrhage (Soto-Hernandez 2008) (Agosto et al. 2011; Papatheodoridis et al. 2010; Hacker et al. 2009).
Calpains are non-lysosomal cytosolic proteases mostly involved in cleavage of intracellular proteins involved in cellular motility and trafficking. Calpains can also be secreted by immune cells and are present on the plasma membrane where EGF activates calpain 2 via ERK/mitogen-activated protein kinases to facilitate productive locomotion of adherent cells (Shao et al. 2006; Pontremoli et al. 1985; Kuboki et al. 1990). As such, Calpain degradation products have been mapped in the lymph and eluted from DC MHC II (Clement et al. 2016). Notably, inflammatory conditions increase Calpain secretion from activated macrophages and T cells and tissue specific antigens, such as myelin proteins (Scarisbrick 2008), have been shown to be processed by Calpains.
Aspartic proteases
Cathepsin D and E are endo-lysosomal aspartic proteases. A cathepsin D degradome has been previously reported in the lymph; likely released from apoptotic cells or during exosomal exit following fusion of the multivesicular late endosomes with the plasma membrane (Clement et al. 2016; Wan et al. 2018). Elevated plasma levels of Cathepsin D have been reported in several inflammatory and neoplastic conditions. In non-alcoholic steatohepatitis, plasma levels of Cathepsin D directly correlate with disease development and regression (Walenbergh et al. 2016). Plasma Cathepsin D has also been found elevated following myocardial infarction, hepatic carcinoma, breast cancer, and inflammatory joint disease associated with cartilage degradation (Naseem et al. 2005; Brouillet et al. 1991; Duffy et al. 1991; Swingler et al. 2009).
Threonine proteases
The Proteasome is the enzyme complex harboring the threonine class of proteases and its role in MHC I and MHC II-cross presentation has been very well characterized. In physiological conditions, low levels of circulating proteasomes have been observed in normal human blood (Sixt and Dahlmann 2008). Also few proteasome-cleaved peptides have been mapped in the lymph. Likely, these peptides are either secreted from parenchymal or immune cells (Wan et al. 2018) or released from the cytosol of apoptotic cells (Olszewski 2001). On the other hand, high levels of proteasomal activity have been mapped in the plasma of patients with solid tumors and hemopoietic malignancies, metastatic melanoma, different kinds of trauma, rheumatoid arthritis and SLE (Sixt and Dahlmann 2008; Stoebner et al. 2005; Matuszczak et al. 2015; Zoeger et al. 2006; Lavabre-Bertrand et al. 2001).
Lymph Peptidome and Degradome contribution to the MHC I and MHC II immunopeptidome
Research in the last 30 years has clearly established that MHC I and MHC II molecules sample both exogenous and endogenous antigens. The former paradigm that MHC I would only bind cytosolic antigens and MHC II would sample phagocytized proteins is now rectified through the discovery of cross-presentation and autophagy. It is now apparent that both MHC molecules intersect intracellular and extracellular pathways (Roche and Furuta 2015; Santambrogio et al. 1999a; Santambrogio et al. 1999b; Geng et al. 2018). As such, many more non-canonical pathways have been added to the canonical MHC-I proteasome and MHC-II- endosomes pathway. Additionally, from early analysis in which only a few MHC peptides could be reliably fragmented and analyzed, several groups have now reported very large sets of naturally processed peptides (Clement et al. 2016; Antwi et al. 2009a; Stern and Santambrogio 2016; Tan et al. 2011; Caron et al. 2015; Fugmann et al. 2017; Bassani-Sternberg et al. 2016; Loffler et al. 2018; Neidert et al. 2018; Shao et al. 2018; Di Marco et al. 2017a; Di Marco et al. 2017b; Schuster et al. 2017; Kowalewski et al. 2015; Rammensee et al. 1999). The increased number of mapped epitopes associated with the availability of incrementally sophisticated software programs that allow mapping of the processing proteases (MEROPS, BRENDA, CutDB) or the analysis of post-translational modifications has allowed the field to move from a merely compilative analysis of the MHC-eluted immunopeptidome to a more mechanistic analysis of how differential MHC-immunopeptidomes contribute to immunosurveillance. We recently sequenced over 3000 HLA-DR1-eluted peptides derived from ex vivo purified dendritic cells (Clement et al. 2016). The eluted immunopeptidome was analyzed using a series of databases comprising experimentally determined peptide cleavage sites. The analysis underscored the wide variety of enzymes and processing pathways that contribute to the MHC II immunopeptidome; besides the endosomal processing pathway that generates Cathepsins-cleaved peptides, tissue-specific proteases, including MMPs, ADAMs, Caspases, Granzymes among many others, were shown to add to the MHC II self peptidome. Some of the eluted peptides overlapped with those found in the lymph and did not derive from cathepsin processing (Clement et al. 2016). Overall, this ensures that dendritic cells present a broad self-peptidome which includes epitopes generated by a multiplicity of proteases with the ultimate goal to present the sampled environment to patrolling T cells (Clement et al. 2016).
Nevertheless, novel epitopes can be generated during pathological conditions through different mechanisms including (i) up-regulation and down-regulation of various tissue proteases which contribute to changes in protein processing and sequence of processed epitopes, (ii) changes in the redox microenvironment which favors protein post-translational modifications, such as carbonylation, glycation, and nitrosylation and (iii) changes in the expression of proteins of the antigen processing machinery, such as HLA-DM and HLA-DO, which contribute to peptide selection mechanisms (Kim and Sadegh-Nasseri 2015).
Proteomic analysis of blood and lymph under physiological or pathological conditions has clearly underscored how the degradome signature can change; the next challenge is to determine whether distinctive degradomic signatures can be specifically associated to disease states and used as liquid biopsy for diagnostic and therapeutic purposes. Additionally, how changes in tissue-specific proteins and proteases affect epitope processing, formation of neo-epitopes, and epitope copy number presented by MHC I and MHC II molecules are still questions to be addressed.
An additional aspect arising from these studies is the influence of drugs on the MHC ligandome. For example, gemcitabine, a cytostatic drug used in cancer chemotherapy, not only increases the density of MHC I molecules on the cell surface but also alters immunoproteasome composition and the MHC ligandome (Gravett et al. 2018). For another example, carfilzomib alters the HLA-presented peptidome of myeloma cells and impairs presentation of peptides with aromatic C-termini (Kowalewski et al. 2016).
Similarly, tissue redox changes, associated with acute and chronic inflammatory states, degenerative conditions, and cancer have been extensively mapped. During these conditions, the cellular and extracellular proteome is qualitatively modified by oxidation (carbonylation, nytrosilation, formylation), glycation (carboxymethylysine or carboxymethylarginine) and lipoxidation (4-hydroxynonenal (HNE), malonaldehyde), to name a few of the over 400 possible modifications. Both MHC classes are found to present phosphorylated peptides (Meyer et al. 2009), and for MHC class I ligands glycosylations have also been reported (Kastrup et al. 2000).
