Abstract
Background
Voiding urosonography (VUS) has proved to be a reliable method for the study of vesicoureteric reflux (VUR). Early reports considered it inadequate for imaging the male urethra.
Objective
To determine the usefulness of contrast-enhanced VUS for the study of the urethra.
Material and methods
A total of 208 children aged 2 days to 10 years underwent VUS to confirm or exclude VUR for different reasons (n = 150) or for follow-up (n = 58). Patients with unconfirmed suspicion of VUR (99 boys and 51 girls) also underwent VUS for the study of the urethra. Examinations were performed using a harmonic imaging mode specific for contrast (Levovist) enhancement. We used a 6–4-MHz convex probe and a transperineal and/or a transpelvic approach.
Results
The neck of the bladder and the entire urethra were visualized in all patients (n = 150). The male urethra was considered normal in 95 boys (95.95%). We diagnosed posterior urethral valves in two patients, diverticulum of the prostatic utricle in one, and diverticulum of the anterior urethra in one. All abnormal cases were confirmed using conventional voiding cystourethrography.
Conclusion
VUS can replace voiding cystourethrography as the method of choice for the initial study of suspected VUR in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of contrast-enhanced voiding urosonography (VUS) for the study of vesicoureteric reflux (VUR) has been thoroughly studied and compared with voiding cystourethrography (VCUG) by different groups, and has been reported to have a sensitivity and specificity in comparison with VCUG approaching 100% (95% CI 96.5%, 100%) [1, 2]. Nevertheless, VCUG remains the most frequently used technique for the diagnosis of VUR, despite exposure of the child to radiation. This might be partly due to the use of pulsed fluoroscopy, which reduces the dose of radiation considerably. In addition, VUS has been considered inadequate for the study of the morphology of the male urethra.
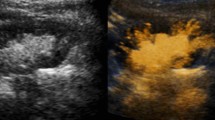
Recent technological advances have brought about a notable improvement in sonographic imaging. Most VUS studies only use grey-scale imaging; however, if a sonographic contrast agent is added, conventional B-mode sonography is unable to differentiate sufficiently signal from the contrast agent from that of the surrounding tissues; thus, structures such as the urinary bladder are only slightly enhanced. To increase the signal from the contrast agent and take advantage of its acoustic properties, diverse techniques called nonlinear imaging techniques have been developed. Specific software based on pulse inversion for use with sonographic contrast agents cancels the signal from tissues without contrast agent while augmenting the signal from the contrast agent (Fig. 1).
The response of the bubbles to the acoustic field depends on the mechanical index (MI) and type of contrast agent. When the MI is low (in general, between 0.05 and 0.5), the bubbles’ oscillation is nonlinear and very rich in harmonics (overtones), which are detected by the nonlinear imaging technology. Moreover, at this MI relatively little destruction of the bubbles occurs, thus enabling real-time viewing of the dynamic enhancement effects over several minutes.
In this article we describe and illustrate how VUS can also be used to study the urethra in children. To our knowledge, this novel technique using low MI combined with pulse-inversion image has not been previously reported.
Materials and methods
Patients
A total of 208 consecutive patients with suspected VUR (n = 150) or VCUG-confirmed VUR (n = 58) underwent contrast-enhanced VUS using galactose-palmitic acid contrast agent (Levovist; Bayer Schering, Berlin, Germany). The first ten patients also underwent VCUG to consolidate the VUS technique. The study was approved by our hospital’s Ethics Committee and written informed consent was obtained from the parents or legal guardians of the children. Patients who were incapable of voiding spontaneously (for example, patients with associated medullary lesions) and patients with neurogenic bladder were excluded from the study.
