Abstract
Background
Contrast-enhanced voiding urosonography (ceVUS) is widely used outside the United States to diagnose vesicoureteral reflux (VUR) in children and is highly sensitive while avoiding exposure to ionizing radiation. At the onset of this study, two ultrasound (US) contrast agents were available in the United States. Pediatric safety data for intravenous administration was published for one, Optison™.
Objective
This study aimed to evaluate the diagnostic performance and safety of ceVUS using Optison™ and compare its diagnostic efficacy with voiding cystourethrogram (VCUG) for VUR detection and grading in children.
Materials and methods
The United States Food and Drug Administration and institutional Investigational New Drug authorizations were obtained to conduct a prospective comparative study of ceVUS with Optison™ and VCUG. CeVUS was performed with intravesical administration of 0.2% Optison™/normal saline solution. A standard VCUG followed. Safety assessment included physical examination, and heart rate, pulse oximetry and adverse reactions monitoring before, during and immediately after the examinations. A follow-up questionnaire was completed by telephone 48-h after the studies.
Results
Sixty-two pelviureteric units were studied in 30 patients with a mean age of 3.5 years (range: 0.1–17 years) including 21 girls and 9 boys. No severe adverse events occurred. All patients had normal heart rate and blood oxygenation saturation prior to, during and after the studies. At the 48-h follow-up, one patient (3.3%) reported transient dysuria. Taking the VCUG as the reference standard, ceVUS had a sensitivity of 91.7% (95%; confidence interval [CI]: 61.5%–99.8%) and specificity of 98% (95%; CI: 89.4%–99.9%). The concordance between ceVUS and VCUG for VUR detection and grading was 84.3% and 81.8%, respectively. VUR grades were discrepant in 4/11 refluxing pelviureteric units, with VCUG upgrading VUR in 2.
Conclusion
Detection of VUR with Optison™ ceVUS was comparable to VCUG without exposure to ionizing radiation. CeVUS with Optison™ is a well-tolerated diagnostic procedure with a favorable safety profile.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Contrast-enhanced voiding urosonography (ceVUS) is a radiation-free, highly sensitive imaging examination for the detection of vesicoureteral reflux (VUR) using ultrasound (US) and the intravesical administration of an US contrast agent [1,2,3]. For more than two decades, the second-generation US contrast agent SonoVue® (Bracco, Milan, Italy) was used off-label for ceVUS performance, primarily in Europe. It is the most commonly used US contrast agent for ceVUS in children. In 2012, a survey among European institutions revealed that more than 4,000 ceVUS examinations with SonoVue® were performed in 29 European centers [4]. Additionally, a literature review identified 15 original studies published by the end of 2016 on ceVUS with SonoVue® involving 2,344 children [5]. It was not until October 2014 that SonoVue® became commercially available in the United States under the proprietary name Lumason®. In December 2016, the United States Food and Drug Administration (FDA) approved the intravesical use of Lumason® for ceVUS performance in children.
In the United States, ceVUS only gained attention in the last three years. Among the factors that contributed to this lag are the complex regulatory requirements for the off-label use of contrast agents in clinical research. Specifically, federal regulations for protection of human subjects participating in research mandate investigators to obtain authorization from the FDA before using a contrast agent in a prospective clinical trial if the agent is not approved by the FDA for the specific indication or patient population. This authorization is achieved by filing an Investigational New Drug application with the FDA. The application provides pertinent safety and efficacy information to the FDA to determine if the product is reasonably safe to be used in a clinical trial.
At the onset of this study, US contrast agents available in the United States included Optison™ (GE Healthcare Inc., Princeton, NJ) and Definity™ (Lantheus Medical Imaging, N. Billerica, MA). At that time, there were safety and efficacy data from the intravenous use of Optison™ in children [6, 7]. In addition, an in vitro study simulating intravesical ceVUS laid the groundwork for determining the appropriate dose of Optison™ and optimized the procedural steps for its future clinical use in children [8]. Accordingly, Optison™ was chosen to initiate ceVUS research in the United States. Optison™ had not been previously evaluated for clinical ceVUS examination.
Therefore, we filed a research Investigational New Drug application to obtain FDA approval to conduct a prospective clinical trial of ceVUS in children with Optison™. The aims were: 1) to evaluate the safety of intravesical administration of Optison™, 2) to compare the diagnostic performance of ceVUS with Optison™ to fluoroscopic voiding cystourethrography (VCUG) for detection and grading of VUR in children, and 3) to define the dose of Optison™ needed to perform ceVUS effectively.
Materials and methods
A research Investigational New Drug application was initiated in the Department of Radiology at the Children’s Hospital of Philadelphia for a prospective pediatric phase I clinical trial comparing ceVUS with Optison™ to VCUG. The application included published safety data from intravenous administration of Optison™ as well as safety and efficacy information from the intravesical use of US contrast agents similar to Optison™ in children. The departmental Radiology Scientific Review Committee and the institutional Clinical Research Support Office reviewed the study protocol. Next, the Investigational New Drug application was submitted to and approved by the FDA Center for Drug Evaluation and Research under the Investigational New Drug application number 121488. Following this approval, the Institutional Review Board further reviewed and approved the study. The study was registered in the national database of clinical trials (clinicaltrials.gov) under the identification number NCT02204917. No external funding from industry or research grant supported this study. The Department of Radiology covered all study-related costs including but not limited to Optison™ contrast, medical equipment and ancillary supplies, and research and nursing support staff.
