Abstract
Purpose
This study aimed to investigate the interactions between posaconazole (POS) and intravenously/orally administered cyclosporine A (CsA) in allogeneic hematopoietic stem cell transplant (HSCT) recipients.
Methods
We included 118 allogeneic HSCT patients who received CsA and POS simultaneously between January 2017 and June 2020 in this study. The ratio of CsA blood concentration (ng/mL) to dosage (mg/day) (C/D) before and after POS initiation was compared.
Results
After the initiation of POS, the level of CsA increased 1 to 2 times in 66% (78/118) of patients compared to those without POS. However, the CsA C/D ratio increased by more than threefold in 6% (7/118) of patients after POS initiation, with an increase of more than fourfold in two patients. The median C/D ratio of CsA increased from 0.89 to 1.23 (P < 0.001) and 0.78 to 1.22 (P < 0.001) after POS initiation when CsA was administered intravenously and orally, respectively. In patients who received POS at the time of transition from intravenous to oral CsA, the value increased from 1.01 to 1.38 (P = 0.001). The route of administration had no significant effect on the change in the CsA C/D ratio (P = 0.615). Additionally, we observed the time required for the C/D ratio to reach a plateau after POS initiation was similar on days 13, 8, and 15 under various scenarios.
Conclusion
POS treatment increased blood CsA levels. A large variability was found in the fold-change in the CsA C/D ratio. Therefore, CsA doses should be adjusted by closely monitoring the blood levels of CsA after POS initiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematopoietic stem cell transplantation (HSCT) has made great progress in the past half-century as the most effective approach for treating hematological malignancies and some inherited and immune disorders [1]. Graft-versus-host disease (GVHD) is a common complication after HSCT, which seriously affects the prognosis and can even lead to transplantation failure and death [2]. Cyclosporine A (CsA), a potent immunosuppressant, can specifically inhibit T lymphocytes without affecting the function of phagocytes and does not produce obvious bone marrow suppression. It is widely used to prevent and treat GVHD after HSCT [1, 3].
The bioavailability of CsA is only 20–50% owing to its incomplete absorption from the gut [4]. The elimination half-life (t1/2) varies widely from 10 to 30 h. After metabolism in the liver, CsA metabolites are mainly excreted into the bile, with only approximately 6% of the parent drug found in the urine. Food intake, time after transplantation, liver and kidney function, bile secretion, genetic factors, drug dosage forms, and gastrointestinal status may affect the absorption, metabolism, and elimination of CsA, resulting in a large individual variability in the disposition of CsA in vivo [5]. CsA use is usually associated with a high incidence of rejection and side effects. As the substrate of cytochrome P450 (CYP) 3A4/5 and P-glycoprotein (P-gp), CsA can interact with various drugs, including antibiotics, antifungals, and glucocorticoids [6].
Posaconazole (POS) is a second-generation triazole drug with a broad spectrum of applications against yeasts and molds. It has been approved for prophylaxis of fungal infections in allogeneic HSCT and bone marrow transplant recipients [7]. Studies indicate that POS is more effective than other azoles, such as fluconazole and itraconazole, in preventing invasive fungal infections in adult patients with myelodysplastic syndrome and other hematological diseases, thus reducing the mortality related to fungal infections [8]. The POS has unique pharmacokinetic characteristics. It is metabolized by the enzyme uridine diphosphate-glucuronosyltransferase (UGT) [9]. One previous study has suggested that POS is a substrate and inhibitor of P-gp efflux transporters. Orally administered POS may increase the blood concentration of CsA by inhibiting P-gp activity in the small intestine or on the biliary canalicular front of hepatocytes [10]. POS is a potent inhibitor of CYP3A4 expression. It can reduce the metabolism of CsA by inhibiting the activity of hepatic enzymes, resulting in an increase in the serum concentration of CsA, which is prone to cumulative poisoning.