The 150 patients (51 girls, mean age 28.2 months, range 15 days to 9 years; 99 boys, mean age 14.1 months, range 2 days to 10 years) with suspected VUR for different reasons (urine infection, high-grade postnatal hydronephrosis, siblings with VUR, and structural anomalies on conventional B-mode studies) underwent VUS. The neck of the bladder and the entire urethra were visualized in all studies. The 58 patients with VCUG-confirmed VUR underwent only contrast-enhanced VUS without a specific study of the urethra. A conventional B-mode study including axial and sagittal views of the kidneys and bladder was performed using 6–4-MHz convex probes before contrast-enhanced VUS.
Prophylactic antibiotic (50 mg/kg amoxicillin per day) was administered 1 day before the procedure, on the day of the procedure, and the day after. Sedation was not necessary in any patient. The examination was performed by a team of one radiologist and two technologists.
Equipment and technology
All studies were performed on an Acuson Sequoia 512 ultrasound system (Siemens, Erlangen, Germany). Multifrequency (6–4-MHz) convex transducers were used for the study of the entire urinary tract, although a 14-MHz transducer was used for the study of the urethra in neonates and nursing infants.
To perform VUS, we used a specific harmonic imaging mode based on pulse inversion called contrast-enhanced cadence coherent pulse sequencing (CPS) in our ultrasound system. CPS uses a predetermined low (0.16–0.22) MI that enables the dose of contrast medium to be reduced to half of that used with fundamental US [4, 5], and extends the effective examination time by reducing the amount of microbubble destruction. This software also enables colour coding of conventional B-mode signals and simultaneous visualization of the target organ in conventional B-mode images and harmonic images, which is useful because it allows the contrast medium to be viewed with a simultaneous reference image of the area studied.
The image characteristics were preadjusted and we only modified the frequency, time-gain compensation, and depth of focus to optimize image quality. We used linear 14-MHz probes in our initial 20 patients (mean age 6 months). Since the attenuation of the harmonic frequency is much higher than in B-mode imaging, we replaced the 14-MHz probe with a 6–4-MHz probe for the study of the urethra; this made it possible to use a single probe for the entire examination (Table 1).
Image analysis in contrast-enhanced VUS
All examinations were recorded and stored in the PACS to enable re-viewing. We calculated the duration of the procedure (from the start of bladder filling, including axial and sagittal series of both kidneys and ureters, selective study of the urethra during voiding, and examination of the urinary tract after voiding) and the duration of the urethral study (from removal of the vesical catheter to the end of spontaneous voiding). It was not necessary to repeat the study in any patient. All examinations were performed and/or verified by a senior radiologist with 26 years experience as a paediatric radiologist and 2.5 years experience of contrast-enhanced VUS.
Contrast-enhanced VUS included axial and longitudinal slices of the kidneys and bladder using a transabdominal approach. The study of the urethra was performed using the transperineal and transpelvic approaches in boys and the transpelvic–translabial approach in girls.
We inserted into the patient’s urethra a 5F or 8F catheter connected to a three-way stopcock attached to a bag of saline solution placed 70–100 cm above the patient’s head and inserted a syringe with 7 ml of galactose-palmitic acid contrast agent (300 mg/ml) into the remaining opening. Contrast medium dosage was 5% of the estimate from the formula [(age in years + 2) × 30] ml [3, 4]. First, a small amount of saline solution was instilled into the bladder by gravity. Then the entire volume of contrast agent was injected slowly to avoid rupture of the microbubbles and to ensure its homogeneous incorporation. Next, the bladder was allowed to fill to maximum capacity by gravity. During bladder filling the distal ureters and the kidneys were screened for VUR. When the bladder was completely full, i.e. when the patient started to void around the catheter, the catheter was withdrawn and the transperineal study began.
The 6–4-MHz convex transducer, which allowed the field of view to be increased, was placed sagittally at the interscrotal level in boys (Fig. 2). The transpelvic approach (i.e. placing the convex transducer sagittally against the suprapubic area of the abdominal wall) was also used in boys (Fig. 3) in cases of urgent or uncontrolled voiding so that the neck of the bladder and entire urethra could be thoroughly studied. Ureters and kidneys were also studied.