From September 2014 to April 2015, 30 consecutive patients referred for clinically indicated VCUG were enrolled in the clinical trial. They were divided into two cohorts. The first cohort consisted of 10 children age 2 to 18 years old and the second cohort included 20 children age 0 to 18 years old. Following enrollment of the first 10 children, a preliminary safety analysis was performed before enrolling the second cohort. Patients were excluded from the trial if they (1) required sedation for VCUG performance or (2) had a history of hypersensitivity to perflutren gas, blood products or albumin.
Informed written consent was obtained from all parents/legal guardians and, when applicable, the assent of participating children was also obtained. Both examinations took place in the fluoroscopy suite. CeVUS examinations were followed immediately by VCUG examinations performed in the same session by the same, single pediatric radiologist (K.D) with more than 20 years of experience in ceVUS examination performance. Before the studies, a transurethral bladder catheterization was performed in all children with a feeding tube under sterile technique by the same, single, same technologist. The catheter was secured to the patient’s leg with a tape. A single bladder catheter was used for both examinations and remained in place until voiding during the VCUG portion of the study. The size of the catheter used was measured and recorded in French units (Fr). The ease of catheter insertion was graded on a five-point scale by the technologist who performed the catheterization based on the resistance of catheter insertion/passage into the bladder and the patient’s perceived distress during the procedure (1 easy - 5 hard) (Table 1).
Contrast-enhanced voiding urosonography
Optison™ was reconstituted in its vial according to the manufacturer’s recommendations. A 0.2% Optison™/normal saline solution was prepared by instilling 0.2 mL of Optison™ into a 100-mL saline bag. The saline bag was gently agitated to mix the solution. The bag was hung on an intravenous pole approximately 50–60 cm above the level of the bladder to facilitate gravity infusion. Additional 100-mL bags each containing 0.2 mL of Optison™ were prepared at the onset of the examination depending on the projected maximum bladder capacity using the formula (age in years +2) × 30 [9]. Prior to infusion, each bag was gently agitated to remix the contrast and saline. Using 100-mL normal saline bags made it easier to monitor the administered infusion volume. Infusion tubing was attached to the saline bag and connected via a three-way stopcock in parallel to the bladder catheter. The parallel orientation minimized shearing stress on the microbubbles during infusion.
A 20-mL syringe filled with normal saline was attached to the port of the three-way stopcock perpendicular to the bladder catheter to permit periodic normal saline flush. Normal saline was directly injected into the bladder if the US contrast agent did not mix homogeneously throughout the bladder or if the concentration of Optison™ solution appeared too high on US images. A high contrast concentration causes posterior acoustic shadowing, which results in incomplete visualization of the posterior wall of the urinary bladder and the retrovesical segment of the ureters. If the contrast appeared too faint on US images, despite image optimization, then additional contrast was added into the saline infusion bag.
The overall volume of Optison™ (mL) administered per patient and the inferred volume of Optison™ administered per ceVUS cycle were recorded. The number of patients who required additional administration of normal saline directly into the bladder or additional injection of Optison™ into the infusion bag for optimal ceVUS performance was recorded. The volumes of normal saline or Optison™ that were additionally administered per patient and per ceVUS cycle were also documented.
The ceVUS examinations were performed with US scanners equipped with low mechanical index contrast-specific mode using multifrequency convex and linear transducers. The first 13 studies were carried out with the ACUSON S3000 (Siemens Medical Solutions, Malvern, PA) and the last 17 with the Philips EPIC 7 (Philips Healthcare, Andover, MA). The mechanical index settings ranged from 0.03 to 0.49 in both US systems. Before contrast administration, baseline gray-scale images of the bladder and each kidney were acquired. After contrast administration, the bladder, ureters and kidneys were scanned repeatedly during bladder filling and voiding. Sonourethrography was not part of the study protocol. VUR was diagnosed if microbubbles were visualized in the ureter, renal pelvis or calyces. VUR was graded on a 5-point scale similar to the International System of Radiographic Grading of VUR used in VCUG [10]. The presence, grade and side of VUR were recorded. Cyclic filling of the bladder was performed in neonates and infants who voided at low volumes during the examination and the number of ceVUS cycles was noted. After ceVUS, the child remained on the fluoroscopy table with the transurethral catheter in place. Children who were unable to void or voided incompletely at the end of ceVUS examination had their bladders emptied through the catheter. The final result of the ceVUS study was documented before starting the VCUG.
Voiding cystourethrography
VCUG was performed using the same bladder catheter placed for ceVUS, with gravity infusion of 17.2% iothalamate meglumine (Cysto-Conray II; Mallinckrodt, St. Louis, MO) and pulsed fluoroscopy (Siemens Luminos Agile; Siemens Medical Solutions, Malvern, PA, and Eleva; Philips Medical Systems, the Netherlands). VUR was graded on the 5-point scale according to the International System of Radiographic Grading of VUR [11]. When present, VUR side and grade were recorded. The number of VCUG cycles and whether the child was or was not able to void on the examination table were documented.