Immunosuppressive agents, such as tacrolimus, sirolimus, and CsA, are frequently used to prevent and treat GVHD in transplant recipients. Drug–drug interactions between azoles and immunosuppressants have received increasing attention in the clinical treatment of transplant recipients. In previous studies, concomitant administration of azoles (e.g., ketoconazole, itraconazole, or voriconazole) with CsA in transplant recipients increased exposure to CsA by 70%–438%, and the dosage of CsA was reduced by 48%–78% [11,12,13,14]. Similar to other azole antifungal agents, POS substantially increases the plasma concentrations of immunosuppressants. A previous study found that co-administering POS with sirolimus can increase the sirolimus blood concentration by approximately nine-fold, resulting in sirolimus toxicity [10]. Kubiak et al. and Greco et al. suggested that an empirical dose reduction of sirolimus was required to maintain therapeutic drug concentrations when using sirolimus and POS concurrently [15, 16]. In addition, a systematic review concluded that when POS is co-administered, the dosage should be reduced by 60–70% for sirolimus/tacrolimus and by 30–40% for CsA following HSCT and solid-organ transplantation [9]. Similar results have been observed by Collin et al. and Peksa et al. [17, 18].
To evaluate the effect of POS on CsA and to guide the rational use of CsA, we retrospectively investigated the concentration of intravenous and oral CsA before and after coadministration with POS in patients who underwent allogeneic HSCT. The study aimed to determine the magnitude of drug interactions between POS and intravenously or orally administered CsA, and the change in trend of CsA concentration when administered via different routes before and after POS initiation.
Methods
Study design and subjects
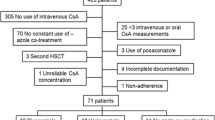
This retrospective study was conducted in a cohort of patients who underwent HSCT at Fujian Medical University Union Hospital between January 2017 and June 2020. Electronic medical records were investigated to identify patients who received a combination of cyclosporine injection (Sandimmune®, Novartis Pharmaceutical Co., Ltd) or cyclosporine soft capsule (Neoral®, Novartis Pharmaceutical Co., Ltd) and POS oral suspension (Noxafil®, Merck Sharp & Dohme Ltd.). Three strategies were used to prevent GVHD after HSCT: CsA combined with mycophenolate mofetil and short-term methotrexate, CsA combined with glucocorticoid, and CsA combined with mycophenolate mofetil and glucocorticoid. The initial dose of CsA was 3 mg/kg/day, administered via an intravenous pump. When the gastrointestinal symptoms and mucosal reactions of the patients were relieved, CsA was administered orally (5 mg/kg/day) twice a day. The CsA dose was adjusted to maintain the trough level (sampling at the end of the dosing interval) between 200 and 400 ng/mL at the initial 2 months after HSCT. The POS oral suspension was administered with meals at a dose of either 400 mg orally twice daily (preemptive treatment) or 200 mg orally three times daily (prophylaxis).
Patients with at least two CsA trough levels, sampled before and after concomitant POS therapy, were enrolled in the study. Exclusion criteria were as follows: (1) blood sample taken at the time of maximum blood concentration (Tmax) of CsA; (2) patients prescribed other drugs that can affect the activity of CYP3A4 enzyme or P-gp efflux transporter, such as erythromycin, clarithromycin, rifampicin, and phenobarbital; and (3) patients with hepatic or renal impairment during the coadministration of CsA and POS.
The study was approved by an independent ethics committee at Fujian Medical University Union Hospital and was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Guidelines for Good Clinical Practice. The requirement for informed consent was waived because only retrospective data were collected.
Data collection
The patients’ medical records were retrieved. Data on the dosage, time, route of administration of CsA, other demographic characteristics, and medical records were collected. Hepatic dysfunction was defined as aspartate transaminase (AST) level > 3 times the upper limit of normal, total bilirubin level > 2 mg/dL, or known hepatic cirrhosis at the start of azole therapy. Renal dysfunction was defined as a serum creatinine level > 2.0 mg/dL or creatinine clearance < 30 mL/min.