A transpelvic approach was used for the study of the urethra in girls (i.e. placing the convex transducer sagittally against the suprapubic area of the abdominal wall; Fig. 4). In some girls, a longitudinal interlabial approach was used.
The transperineal approach was used in patients with a fully distended bladder just before voiding, because this improved the morphological detail and ensured that the images obtained would correlate with those obtained at VCUG. We opted for the transpelvic approach in patients in whom voiding occurred immediately or was uncontrollable, as well as at the end of each examination to assess bladder voiding (Fig. 5).
We were able to use both approaches in many patients by starting the examination of the urethra with the transperineal approach and using the transpelvic approach to evaluate the voiding of the bladder and the homogeneous progression of the contrast material through the urethra. During voiding, the presence of obstruction or other alterations in the urethra were evaluated. In boys, the transverse urethral diameter was determined in the posterior and bulbar portions at maximum distension. Urethras with acceptable distension and continuous homogeneous progression of contrast medium were considered normal [2]. Lastly, the kidneys were studied again with the convex probe and the study was completed with a final transpelvic approach to observe bladder voiding and the residue after voiding.
Results
Only the results of the urethral study are presented. We were able to study the entire urethra using contrast-enhanced VUS in all patients.
Male patients
The transperineal approach was used in 94 patients (95%), the transpelvic approach in 5 (5%), and both approaches in 44 (44%). The quality of the images obtained depended on the frequency used in the transperineal approach, whereas in the transpelvic approach image quality was related to anatomical parameters, as the best image quality was obtained in patients under 2 years of age. The mean duration of the examination when the same convex transducer was used for both the study of the upper urinary tract and the urethra was 8.9 min (range 3–26 min). The mean duration of the study of the urethra was 44 s (range 3–100 s). Examinations were recorded on video and/or as single or sequential still images without freezing the image on the monitor.
In 95 of the 99 patients, the urethral findings were normal. The mean distension of the posterior urethra during voiding was 6.4±0.78 mm (range 4.0–9.2 mm) and of the anterior urethra was 5.8±0.91 mm (range 3.3–8.9 mm). The difference in calibre between the posterior and anterior urethras ranged between 0 and 2 mm.
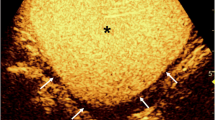
Posterior urethral valves were diagnosed in two patients (Fig. 6) and these findings were confirmed at VCUG (Fig. 7). In comparison with healthy subjects, these patients had a dilated posterior urethra (10 and 14 mm, respectively), poor distension of the valve area and reduced calibre of the anterior urethra (2 and 1.5 mm, respectively), and progression of the contrast agent through the urethra was clearly slower. Moreover, both had a thickened irregular bladder wall with diverticula and bilateral grade V VUR.
A 3-day-old boy with posterior urethral valves. Note the thick-walled bladder (b), pseudodiverticula (D), marked dilatation of the posterior urethra (PU) (distance between callipers 10 mm) and reduced calibre of the anterior urethra (AU). There is a thin column of contrast agent through the region of the valve (V)
In one patient anterior urethral diverticulum was diagnosed when a difference one-third or more of the urethral diameter was observed in the diverticular and post-diverticular areas (Fig. 8). A selective study of the anterior urethra using an 8-MHz linear probe demonstrated the presence of a valve in the posterior edge of the dilated portion of the urethra proximal to the stenosis (Fig. 9).
Finally, we observed a prostatic diverticulum associated with scrotal hypospadias in a patient with WARG syndrome (Wilms tumour, aniridia, mental retardation, and genitourinary anomalies) and in one patient an intravesical ureterocele with a normal urethra.
Female patients
A 6-MHz probe was used in 43 girls (mean age 24 months) and a 4-MHz probe was necessary in 8 girls (mean age 70 months). In most patients, the transpelvic approach was used; the interlabial approach was only used in five patients to enable adequate study of the urethra. The mean duration of the entire study, including the bladder and the kidney, was 7.5 min (range 3–16 min) and of the urethra 28 s (range 5–94 s), and video or still images were obtained of a single voiding.