Although most amino acids are susceptible to oxidation by these reactive species, lysine, arginine, methionine, and cysteine are the most susceptible due to the presence of free amino and sulfhydryl groups on their side chains. For example, in our extensive database of HLA ligands from human tumor and normal tissues, around 8% of HLA class II and 6% of HLA class I ligand entries are oxidized at one or more amino acids (Neumann et al. 2004; Wagner et al. 2003). Other notable modifications are arginine citrullination, which has been linked to autoimmune diseases such as rheumatoid arthritis (Fox 2015), peptide oxidative cleavage for generation of neo-epitopes and autoimmunity (Sadegh-Nasseri and Kim 2015), and peptide glycation in diabetes and metabolic syndrome (Horvat and Jakas 2004; Walcher and Marx 2009). The full effects of protein modifications on the MHC I and MHC II antigen processing machinery, peptide processing loading affinity and presentation need to be further evaluated. Additionally, how peptides and specific PTM can be exploited diagnostically and therapeutically, in cancer, autoimmune and degenerative diseases are also an important open question.
Conclusions
Overall, the literature from the last decade has solidified the notion that plasma and lymph provides a rich degradome/peptidome that could facilitate the discovery of novel biomarkers that reflect disease status (Clement et al. 2011; Dzieciatkowska et al. 2014; Ling et al. 2010; Quesada et al. 2009; Petricoin et al. 2006; Meng and Veenstra 2007; Anderson et al. 2004; Omenn et al. 2005). In contrast to organ biopsies, which are limited to a small number of cells, liquid biopsy can provide a more accurate fingerprint of the overall organ physiological or pathological state. In particular, unlike the blood, liquid biopsy of lymphatic fluid can provide a specific signature of the organ from which it drains (Santambrogio 2013). How to diagnostically use the blood and lymphatic fluid peptidome/degradome and how to therapeutically exploit it for immunotherapy design are important challenges for the future.
References
Affara NI, Andreu P, Coussens LM (2009) Delineating protease functions during cancer development. Methods Mol Biol 539:1–32
Agosto M, Azrin M, Singh K, Jaffe AS, Liang BT (2011) Serum caspase-3 p17 fragment is elevated in patients with ST-segment elevation myocardial infarction: a novel observation. J Am Coll Cardiol 57:220–221
Anderson NL et al (2004) The human plasma proteome: a nonredundant list developed by combination of four separate sources. Mol Cell Proteomics 3:311–326
Antwi K, Hanavan PD, Myers CE, Ruiz YW, Thompson EJ, Lake DF (2009a) Proteomic identification of an MHC-binding peptidome from pancreas and breast cancer cell lines. Mol Immunol 46:2931–2937
Antwi K, Hostetter G, Demeure MJ, Katchman BA, Decker GA, Ruiz Y, Sielaff TD, Koep LJ, Lake DF (2009b) Analysis of the plasma peptidome from pancreas cancer patients connects a peptide in plasma to overexpression of the parent protein in tumors. J Proteome Res 8:4722–4731
Armandola EA (2003) Proteome profiling in body fluids and in cancer cell signaling. Med Gen Med 5:18
Aukland K, Kramer GC, Renkin EM (1984) Protein concentration of lymph and interstitial fluid in the rat tail. Am J Phys 247:H74–H79
Bassani-Sternberg M (2018) Mass spectrometry based Immunopeptidomics for the discovery of cancer neoantigens. Methods Mol Biol 1719:209–221
Bassani-Sternberg M, Bräunlein E, Klar R, Engleitner T, Sinitcyn P, Audehm S, Straub M, Weber J, Slotta-Huspenina J, Specht K, Martignoni ME, Werner A, Hein R, H. Busch D, Peschel C, Rad R, Cox J, Mann M, Krackhardt AM (2016) Direct identification of clinically relevant neoepitopes presented on native human melanoma tissue by mass spectrometry. Nat Commun 7:13404
Bedin C, Crotti S, Ragazzi E, Pucciarelli S, Agatea L, Tasciotti E, Ferrari M, Traldi P, Rizzolio F, Giordano A, Nitti D, Agostini M (2016) Alterations of the plasma Peptidome profiling in colorectal cancer progression. J Cell Physiol 231:915–925
Benoit JN, Zawieja DC (1992) Effects of f-Met-Leu-Phe-induced inflammation on intestinal lymph flow and lymphatic pump behavior. Am J Phys 262:G199–G202
Bery A, Leung F, Smith CR, Diamandis EP, Kulasingam V (2014) Deciphering the ovarian cancer ascites fluid peptidome. Clin Proteomics 11:13
Bhalla S, Verma R, Kaur H, Kumar R, Usmani SS, Sharma S, Raghava GPS (2017) CancerPDF: a repository of cancer-associated peptidome found in human biofluids. Sci Rep 7(1511):1511
Blobel CP (2005) ADAMs: key components in EGFR signalling and development. Nat Rev Mol Cell Biol 6:32–43
Bournazou I, Pound JD, Duffin R, Bournazos S, Melville LA, Brown SB, Rossi AG, Gregory CD (2009) Apoptotic human cells inhibit migration of granulocytes via release of lactoferrin. J Clin Invest 119:20–32
Brouillet JP, Hanslick B, Maudelonde T, Pivat MT, Grenier J, Blanc F, Rochefort H (1991) Increased plasma cathepsin D concentration in hepatic carcinoma and cirrhosis but not in breast cancer. Clin Biochem 24:491–496
Buchbinder EI, Flaherty KT (2016) Biomarkers in melanoma: lessons from translational medicine. Trends Cancer 2:305–312
Caglic D et al (2013) The proinflammatory cytokines interleukin-1alpha and tumor necrosis factor alpha promote the expression and secretion of proteolytically active cathepsin S from human chondrocytes. Biol Chem 394:307–316
Cal S, Moncada-Pazos A, Lopez-Otin C (2007) Expanding the complexity of the human degradome: polyserases and their tandem serine protease domains. Front Biosci 12:4661–4669
Caron E, Kowalewski DJ, Chiek Koh C, Sturm T, Schuster H, Aebersold R (2015) Analysis of major histocompatibility complex (MHC) Immunopeptidomes using mass spectrometry. Mol Cell Proteomics 14:3105–3117
