Abstract
Cervical dystonia (CD) is a movement disorder characterized by involuntary muscle contractions leading to an abnormal head posture or movements of the neck. Dysfunctions in somatosensory integration are present and previous data showed enlarged postural sway in stance. Postural control during quiet sitting and the correlation with cervical sensorimotor control were investigated. Postural control during quiet sitting was measured via body sway parameters in 23 patients with CD, regularly receiving botulinum toxin treatment and compared with 36 healthy controls. Amplitude and velocity of displacements of the center of pressure (CoP) were measured by two embedded force plates at 1000 Hz. Three samples of 30 s were recorded with the eyes open and closed. Disease-specific characteristics were obtained in all patients by the Tsui scale, Cervical Dystonia Impact Profile (CDIP-58) and Toronto Western Spasmodic Rating Scale (TWSTRS). Cervical sensorimotor control was assessed with an infrared Vicon system during a head repositioning task. Body sway amplitude and velocity were increased in patients with CD compared to healthy controls. CoP displacements were doubled in patients without head tremor and tripled in patients with a dystonic head tremor. Impairments in cervical sensorimotor control were correlated with larger CoP displacements (rs ranged from 0.608 to 0.748). Postural control is impaired and correlates with dysfunction in cervical sensorimotor control in patients with CD. Treatment is currently focused on the cervical area. Further research towards the potential value of postural control exercises is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult-onset idiopathic cervical dystonia (CD) is a rare movement disorder. It is a focal dystonia which is characterized by involuntary contractions of neck muscles resulting in an abnormal head posture and neck movement. CD is frequently painful and sometimes accompanied by head tremor (Albanese et al. 2011; Jinnah and Albanese 2014). Treatment of choice is injection with Botulinum Toxin (Albanese et al. 2011) and physical therapy can be used as an adjuvant therapy (De Pauw et al. 2014). The cause of CD remains unknown and in addition to motor symptoms CD is associated with non-motor symptoms such as sleep disorders, sensory deficits, deficits in somatosensory integration such as enlarged temporal and spatial discrimination thresholds (Fiorio et al. 2007; Tinazzi et al. 2009; Avanzino et al. 2010; Patel et al. 2014a, b; Antelmi et al. 2016). Deficits of sensorimotor integration have been observed with motor-evoked potentials through transcranial stimulation (Abbruzzese et al. 2001) and are thought to play a role in alleviation maneuvers in which a slight sensory touch alters motor response (Konczak and Abbruzzese 2013; Patel et al. 2014a, b).
In CD, deficits of sensorimotor integration have been observed related to impaired neck proprioception (Bove et al. 2007; De Pauw et al. 2017a). Impairment in neck proprioception may lead to disturbances in balance and posture (Treleaven et al. 2006; Field et al. 2008; Vuillerme and Pinsault 2009) as well as neck pain and dizziness (Revel et al. 1994; Treleaven et al. 2003; Eva-Maj et al. 2013). Postural control and maintaining balance depends on the incorporation of somatosensory, visual and vestibular afferent information. Body sway increases when one or more sensory stimuli are altered (Peterka 2002). Changes in support surface or motion stimuli as well as alterations in cervical proprioceptive information increase postural sway. For instance, neck muscle vibration in particular or cervical muscular fatigue affects postural steadiness (Bove et al. 2007; Vuillerme and Pinsault 2009). Experimentally induced neck muscle fatigue or neck muscle vibration stimulates sensory receptors in the muscle spindles. Given the high density of muscle spindles in suboccipital muscles, neck proprioception plays an important role in maintaining postural control (Pettorossi and Schieppati 2014).
