Abstract
Voiding urosonography (VUS) entails the intravesical administration of US contrast agent (USCA) for the diagnosis of vesicoureteric reflux (VUR). VUS is now recognized as a practical, safe, radiation-free modality with comparable or higher sensitivity than direct radionuclide cystography (DRNC) and voiding cystourethrography (VCUG), respectively. An extensive review of the literature regarding both the procedural aspects and comparative diagnostic values of VUS has been published (Darge Pediatr Radiol 38:40–63, 2008a, b). The aim of this review is to provide an update on various facets of VUS that have taken place since the publication of the above-mentioned two reviews.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Voiding urosonography (VUS) entails the intravesical administration of US contrast agent (USCA) for the diagnosis of vesicoureteric reflux (VUR). VUS is now recognized as a practical, safe, radiation-free modality with comparable or higher sensitivity than direct radionuclide cystography (DRNC) and voiding cystourethrography (VCUG), respectively. An extensive review of the literature regarding both the procedural aspects and comparative diagnostic values of VUS has been published [1, 2]. The aim of this review is to provide an update on various facets of VUS that have taken place since the publication of the above-mentioned two reviews.
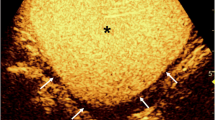
VUS with the intravesical administration of the second-generation US contrast agent SonoVue and use of low MI contrast-specific modality (Coded Contrast Imaging, General Electric, Fairfield, CT). a Pre-contrast scan of the right kidney and (b) contrast-enhanced image demonstrate only the hyperechogenic microbubbles in the renal pelvis with background subtraction; conspicuous depiction of vesicoureteric reflux (arrow) (courtesy of Papadopoulou F, Ioannina, Greece)
There is mounting evidence that VUR does not play such a central role in the pathophysiology of renal damage, as was believed in the past. Consequently, there is decreasing priority and emphasis in imaging for VUR [3, 4]. There is an increasing trend in the management of urinary tract infection (UTI) in children, to primarily diagnose acute pyelonephritis rather than VUR [5]. In one current study in young children with first febrile UTI, the sensitivity for high grade VUR of the combined use of US of the bladder and kidneys and technetium-99 m-labeled dimercaptosuccinic acid (DMSA) scanning was 83% [6]. The negative predictive value of the two modalities together turned out to be 92%. Thus the “top-down” approach with reflux diagnosis first, has started to be taken over by the “bottom-up” pathway by performing US and DMSA first and only if these are positive going on to do reflux study [5, 6]. This is also evident in the imaging recommendation on UTI by the European Society of Uroradiology (ESUR) Paediatric Guideline Subcommittee and the European Society of Paediatric Radiology (ESPR) Paediatric Uroradiology Working Group [7]. Consequently, VUS is facing this decreasing trend as much as VCUG and DRNC. On the other hand, coupled with increasing awareness of the negative effects of ionizing radiation in children, there is growing interest in replacing VCUG with VUS to diagnose VUR. The higher sensitivity of VUS in the detection of VUR is an additional advantage of the method over VCUG [2]. The reduced sensitivity of VCUG had also been demonstrated in a comparative study with DRNC, 45% versus 91%, respectively [8]. In a cyclic VCUG study when the initial VCUG showed no VUR, 20% of second cycle studies demonstrated VUR [9]. Higher sensitivity and absence of radiation stand out with VUS.
Procedural details
The basic procedural steps of VUS encompass: (a) US of the kidneys and bladder; (b) bladder catheterization and intravesical administration of normal saline and USCA and (c) repeat scan of the bladder and kidneys during and after bladder filling and finally all through voiding [1]. During the latter step, in some centres, urethrosonography (transpubic and/or transperineal) is added. The reflux is ranked in grades 1–5 similar to that for VCUG. The most commonly used USCAs are Levovist (Bayer-Schering Pharma, Berlin, Germany) and SonoVue (Bracco, Milan, Italy) [1]. Levovist is a first-generation USCA based on galactose with air-filled microbubbles stabilized with palmitic acid [1, 10]. SonoVue is a second-generation USCA composed of stabilized aqueous suspension of sulphur hexafluoride (SF6) microbubbles with a phospholipid shell [1, 10]. Echovist (Bayer-Schering Pharma, Berlin, Germany) and Albunex (Mallinckrodt, Pharmaceuticals Covidien, Hazelwood, MO, USA), both first-generation USCAs, are no longer used for VUS [10, 11].