Clement CC, Santambrogio L (2013) The lymph self-antigen repertoire. Front Immunol 4(424)
Clement CC, Cannizzo ES, Nastke MD, Sahu R, Olszewski W, Miller NE, Stern LJ, Santambrogio L (2010) An expanded self-antigen peptidome is carried by the human lymph as compared to the plasma. PLoS One 5:e9863
Clement CC, Rotzschke O, Santambrogio L (2011) The lymph as a pool of self-antigens. Trends Immunol 32:6–11
Clement CC, Aphkhazava D, Nieves E, Callaway M, Olszewski W, Rotzschke O, Santambrogio L (2013) Protein expression profiles of human lymph and plasma mapped by 2D-DIGE and 1D SDS-PAGE coupled with nanoLC-ESI-MS/MS bottom-up proteomics. J Proteome 78:172–187
Clement CC, Becerra A, Yin L, Zolla V, Huang L, Merlin S, Follenzi A, Shaffer SA, Stern LJ, Santambrogio L (2016) The dendritic cell major histocompatibility complex II (MHC II) Peptidome derives from a variety of processing pathways and includes peptides with a broad spectrum of HLA-DM sensitivity. J Biol Chem 291:5576–5595
Clement CC, Wang W, Dzieciatkowska M, Cortese M, Hansen KC, Becerra A, Thangaswamy S, Nizamutdinova I, Moon JY, Stern LJ, Gashev AA, Zawieja D, Santambrogio L (2018) Quantitative profiling of the lymph node clearance capacity. Sci Rep 8:11253
Dabrosin C, Johansson AC, Ollinger K (2004) Decreased secretion of Cathepsin D in breast cancer in vivo by tamoxifen: mediated by the mannose-6-phosphate/IGF-II receptor? Breast Cancer Res Treat 85:229–238
D'Alessandro A, Gevi F, Zolla L (2011) A robust high resolution reversed-phase HPLC strategy to investigate various metabolic species in different biological models. Mol BioSyst 7:1024–1032
D'Alessandro A et al (2014) Dynamic changes in rat mesenteric lymph proteins following trauma using label-free mass spectrometry. Shock 42:509–517
De Paiva CS et al (2009) Cleavage of functional IL-2 receptor alpha chain (CD25) from murine corneal and conjunctival epithelia by MMP-9. J Inflamm (Lond) 6:31
Denadai-Souza A, Bonnart C, Tapias NS, Marcellin M, Gilmore B, Alric L, Bonnet D, Burlet-Schiltz O, Hollenberg MD, Vergnolle N, Deraison C (2018) Functional proteomic profiling of secreted serine proteases in health and inflammatory bowel disease. Sci Rep 8(7834):7834
Di Marco M et al (2017a) Unveiling the peptide motifs of HLA-C and HLA-G from naturally presented peptides and generation of binding prediction matrices. J Immunol 199:2639–2651
Di Marco M, Peper JK, Rammensee HG (2017b) Identification of immunogenic epitopes by MS/MS. Cancer J 23:102–107
Drumea-Mirancea M et al (2006) Characterization of a conduit system containing laminin-5 in the human thymus: a potential transport system for small molecules. J Cell Sci 119:1396–1405
Duffy MJ, Brouillet JP, Reilly D, McDermott E, O'Higgins N, Fennelly JJ, Maudelonde T, Rochefort H (1991) Cathepsin D concentration in breast cancer cytosols: correlation with biochemical, histological, and clinical findings. Clin Chem 37:101–104
Dzieciatkowska M, Wohlauer MV, Moore EE, Damle S, Peltz E, Campsen J, Kelher M, Silliman C, Banerjee A, Hansen KC (2011) Proteomic analysis of human mesenteric lymph. Shock 35:331–338
Dzieciatkowska M, D’Alessandro A, Moore EE, Wohlauer M, Banerjee A, Silliman CC, Hansen KC (2014) Lymph is not a plasma ultrafiltrate: a proteomic analysis of injured patients. Shock 42:485–498
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2:161–174
El Azreq MA, Naci D, Aoudjit F (2012) Collagen/beta1 integrin signaling up-regulates the ABCC1/MRP-1 transporter in an ERK/MAPK-dependent manner. Mol Biol Cell 23:3473–3484
Fan NJ, Gao CF, Zhao G, Wang XL, Liu QY (2012a) Serum peptidome patterns of breast cancer based on magnetic bead separation and mass spectrometry analysis. Diagn Pathol 7:45
Fan NJ et al (2012b) Serum peptidome patterns of colorectal cancer based on magnetic bead separation and MALDI-TOF mass spectrometry analysis. J Biomed Biotechnol 985020, 2012
Fang JF, Shih LY, Yuan KC, Fang KY, Hwang TL, Hsieh SY (2010) Proteomic analysis of post-hemorrhagic shock mesenteric lymph. Shock 34:291–298
Farrah T, Deutsch EW, Omenn GS, Campbell DS, Sun Z, Bletz JA, Mallick P, Katz JE, Malmström J, Ossola R, Watts JD, Lin B, Zhang H, Moritz RL, Aebersold R (2011) A high-confidence human plasma proteome reference set with estimated concentrations in PeptideAtlas. Mol Cell Proteomics 10:M110 006353
Fiedler GM, Leichtle AB, Kase J, Baumann S, Ceglarek U, Felix K, Conrad T, Witzigmann H, Weimann A, Schutte C, Hauss J, Buchler M, Thiery J (2009) Serum peptidome profiling revealed platelet factor 4 as a potential discriminating Peptide associated with pancreatic cancer. Clin Cancer Res 15:3812–3819
Fox DA (2015) Citrullination: a specific target for the autoimmune response in rheumatoid arthritis. J Immunol 195:5–7
Fredolini C, Meani F, Luchini A, Zhou W, Russo P, Ross M, Patanarut A, Tamburro D, Gambara G, Ornstein D, Odicino F, Ragnoli M, Ravaggi A, Novelli F, Collura D, D’Urso L, Muto G, Belluco C, Pecorelli S, Liotta L, Petricoin EF (2010) Investigation of the ovarian and prostate cancer peptidome for candidate early detection markers using a novel nanoparticle biomarker capture technology. AAPS J 12:504–518
Frosch BA, Berquin I, Emmert-Buck MR, Moin K, Sloane BF (1999) Molecular regulation, membrane association and secretion of tumor cathepsin B. APMIS 107:28–37
Fugmann T, Sofron A, Ritz D, Bootz F, Neri D (2017) The MHC class II Immunopeptidome of lymph nodes in health and in chemically induced colitis. J Immunol 198:1357–1364