The urethral findings were normal in all examinations, with rapid passage of contrast agent from the bladder and homogeneous urethral distension (mean 5.9±1.1 mm, range 4.0–9.0 mm). Urethrovaginal reflux, considered physiological, was documented in 15 patients. The microbubbles remained stable long enough to enable thorough study of the urethra in all patients, even in those with delayed voiding.
Discussion
To date, six studies of selective study of the urethra with contrast-enhanced VUS using the transperineal approach and B-mode imaging have been reported [5–10]. The most noteworthy, by Berrocal et al. [9], correlated the urethral findings on contrast-enhanced VCUS (voiding cystourethrosonography) and VCUG in 146 patients. Nevertheless, the latest guidelines do not include contrast-enhanced VCUS or VUS in the diagnostic work-up for VUR, and it is generally believed that this technique should not replace VCUG in the initial study of the urethra in boys with suspected VUR.
In recent years, specific harmonic programs for use with sonographic contrast agents have evolved considerably, and it is now possible to obtain images of much higher quality in comparison with those of earlier studies. We believe that two factors are mainly responsible for the improvement in the images obtained. Low MI (0.1–0.5) avoids much of the destruction of contrast bubbles that limited earlier studies performed at higher MI. Thus the viable imaging time has increased enough to allow dynamic enhancement to be continuously visualized in real time throughout the examination. On the other hand, due to the much higher attenuation of harmonic frequency, the 14-MHz linear probe used in other studies can be replaced by a 6-MHz convex probe for the study of the urethra. This not only clearly improves the anatomical definition of the examination, but also makes the examination easier to perform, as it is not necessary to change probes to study the different areas of the urinary system. Moreover, unlike linear or microconvex probes, the convex probe allows a complete panoramic image of the urethra and neck of the bladder, as well as of much of the bladder, without moving the probe.
Thus the use of harmonic programs for contrast enhancement with colour coding of the sonographic signal (B-mode) on the one hand, and the use of convex probes on the other, enabled us to obtain high-quality morphological and functional images of the urethra, regardless of whether we used the transperineal or transpelvic approach. The transperineal approach, which has already been used for the study of the urethra in B-mode sonographic studies, makes it possible to obtain VUS images that can be superimposed over VCUG images. The images obtained at VUS are of similar or superior quality to the VCUG images; they can be easily interpreted by radiologists and easily explained to other specialists who deal with nephrological pathology. Therefore, in our experience, VUS should be the technique of choice. The transpelvic approach, not previously described, is useful in patients with uncontrollable or urgent voiding to guarantee the morphological study, and also for the overall dynamic and functional evaluation of bladder voiding. The best quality images are obtained in patients under 2 years of age, which is also the age when the technique is most indicated.
The most common urethral pathology and the primary pathological consideration is posterior urethral valves. Some urethral pathologies that can cause VUR are extremely rare. To date, 22 patients with posterior urethral valves and two with anterior urethral diverticulum diagnosed with VUS have been reported [11]. Other entities such as syringocele or urethral duplication are so rare that they have yet to be encountered with VUS. On the other hand, other authors [12] believe that VUS should also demonstrate its utility in the evaluation of complex anorectal and cloacal malformations or of ectopic ureter (70% are associated with complete ureteric duplication), in which patients usually undergo several cystographic studies. In our experience, MRI provides the necessary information and should be the technique of choice in these cases.
In our study, in the two patients with posterior urethral valves, we observed a dilated posterior urethra and difficulty in the flow of contrast material into the anterior urethra; only a thin thread of contrast medium reached the anterior urethra in an intermittent urinary jet that lengthened the voiding time. Furthermore, unlike in healthy subjects, the contrast material was retained behind the valve area throughout the voiding phase. The differences between healthy patients and those with posterior urethral valves were, therefore, very clear. In the patient with an anterior urethral diverticulum we observed dilatation of the portion of the urethra that was proximal to the stenosis and an abrupt change of calibre between the pre- and poststenotic segments.