Different US modalities are employed for contrast-enhanced studies. These include gray-scale (fundamental) US, colour Doppler US, harmonic imaging and contrast-specific modalities [1, 12, 13]. The latter are the newest US modalities with the highest contrast resolution including the option of colour overlay of the microbubbles. The additional important feature is the capability to suppress the signal from surrounding tissues with only the microbubbles being visible, analogous to a subtraction image in MRI or angiography [1, 12, 13]. The contrast-specific modalities can be tuned for the USCA according to the resonance frequency of the specific microbubbles, and carried out with high or low mechanical indices (MI). Depending on the manufacturer of the US scanner, the types of contrast-specific US techniques are variable and come under different names. They are based on some form of pseudo-Doppler, harmonic imaging, coded imaging, phase or amplitude modulation or a combination of the above. A detailed description and listing of the current contrast-specific techniques has been published by Quaia [12]. In consideration of potential safety issues, and also not to disrupt the microbubbles and reduce the available scan time, the low-MI contrast-specific technique will most likely turn out in the future to be the modality of choice for VUS (Fig. 1).
The duration for VUS with Levovist using just gray-scale imaging had been reported to be between 26 and 34 min [1]. This included catheterization and the pre-contrast US took up almost one-third of the time. Comparable duration for a VCUG was 13–20 min. In a recent study by Piscitelli et al. [14] using gray-scale and colour Doppler the average VUS duration was 32 min and thus has not changed very much. Duran et al. [15] performed VUS and urethrosonography with Levovist and low-MI contrast-specific modality. The mean duration of the examination when the same convex transducer was used for both the study of the upper urinary tract and the urethra, was 8.9 min. This is indeed a significant reduction in examination time. The mean duration of just urethrosonography was 44 s. Papadopoulou et al. [16] using SonoVue and low-MI contrast-specific modality reported the duration of VUS study to be 15–20 min [16]. With the advancement of contrast US modalities and the availability of more stable USCAs, there is definitely increasing potential to reduce the time of the study to one comparable to VCUG.
The addition of urethrosonography to VUS had been shown to be feasible and that for practical purposes provided all the necessary diagnostic information. In the last review the conglomerate data of six studies dealing exclusively or partly with contrast-enhanced voiding US of the urethra comprised 647 boys and 200 girls. An unbiased comparison of all cases with VCUG was carried out in only two studies. In one of these the sensitivity and specificity of contrast-enhanced urethrosonography was reported to be 100% [2]. In a newer study 150 children, 51 girls (15 days to 9 years, mean 28 months) and 99 boys (2 days to 10 years, mean 14 months) underwent Levovist-enhanced VUS combined with evaluation of the urethra [15]. In those with an abnormal finding VCUG was performed subsequently. The dose of USCA administered was a volume of 5% of that of bladder filling and the contrast-specific modality used low MI and colour overlay. The urethra was imaged with transpelvic and transperineal US. The normal values of urethral distension during voiding were determined. For boys the mean posterior/anterior urethral distension was 6.4 ± 0.78/5.8 ± 0.91 mm, respectively. The mean urethral distension in girls was 5.9 ± 1.1 mm. Two boys were found to have posterior urethral valves (posterior urethra diameters 10 and 14 mm), one boy a diverticulum of the prostatic utricle and one other a diverticulum of the anterior urethra, that were all confirmed at VCUG. Incidentally, in 15 girls urethrovaginal reflux, regarded as physiological, was observed. The quality of the contrast-enhanced urethra images presented in the publication is of unparalleled excellent quality. The low MI contrast-specific modality is a significant leap in quality compared to the gray-scale images presented in the past [1]. From the images and results of the study one can confidently agree with the title of the paper: “Voiding urosonography: the study of the urethra is no longer a limitation of the technique” [15]. Kopac et al. [17] went further and combined VUS with genitography in a baby with ambiguous genitalia. They were able to depict vaginal reflux from the urethra and a common distal urethral and vaginal channel, a urogenital sinus.