Garnotel R, Monboisse JC, Randoux A, Haye B, Borel JP (1995) The binding of type I collagen to lymphocyte function-associated antigen (LFA) 1 integrin triggers the respiratory burst of human polymorphonuclear neutrophils. Role of calcium signaling and tyrosine phosphorylation of LFA 1. J Biol Chem 270:27495–27503
Garton KJ, Gough PJ, Raines EW (2006) Emerging roles for ectodomain shedding in the regulation of inflammatory responses. J Leukoc Biol 79:1105–1116
Geho DH, Liotta LA, Petricoin EF, Zhao W, Araujo RP (2006) The amplified peptidome: the new treasure chest of candidate biomarkers. Curr Opin Chem Biol 10:50–55
Geng J, Altman JD, Krishnakumar S, Raghavan M (2018) Empty conformers of HLA-B preferentially bind CD8 and regulate CD8(+) T cell function. Elife 7
Goldfinch GM, Smith WD, Imrie L, McLean K, Inglis NF, Pemberton AD (2008) The proteome of gastric lymph in normal and nematode infected sheep. Proteomics 8:1909–1918
Goth CK, Halim A, Khetarpal SA, Rader DJ, Clausen H, Schjoldager KTBG (2015) A systematic study of modulation of ADAM-mediated ectodomain shedding by site-specific O-glycosylation. Proc Natl Acad Sci U S A 112:14623–14628
Gravett AM, Trautwein N, Stevanovic S, Dalgleish AG, Copier J (2018) Gemcitabine alters the proteasome composition and immunopeptidome of tumour cells. Oncoimmunology 7:e1438107
Greening DW, Kapp EA, Simpson RJ (2017) The Peptidome comes of age: mass spectrometry-based characterization of the circulating cancer Peptidome. Enzymes 42:27–64
Gretz JE, Norbury CC, Anderson AO, Proudfoot AE, Shaw S (2000) Lymph-borne chemokines and other low molecular weight molecules reach high endothelial venules via specialized conduits while a functional barrier limits access to the lymphocyte microenvironments in lymph node cortex. J Exp Med 192:1425–1440
Guyton AC, Coleman TG (1968) Regulation on interstitial fluid volume and pressure. Ann N Y Acad Sci 150:537–547
Hacker S, Lambers C, Pollreisz A, Hoetzenecker K, Lichtenauer M, Mangold A, Niederpold T, Hacker A, Lang GÃ, Dworschak M, Vukovich T, Gerner C, Klepetko W, Ankersmit HJ (2009) Increased soluble serum markers caspase-cleaved cytokeratin-18, histones, and ST2 indicate apoptotic turnover and chronic immune response in COPD. J Clin Lab Anal 23:372–379
Hamano, Y., et al. Physiological levels of tumstatin, a fragment of collagen IV alpha3 chain, are generated by MMP-9 proteolysis and suppress angiogenesis via alphaV beta3 integrin. Cancer Cell 3, 589–601 (2003)
Hashiguchi T, Tanaka K, Lee LJ, Sasaki K, Natsugoe S, Kawahara KI, Arimura K, Maruyama I (2009) Diagnostic value of serum peptidome analyses for protease activated pathological conditions beyond cancer diagnosis. Med Hypotheses 73:760–763
He K, Wen XY, Li AL, Li T, Wang J, Wang HX, Wang N (2013) Serum peptidome variations in a healthy population: reference to identify cancer-specific peptides. PLoS One 8:e63724
Hood JL (2017) The association of exosomes with lymph nodes. Semin Cell Dev Biol 67:29–38
Horvat S, Jakas A (2004) Peptide and amino acid glycation: new insights into the Maillard reaction. J Pept Sci 10:119–137
Hsiao KC, Shih NY, Fang HL, Huang TS, Kuo CC, Chu PY, Hung YM, Chou SW, Yang YY, Chang GC, Liu KJ (2013) Surface alpha-enolase promotes extracellular matrix degradation and tumor metastasis and represents a new therapeutic target. PLoS One 8:e69354
Huang SK, Hoon DS (2016) Liquid biopsy utility for the surveillance of cutaneous malignant melanoma patients. Mol Oncol 10:450–463
Huang X, Zhou J, Tang R, Han S, Zhou X (2018) Potential significance of Peptidome in human ovarian cancer for patients with ascites. Int J Gynecol Cancer 28:355–362
Huovila AP, Turner AJ, Pelto-Huikko M, Karkkainen I, Ortiz RM (2005) Shedding light on ADAM metalloproteinases. Trends Biochem Sci 30:413–422
Interewicz B, Olszewski WL, Leak LV, Petricoin EF, Liotta LA (2004) Profiling of normal human leg lymph proteins using the 2-D electrophoresis and SELDI-TOF mass spectrophotometry approach. Lymphology 37:65–72
Ito H, Miyazaki M, Nishimura F, Nakajima N (2000) Secretion of extracellular matrix (fibronectin), growth factor (transforming growth factor beta) and protease (cathepsin D) by hepatoma cells. Oncology 58:261–270
Jamalian S, Jafarnejad M, Zawieja SD, Bertram CD, Gashev AA, Zawieja DC, Davis MJ, Moore JE (2017) Demonstration and analysis of the suction effect for pumping lymph from tissue beds at subatmospheric pressure. Sci Rep 7(12080):12080
Jordan JR, Moore EE, Damle SS, Eckels P, Johnson JL, Roach JP, Redzic JS, Hansen KC, Banerjee A (2007) Gelsolin is depleted in post-shock mesenteric lymph. J Surg Res 143:130–135
Junt T, Moseman EA, Iannacone M, Massberg S, Lang PA, Boes M, Fink K, Henrickson SE, Shayakhmetov DM, di Paolo NC, van Rooijen N, Mempel TR, Whelan SP, von Andrian UH (2007) Subcapsular sinus macrophages in lymph nodes clear lymph-borne viruses and present them to antiviral B cells. Nature 450:110–114
Kagami S et al (2001) Requirement for tyrosine kinase-ERK1/2 signaling in alpha 1 beta 1 integrin-mediated collagen matrix remodeling by rat mesangial cells. Exp Cell Res 268:274–283
Kastrup IB, Stevanovic S, Arsequell G, Valencia G, Zeuthen J, Rammensee HG, Elliott T, Haurum JS (2000) Lectin purified human class I MHC-derived peptides: evidence for presentation of glycopeptides in vivo. Tissue Antigens 56:129–135
Kato D et al (2005) Activity-based probes that target diverse cysteine protease families. Nat Chem Biol 1:33–38
Keppler D, Abrahamson M, Sordat B (1994) Secretion of cathepsin B and tumour invasion. Biochem Soc Trans 22:43–49
Kim A, Sadegh-Nasseri S (2015) Determinants of immunodominance for CD4 T cells. Curr Opin Immunol 34:9–15