The last post-voiding VCUG spot image of the bladder was used to evaluate the residual volume of urine. This was regarded as none if there was complete emptying of the bladder after voiding, or it was graded as small, moderate or large, based on the position of the opacified bladder dome in relation to specific anatomical pelvic landmarks. Specifically, small post-voiding residual urine volume was regarded when the dome of the opacified bladder was below the horizontal level of the acetabula roof, moderate when the bladder dome was above the acetabula roof level but below the middle part of the sacrum and large when the bladder dome exceed that level [12].
Evaluation of adverse events
Safety assessments were performed and possible adverse events were documented in FDA-approved monitoring forms at baseline, during and immediately after each ceVUS and VCUG examination, and in follow-up telephone interviews. Assessments included: (a) evaluation of body systems for signs of generalized hypersensitivity, allergic or anaphylactoid reactions; (b) monitoring of heart rate and pulse oxygen saturation by fingertip pulse oximeter, and (c) telephone questionnaire-based interview of parents/guardians and children 48-h after the examinations to evaluate for delayed adverse events.
The type, severity, onset, duration and frequency of adverse events as well as the body systems involved were recorded. The severity of the event was classified as mild, moderate or serious and the onset of symptoms was categorized as acute, subacute or delayed according to the World Health Organization classifications. In addition, potential adverse events were classified as anticipated if these were expected given the study-related procedures or unanticipated if the subject was exposed to greater risk of harm than was previously known or recognized.
Comparison of ceVUS with VCUG
The diagnostic accuracy of ceVUS with Optison™ was compared to that of VCUG in terms of VUR detection rate and grade.
Statistical analysis
Descriptive statistics including mean, median and range were used for continuous variables. Counts and percentages were used for nominal and ordinal data. Nonparametric tests were used for group comparisons and using VCUG as the reference standard, the diagnostic accuracy values computed for ceVUS.
Results
The demographics of the 30 enrolled patients are presented in Table 2. The first cohort comprised 10 patients, 6 girls and 4 boys, with a mean age of 6.5±3.6 years. The second cohort included 20 patients, 15 girls and 5 boys, with a mean age of 2.0±3.7 years. Bladder catheterization was performed with a 6-Fr and an 8-Fr size feeding tube in 23 and 7 patients, respectively. In 27 cases, the process of catheter insertion into the bladder was scored as “1-very easy”, in 2 as “2-easy” and in 1 as “3-moderately easy”. No bladder catheterizations were scored as 4 or 5. The catheter dislodged in one female patient after the ceVUS and a new one had to be placed prior to the VCUG examination.
Adverse events
The safety analysis following the first cohort of 10 patients showed no serious or acute adverse events. In the 48-h telephone follow-up interview, an 11.8-year-old boy reported dysuria on the day of the ceVUS and VCUG examinations. The symptom resolved by the following day without medication or medical consultation. The dysuria was categorized as mild severity, subacute onset, self-limited course and anticipated. No adverse events occurred in the second cohort of children. There were no clinically relevant changes in vital signs in either cohort. Thus, overall there was only a single incident of a mild adverse event in 1 patient (3.33%).
Contrast-enhanced voiding urosonography
A Mann-Whitney U test showed that the actual volume of administered contrast/saline infusion was not significantly larger compared to the expected for age bladder capacity (P>0.05). In 19/30 patients (63.3%), one 100-mL infusion bag of 0.2% contrast/saline infusion was used, whereas a second infusion bag was required in 11/30 patients (36.7%). In 29/30 (96.7%) children, additional intravesical injections of normal saline were required to achieve homogenous contrast remix within the bladder. The mean number of additional intravesical saline injections required was 1.5 (range: 1–4) and the mean volume of additional normal saline injected per ceVUS cycle was 24 mL (range: 5–50 mL). In 6/30 (20%) children, additional Optison™ was injected into the contrast/saline infusion bag to increase the concentration of contrast within the bladder. The mean volume of the additional Optison™ injected was 0.1 mL (range: 0.1–0.2 mL). Including the additional administration of contrast required for ceVUS optimization the mean total volume of Optison™ used was 0.3 mL (range: 0.2–0.5 mL).
In 16/30 children (53.3%) (mean age: 5.4 years, range: 4.8 months-17 years), one ceVUS cycle was performed. Cyclic ceVUS was required in 14/30 children (46.7%) including: two cycles in nine children with a mean age of 1 year (range: 1.2 months-2.4 years); three cycles in one 18-day-old child, and multiple cycles in four children with a mean age of 2.5 years (range: 9.7 months–6.3 years).
The extrapolated mean volume of Optison™ administered in the first ceVUS cycle was 0.2 mL (range: 0.1–0.5 mL) and in the second ceVUS cycle was 0.1 mL (range: 0.04–0.2 mL). One child had a third ceVUS cycle performed and the extrapolated volume of Optison™ in this cycle was 0.15 mL. In the four children with multiple incomplete filling and voiding cycles, calculation of Optison™ volume per cycle was not feasible.