Commonly, the diagnosis of VUR is based on a real-time examination decision at the time of the study. With standardization of the VUS documentation and reading in mind, Galloy et al. [18] evaluated whether there would be a difference in the detection of VUR based on the off-site review of digital US clips compared to digital VCUG images [18]. Levovist-enhanced VUS with harmonic imaging and VCUG were performed in 130 children. Digital VUS clips and digital VCUG images were reviewed off-site each by two radiologists. For VUS the intraobserver reproducibility for detection and grading of VUR was good to moderate (k = 0.53 and 0.67) and good (k = 0.64 and 0.70), respectively. The interobserver reproducibility for VUS was also good to moderate (k = 0.51 and 0.73), but for VCUG excellent (k = 0.89 and 0.91). Thus, for VUS, just reading selected US clips by someone not performing or present during the study appears to be disadvantageous. The authors do point out some of the limitations of their study: (a) the radiologists reading VUS were not experienced with doing or reading such a study; (b) possible image degradation due to clip transfer; (c) loss of real-time targeted evaluation and (d) no use of contrast-specific modality. Future efforts to improve the quality of VUS need to incorporate measures to standardize the documentation of the VUS.
For the first time VUS has been added by the European Federation of Societies of Ultrasound in Medicine and Biology (EFSUMB) in their “Guidelines and good clinical practice recommendation for contrast enhanced ultrasound (CEUS)—update 2008” [19]. Furthermore, detailed procedural description of VUS can also be found in the recent recommendation by the ESPR and ESUR [7].
Adverse events monitoring of intravesical US contrast agents
The absence of USCA-related adverse event after the intravesical administration of Levovist had been previously reported by five different studies that comprised a total of 626 patients with an age range of 2 days to 20 years [1]. Newer studies have confirmed this observation. Piscitelli et al. [14] performed Levovist-enhanced VUS in 157 children, ages 6 weeks to 4.7 years. Although it is not explicitly described how the monitoring for possible adverse events was conducted, it is stated that no adverse event related to the intravesical administration of Levovist was observed. Similarly, Kljucevsek et al. [20] conducted Levovist-enhanced VUS in 75 children (3–12 years), without encountering any adverse event. In the largest study to date Papadopoulou et al. [16] evaluated the second-generation USCA SonoVue for possible adverse events. VUS was carried out with intravesical administration at a dose of 1 ml/bladder filling in 228 children. Contrast-specific US imaging modality with low MI was employed. Following VUS, the children were kept and monitored for 6 h in the day clinic and followed up 24 h later by phone. Again no problem related to the intravesical administration of SonoVue was reported.
The possibility of inducing glomerular capillary haemorrhage with US when scanning after intravenous administration of USCA has been described in some animal studies [21, 22]. A recent study using diagnostic US has shown that this adverse event is frequency dependent [23]. In animal experiments glomerular capillary haemorrhage was not detected for diagnostic US at 5.0 or 7.4 MHz for the highest peak rarefactional pressure amplitudes (PRPAs), but at 1.5–3.5 MHz [23]. To reduce potential glomerular capillary haemorrhage during intravenous use of USCA the following measures are generally recommended: low MI setting, US modality incorporating colour Doppler, low USCA dose and short scan time. It has also been stressed that the animal studies results may not be extrapolated to human diagnostic US as additional factors come into play in mitigating the US power. The medical significance of the experimentally observed microscale bioeffects of diagnostic US with USCA are presently uncertain.
When considering the above points, the advantages of intravesical administration of USCA compared to intravenous administration stand out: (a) USCA is administered in a bladder already filled with at least some normal saline thus the microbubble concentration is low and they occupy a relatively large volume and are not confined in a small space such as in a capillary; (b) in the renal pelves and calyces again the USCA is in a relatively large space and mixed with normal saline and urine; (c) once reflux is documented there is no need to continue scanning and thus the actual scan of the renal pelvis filled with microbubbles does not exceed a few seconds; (d) US transducers used in children are of higher frequency and thus decrease the chance of disrupting the microbubbles; (e) the newer contrast-specific US modalities allow the use of low MI and some have integrated in the specific modality colour/power Doppler imaging, too. Thus the intravesical administration of USCA during paediatric diagnostic US have potentially a much higher safety margin than the intravenous use of the same USCA.
Comparison of VUS with radiological examinations
Comparative studies of VUS with VCUG or DRNC up to early 2007 had been analyzed and detailed tables demonstrating the diagnostic values and reflux grading presented by Darge [2]. Comparative studies with DRNC were too few and thus conclusive statement regarding sensitivity of VUS was not possible. A recent study compared in 39 patients Levovist-enhanced VUS (grayscale and colour Doppler) with DRNC and reported the sensitivity and specificity of VUS to be 100% [14].