Although half of the patients with CD report difficulties with walking (De Pauw et al. 2017b), postural control in CD is not well-documented. Alterations in gait stability as well as poor balance performance on functional balance tests such as the timed up and go test have been reported (Barr et al. 2017). Regarding postural steadiness, previous posturographic research in quiet stance shows conflicting results. Two studies reported increased postural sway in quiet stance as shown by enlarged antero-posterior and medio-lateral sway, sway path and area (Wöber et al. 1999; Bove et al. 2007) in a population of patients with and without head tremor. Two other studies observed no difference between healthy controls and patients with CD (Lekhel et al. 1997; Moreau et al. 1999) in a population of patients without tremor. Maintaining postural balance in stance predominantly relies on ankle strategy (Gatev et al. 1999). To minimize somatosensory input from the lower limbs, the aim of this exploratory study was to investigate seated postural control. As neck proprioception plays an important role in maintaining postural control (Pettorossi and Schieppati 2014), the secondary aim was to uncover correlations between seated postural control and cervical sensorimotor control. Additionally, to explore whether disease severity influences postural control, correlations were investigated.
Materials and methods
Subject characteristics and clinical assessment
In this cross-sectional study, a group of 23 patients with adult-onset idiopathic CD was compared to a group of 36 healthy controls. Patients were recruited at a tertiary care center in the department of Neurology at the Antwerp University Hospital. All patients were diagnosed by an experienced neurologist in accordance with the European Federation of Neurological Societies/Movement Disorders Society European Section (EFNS/MDS-ES) guidelines (Albanese et al. 2011) and received regular treatments of botulinum toxin injections. The assessment took place at least 3 months after the last injection, immediately prior to a new injection of botulinum toxin. Patients were excluded in case of clinical features suggestive for segmental distribution of dystonia, other neurological disorders, vestibular dysfunction, or previous surgery of the cervical spine and alcohol intake in the last 24 h.
Clinical assessment of the CD symptoms was performed using three disease-specific rating scales: the Cervical Dystonia Impact Profile (CDIP-58) and Toronto Western Spasmodic Rating Scale (TWSTRS) for disease severity and the tremor subscale of the Tsui scale for the assessment of the dystonic head tremor.
The protocol was approved by the Ethics Committee of the Antwerp University Hospital (reference 14/8/74) and all participants provided written informed consent. The assessment was performed in the Multidisciplinary Motor Centre Antwerp (M2OCEAN).
Measurements
Seated postural control was assessed during quiet sitting with two embedded force plates (AMTI®, Advanced Mechanical Technology Inc., Watertown, MA). Center of Pressure (CoP) displacement was measured with a sampling frequency of 1000 Hz and filtered through a 4th order zero-phase Butterworth lowpass filter with a cut-off frequency of 10 Hz (Latash et al. 2003). Participants were seated on a chair without back or arm rests on one force plate. Both feet were placed next to each other with the hands resting on the thighs on the adjacent force plate (see Fig. 1). The force plates generated three force components, F x , F y and F z and three components of the moment of force acting on the force plate M x , M y , M z (x, y and z are the anterior–posterior, medial–lateral and vertical directions, respectively). The signals were processed with Vicon® software (version 1.8.5). A custom-made Matlab model was written to calculate CoP parameters in which total CoP was calculated as the weighted average of the CoP displacements on the two force plates. Following CoP parameters as previously described by Prieto et al. (1996) were calculated: range of the antero-posterior and mediolateral displacements (mm) (range ML, range AP), CoP path as distance covered by the successive positions of the moving CoP (mm), the area (mm2) of an ellipse which encompassed 95% of the CoP distribution and the mean velocity of CoP displacements in the antero-posterior and medio-lateral direction (mm/s) (mVel ML and mVel AP). Three samples of 30 s were recorded with the eyes closed and eyes open (Duarte and Freitas 2010) with a 30 s rest between trials. To increase reliability, the first 10 s of each trial were discarded to avoid fluctuations in CoP and non-stationarity start of the measurement (Carpenter et al. 2001).