Determination of concentration/dose (C/D) ratio of CsA
The trough concentration of CsA was measured before and after POS combination of POS. The dose-normalized trough level (C/D) was calculated according to the following equation:
After the combination of POS and CsA for more than 7 days, if the patient took the same dose of CsA for several consecutive days with the trough level within the therapeutic window, we assumed that the CsA concentration had reached a steady state. In this case, the mean C/D ratio was calculated and defined as the steady-state C/D ratio after the coadministration of POS and CsA. The fold change in the C/D ratio is considered as a surrogate reflecting the effect of POS on CsA concentration.
Statistical method
Data are expressed as mean ± standard deviation (SD) or median (range), depending on the data distribution. Normality was tested using the Shapiro–Wilk test. Statistically significant differences in the C/D ratio before and after initiating POS were assessed using student’s t-test if the data conformed to a normal distribution; otherwise, the Wilcoxon signed-rank test was applied. Similarly, a one-way analysis of variance (ANOVA) test or Kruskal–Wallis test was used for three or more groups. The Chi-squared test was used to analyze categorical data. All analyses were performed using IBM SPSS Statistics, version 26 (IBM, New York, NY, USA). Statistical significance was set at P < 0.05.
Results
Patient demographics
In total, 118 patients were enrolled in this study. The cohort was stratified into Group 1 (N = 50), Group 2 (N = 39), and Group 3 (N = 29) based on the administration route of CsA. CsA was intravenously administered to patients before and after the initiation of POS treatment in Group 1, while oral CsA was administered in Group 3. In Group 2, the patients received POS at the time of transition from intravenous to oral CsA. The characteristics of the study population are summarized in Table 1. There was no significant difference across the three groups in basic demographic data and clinical examination before coadministration with POS (P > 0.05).
Changes in CsA C/D ratio with POS co-therapy
The C/D ratio of CsA increased in 82% (97/118) of patients after the initiation of POS, with 82% (41/50), 82% (32/39), and 83% (24/29) in Groups 1, 2, and 3, respectively. In Group 1, the median C/D ratio of CsA post-POS treatment was 1.23 (ng/mL)/(mg/d) (range: 0.51–3.12), significantly higher than the value of pre-POS treatment [0.89 (ng/mL)/(mg/d), range: 0.30–3.17, P < 0.001]. The median C/D ratio of CsA was 1.01 (ng/mL)/(mg/d) (range: 0.45–2.34, P = 0.001) and 1.38 (ng/mL)/(mg/d) (range: 0.65–2.87) before and after coadministration with POS in Group 2. In Group 3, the median C/D ratio of CsA 1.22 (ng/mL)/(mg/d) (range: 0.64–3.90) with POS is also higher than 0.78 (ng/mL)/(mg/d) (range: 0.35–2.68, P < 0.001) without POS. The change in the C/D ratio of CsA before and after the initiation of POS in the three groups is shown in Fig. 1.
Figure 2 shows the distribution of the fold change in CsA C/D in the three groups. Compared with the C/D ratio of CsA without POS, the level of CsA with POS co-therapy increased 1–2 times in 66% (78/118) of patients, including 64% (32/50) in Group 1, 77% (30/39) in Group 2, and 55% (16/29) in Group 3. The C/D ratio increased more than two-fold in 9 (18%), 2 (5%), and 8 (28%) patients in the three groups, respectively. Notably, the CsA C/D ratio in 6% (7/118) of the patients increased more than threefold after POS initiation, with an increase of more than fourfold in two patients.