Twenty-three children were able to void around the catheter at the end of the ceVUS examination, 10 of whom emptied their bladders completely while on the examination table. The remaining 13 children who had incomplete bladder emptying and the 7 who did not void at all at the end of the ceVUS examination had their bladders emptied via the catheter.
Excluding the catheterization time, the mean duration of ceVUS examination was 9 min and 40 s (median: 9 min and 39 s, range: 4 min and 7 s to 18 min and 52 s). In the first age cohort, the mean duration of ceVUS was longer (mean time: 10 min and 53 s, median: 11 min and 58 s, range: 4 min and 9 s to 18 min and 52 s) compared to the second age cohort (mean time: 9 min, median: 8 min and 43 s, range: 4 min and 55 s to 17 min and 54 s). However, a Mann-Whitney U test showed that this difference was not statistically significant (P>0.05).
ceVUS VUR
Fifty-nine kidneys with 62 pelviureteric units were analyzed. One child had a horseshoe kidney and one child had duplicated collecting systems of both kidneys, which was established by previous imaging examinations. VUR was detected by ceVUS in 12/62 pelviureteric units in nine children. The grading of VUR was as follows: grade 0=50, grade I=2, grade II=8, grade III=2, grade IV=0, grade V=0 pelviureteric units, respectively.
Voiding cystourethrography
VCUG was performed with intravesical administration of Cysto-Conray® II by gravity drip. The mean volume of Cysto-Conray® II was 140.5 mL (median: 100 mL, range: 40–360 mL). A Mann-Whitney U test showed that the actual volume of Cysto-Conray® infusion administered in all children was not significantly larger compared to the expected for age bladder capacity (P>0.05).
Twenty-seven children were able to void on the fluoroscopic table at the end of the VCUG examination, including 9 with complete emptying, 15 with small and 3 with moderate post-void residual urinary volumes. Three girls with a mean age of 10.7 years old (range: 5.2–17 years) did not void at all. Two of these girls were asked to empty their bladders in the bathroom and the third, a younger girl, had her bladder emptied via the catheter.
The mean overall duration of the VCUG examination was 5 min and 48 s (median: 4 min and 31 s, range: 1 min and 21 s to 14 min and 37 s). The mean fluoroscopic time was 1.3 min (median: 1.28 min, range: 0.1 to 3.6 min) and the mean radiation dose that was delivered to the children who underwent VCUG was 1.5 dGy cm2 (median: 0.7, range: 0.2–10.3).
Comparative information regarding the diagnostic performance of ceVUS and VCUG are presented in Table 3.
VCUG VUR
VUR was detected by VCUG in 12/62 pelviureteric units in eight children. The grading of VUR with VCUG was as follows: grade 0=50, grade I=2, grade II=6, grade III=4, grade IV=0, grade V=0 pelviureteric units, respectively. The mean number of VCUG cycles performed was 1.3 (range: 1–4). In one child, multiple incomplete cycles of bladder filling and voiding were performed.
Comparative performance of ceVUS with VCUG
Taking into account all VUR cases that were detected by ceVUS and/or VCUG, VUR was detected in 13/62 pelviureteric units of 9 children (Table 4). There was agreement between ceVUS and VCUG regarding the presence of reflux in 11/13 refluxing pelviureteric units (Figs. 1, 2, and 3). The concordance rate for detecting reflux was 84.3%. Both modalities did not detect the presence of VUR in one pelviureteric unit each; however, it was diagnosed by the other modality. Specifically, the presence of reflux was not detected by ceVUS in one pelviureteric unit where VCUG demonstrated grade I reflux (Fig. 4) whereas VCUG did not detect grade II VUR in one pelviureteric unit that was only detected on ceVUS (Figs. 2 and 5).