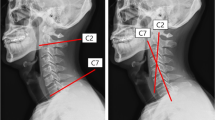
Cervical sensorimotor control was evaluated by joint position error (JPE) in the head repositioning accuracy (HRA) test, which was measured in degrees (°). Measurements were obtained through 3D motion analysis using an infrared camera system with eight cameras recording at 100 Hz (VICON® T10, Oxford Metrics, Oxford). Rigid plates with reflective markers were placed on the head and sternum (see Fig. 2). No alleviating effect was reported of the pressure of the head band in the patient group. In the HRA test, blindfolded participants had to relocate their head as accurately as possible to a self-determined neutral head position (NHP) after performing an active movement (flexion, extension, left and right rotation of the neck) (Revel et al. 1991). The NHP for patients was equal to the dystonic head position. This test is proven to be valid and reliable (Michiels et al. 2013). Participants performed 10 repetitions in every movement direction. The captured data of the Vicon® markers were first reconstructed and labeled using Nexus® software. Afterwards, a custom-made biomechanical model was used to calculate angle positions for each captured frame. Hence, movement angles of the neck were calculated using XYZ Euler/Cardan rotations of the head segment relative to the sternum segment. These data were then processed, using a custom-made MATLAB® code to calculate the JPE (De Pauw et al. 2017a). The absolute JPE, e.g. absolute error (AE), was calculated as the mean difference between the absolute values of the NHP and the position of the head after relocation (Hill et al. 2009). AE = (absolute of raw error trial 1) + (absolute of raw error trial 2) +⋯+ (absolute of raw error trial 10)/10. The AE is a measure for cervical sensorimotor control and larger AE indicates poorer cervical sensorimotor control (Röijezon et al. 2015). Comparison was made between the patient group and a normative database of 70 healthy controls.
Statistical analysis
Data were analyzed using SPSS® vs. 22. Non-parametric statistical tests were used for the posturographic measures for non-normally distributed data. The level of significance was set at p < 0.05 and was adjusted with a post hoc Bonferroni correction given the multiple outcome parameters. As six parameters of postural control were obtained, Bonferroni correction was calculated as 0.05/6 = 0.00833.
As the presence of head tremor could influence cervical sensorimotor control and posturographic measures, the patient group was divided in two groups. Group 1 included patients with CD showing no head tremor, group 2 included patients with CD showing a visible dystonic head tremor. Between group differences between the control group and the two patients groups for postural control were analyzed with a Kruskall–Wallis test with a post hoc analysis by a Mann–Whitney U test. For cervical sensorimotor control, we found no differences between patients with and without head tremor so a Mann–Whitney U test was used to calculate between group differences in cervical sensorimotor control between the control group and the patient group.
Spearman’s rho correlations were calculated in the three groups first between the JPE as a measure for cervical sensorimotor control and postural sway parameters. Second, Spearman’s rho correlations were calculated between clinical measures and postural sway parameters.
Results
Patient characteristics
We included 23 patients with adult-onset idiopathic CD (3 men, 19 females) with a mean disease duration of 13.0 years (± 8.7 SD) and 36 healthy controls (16 men, 20 females). Of the patients with CD, 11 patients showed a visible dystonic head tremor. The mean age of the patient group (59.4 years ± 14.6, mean ± SD) and control group (58.9 years ± 16.6, mean ± SD) did not differ (unpaired t test: p = 0.904). Patient characteristics are shown in Table 1.
Seated postural control
All postural sway parameters were significantly larger in patients with CD compared to controls (p < 0.0001 with Kruskall–Wallis test). In the patient group, postural sway parameters of patients with head tremor were significantly larger compared to patients without head tremor especially in the eyes open condition. Body sway amplitude and velocity were twice as large in patients without head tremor compared to controls in the eyes closed condition (see Table 2 and Fig. 3). In patients with head tremor, CoP displacements were 3–4 times larger compared to displacements in the control group.
No significant differences were observed between the CoP displacements in the condition eyes open and eyes closed in the control group nor the patient groups. (range ML p = 0.263, range AP p = 0.077, path p = 0.884, mVel ML p = 0.408, mVel AP p = 0.685, area p = 0.077).
No correlations were observed between posturographic parameters and disease-specific characteristics such as severity of CD (p = 0.300), head tilt (p = 0.546) nor duration of the disease (p = 0.693) (see Table 3).
Cervical sensorimotor control
The AE was larger in the patient group compared to the control group (Mann-Whitney U test: AE extension: p = 0.015, AE flexion: p = 0.002, AE left rotation: p < 0.0001, AE right rotation: p = 0.0006). For more detailed information, see De Pauw et al. (2017a).