Klupczynska A, Swiatly A, Hajduk J, Matysiak J, Dyszkiewicz W, Pawlak K, Kokot Z (2016) Identification of serum Peptidome signatures of non-small cell lung cancer. Int J Mol Sci 17:410
Kojima M, Gimenes-Junior JA, Langness S, Morishita K, Lavoie-Gagne O, Eliceiri B, Costantini TW, Coimbra R (2017) Exosomes, not protein or lipids, in mesenteric lymph activate inflammation: unlocking the mystery of post-shock multiple organ failure. J Trauma Acute Care Surg 82:42–50
Kojima M, Gimenes-Junior JA, Chan TW, Eliceiri BP, Baird A, Costantini TW, Coimbra R (2018) Exosomes in postshock mesenteric lymph are key mediators of acute lung injury triggering the macrophage activation via Toll-like receptor 4. FASEB J 32:97–110
Korkmaz B, Horwitz MS, Jenne DE, Gauthier F (2010) Neutrophil elastase, proteinase 3, and cathepsin G as therapeutic targets in human diseases. Pharmacol Rev 62:726–759
Kowalewski DJ et al (2015) HLA ligandome analysis identifies the underlying specificities of spontaneous antileukemia immune responses in chronic lymphocytic leukemia (CLL). Proc Natl Acad Sci U S A 112:E166–E175
Kowalewski DJ, Walz S, Backert L, Schuster H, Kohlbacher O, Weisel K, Rittig SM, Kanz L, Salih HR, Rammensee HG, Stevanović S, Stickel JS (2016) Carfilzomib alters the HLA-presented peptidome of myeloma cells and impairs presentation of peptides with aromatic C-termini. Blood Cancer J 6:e411
Kramer GC, Sibley L, Aukland K, Renkin EM (1986) Wick sampling of interstitial fluid in rat skin: further analysis and modifications of the method. Microvasc Res 32:39–49
Kuboki M, Ishii H, Kazama M (1990) Characterization of calpain I-binding proteins in human erythrocyte plasma membrane. J Biochem 107:776–780
Lauber K, Bohn E, Kröber SM, Xiao YJ, Blumenthal SG, Lindemann RK, Marini P, Wiedig C, Zobywalski A, Baksh S, Xu Y, Autenrieth IB, Schulze-Osthoff K, Belka C, Stuhler G, Wesselborg S (2003) Apoptotic cells induce migration of phagocytes via caspase-3-mediated release of a lipid attraction signal. Cell 113:717–730
Lavabre-Bertrand T, Henry L, Carillo S, Guiraud I, Ouali A, Dutaud D, Aubry L, Rossi JF, Bureau JP (2001) Plasma proteasome level is a potential marker in patients with solid tumors and hemopoietic malignancies. Cancer 92:2493–2500
Leak LV, Liotta LA, Krutzsch H, Jones M, Fusaroa VA, Ross SJ, Zhao Y, Petricoin EF (2004) Proteomic analysis of lymph. Proteomics 4:753–765
Levine SJ (2008) Molecular mechanisms of soluble cytokine receptor generation. J Biol Chem 283:14177–14181
Ling XB, Lau K, Deshpande C, Park JL, Milojevic D, Macaubas C, Xiao C, Lopez-Avila V, Kanegaye J, Burns JC, Cohen H, Schilling J, Mellins ED (2010) Urine peptidomic and targeted plasma protein analyses in the diagnosis and monitoring of systemic juvenile idiopathic arthritis. Clin Proteomics 6:175–193
Liotta LA, Petricoin EF (2006) Serum peptidome for cancer detection: spinning biologic trash into diagnostic gold. J Clin Invest 116:26–30
Loffler MW et al (2018) Mapping the HLA ligandome of colorectal cancer reveals an imprint of malignant cell transformation. Cancer Res 78:4627–4641
Matuszczak E, Tylicka M, Debek W, Hermanowicz A, Ostrowska H (2015) The comparison of C-proteasome activity in the plasma of children after burn injury, mild head injury and blunt abdominal trauma. Adv Med Sci 60:253–258
Mebius RE, Kraal G (2005) Structure and function of the spleen. Nat Rev Immunol 5:606–616
Meng Z, Veenstra TD (2007) Proteomic analysis of serum, plasma, and lymph for the identification of biomarkers. Proteomics Clin Appl 1:747–757
Meng Z, Veenstra TD (2011) Targeted mass spectrometry approaches for protein biomarker verification. J Proteome 74:2650–2659
Meyer VS et al (2009) Identification of natural MHC class II presented phosphopeptides and tumor-derived MHC class I phospholigands. J Proteome Res 8:3666–3674
Michel CC (2004) Microvascular permeability, ultrafiltration, and restricted diffusion. Am J Physiol Heart Circ Physiol 287:H1887–H1888
Mittal A, Middleditch M, Ruggiero K, Buchanan CM, Jullig M, Loveday B, Cooper GJS, Windsor JA, Phillips ARJ (2008) The proteome of rodent mesenteric lymph. Am J Physiol Gastrointest Liver Physiol 295:G895–G903
Mittal A, Phillips AR, Middleditch M, Ruggiero K, Loveday B, Delahunt B, Cooper GJ, Windsor JA (2009) The proteome of mesenteric lymph during acute pancreatitis and implications for treatment. JOP 10:130–142
Mohamed MM et al (2010) Interleukin-6 increases expression and secretion of cathepsin B by breast tumor-associated monocytes. Cell Physiol Biochem 25:315–324
Moon HY, Becke A, Berron D, Becker B, Sah N, Benoni G, Janke E, Lubejko ST, Greig NH, Mattison JA, Duzel E, van Praag H (2016) Running-induced systemic Cathepsin B secretion is associated with memory function. Cell Metab 24:332–340
Moussion C, Sixt M (2013) A conduit to amplify innate immunity. Immunity 38:853–854
Mukaro VR, Quach A, Gahan ME, Boog B, Huang ZH, Gao X, Haddad C, Mahalingam S, Hii CS, Ferrante A (2018) Small tumor necrosis factor receptor biologics inhibit the tumor necrosis factor-p38 signalling axis and inflammation. Nat Commun 9(1365):1365
Naseem RH, Hedegard W, Henry TD, Lessard J, Sutter K, Katz SA (2005) Plasma cathepsin D isoforms and their active metabolites increase after myocardial infarction and contribute to plasma renin activity. Basic Res Cardiol 100:139–146
Neidert MC, Kowalewski DJ, Silginer M, Kapolou K, Backert L, Freudenmann LK, Peper JK, Marcu A, Wang SSY, Walz JS, Wolpert F, Rammensee HG, Henschler R, Lamszus K, Westphal M, Roth P, Regli L, Stevanović S, Weller M, Eisele G (2018) The natural HLA ligandome of glioblastoma stem-like cells: antigen discovery for T cell-based immunotherapy. Acta Neuropathol 135:923–938