The fold change in the CsA C/D ratio was analyzed. Figure 3 shows that there was no significant difference in the C/D ratio alteration of CsA among the three groups (P = 0.615). Compared with the value prior to POS initiation, the median C/D ratio of CsA post-POS co-therapy increased by 1.39 (range: 0.69–3.89) fold in Group 1, 1.43 (range: 0.45–2.32) fold in Group 2, and 1.44 (range: 0.85–4.55) fold in Group 3. The mean magnitude increased in the CsA C/D ratio after POS initiation was found to be approximately 1.5 in all patients. The mean coefficients of fold-change variation were 43.4%, 32.3%, and 55.7% in Groups 1, 2, and 3, respectively.
Changes in CsA C/D ratio overtime after POS initiation
The C/D ratio of CsA was plotted against the number of days after coadministration with POS (Fig. 4). The level of CsA slowly increased and gradually reached a steady state in all three groups when POS was used concomitantly. We observed that the C/D ratio reached a plateau after the initiation of POS at a similar time in all three groups. In Group 1, the C/D ratio reached a steady state around day 13 after POS initiation, with values ranging from 0.43 4.07 (ng/mL)/(mg/d). The LOWESS curve of Group 2 shows that the CsA C/D ratio fluctuated between 0.41 and 3.46 (ng/mL)/(mg/d) after the initiation of POS treatment, and two peaks were observed on Days 8 and 20. When the co-therapy with POS took effect, a zenith around day 15 was observed in Group 3 with a range of 0.48 to 3.90 (ng/mL)/(mg/d) in CsA C/D ratio.
Discussion
To the best of our knowledge, this is the first study to analyze the impact of oral POS on the concentration of oral and/or intravenous CsA simultaneously in the largest number of patients. We observed that, regardless of the administration route of CsA (oral or intravenous), oral POS could significantly influence the blood concentrations of CsA by 0.45 to 4.55-fold in recipients undergoing allogeneic HSCT. Large inter-individual variability was observed in the fold change in the CsA C/D ratio, with the coefficient variation ranging from 32.3% to 55.7%. We also investigated the tendency of CsA levels over time after POS initiation, with the C/D ratio reaching a steady state 8–20 days after the initiation of POS.
Wide inter-individual variability in the magnitude of drug interaction between POS and CsA was observed in our program. Similar to the results of previous studies, the C/D ratio of CsA with POS co-therapy increased by 1 to 2 times in most patients across various subgroups when compared to that without POS. One study assessed four heart transplant recipients on a regular regimen of CsA and found that the AUC0-τ of CsA increased by 1.3-fold at the initiation of POS therapy [14]. In another study conducted in 41 blood and marrow transplant recipients, the authors reported that after 30 days of combined treatment, POS led to a 50% reduction in CsA dose and an approximate doubling of the C/D ratio [7]. Robinson et al. performed a retrospective and prospective study in patients undergoing allogeneic HSCT [19]. They demonstrated a high incidence of cyclosporin-related toxicity when patients received CsA and POS concomitantly. Consistent with Chengcheng Fu, we recommended an initial empirical CsA dose reduction of 30–40% based on our results [9]. Furthermore, a review of drug interactions with azole antifungals came to a similar conclusion that a 30% reduction in the dose of CsA was required upon initiation of POS treatment [20]. The POS prescribing information also suggests that CsA should be reduced by 25% at the initiation of combined treatment with POS [9]. Therefore, our results, together with those of previous studies, demonstrate that POS could increase the concentration of CsA, leading to related toxic reactions. Caution should be exercised when CsA is co-administered with POS.
The administration route of CsA did not significantly affect the change in the CsA C/D ratio in our study. The highest coefficient of variation of fold change after POS co-medication was observed in the group receiving oral CsA. Since CYP3A4 enzymes are present in the small intestine and liver, intestinal and hepatic enzymes are major interaction sites during the oral administration of CsA. In patients following HSCT co-administered voriconazole, Atiq et al. found that the bioavailability of orally administered CsA was nearly 100%, possibly due to the inhibition of CYP3A4 enzymes in the gut wall by voriconazole [5]. Therefore, intestinal CYP3A4 may play an essential role in oral CsA metabolism. Additionally, orally administered POS inhibited P-g activity in the small intestine, increasing the blood concentrations of oral CsA [9, 21]. Combination therapy of patients may also cause the high variability; for example, POS absorption is influenced by gastric acid and gastric motility, while drugs that reduce gastric acid such as proton pump inhibitors can reduce POS absorption and thus affect CsA metabolism [10]. The large inter-individual variability in the oral absorption and first-pass effect of CsA is also one of the reasons for the extensive variation in the C/D ratio in orally administered CsA.