There were at least 18 comparative studies of Levovist-enhanced VUS with VCUG encompassing 1,338 patients with 2,893 pelvi-ureteral-units (PUUs) [2]. With the exception of two studies the diagnostic accuracy was 90% and above with a mean of 91%. With VCUG as the reference method the range of results for VUS were as follows: sensitivity 57–100%, specificity 85–100%, positive/negative predictive values 58–100%/87–100%, respectively, diagnostic accuracy 78–96%. In 19% of PUUs the diagnosis was made only in VUS and in 10% only in VCUG. Thus, in 9% of PUUs more refluxing systems were detected using VUS. In 73.6% the reflux grades were concordant in VUS and VCUG. Reflux grade was found to be higher in VUS than VCUG in 19.6% of PUUs. In 71.2% of PUUs with grade I reflux on VCUG, microbubbles were detected in the respective renal pelvises on VUS i.e. were grade II and higher. A recent comparative study with 118 patients with 233 PUUs again demonstrated for VUS sensitivity and specificity of 96% and 95%, respectively [14]. Seven cases of reflux detected by VUS, five grade II and two grade III were not identified by VCUG. Only two cases of grade I reflux on VCUG were not detected by VUS. However, it is important to note that VCUG demonstrated four bladder and two para-ureteral diverticulae not detected on VUS [14].
The largest comparative study between VCUG and VUS with the intravesical administration of the second-generation USCA SonoVue, published to date, is by Papadopoulou et al. [16]. It comprises a total of 228 children, 123 boys and 105 girls, 6 days to 13 years old, with a total of 463 PUUs. SonoVue was administered at a dose of 1 ml/bladder filling and a contrast-specific harmonic modality with low-MI and subtractive imaging technique (Esatune 570 FD high-definition scanner, Esaote, Milan, Italy) was employed. In 161 (35%) PUUs reflux was detected by one or both methods. In 90 (56%) PUUs reflux was detected only by VUS and in 14 (9%) PUUs only by VCUG. This implies a 47% higher reflux detection rate for SonoVue-enhanced VUS compared to VCUG, which is almost 1.5-times higher than the highest reported rate for Levovist-enhanced VUS [2]. Concordance of VUS and VCUG was 78%. More importantly refluxes missed by VCUG were of higher grades (2 grade 1, 65 grade II, 19 grade III, 4 grade IV) compared to those missed by VUS (8 grade I, 5 grade II, 1 grade III). When VCUG was used as the reference method the sensitivity of VUS was 80%. When all refluxing PUUs in either method were considered as true positive, sensitivity of VUS and VCUG was 92% and 64%, respectively. These results underline that VUS with a second-generation USCA and contrast-specific US modality is not only from a safety perspective, but with a much higher sensitivity, potentially the study of choice in the future.
The comparison of VUS using solely short digital clips with digital images of VCUG, in an off-site manner by a radiologist not experienced with VUS, resulted in lower sensitivity (63%), specificity (83%) and positive predictive value (50%) [17]. The negative predictive value (89%) was still in the higher range. The limitations of such a reading have been discussed above.
Selection criteria for VUS
VUS has the potential to fully replace DRNC. When it comes to VCUG the commonly used selection criteria of VUS as the primary diagnostic imaging modality for VUR are: (a) follow-up examinations; (b) first examination in girls and (c) screening high-risk patients [2, 24]. VCUG is selected as the primary modality (a) when on US the bladder or one of the kidneys cannot be visualized, (b) as first examination in boys, and (c) for specific urethral and/or bladder morphology and/or functional evaluation. The fact that urethral imaging may not be a limitation has been pointed out in the recent study discussed above [15]. Others are performing VUS as a primary modality for reflux [25]. These may point to a trend of expansion of the selection criteria for VUS.