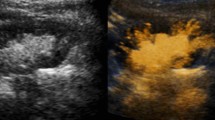
A 1.9 year-old girl with vesicoureteral reflux (VUR). Voiding cystourethrogram (VCUG) and contrastenhanced voiding ultrasound (ceVUS) showed agreement for presence of the right-side grade 1 VUR. a VCUG: Grade 1 reflux in the dilated retrovesical portion of the right ureter (arrow). b, c CeVUS. Transverse “contrast-only” image of the urinary bladder (b) and corresponding gray-scale image (c) of the same anatomical region to ensure in-plane scanning. Echogenic microbubbles are depicted within the dilated right terminal ureter, corresponding to grade 1 reflux (arrows)
A 2-year-old girl with vesicoureteral reflux. Voiding cystourethrogram (VCUG) and contrast-enhanced voiding ultrasound (ceVUS) showed disagreement for the grade of reflux in the left kidney (VCUG grade 3; ceVUS grade 2) and agreement (both VCUG and ceVUS grade 2) in the right kidney. a VCUG: Grade 2 reflux in the right kidney. Grade 3 reflux in the left kidney with intermittent dilation of the major and minor calyces of the upper pole. b, c CeVUS: Sagittal “contrast-only” image of the right (b) and left (c) kidney. Grade 2 vesicoureteral reflux depicted on both kidneys (arrows). There is no dilation of the pelvicalyceal systems in either kidney
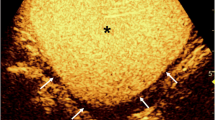
A 2.4-year-old girl with vesicoureteral reflux (VUR). Voiding cystourethrogram (VCUG) and contrastenhanced voiding ultrasound (ceVUS) showed agreement for the presence and grade of reflux in the left kidney. a VCUG: Grade 3 reflux on the left kidney during bladder filling. b CeVUS: Sagittal “contrast-only” image of the left kidney with the signal from surrounding tissues suppressed. Refluxed microbubbles appear echogenic in the dilated left pelvis or calyces (arrows) corresponding to grade 3 VUR
An 11.8-year-old boy with vesicoureteral reflux. Voiding cystourethrogram (VCUG) and contrastenhanced voiding ultrasound (ceVUS) showed disagreement for the presence of reflux. Right-side grade 1 reflux was only detected by VCUG. a VCUG: Grade 1 reflux was seen in the non-dilated right distal ureter during bladder filling. b CeVUS. “Contrast-only” transverse image through the bladder showing homogeneous filling. There is no dilation of the distal ureters and no reflux was detected
A 4.8- month-old girl. Voiding cystourethrogram (VCUG) and contrast-enhanced voiding ultrasound (ceVUS) showed disagreement for the presence of reflux in the left kidney. Left grade 2 reflux was only depicted by ceVUS. a VCUG: No vesicoureteral reflux was demonstrated bilaterally. b CeVUS. Sagittal “contrast-only” image showing refluxed US contrast material in the non-dilated left renal pelvis and calyces (arrows) consistent with grade 2 reflux
There was agreement about the grade of VUR between the modalities in 9/11 pelviureteric units where VUR was detected by both studies. The concordance between ceVUS and VCUG for VUR grading was 81.8%. In the two discrepant cases, reflux was higher grade by VCUG than ceVUS. In both pelviureteric units, the reflux was grade III by VCUG; however, during the ceVUS exam, one pelviureteric unit was grade I and the other pelviureteric unit was grade II. Specifically, the first patient was a 5.8-year-old girl who had a noncyclic ceVUS exam followed by a noncyclic VCUG. The bladder was filled with the same volume of contrast during each study and the patient was able to void completely at the conclusion of each exam; however, ceVUS demonstrated grade I reflux while VCUG showed grade III. The second patient was a 2-year-old girl who had a cyclic ceVUS exam followed by a cyclic VCUG. This subject was also able to void completely during each examination. CeVUS showed grade II VUR while VCUG showed grade III, with intermittent dilation of the minor and major calyces of the upper pole of the kidney.
When we take the VCUG as the reference standard, the diagnostic accuracy results for ceVUS are as follows: sensitivity 91.7% (95%; confidence interval [CI]: 61.5%–99.8%), specificity 98% (95%; CI: 89.4%–99.9%), positive predictive value 91.7% (61.1%–98.7%) and negative predictive value 98.0% (88.2%–99.7%).
A Wilcoxon signed rank test showed no significant difference in the actual filling volume of the bladder for ceVUS versus VCUG (P>0.05). A Wilcoxon signed rank test showed that the duration of the ceVUS was significantly longer compared to VCUG, mean time of 9 min and 40 s versus 5 min and 48 s, respectively, (P<0.001).
VCUG detected retrovesical pathology in two children with three periureteral diverticula that were not seen during ceVUS. One child had a unilateral diverticulum associated with grade II VUR and the other child had bilateral diverticula each associated with grade II and III VUR, respectively. All three children had an irregular bladder wall.
Discussion
This phase I clinical trial is the first prospective study of the safety, efficacy and dosing of Optison™ for ceVUS, conducted under an FDA-approved research Investigational New Drug application in the United States. The results provide valuable information about the favorable safety profile of intravesical administration of Optison™ in children, the effective detection and grading of VUR, and the low dose of contrast needed for this examination.
Because there is no prior experience with the intravesical use of Optison™, the study protocol included precautionary measurements to ensure protection of patients and to provide baseline human safety data. The initial cohort enrolled children 2 years of age and older followed by an interim safety review prior to including the more vulnerable populations of infants and neonates in the second cohort. No acute or serious adverse events occurred. The 3.33% observed adverse events rate with one report of transient dysuria is similar to reported adverse events of SonoVue® ceVUS. Ten of the 15 original studies published on SonoVue® ceVUS involving 2,189 children reported safety evaluations [13,14,15,16,17,18,19,20,21,22]. Of these studies, nine specifically noted absence of adverse events [13,14,15,16,17,18,19, 21, 22]. One study reported minor adverse events in 37 children out of 1,010 ceVUS examinations, accounting for 3.66% of the study population [20]. The most common adverse events in that study were dysuria, urinary retention, abdominal pain, anxiety and crying during micturition, blood and mucous discharge, increased frequency of micturition, vomiting, perineal irritation and urinary tract infection. These events were thought to be most likely related to bladder catheterization rather than the intravesical administration of SonoVue®. Our study with Optison™ showed no new or unexpected safety findings compared to SonoVue®.