Neumann F, Wagner C, Kubuschok B, Stevanovic S, Rammensee HG, Pfreundschuh M (2004) Identification of an antigenic peptide derived from the cancer-testis antigen NY-ESO-1 binding to a broad range of HLA-DR subtypes. Cancer Immunol Immunother 53:589–599
Nguyen VP et al (2010) Differential proteomic analysis of lymphatic, venous, and arterial endothelial cells extracted from bovine mesenteric vessels. Proteomics 10:1658–1672
Noris M, Remuzzi G (2013) Overview of complement activation and regulation. Semin Nephrol 33:479–492
Olszewski WL (2001) Human afferent lymph contains apoptotic cells and "free" apoptotic DNA fragments--can DNA be reutilized by the lymph node cells? Lymphology 34:179–183
Olszewski WL, Pazdur J, Kubasiewicz E, Zaleska M, Cooke CJ, Miller NE (2001) Lymph draining from foot joints in rheumatoid arthritis provides insight into local cytokine and chemokine production and transport to lymph nodes. Arthritis Rheum 44:541–549
Omenn GS et al (2005) Overview of the HUPO plasma proteome project: results from the pilot phase with 35 collaborating laboratories and multiple analytical groups, generating a core dataset of 3020 proteins and a publicly-available database. Proteomics 5:3226–3245
Osenkowski P, Toth M, Fridman R (2004) Processing, shedding, and endocytosis of membrane type 1-matrix metalloproteinase (MT1-MMP). J Cell Physiol 200:2–10
Osman R, Tacnet-Delorme P, Kleman JP, Millet A, Frachet P (2017) Calreticulin release at an early stage of death modulates the clearance by macrophages of apoptotic cells. Front Immunol 8(1034)
Papatheodoridis GV, Hadziyannis E, Tsochatzis E, Georgiou A, Kafiri G, Tiniakos DG, Margariti K, Manolakopoulos S, Manesis EK, Archimandritis AJ (2010) Serum apoptotic caspase activity in chronic hepatitis C and nonalcoholic fatty liver disease. J Clin Gastroenterol 44:e87–e95
Peltz ED, Moore EE, Zurawel AA, Jordan JR, Damle SS, Redzic JS, Masuno T, Eun J, Hansen KC, Banerjee A (2009) Proteome and system ontology of hemorrhagic shock: exploring early constitutive changes in postshock mesenteric lymph. Surgery 146:347–357
Petricoin EF, Belluco C, Araujo RP, Liotta LA (2006) The blood peptidome: a higher dimension of information content for cancer biomarker discovery. Nat Rev Cancer 6:961–967
Piacentini M, Farrace MG, Hassan C, Serafini B, Autuori F (1999) 'Tissue' transglutaminase release from apoptotic cells into extracellular matrix during human liver fibrogenesis. J Pathol 189:92–98
Pontremoli S, Sparatore B, Salamino F, Michetti M, Sacco O, Melloni E (1985) Reversible activation of human neutrophil calpain promoted by interaction with plasma membranes. Biochem Int 11:35–44
Poole AR, Hembry RM, Dingle JT, Pinder I, Ring EFJ, Cosh J (1976) Secretion and localization of cathepsin D in synovial tissues removed from rheumatoid and traumatized joints. An immunohistochemical study. Arthritis Rheum 19:1295–1307
Popova TG, Espina V, Zhou W, Mueller C, Liotta L, Popov SG (2014) Whole proteome analysis of mouse lymph nodes in cutaneous anthrax. PLoS One 9:e110873
Postawski K, Rechberger T, Jakimiuk AJ, Skorupski P, Bogusiewicz M, Jakowicki JA (1999) Interstitial collagenase (MMP-1) activity in human ovarian tissue. Gynecol Endocrinol 13:273–278
Qi H, Kastenmuller W, Germain RN (2014) Spatiotemporal basis of innate and adaptive immunity in secondary lymphoid tissue. Annu Rev Cell Dev Biol 30:141–167
Quesada V, Ordonez GR, Sanchez LM, Puente XS, Lopez-Otin C (2009) The Degradome database: mammalian proteases and diseases of proteolysis. Nucleic Acids Res 37:D239–D243
Rammensee H, Bachmann J, Emmerich NP, Bachor OA, Stevanovic S (1999) SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics 50:213–219
Reed RK, Wiig H (1983) Interstitial albumin mass and transcapillary extravasation rate of albumin in DMBA-induced rat mammary tumours. Scand J Clin Lab Invest 43:503–512
Renehan AG, Booth C, Potten CS (2001) What is apoptosis, and why is it important? BMJ 322:1536–1538
Rizzo R, Trentini A, Bortolotti D, Manfrinato MC, Rotola A, Castellazzi M, Melchiorri L, di Luca D, Dallocchio F, Fainardi E, Bellini T (2013) Matrix metalloproteinase-2 (MMP-2) generates soluble HLA-G1 by cell surface proteolytic shedding. Mol Cell Biochem 381:243–255
Robbins RJ, Villanueva J, Tempst P (2005) Distilling cancer biomarkers from the serum peptidome: high technology reading of tea leaves or an insight to clinical systems biology? J Clin Oncol 23:4835–4837
Roche PA, Furuta K (2015) The ins and outs of MHC class II-mediated antigen processing and presentation. Nat Rev Immunol 15:203–216
Roozendaal R et al (2009) Conduits mediate transport of low-molecular-weight antigen to lymph node follicles. Immunity 30:264–276
Roth W et al (2000) Cathepsin L deficiency as molecular defect of furless: hyperproliferation of keratinocytes and pertubation of hair follicle cycling. FASEB J 14:2075–2086
Rudensky A, Preston-Hurlburt P, Hong SC, Barlow A, Janeway CA Jr (1991) Sequence analysis of peptides bound to MHC class II molecules. Nature 353:622–627
Russo E, Teijeira A, Vaahtomeri K, Willrodt AH, Bloch JS, Nitschké M, Santambrogio L, Kerjaschki D, Sixt M, Halin C (2016) Intralymphatic CCL21 promotes tissue egress of dendritic cells through afferent lymphatic vessels. Cell Rep 14:1723–1734
Sabbota AL, Kim HRC, Zhe X, Fridman R, Bonfil RD, Cher ML (2010) Shedding of RANKL by tumor-associated MT1-MMP activates Src-dependent prostate cancer cell migration. Cancer Res 70:5558–5566
Sadegh-Nasseri S, Kim A (2015) MHC class II auto-antigen presentation is unconventional. Front Immunol 6(372)