One aspect of VUS that has not been evaluated in-depth before is how it may have changed the diagnostic and management algorithm of VUR in daily practice. Giordano et al. [25] had performed a total of 610 VUS studies, over a period of 6 years, for the primary investigation of reflux. Only 2 boys suspected to have PUV from US went directly to VCUG. If the VUS turned out to be positive, therapeutic decision was made together with the urologists as to whether antibiotic prophylaxis, endoscopic treatment or open surgery should be carried out. VCUG was performed only in cases (a) where the VUS was non-diagnostic due to poor patient cooperation; (b) in the context of high-grade reflux after consultation with the urologists when surgical intervention was being considered; (c) de-novo onset of UTI during antibiotic prophylaxis and (d) in the presence of complex malformations. As a second step VCUG was performed in only 60 of 610 children. In 90% of children VCUG could be avoided. This is significantly higher than reported previously [24]. In the 60 children who underwent both VUS and VCUG the diagnostic agreement of both studies was 96%. When they compared the results of the VCUG (prior to instituting VUS as the primary reflux diagnostic modality) to the results of the VUS years, the reflux detection rates were as follows for VCUG/VUS: UTI group 30%/36% and non-UTI group 8.7%/27%, respectively. Thus after establishing VUS as the primary reflux imaging modality more refluxes were being detected than during a comparable period with VCUG alone.
With regard to selection of VUS, one other interesting aspect being discussed is the use of catheter-free methods for reflux screening prior to performing VUS [20]. This is important as it is in particular propagated by the University Medical Centre in Ljubljana, Slovenia where probably the highest number of VUS (>5,000) have been performed to date worldwide (personal communication). It is no doubt that bladder catheterization is the most invasive part of reflux examination and many attempts have been made in the past to diagnose reflux without direct bladder filling using a catheter [11].
Kljucevsek et al. [20] performed in 75 children (age range 3–12 years) ureteric jet Doppler waveform (UJDW) evaluation prior to Levovist-enhanced VUS [20]. They recorded at least 10 UJDWs per ureteric unit. UJDW was classified according to the shape of the waveform as suggestive or not suggestive of reflux. Using VUS as a reference the overall sensitivity and specificity of the UJDW for detection of reflux was 88.5% and 82.3%, respectively. They concluded that UJDW study should be considered primarily for screening prior to catheterization and performing VUS. This will not only lead to less invasive catheterization for reflux diagnosis, but also decrease the amount of USCA needed and thus lower the cost of the overall studies.
Status of contrast-enhanced US and VUS
There is increasing use of intravenous USCA in adults for both cardiac and non-cardiac studies [26]. In the latter group the most advanced and widely used contrast-enhanced US (CEUS) is that of the liver. This is particularly true in Europe and Asia. Non-cardiac CEUS has also become a cost-effective method. It can be performed at the bedside and is without radiation and nephrotoxicity. Most importantly it can provide accurate diagnostic information comparable to CT and MRI. Contrary to other parts of the world, in the United States only two agents are approved for intravenous contrast-enhanced echocardiography. These two USCA are both second-generation perfluorocarbon contrast agents: Optison (GE Healthcare, Little Chalfont, UK) and Definity (Lantheus Medical Imaging, North Billerica, MA, USA). For non-cardiac use no agent has been approved to date by the U. S. Food and Drug Administration (FDA) [26]. The obstacles in the non-cardiac use of USCA are both regulatory and practice patterns. To support approval of USCA by the FDA a taskforce for CEUS has been established in the American Institute of Ultrasound in Medicine (AIUM). This taskforce has also produced a protocol for the performance of a clinical trial using USCAs to image the liver [27]. Key issues addressed in the protocol are appropriate end points, examination procedures, equipment criteria, safety and training. One of the practice patterns that hampers the use of CEUS is that for many of the indications, CT or MRI are carried out. These do not require the direct involvement of the radiologist as much as CEUS would entail. The differences in reimbursement based on relative value units between US and CT or MRI and the fact that CEUS is currently not reimbursable are additional obstacles. Therefore, radiologists have little incentive to use CEUS. This may change with increasing concern about the excess radiation dose of CT and possible nephrogenic systemic fibrosis with the use of gadolinium contrast agents in MRI. Recently, an International Contrast Ultrasound Society (ICUS, www.ICUS-society.org) was formed to promote the use of USCA, respond to regulatory agencies and educate the medical community and the public about the benefits of USCAs.