The second objective of our study was to evaluate the diagnostic accuracy of Optison™ ceVUS for the diagnosis of VUR in children compared to VCUG. Using the VCUG as the gold standard, the sensitivity and specificity of ceVUS were 91.7% and 98%, respectively. These findings are in keeping with the results from studies comparing SonoVue® ceVUS and VCUG. Six previous comparative studies including 684 children demonstrated the high sensitivity and specificity of SonoVue® ceVUS ranging from 80% to 100% and 77.5–98%, respectively [13, 16, 18, 19, 22, 23].
In our series, the concordance between Optison™ ceVUS and VCUG for VUR detection and grading was 84.3% and 81.8%, respectively. VCUG upgraded VUR in two pelviureteric units. These results differ from studies that compared SonoVue® ceVUS and VCUG that found that ceVUS was not only more sensitive for VUR detection but also for higher grades and therefore more clinically significant reflux [19]. The largest comparative study of SonoVue® ceVUS and VCUG evaluated the presence or absence of VUR in 463 pelviureteric units of 228 children. The sensitivities of ceVUS and VCUG in that study were 92% and 64%, respectively. Fifty-six percent of VUR cases were detected only by SonoVue® ceVUS [19]. In the same study, SonoVue® ceVUS also upgraded reflux in 13 pelviureteric units compared with the VCUG VUR grade, whereas the opposite occurred in 4 pelviureteric units. In our series, in the two cases where VCUG upgraded reflux, we found no aberration in contrast preparation, in the procedural technique or the patient’s ability to void during the examinations. Therefore, we assume that the discrepancy between our findings with Optison™ ceVUS and previous studies of SonoVue® ceVUS could be attributed to the intermittent nature of reflux phenomenon and to the fact that although SonoVue® and Optison™ are similar second-generation US contrast agents, there are inherent differences in their molecular structures and microbubble concentrations that may affect their physic-chemical properties and thus their overall echogenic effect. Optison™ microbubbles contain perflutren gas and the shell is composed of human plasma albumin, whereas SonoVue® microbubbles are composed of sulfur hexafluoride gas encapsulated in a monolayer of phospholipids. Moreover, it is also known that the sensitivity of the contrast-specific software for the visualization of microbubbles varies between US manufacturers. Although previous studies provided comprehensive knowledge regarding the procedural steps for ceVUS performance, applying these steps in the clinical setting and adapting them to different sonographic equipment require careful and ongoing adaptation and optimization.
Evaluation of the retrovesical space and associated periureteral pathology is a well-known limitation of ceVUS. The complex pelvic anatomy, two-dimensional imaging and the strong reflective surfaces including rectal gas and ligamentous tissues seen during ceVUS may account for the decreased ability of ceVUS to accurately evaluate the retrovesical space in the absence of a dilated distal ureter [2]. These reasons may account for ceVUS missing a grade I reflux and not detecting the three periureteral diverticula in two patients. Each diverticulum was associated with reflux that was correctly detected and graded by both modalities. In these cases, VCUG with lateral and oblique projections may still have a role in delineation of this complex pelvic anatomy and associated pathology.
Regarding the diagnostic performance of ceVUS, the duration of the examination was significantly longer compared to VCUG. This was expected considering that each kidney kidney and the bladder are scanned individually and repeatedly during ceVUS, which increases the conspicuity of VUR detection due to its intermittent nature. In addition, since this was the first time Optison™ ceVUS was performed, image optimization and operator experience likely led to some degree of increased scan time. The duration of ceVUS examination was shorter for the second age cohort, perhaps due to growing examiner experience, although this difference is not statistically significant. Overall, a 10-min US examination is relatively short and may be tolerated when taking into account all of the added advantages of ceVUS.
We also found that more patients were unable to void completely following ceVUS than VCUG. While the exact reason for this is unknown, one difference was that the catheter was maintained throughout voiding during ceVUS and removed for voiding during VCUG.
Finally, the third objective of our study was to determine the optimal Optison™ dose for ceVUS performance. The results from the previous in vitro study showed that a 0.5% intravesical contrast concentration was optimal. However, this concentration could range from 0.1% up to 1% depending on the US settings and the contrast administration mode [8]. In the present trial, from the very first ceVUS examination the 0.5% concentration of Optison™/normal saline solution was too high and resulted in posterior acoustic shadowing with incomplete visualization of the posterior wall of the urinary bladder and the retrovesical segment of the ureters. Subsequently, the concentration was lowered to 0.2%. Real-time US scanning of the 0.2% solution in the bladder resulted in a homogenous distribution of Optison™ microbubbles. However, throughout each examination, adjustments were necessary to maintain the appearance of the Optison™ solution. For the majority of patients, additional saline was added to facilitate ongoing mixing of bladder contrast. Fewer patients required additional contrast administration.