The magnitude of the effect of POS on CsA correlates with the intensity of its inhibition of hepatic drug enzymes. Groll et al. reported that the strength of the inhibitory effect of POS on CYP3A4 is comparable to that of voriconazole, which are strong inhibitors of CYP3A isoenzymes [21]. Valenzuela et al. showed a 23.1% increase in the level of CsA in pediatric patients [12], and Masoumi et al. claimed that the CsA C/D ratio increased significantly by a factor of 1.4 [22], when CsA was concurrently used with voriconazole in HSCT patients. A similar effect was observed for POS in our study, with an approximately 1.5-fold increase in the C/D ratio, which supports the findings of Groll et al. [21, 23]. Fluconazole and isavuconazole are considered moderate CYP3A4 inhibitors. Gu et al. found that fluconazole initiation led to a 25% reduction in the CsA dose to maintain the goal concentration [24], while Groll et al. reported that isavuconazole resulted in a 29% increase in CsA exposure [25]. This is consistent with the moderate inhibition of CYP3A4 enzyme [24, 26].
Because of the long half-lives of azoles, most reach steady-state concentrations after 5–7 days and exhibit their maximal effect on enzyme inhibition. Nara et al. investigated the interactions between itraconazole and orally administered calcineurin inhibitors over seven days [11]. They reported that the dose-adjusted trough concentrations of tacrolimus and CsA significantly increased from day 3 and stabilized on day 5 after itraconazole initiation. In the study by Cho et al. the highest C/D ratio of sirolimus was observed 9–12 days after POS initiation, and a new steady state was reached in approximately 17–20 days [10]. Currently, it has not been clarified how long the interaction reaches a steady state after coadministration with CsA and POS. Our study observed that the time required for the C/D ratio of CsA to reach a plateau after POS initiation was similar under various scenarios. After concomitant administration of POS, the C/D ratio of CsA slowly increased and gradually plateaued at approximately 8–20 days. The influence of POS on CsA levels, in our opinion, is associated with the steady state of POS, which is considered to be eight days based on the half-life of approximately 35 h provided in POS instruction.
Consistent with earlier reports, our findings further confirmed that POS could lead to an increase in the CsA C/D ratio by a factor of 1.5 for the majority of patients. Of note, at the start of POS, 6% (7/118) of patients in our study showed more than a threefold increase in concentration, with two of them showing a fourfold increase. Our results showed a wide variability in the fold increase in the CsA C/D ratio fluctuating between 0.4 and 4.5 fold after POS initiation. One possible reason is the variability in the pharmacokinetics of CsA, which is correlated with various factors, such as food intake, time since transplantation, liver function, bile flow, genetics, gastrointestinal state, and the application of combined drugs, causing inter-individual differences in the interaction between the two drugs.
We acknowledge that because POS levels were not evaluated, we could not assess the relationship between the blood concentration of POS and its drug interaction with CsA. One report demonstrated that the apparent dose responsiveness of CYP3A inhibition with POS appeared to reflect the submaximal inhibition potential of CYP3A4 with lower exposure to POS [21]. In a population pharmacokinetic study, Boonsathorn et al. found that immunosuppressants, including CsA, tacrolimus, sirolimus, and everolimus, did not affect the pharmacokinetics of POS [27]. In addition, the efficacy of azoles is closely related to their plasma concentrations; thus, no adjustment of the POS dose is required when combined with CsA [9, 14, 28]. This was also the case in our study, with a maintenance dose of 200 mg TID or 400 mg BID. In the future, studies on POS pharmacokinetics are required to define drug interactions further.