Most of the publications on VUS are from Europe [1, 2]. There had been few reports from other parts of the world, except North America. A 2009 publication on a survey points to the possibility that this may change in the near future [28]. The survey was on voiding cystography practices and preferences of fellows of the American Academy of Pediatrics Section of Urology, the largest organization of paediatric urologists in North America. A 5-page survey with 40 questions was sent out to the 301 fellows. The response rate was 62%. In this questionnaire information about the use of VCUG, DRNC, and surprisingly about VUS was asked. Sixteen-percent indicated that VUS was available in their community. Factors influencing the modality choice were imaging of urethra, accuracy of grading and sensitivity of the test. Child friendliness of staff or availability of a paediatric radiology service, radiation dose, patient age and availability of modalities were found to be of lesser importance in the choice of imaging for VUR. Although the conventional methods VCUG or DRNC were listed as the preferred methods in most cases, it is interesting to note the following percentages regarding the selection of VUS as the primary imaging modality for VUR: initial mode of study (1%), follow-up of VUR (2%), sibling screening (11%), postnatal evaluation of prenatal hydronephrosis (3%), follow-up after open correction of VUR (5%) and follow-up after endoscopic correction of VUR (4%). The fact that VUS was considered for the very first time in such a survey combined with the unexpected high response regarding VUS are positive trends regarding the future of VUS in the USA. The approval by the FDA of SonoVue that is being used for VUS in Europe would give further boost for VUS. Bracco started in October 2009 in the USA a Phase III clinical trial on the application of SonoVue for imaging focal liver lesions (http://clinicaltrials.gov/ct2/show/NCT00788697?term=SonoVue&rank=20). There are no publications on VUS with the use of the 2 USCAs available in the USA, Optison and Definity. According to the above survey and the number of paediatric urologists having access to VUS it is postulated that there may be indeed some centres using these USCA on an off-label manner for VUS. The survey numbers may include some centres in Canada that are starting to do SonoVue-enhanced VUS. This USCA is approved in Canada and available for intravenous use in adults (personal communications).
Levovist is the only USCA approved for intravesical administration in a number of European countries. With increasing availability of second-generation USCAs the indication for use of Levovist for both intravenous and intravesical administration are diminishing. The manufacturer Bayer-Schering Pharma had already stopped marketing Levovist and apparently there is the intention to stop completely its production in the near future (personal communication, Bayer-Schering Pharma). With this possibility in mind there is a need to gradually switch to using a second-generation USCA like SonoVue. Until the time that such USCAs are approved for VUS the use will be in an off-label manner. Due to the fact that significantly less dose of USCA is required for VUS, SonoVue has a potentially higher safety profile and also becomes relatively cheaper. Moreover, available data show that there is significant increase in reflux detection rate when this USCA is used together with contrast-specific US modality.
Conclusion
Since the last comprehensive reviews of VUS published in 2008 a number of new studies have come out pointing to developments of different aspects of VUS:
-
1.
In different clinical scenarios the diagnosis of VUR is becoming increasingly less important and thus overall imaging for reflux is decreasing.
-
2.
Contrast-specific US techniques, particularly with the use of low MI, are increasingly becoming the modality of choice for VUS.
-
3.
The advantages of the second-generation USCA, SonoVue, for VUS compared to the first-generation USCA, Levovist, are becoming more evident: lower contrast dose, higher safety margin, lower cost, higher sensitivity.
-
4.
The intravesical administration of USCA and paediatric diagnostic US have potentially a much higher safety margin than the intravenous use of the same USCA.
-
5.
Newer comparative studies of VUS and VCUG reaffirm the high diagnostic accuracy of VUS.
-
6.
There is need to standardize the documentation of VUS in order to allow a high diagnostic yield through off-site reading.
-
7.
Contrast-enhanced urethrosonography seems easier to perform with the use of contrast-specific modality, allowing the expansion of the application of VUS.
-
8.
VUS is starting to be used as the primary imaging modality for all cases of reflux and changing the conventional diagnostic and management algorithm of VUR.
-
9.
A recent survey of paediatric urologists in North America has shown that apparently some centres are doing VUS.
-
10.
There is a concerted effort in the US to advance CEUS. A taskforce on CEUS has been established in the AIUM. The newly formed International Contrast Ultrasound Society is expected to support this undertaking.