Saftig P, Hunziker E, Wehmeyer O, Jones S, Boyde A, Rommerskirch W, Moritz JD, Schu P, von Figura K (1998) Impaired osteoclastic bone resorption leads to osteopetrosis in cathepsin-K-deficient mice. Proc Natl Acad Sci U S A 95:13453–13458
Santambrogio L (2013) Immunology of the lymphatic system. Springer, New York
Santambrogio L, Sato AK, Carven GJ, Belyanskaya SL, Strominger JL, Stern LJ (1999a) Extracellular antigen processing and presentation by immature dendritic cells. Proc Natl Acad Sci U S A 96:15056–15061
Santambrogio L, Sato AK, Fischer FR, Dorf ME, Stern LJ (1999b) Abundant empty class II MHC molecules on the surface of immature dendritic cells. Proc Natl Acad Sci U S A 96:15050–15055
Sanz RL, Ferraro GB, Kacervosky J, Salesse C, Gowing E, Hua L, Rambaldi I, Beaubien F, Holmbeck K, Cloutier JF, Lévesque M, Murai K, Fournier AE (2018) MT3-MMP promotes excitatory synapse formation by promoting Nogo-66 receptor ectodomain shedding. J Neurosci 38:518–529
Scarisbrick IA (2008) The multiple sclerosis degradome: enzymatic cascades in development and progression of central nervous system inflammatory disease. Curr Top Microbiol Immunol 318:133–175
Schuster H, Peper JK, Bösmüller HC, Röhle K, Backert L, Bilich T, Ney B, Löffler MW, Kowalewski DJ, Trautwein N, Rabsteyn A, Engler T, Braun S, Haen SP, Walz JS, Schmid-Horch B, Brucker SY, Wallwiener D, Kohlbacher O, Fend F, Rammensee HG, Stevanović S, Staebler A, Wagner P (2017) The immunopeptidomic landscape of ovarian carcinomas. Proc Natl Acad Sci U S A 114:E9942–E9951
Shao H, Chou J, Baty CJ, Burke NA, Watkins SC, Stolz DB, Wells A (2006) Spatial localization of m-calpain to the plasma membrane by phosphoinositide biphosphate binding during epidermal growth factor receptor-mediated activation. Mol Cell Biol 26:5481–5496
Shao W, Pedrioli PGA, Wolski W, Scurtescu C, Schmid E, Vizcaíno JA, Courcelles M, Schuster H, Kowalewski D, Marino F, Arlehamn CSL, Vaughan K, Peters B, Sette A, Ottenhoff THM, Meijgaarden KE, Nieuwenhuizen N, Kaufmann SHE, Schlapbach R, Castle JC, Nesvizhskii AI, Nielsen M, Deutsch EW, Campbell DS, Moritz RL, Zubarev RA, Ytterberg AJ, Purcell AW, Marcilla M, Paradela A, Wang Q, Costello CE, Ternette N, van Veelen PA, van Els CACM, Heck AJR, de Souza GA, Sollid LM, Admon A, Stevanovic S, Rammensee HG, Thibault P, Perreault C, Bassani-Sternberg M, Aebersold R, Caron E (2018) The SysteMHC atlas project. Nucleic Acids Res 46:D1237–D1247
Shen Z, Want EJ, Chen W, Keating W, Nussbaumer W, Moore R, Gentle TM, Siuzdak G (2006) Sepsis plasma protein profiling with immunodepletion, three-dimensional liquid chromatography tandem mass spectrometry, and spectrum counting. J Proteome Res 5:3154–3160
Shen Y, Tolić N, Liu T, Zhao R, Petritis BO, Gritsenko MA, Camp DG, Moore RJ, Purvine SO, Esteva FJ, Smith RD (2010a) Blood peptidome-degradome profile of breast cancer. PLoS One 5:e13133
Shen Y, Liu T, Tolić N, Petritis BO, Zhao R, Moore RJ, Purvine SO, Camp DG II, Smith RD (2010b) Strategy for degradomic-peptidomic analysis of human blood plasma. J Proteome Res 9:2339–2346
Shi ZD, Ji XY, Qazi H, Tarbell JM (2009) Interstitial flow promotes vascular fibroblast, myofibroblast, and smooth muscle cell motility in 3-D collagen I via upregulation of MMP-1. Am J Physiol Heart Circ Physiol 297:H1225–H1234
Shi ZD, Ji XY, Berardi DE, Qazi H, Tarbell JM (2010) Interstitial flow induces MMP-1 expression and vascular SMC migration in collagen I gels via an ERK1/2-dependent and c-Jun-mediated mechanism. Am J Physiol Heart Circ Physiol 298:H127–H135
Shi ZD, Wang H, Tarbell JM (2011) Heparan sulfate proteoglycans mediate interstitial flow mechanotransduction regulating MMP-13 expression and cell motility via FAK-ERK in 3D collagen. PLoS One 6:e15956
Sixt SU, Dahlmann B (2008) Extracellular, circulating proteasomes and ubiquitin - incidence and relevance. Biochim Biophys Acta 1782:817–823
Sixt M, Kanazawa N, Selg M, Samson T, Roos G, Reinhardt DP, Pabst R, Lutz MB, Sorokin L (2005) The conduit system transports soluble antigens from the afferent lymph to resident dendritic cells in the T cell area of the lymph node. Immunity 22:19–29
Smith CR, Batruch I, Bauça J, Kosanam H, Ridley J, Bernardini MQ, Leung F, Diamandis EP, Kulasingam V (2014) Deciphering the peptidome of urine from ovarian cancer patients and healthy controls. Clin Proteomics 11:23
Soto-Hernandez JL (2008) Detection of caspase-3, neuron specific enolase, and high-sensitivity C-reactive protein levels in both cerebrospinal fluid and serum of patients after aneurysmal subarachnoid hemorrhage. Neurosurgery 62, E1384; author reply:E1384
Srinivasan S, Vannberg FO, Dixon JB (2016) Lymphatic transport of exosomes as a rapid route of information dissemination to the lymph node. Sci Rep 6(24436)
Steiniger B, Barth P (2000) Microanatomy and function of the spleen. Adv Anat Embryol Cell Biol 151, III-IX:1–101
Stern LJ, Santambrogio L (2016) The melting pot of the MHC II peptidome. Curr Opin Immunol 40:70–77
Sternlicht MD, Werb Z (2001) How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 17:463–516
Stoebner PE, Lavabre-Bertrand T, Henry L, Guiraud I, Carillo S, Dandurand M, Joujoux JM, Bureau JP, Meunier L (2005) High plasma proteasome levels are detected in patients with metastatic malignant melanoma. Br J Dermatol 152:948–953
Sturm T, Leinders-Zufall T, Maček B, Walzer M, Jung S, Pömmerl B, Stevanović S, Zufall F, Overath P, Rammensee HG (2013) Mouse urinary peptides provide a molecular basis for genotype discrimination by nasal sensory neurons. Nat Commun 4(1616)
Stypmann J et al (2002) Dilated cardiomyopathy in mice deficient for the lysosomal cysteine peptidase cathepsin L. Proc Natl Acad Sci U S A 99:6234–6239