Despite the larger number of patients in this study, we cannot ignore some limitations. First, data on POS concentrations and genetic polymorphisms of patients were not available because of the retrospective nature of the analysis. Moreover, the association between blood POS and CsA levels could not be analyzed. In particular, oral suspensions of POS have a more complex absorption profile and may cause differential effects. In addition, after the impact of POS on CsA has reached a steady state, CsA concentrations are usually monitored once per week or per two weeks in our institution. Thus, the concentration of oral CsA was much lower after 20 days of coadministration, which may affect the trend of CsA concentration changes. Overall, data on the impact of POS on CsA pharmacokinetics are limited, and further analysis is essential to explore the trends detected in this retrospective program. Moreover, only POS oral suspension was examined in this study, and since the availability of POS tablets have more consistent and better bioavailability than the oral suspension [10, 17], we can also investigate the magnitude of the interaction between POS tablets and CsA in the future.
Conclusions
The coadministration of POS can increase CsA concentration levels, with a great deal of individual variability in the magnitude of change after allogeneic HSCT. Based on the findings of our study, an initial empirical CsA dose reduction between 30 and 40% is recommended. Nevertheless, empirical dose reductions cannot be applied to all patients, and CsA dose adjustment via therapeutic drug concentration monitoring is required.
Data availability
All data included in this study are available from corresponding author upon request.
References
Tafazoli A (2015) Cyclosporine use in hematopoietic stem cell transplantation: Pharmacokinetic approach. Immunotherapy 7:811–836. https://doi.org/10.2217/imt.15.47
Xue L, Zhang WJ, Tian JX, Liu LN, Yan HH, Zhang WW, Ding XL, Zhang JJ, Miao LY (2019) Multicenter-based population pharmacokinetic analysis of ciclosporin in hematopoietic stem cell transplantation patients. Pharm Res 37:15. https://doi.org/10.1007/s11095-019-2740-2
Zhou H, Gao Y, Cheng XL, Li ZD (2012) Population pharmacokinetics of cyclosporine a based on nonmem in chinese allogeneic hematopoietic stem cell transplantation recipients. Eur J Drug Metab Pharmacokinet 37:271–278. https://doi.org/10.1007/s13318-012-0087-8
Chen B, Zhang W, Gu Z, Li J, Zhang Y, Cai W (2011) Population pharmacokinetic study of cyclosporine in chinese renal transplant recipients. Eur J Clin Pharmacol 67:601–612. https://doi.org/10.1007/s00228-010-0959-2
Atiq F, Hameli E, Broers AEC, Doorduijn JK, Van Gelder T, Andrews LM, Koch BCP, Versmissen J, de Winter BCM (2018) Converting cyclosporine a from intravenous to oral administration in hematopoietic stem cell transplant recipients and the role of azole antifungals. Eur J Clin Pharmacol 74:767–773. https://doi.org/10.1007/s00228-018-2434-4
Inoue Y, Saito T, Ogawa K, Nishio Y, Kosugi S, Suzuki Y, Kato M, Sakai H, Takahashi M, Miura I (2014) Pharmacokinetics of cyclosporine a conversion from twice-daily infusion to oral administration in allogeneic hematopoietic stem cell transplantation. Am J Ther 21:377–384. https://doi.org/10.1097/MJT.0b013e318256ed25
Sanchez-Ortega I, Vazquez L, Montes C, Patino B, Arnan M, Bermudez A, Yanez L, Caballero T, Duarte RF (2012) Effect of posaconazole on cyclosporine blood levels and dose adjustment in allogeneic blood and marrow transplant recipients. Antimicrob Agents Chemother 56:6422–6424. https://doi.org/10.1128/AAC.01489-12
Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, Helfgott D, Holowiecki J, Stockelberg D, Goh YT, Petrini M, Hardalo C, Suresh R, Angulo-Gonzalez D (2007) Posaconazole vs. Fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356:348–359. https://doi.org/10.1056/NEJMoa061094
Fu C, Chen J, Xu Y, Wu D (2018) Dose adjustment of immunosuppressants during co-administration of posaconazole: A systematic review. Clin Invest Med 41:E5-e15. https://doi.org/10.25011/cim.v41i1.29458
Cho E, Chan H, Nguyen HM, Shayani S, Nakamura R, Pon D (2015) Management of drug interaction between posaconazole and sirolimus in patients who undergo hematopoietic stem cell transplant. Pharmacotherapy 35:578–585. https://doi.org/10.1002/phar.1600
Nara M, Takahashi N, Miura M, Niioka T, Kagaya H, Fujishima N, Saitoh H, Kameoka Y, Tagawa H, Hirokawa M, Sawada K (2013) Effect of itraconazole on the concentrations of tacrolimus and cyclosporine in the blood of patients receiving allogeneic hematopoietic stem cell transplants. Eur J Clin Pharmacol 69:1321–1329. https://doi.org/10.1007/s00228-013-1471-2
Valenzuela R, Torres JP, Salas C, Gajardo I, Palma J, Catalán P, Santolaya ME, Morales J (2017) drug interaction of voriconazole-cyclosporine in children undergoing hematopoietic stem cell transplantation (2013–2014). Rev Chilena Infectol 34:14–18. https://doi.org/10.4067/s0716-10182017000100002
Vanhove T, Bouwsma H, Hilbrands L, Swen JJ, Spriet I, Annaert P, Vanaudenaerde B, Verleden G, Vos R, Kuypers DRJ (2017) Determinants of the magnitude of interaction between tacrolimus and voriconazole/posaconazole in solid organ recipients. Am J Transplant 17:2372–2380. https://doi.org/10.1111/ajt.14232
Sansone-Parsons A, Krishna G, Martinho M, Kantesaria B, Gelone S, Mant TG (2007) Effect of oral posaconazole on the pharmacokinetics of cyclosporine and tacrolimus. Pharmacotherapy 27:825–834. https://doi.org/10.1592/phco.27.6.825
Kubiak DW, Koo S, Hammond SP, Armand P, Baden LR, Antin JH, Marty FM (2012) Safety of posaconazole and sirolimus coadministration in allogeneic hematopoietic stem cell transplants. Biol Blood Marrow Transplant 18:1462–1465. https://doi.org/10.1016/j.bbmt.2012.04.015
Greco R, Barbanti MC, Lupo Stranghellini MT, Giglio F, Morelli M, Messina C, Forcina A, Oltolini C, Piemontese S, Scarpellini P, Marktel S, Assanelli A, Carrabba M, Vago L, Corti C, Bernardi M, Peccatori J, Ciceri F (2016) Coadministration of posaconazole and sirolimus in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant 51:1022–1024. https://doi.org/10.1038/bmt.2016.112
Collins J, Shea K, Parsad S, Plach K, Lee P (2020) The impact of initiating posaconazole on tacrolimus pharmacokinetics in allogeneic stem cell transplantation. J Oncol Pharm Pract 26:5–12. https://doi.org/10.1177/1078155219833440
Peksa GD, Schultz K, Fung HC (2015) Dosing algorithm for concomitant administration of sirolimus, tacrolimus, and an azole after allogeneic hematopoietic stem cell transplantation. J Oncol Pharm Pract 21:409–415. https://doi.org/10.1177/1078155214539825
Robinson DH, Hughes CFM, Grigg A (2020) Optimal oral cyclosporin dosing with concomitant posaconazole post allogeneic stem cell transplantation. Leuk Lymphoma 61:2448–2452. https://doi.org/10.1080/10428194.2020.1768381
Dodds-Ashley E (2010) Management of drug and food interactions with azole antifungal agents in transplant recipients. Pharmacotherapy 30:842–854. https://doi.org/10.1592/phco.30.8.842