The lower concentration of Optison™ for in vivo applications compared with the in vitro ones, can be attributed to differences in US equipment and technical parameters such as transducer selection, mechanical index and molecular composition of the contrast agent. This dose of Optison™ is also lower than reported doses of SonoVue® that range from 0.5 mL [13, 20, 21, 24] to 2.5 mL [16, 25], with the majority of the studies considering 1 mL adequate [15, 17,18,19, 22]. These studies also employed a different ceVUS procedural technique where SonoVue® was directly injected into a partially filled bladder and bladder filling was completed by a gravity infusion of normal saline without additional contrast. Duran et al. [15] previously described a technique where a pressure gauge was used to apply a constant pressure, equivalent to a 100-cm column of water, to the contrast/saline bag to maintain a homogenous distribution of microbubbles in the solution. In the current study, we forewent the pressure bag and hung the contrast solution 50–60 cm above the bladder level to evaluate Optison™ under physiological conditions comparable to the practice of VCUG and to assess microbubble distribution as well as the quality of contrast visualization under these conditions.
While preparing the current manuscript, two studies with the use of Optison™ ceVUS in the United States were published [26, 27]. These were retrospective studies and therefore did not require FDA authorization. The first study entailed a group of four children with high grade VUR and intrarenal reflux who underwent comparative performance of Optison™ ceVUS and VCUG in the same session [26]. Similar to our study protocol, Optison™ ceVUS was performed with the infusion technique. The Optison™ dose for ceVUS performance ranged from 0.15 mL to 0.3 mL and was injected into a 250-mL bag of normal saline. In this study, and similar to our results, Optison™ ceVUS and VCUG were equally sensitive to VUR detection in all cases. However, Optison™ ceVUS was more sensitive to detect a case of intrarenal reflux that was missed by VCUG. The second study, from the same group, was a case report of comparative Optison™ ceVUS and VCUG performance in a 9-month-old child [27]. In this study, ceVUS was performed with an infusion of 0.15 mL of Optison™ in a 250-mL bag of normal saline. However, ceVUS was performed after VCUG. Although the VCUG examination showed unilateral grade II reflux, the ceVUS showed no reflux. This presumably was due to the residual volume of the iodinated contrast material that prevented reflux of US microbubbles and resulted in false-negative results. Also of note, these two studies used a different US scanner than our series.
Several limitations and systematic biases are noted in our study. First, there was a small sample population. However, the sample size is in keeping with other phase I trials defined by the FDA that typically enroll 20–80 subjects. Testing in larger patient groups is needed for confirmation. Second, while both ceVUS and VCUG examinations were performed by the same radiologist and therefore could not be blinded, ceVUS was performed first in all cases. Third, the urethra was not evaluated by ceVUS in the present study and therefore the diagnostic accuracy of ceVUS and VCUG regarding urethral morphology was not assessed. Previous studies showed high sensitivity of ceVUS to delineate urethral anatomy and reliably detect urethral pathology in children [28]. Fourth, there is an inherent limitation of ceVUS to evaluate the retrovesical space, particularly in the absence of dilated distal ureter. Fifth, throughout ceVUS examination there was need for ongoing adjustments to optimize the contrast dose. However, since this was the first time that Optison™ was used in a prospective clinical trial, adaptation of ceVUS procedural steps that were established with the use of other similar, but not the same, contrast agents was necessary. Finally, introducing ceVUS into the imaging armamentarium in the United States will not only take time to teach and train practitioners, but will also require evidence that changing to this radiation-free practice is equal to if not more effective than existing standards. Direct comparison of ceVUS with VCUG is an integral part of this process.
Our results demonstrate that when using the Acuson S3000 or Philips Epic US scanners for ceVUS a dose of 0.2 to 0.5 mL Optison™ provides a safe and effective examination, comparable to VCUG to diagnosis of VUR in children. Because Optison™ is approved for adult echocardiography, hospitals and imaging facilities may already have this US contrast agent available in their pharmacies. The results of this study provide necessary guidance for use Optison™ for ceVUS.
Conclusion
The results of this first prospective clinical trial of ceVUS with Optison™ in the United States are in line with prior ceVUS studies and show accuracy and safety of this method. We hope that this trial leads to further development and widespread use of ceVUS in pediatric diagnostic practice as well as support to those who seek to use Optison™ ceVUS.