References
Darge K (2008) Voiding urosonography with ultrasound contrast agents for the diagnosis of vesicoureteric reflux in children. I. Procedure. Pediatr Radiol 38:40–53
Darge K (2008) Voiding urosonography with US contrast agents for the diagnosis of vesicoureteric reflux in children. II. Comparison with radiological examinations. Pediatr Radiol 38:54–63
Demède D, Mouriquand P (2008) Vesicoureteral reflux: why we can’t agree on its management! An evidence based approach. Arch Esp Urol 61:160–166
Marks SD, Gordon I, Tullus K (2008) Imaging in childhood urinary tract infections: time to reduce investigations. Pediatr Nephrol 23:9–17
Lim R (2009) Vesicoureteral reflux and urinary tract infection: evolving practices and current controversies in pediatric imaging. AJR 192:1197–1208
Lee MD, Lin CC, Huang FY et al (2009) Screening young children with a first febrile urinary tract infection for high-grade vesicoureteral reflux with renal ultrasound scanning and technetium-99 m-labeled dimercaptosuccinic acid scanning. J Pediatr 154:797–802
Riccabona M, Avni FE, Blickman JG et al (2008) Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol 38:138–145
McLaren CJ, Simpson ET (2001) Direct comparison of radiology and nuclear medicine cystograms in young infants with vesico-ureteric reflux. BJU Int 87:93–97
Papadopoulou F, Efremidis SC, Oiconomou A et al (2002) Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol 12:666–670
Quaia E (2007) Microbubble ultrasound contrast agents: an update. Eur Radiol 17:1995–2008
Darge K (2002) Diagnosis of vesicoureteral reflux with ultrasonography. Pediatr Nephrol 17:52–60
Quaia E (2007) Contrast-specific ultrasound techniques. Radiol Med 112:473–490
Zimbaro G, Ascenti G, Visalli C (2007) Contrast-enhanced ultrasonography (voiding urosonography) of vesicoureteral reflux: state of the art. Radiol Med 112:1211–1224
Piscitelli A, Galiano R, Serrao F et al (2008) Which cystography in the diagnosis and grading of vesicoureteral reflux? Pediatr Nephrol 23:107–110
Duran C, Valera A, Alguersuari A et al (2009) Voiding urosonography: the study of the urethra is no longer a limitation of the technique. Pediatr Radiol 39:124–131
Papadopoulou F, Anthopoulou A, Siomou E et al (2009) Harmonic voiding urosonography with a second-generation contrast agent for the diagnosis of vesicoureteral reflux. Pediatr Radiol 39:239–244
Kopac M, Riccabona M, Haim M (2009) Contrast-enhanced voiding urosonography and genitography in a baby with ambiguous genitalia and urogenital sinus. Ultraschall Med 30:299–300
Galloy MA, Guillemin F, Couture A et al (2008) Voiding ultrasonography: evaluation of the detection of vesicoureteral reflux based on the review of digital ultrasound clips. Ultraschall Med 29:53–59
Claudon M, Cosgrove D, Albrecht T (2008) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update 2008. Ultraschall Med 29:28–44
Kljucevsek D, Kljucevsek T, Kersnik Levart T et al (2009) Ureteric jet Doppler waveform: is it a reliable predictor of vesicoureteric reflux in children? Pediatr Nephrol 24:313–318
Miller DL, Averkiou MA, Brayman AA et al (2008) Bioeffects considerations for diagnostic ultrasound contrast agents. J Ultrasound Med 27:611–632
Miller DL, Dou C, Wiggins RC et al (2007) An in vivo rat model simulating imaging of human kidney by diagnostic ultrasound with gas-body contrast agent. Ultrasound Med Biol 33:129–135
Miller DL, Dou C, Wiggins RC (2008) Frequency dependence of kidney injury induced by contrast-aided diagnostic ultrasound in rats. Ultrasound Med Biol 34:1678–1687
Darge K, Ghods S, Zieger B et al (2001) Reduction in voiding cystourethrographies after the introduction of contrast enhanced sonographic reflux diagnosis. Pediatr Radiol 31:790–795
Giordano M, Marzolla R, Puteo F (2007) Voiding urosonography as first step in the diagnosis of vesicoureteral reflux in children: a clinical experience. Pediatr Radiol 37:674–677
Wilson SR, Greenbaum LD, Goldberg BB (2009) Contrast-enhanced ultrasound: what is the evidence and what are the obstacles? AJR 193:55–60
Greenbaum L, Burns P, Copel J et al (2007) American Institute of Ultrasound in Medicine recommendations for contrast-enhanced liver ultrasound imaging clinical trials. J Ultrasound Med 26:705–716
Ellison JS, Maxfield CM, Wiener JS (2009) Voiding cystography practices and preferences of North American pediatric urologists. J Urol 182:299–304
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Darge, K. Voiding urosonography with US contrast agent for the diagnosis of vesicoureteric reflux in children: an update. Pediatr Radiol 40, 956–962 (2010). https://doi.org/10.1007/s00247-010-1623-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1623-9