Groll AH, Townsend R, Desai A, Azie N, Jones M, Engelhardt M, Schmitt-Hoffman AH, Bruggemann RJM (2017) Drug-drug interactions between triazole antifungal agents used to treat invasive aspergillosis and immunosuppressants metabolized by cytochrome p450 3a4. Transpl Infect Dis 19:e12751. https://doi.org/10.1111/tid.12751
Masoumi HT, Hadjibabaie M, Vaezi M, Ghavamzadeh A (2017) Evaluation of the interaction of intravenous and oral voriconazole with oral cyclosporine in iranian hsct patients. J Res Pharm Pract 6:77–82. https://doi.org/10.4103/jrpp.JRPP_16_163
Groll AH, Kolve H, Ehlert K, Paulussen M, Vormoor J (2004) Pharmacokinetic interaction between voriconazole and ciclosporin a following allogeneic bone marrow transplantation. J Antimicrob Chemother 53:113–114. https://doi.org/10.1093/jac/dkh022
Gu TM, Lewis JS, 2nd, Le H, Bubalo JS (2021) Comparative effects of fluconazole, posaconazole, and isavuconazole upon tacrolimus and cyclosporine serum concentrations. J Oncol Pharm Pract 1–6. https://doi.org/10.1177/10781552211029046
Groll AH, Desai A, Han D, Howieson C, Kato K, Akhtar S, Kowalski D, Lademacher C, Lewis W, Pearlman H, Mandarino D, Yamazaki T, Townsend R (2017) Pharmacokinetic assessment of drug-drug interactions of isavuconazole with the immunosuppressants cyclosporine, mycophenolic acid, prednisolone, sirolimus, and tacrolimus in healthy adults. Clin Pharmacol Drug Dev 6:76–85. https://doi.org/10.1002/cpdd.284
Townsend R, Dietz A, Hale C, Akhtar S, Kowalski D, Lademacher C, Lasseter K, Pearlman H, Rammelsberg D, Schmitt-Hoffmann A, Yamazaki T, Desai A (2017) Pharmacokinetic evaluation of cyp3a4-mediated drug-drug interactions of isavuconazole with rifampin, ketoconazole, midazolam, and ethinyl estradiol/norethindrone in healthy adults. Clin Pharmacol Drug Dev 6:44–53. https://doi.org/10.1002/cpdd.285
Boonsathorn S, Cheng I, Kloprogge F, Alonso C, Lee C, Doncheva B, Booth J, Chiesa R, Irwin A, Standing JF (2019) Correction to: Clinical pharmacokinetics and dose recommendations for posaconazole in infants and children. Clin Pharmacokinet 58:141. https://doi.org/10.1007/s40262-018-0722-x
Lempers VJ, Martial LC, Schreuder MF, Blijlevens NM, Burger DM, Aarnoutse RE, Bruggemann RJ (2015) Drug-interactions of azole antifungals with selected immunosuppressants in transplant patients: Strategies for optimal management in clinical practice. Curr Opin Pharmacol 24:38–44. https://doi.org/10.1016/j.coph.2015.07.002
Acknowledgements
The authors thank all patients who contributed to this work.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the initial discussion. ZLE, HHP, CYP, WY and XBH designed the study, collected data, analyzed and interpreted data. ZLE wrote the first draft. LMB and WXM supervised the study and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by an independent ethics committee at Fujian Medical University Union Hospital and was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Guidelines for Good Clinical Practice. The requirement for informed consent was waived because only retrospective data were collected.
Consent to participate
Consent to participate is not required.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, LE., Huang, HP., Cai, YP. et al. Effect of posaconazole on the concentration of intravenous and oral cyclosporine in patients undergoing hematopoietic stem cell transplantation. Eur J Clin Pharmacol 78, 1677–1685 (2022). https://doi.org/10.1007/s00228-022-03378-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03378-z