References
Darge K (2008) Voiding urosonography with ultrasound contrast agents for the diagnosis of vesicoureteric reflux in children. I. Procedure. Pediatr Radiol 38:40–53
Darge K (2008) Voiding urosonography with US contrast agents for the diagnosis of vesicoureteric reflux in children. II. Comparison with radiological examinations. Pediatr Radiol 38:54–63
Darge K (2010) Voiding urosonography with US contrast agent for the diagnosis of vesicoureteric reflux in children: an update. Pediatr Radiol 40:956–962
Riccabona M (2012) Application of a second-generation US contrast agent in infants and children--a European questionnaire-based survey. Pediatr Radiol 42:1471–1480
Rosado E, Riccabona M (2016) Off-label use of ultrasound contrast agents for intravenous applications in children: analysis of the existing literature. J Ultrasound Med 35:487–496
Coleman JL, Navid F, Furman WL et al (2014) Safety of ultrasound contrast agents in the pediatric oncologic population: a single-institution experience. AJR Am J Roentgenol 202:966–970
McCarville MB, Kaste SC, Hoffer FA et al (2012) Contrast-enhanced sonography of malignant pediatric abdominal and pelvic solid tumors: preliminary safety and feasibility data. Pediatr Radiol 42:824–833
Back SJ, Edgar JC, Canning DA et al (2015) Contrast-enhanced voiding urosonography: in vitro evaluation of a second-generation ultrasound contrast agent for in vivo optimization. Pediatr Radiol 45:1496–1505
Koff SA (1983) Estimating bladder capacity in children. Urology 21:248
Darge K, Troeger J (2002) Vesicoureteral reflux grading in contrast-enhanced voiding urosonography. Eur J Radiol 43:122–128
Lebowitz RL, Olbing H, Parkkulainen KV et al (1985) International system of radiographic grading of vesicoureteric reflux. International reflux study in children. Pediatr Radiol 15:105–109
Noga ML, Yarr JE, Chen PE (2012) Evaluation of sevoflurane as an anesthetic agent for voiding cystourethrography in pediatric patients. Can Assoc Radiol J 63:222–227
Ascenti G, Zimbaro G, Mazziotti S et al (2004) Harmonic US imaging of vesicoureteric reflux in children: usefulness of a second generation US contrast agent. Pediatr Radiol 34:481–487
Battelino N, Kljucevsek D, Tomazic M et al (2016) Vesicoureteral refux detection in children: a comparison of the midline-to-orifice distance measurement by ultrasound and voiding urosonography. Pediatr Nephrol 31:957–964
Duran C, del Riego J, Riera L et al (2012) Voiding urosonography including urethrosonography: high-quality examinations with an optimised procedure using a second-generation US contrast agent. Pediatr Radiol 42:660–667
Faizah MZ, Hamzaini AH, Kanaheswari Y et al (2015) Contrast enhanced voiding urosonography (ce-VUS) as a radiation-free technique in the diagnosis of vesicoureteric reflux: our early experience. Med J Malaysia 70:269–272
Kis E, Nyitrai A, Varkonyi I et al (2010) Voiding urosonography with second-generation contrast agent versus voiding cystourethrography. Pediatr Nephrol 25:2289–2293
Kljucevsek D, Battelino N, Tomazic M et al (2012) A comparison of echo-enhanced voiding urosonography with X-ray voiding cystourethrography in the first year of life. Acta Paediatr 101:e235–e239
Papadopoulou F, Anthopoulou A, Siomou E et al (2009) Harmonic voiding urosonography with a second-generation contrast agent for the diagnosis of vesicoureteral reflux. Pediatr Radiol 39:239–244
Papadopoulou F, Ntoulia A, Siomou E et al (2014) Contrast-enhanced voiding urosonography with intravesical administration of a second-generation ultrasound contrast agent for diagnosis of vesicoureteral reflux: prospective evaluation of contrast safety in 1,010 children. Pediatr Radiol 44:719–728
Piskunowicz M, Swieton D, Rybczynska D et al (2016) Premature destruction of microbubbles during voiding urosonography in children and possible underlying mechanisms: post hoc analysis from the prospective study. Biomed Res Int 2016:1764692
Wong LS, Tse KS, Fan TW et al (2014) Voiding urosonography with second-generation ultrasound contrast versus micturating cystourethrography in the diagnosis of vesicoureteric reflux. Eur J Pediatr 173:1095–1101
Darge K, Beer M, Gordjani N (2004) Contrast-enhanced voiding urosonography with the use of a 2nd generation US contrast medium: preliminary results. Pediatr Radiol 34:97
Babu R, Gopinath V, Sai V (2015) Voiding urosonography: contrast-enhanced ultrasound cystography to diagnose vesico-ureteric reflux: a pilot study. J Indian Assoc Pediatr Surg 20:40–41
Wozniak MM, Osemlak P, Pawelec A et al (2014) Intraoperative contrast-enhanced urosonography during endoscopic treatment of vesicoureteral reflux in children. Pediatr Radiol 44:1093–1100
Colleran GC, Barnewolt CE, Chow JS et al (2016) Intrarenal reflux: diagnosis at contrast-enhanced voiding urosonography. J Ultrasound Med 35:1811–1819
Colleran GC, Paltiel HJ, Barnewolt CE et al (2016) Residual intravesical iodinated contrast: a potential cause of false-negative reflux study at contrast-enhanced voiding urosonography. Pediatr Radiol 46:1614–1617
Duran C, Valera A, Alguersuari A et al (2009) Voiding urosonography: the study of the urethra is no longer a limitation of the technique. Pediatr Radiol 39:124–131
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Ntoulia, A., Back, S.J., Shellikeri, S. et al. Contrast-enhanced voiding urosonography (ceVUS) with the intravesical administration of the ultrasound contrast agent Optison™ for vesicoureteral reflux detection in children: a prospective clinical trial. Pediatr Radiol 48, 216–226 (2018). https://doi.org/10.1007/s00247-017-4026-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-4026-3