Swingler TE, Waters JG, Davidson RK, Pennington CJ, Puente XS, Darrah C, Cooper A, Donell ST, Guile GR, Wang W, Clark IM (2009) Degradome expression profiling in human articular cartilage. Arthritis Res Ther 11:R96
Tan CT, Croft NP, Dudek NL, Williamson NA, Purcell AW (2011) Direct quantitation of MHC-bound peptide epitopes by selected reaction monitoring. Proteomics 11:2336–2340
Tapiola T, Alafuzoff I, Herukka SK, Parkkinen L, Hartikainen P, Soininen H, Pirttilä T (2009) Cerebrospinal fluid {beta}-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol 66:382–389
Terawaki S, Kitano K, Aoyama M, Mori T, Hakoshima T (2015) MT1-MMP recognition by ERM proteins and its implication in CD44 shedding. Genes Cells 20:847–859
Tran BQ, Miller PR, Taylor RM, Boyd G, Mach PM, Rosenzweig CN, Baca JT, Polsky R, Glaros T (2018) Proteomic characterization of dermal interstitial fluid extracted using a novel microneedle-assisted technique. J Proteome Res 17:479–485
Ugalde AP, Ordonez GR, Quiros PM, Puente XS, Lopez-Otin C (2010) Metalloproteases and the degradome. Methods Mol Biol 622:3–29
Veenstra TD (2007) Global and targeted quantitative proteomics for biomarker discovery. J Chromatogr B Analyt Technol Biomed Life Sci 847:3–11
Veenstra TD, Conrads TP, Hood BL, Avellino AM, Ellenbogen RG, Morrison RS (2005) Biomarkers: mining the biofluid proteome. Mol Cell Proteomics 4:409–418
Villanueva J et al (2006) Serum peptidome patterns that distinguish metastatic thyroid carcinoma from cancer-free controls are unbiased by gender and age. Mol Cell Proteomics 5:1840–1852
Wagner C et al (2003) Identification of an HLA-A*02 restricted immunogenic peptide derived from the cancer testis antigen HOM-MEL-40/SSX2. Cancer Immun 3:18
Walcher D, Marx N (2009) Advanced glycation end products and C-peptide-modulators in diabetic vasculopathy and atherogenesis. Semin Immunopathol 31:103–111
Walenbergh SM et al (2016) Plasma cathepsin D correlates with histological classifications of fatty liver disease in adults and responds to intervention. Sci Rep 6(38278)
Wan X, Zinselmeyer BH, Zakharov PN, Vomund AN, Taniguchi R, Santambrogio L, Anderson MS, Lichti CF, Unanue ER (2018) Pancreatic islets communicate with lymphoid tissues via exocytosis of insulin peptides. Nature 560:107–111
Wang H, Luo C, Zhu S, Fang H, Gao Q, Ge S, Qu H, Ma Q, Ren H, Wang Y, Wang W (2017) Serum peptidome profiling for the diagnosis of colorectal cancer: discovery and validation in two independent cohorts. Oncotarget 8:59376–59386
Weigert A, Cremer S, Schmidt MV, von Knethen A, Angioni C, Geisslinger G, Brune B (2010) Cleavage of sphingosine kinase 2 by caspase-1 provokes its release from apoptotic cells. Blood 115:3531–3540
Wiig H, Noddeland H (1983) Interstitial fluid pressure in human skin measured by micropuncture and wick-in-needle. Scand J Clin Lab Invest 43:255–260
Wiig H, Swartz MA (2012) Interstitial fluid and lymph formation and transport: physiological regulation and roles in inflammation and cancer. Physiol Rev 92:1005–1060
Wilson TJ, Nannuru KC, Futakuchi M, Singh RK (2010) Cathepsin G-mediated enhanced TGF-beta signaling promotes angiogenesis via upregulation of VEGF and MCP-1. Cancer Lett 288:162–169
Yan D, Wang HW, Bowman RL, Joyce JA (2016) STAT3 and STAT6 signaling pathways synergize to promote Cathepsin secretion from macrophages via IRE1alpha activation. Cell Rep 16:2914–2927
Yang J, Yang SY, Hu XY, Huo SF, Shang WL, Li ZF, Ni L, Wang AY, Guo YM, Song TS, Chen-Huang (2010) Serum peptidome profiling in patients with lung cancer. Anat Rec (Hoboken) 293:2027–2033
Yang J, Song YC, Dang CX, Song TS, Liu ZG, Guo YM, Li ZF, Huang C (2012a) Serum peptidome profiling in patients with gastric cancer. Clin Exp Med 12:79–87
Yang J, Song YC, Song TS, Hu XY, Guo YM, Li ZF, Dang CX, Huang C (2012b) Identification of novel low molecular weight serum peptidome biomarkers for non-small cell lung cancer (NSCLC). J Clin Lab Anal 26:148–154
Zapico-Muniz E, Farre-Viladrich A, Rico-Santana N, Gonzalez-Sastre F, Mora-Brugues J (2010) Standardized peptidome profiling of human serum for the detection of pancreatic cancer. Pancreas 39:1293–1298
Zhang X, Adamson RH, Curry FR, Weinbaum S (2006) A 1-D model to explore the effects of tissue loading and tissue concentration gradients in the revised Starling principle. Am J Physiol Heart Circ Physiol 291:H2950–H2964
Zhang J, Hao N, Liu W, Lu M, Sun L, Chen N, Wu M, Zhao X, Xing B, Sun W, He F (2017) In-depth proteomic analysis of tissue interstitial fluid for hepatocellular carcinoma serum biomarker discovery. Br J Cancer 117:1676–1684
Zhou M et al (2004) An investigation into the human serum "int0eractome". Electrophoresis 25:1289–1298
Zoeger A, Blau M, Egerer K, Feist E, Dahlmann B (2006) Circulating proteasomes are functional and have a subtype pattern distinct from 20S proteasomes in major blood cells. Clin Chem 52:2079–2086
Zuo L, Ma YC, Zhou YH, Wang M, Xu GB, Wang HY (2005) Application of GFR-estimating equations in Chinese patients with chronic kidney disease. Am J Kidney Dis 45:463–472
Zurawel A, Moore EE, Peltz ED, Jordan JR, Damle S, Dzieciatkowska M, Banerjee A, Hansen KC (2011) Proteomic profiling of the mesenteric lymph after hemorrhagic shock: differential gel electrophoresis and mass spectrometry analysis. Clin Proteomics 8(1):1
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Biology and Evolution of Antigen Presentation
Rights and permissions
About this article
Cite this article
Santambrogio, L., Rammensee, HG. Contribution of the plasma and lymph Degradome and Peptidome to the MHC Ligandome. Immunogenetics 71, 203–216 (2019). https://doi.org/10.1007/s00251-018-1093-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00251-018-1093-z