The dynamic information obtained by VUS can be especially useful in patients who have undergone surgery for posterior urethral valves. In our study, all these patients had some dilatation of the posterior urethra; however, the passage of contrast agent through the entire urethra and the degree of distension of the anterior urethra was normal in all patients.
Some authors argue that, unlike VCUG, the sensitivity of VUS depends on the experience of the operator. We believe that if the procedure is done correctly the diagnostic performance should not be influenced by this factor. The cooperation of the patient and the preparation of the health-care team are also important to ensure good results.
In our study, we evaluated each of the anatomical regions of the male and female urethra. Although the group of patients with urethral anomalies is small, we consider that the images obtained with VUS are comparable to VCUG images in patients with posterior urethral valves (the most common anomaly) and anterior urethral diverticulum.
Conclusion
VUS is a reliable technique that is sufficiently sensitive and specific for study of the urethra. It should be the initial imaging examination in children, both boys and girls, with suspected VUR. Image quality is equal or superior to that of VCUG and it does not use ionizing radiation; therefore, it can replace VCUG in this context. Conventional cystography should be indicated in patients with abnormal urethral findings not yet described by VUS and/or to plan surgery if necessary.
References
Darge K (2008) Voiding urosonography with ultrasound contrast agents for the diagnosis of vesicoureteric reflux in children. II Comparison with radiological examinations. Pediatr Radiol 38:54–63
Berrocal T, Gayá F, Arjonilla A et al (2001) Vesicoureteral reflux: diagnosis and grading with echo-enhanced cystourethrography versus voiding cystourethrography. Radiology 221:359–365
Kopitzko A, Cornely D, Reither K et al (2004) Low contrast dose voiding urosonography in children with phase inversion imaging. Eur Radiol 14:2290–2296
Darge K, Moeller RT, Trusen A et al (2005) Diagnosis of vesicoureteric reflux with low-dose contrast-enhanced harmonic ultrasound imaging. Pediatr Radiol 35:73–78
Bosio M, Manzoni GA (2002) Detection of posterior urethral valves with voiding cystourethrosonography with echo contrast. J Urol 168:1711–1715
Maté A, Bargiela A, Mosteiro S et al (2003) Contrast ultrasound of the urethra in children. Eur Radiol 13:1534–1537
Xhepa R, Bosio M, Manzoni G (2004) Voiding cystourethrosonography for the diagnosis of vesicoureteral reflux in a developing country. Pediatr Nephrol 19:638–643
Berrocal T, Rivas S, Jaureguizar E et al (2004) Contrast-enhanced sonourethrography versus conventional miction cystourethrography in the assessment of the urethra: preliminary study. Cir Pediatr 17:58–60
Berrocal T, Gaya F, Arjonilla A (2005) Vesicoureteral reflux: can the urethra be adequately assessed by using contrast-enhanced voiding US of the bladder. Radiology 234:235–241
Bosio M (2002) Role of ultrasound in the imaging of posterior urethral valves. Rays 27:135–139
Darge K (2008) Voiding urosonography with ultrasound contrast agents for the diagnosis of vesicoureteric reflux in children. I Procedure. Pediatr Radiol 38:40–53
Riccabona M (2003) Contrast ultrasound of the urethra in children. Eur Radiol 13:1494–1495
Acknowledgements
We gratefully acknowledge the contribution and support of our special procedure technicians Ines Artacho and Lourdes Sanchez. We also thank John Giba for linguistic aid. Without their help this work would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duran, C., Valera, A., Alguersuari, A. et al. Voiding urosonography: the study of the urethra is no longer a limitation of the technique. Pediatr Radiol 39, 124–131 (2009). https://doi.org/10.1007/s00247-008-1050-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-008-1050-3