Correlation between cervical sensorimotor control and postural sway
The AE was moderately to strongly correlated with postural sway in the patient group without head tremor. Larger joint repositioning errors, i.e. poorer cervical sensorimotor control, correlated with larger CoP parameters. The AE of flexion correlated with all measurements of CoP parameters in the condition eyes closed. The AE of left rotation was positively correlated with the range of antero-posterior CoP displacements and the mean medio-lateral and antero-posterior velocity of CoP displacements. The mean medio-lateral and antero-posterior velocity of CoP displacements remained significant after a Bonferroni correction given the multiple parameters. These correlations were found in neither the control group nor the patient group with head tremor. In the condition eyes open, the AE correlated with the same CoP parameters, although less strongly.
Discussion
Postural control during quiet sitting in patients with adult-onset idiopathic CD was compared with healthy controls. Secondary, the influence of cervical sensorimotor control and disease characteristics was investigated. The data showed that all CoP parameters were increased in patients with and without head tremor compared to the control group. Patients with a dystonic head tremor showed a larger postural sway and higher sway velocity than patients without a head tremor. In a stable sitting position, the area of the CoP displacement is four times larger in patients without head tremor than in controls. The impaired postural control was strongly correlated with impairments in cervical sensorimotor control, not with disease-specific characteristics. Impairments in cervical sensorimotor control were not different between patients with or without head tremor. We assume patients with head tremor were able to maintain their head still for a short moment when repositioning measurements were obtained.
Previous posturographic reports in quiet stance showed conflicting results. Two studies reported no differences in postural sway in stance between healthy controls and patients with CD (Lekhel et al. 1997; Moreau et al. 1999). Contrary, two studies reported that several parameters of postural sway were enlarged in patients with CD (Wöber et al. 1999; Bove et al. 2007). Sway path, sway area as well as medio-lateral and antero-posterior displacements were enlarged. Differences in patient inclusion might have contributed to these contradictory results. The latter included patients with a dystonic head tremor whereas the first studies excluded patients with head tremor. It is, therefore, not clear whether the enlarged postural sway might be induced by the presence of head tremor. For this reason, the patient group in this study was subdivided based on the presence of head tremor. Our findings show that head tremor is not the sole explanation for impaired postural control as patients without head tremor also showed significantly larger postural sway parameters compared to asymptomatic controls.
This is the first study to investigate postural control in a sitting posture. The increased postural sway suggests higher susceptibility to postural instability. Even in a stable seated condition, the postural sway of both patients with and without dystonic head tremor is enlarged. Different explanations should be considered. First, somatosensory input from the neck is altered in CD. Our data show that patients have impaired cervical sensorimotor control. These findings corroborate previous research in which impairments in somatosensory integration and muscle spindle afference have been observed (Tinazzi et al. 2003; Konczak and Abbruzzese 2013). The strong correlation between postural sway and impaired cervical sensorimotor control leads to the assumption that the altered somatosensory input from the neck might contribute to impaired postural control. We found no difference between the eyes open and eyes closed condition. Therefore, patients do not predominantly rely on visual input for postural control in a seated position. As vestibular function seems to be intact in CD (Rosengren and Colebatch 2010), we assume that impaired cervical sensorimotor control resulted in the larger postural sway. This might seem contradictory to previous research where upright stance is not affected by neck muscle vibration in patients with CD. Patients seemingly ignored the sensory afference from the muscle spindles so that postural sway in stance was not affected by neck muscle vibration (Wöber et al. 1999; Bove et al. 2007). In stance, ankle strategy is predominantly used to maintain postural control (Gatev et al. 1999). In this study, patients sat in a stable position thus limiting the contribution of somatosensory afferent input and balance strategies of the lower limbs. This might imply that in the sensory weighting processes during postural control, the dependence on somatosensory input from the trunk and neck increased (Peterka 2002; Putzki et al. 2006). This might explain the distinct difference found in this study between healthy controls and patients with CD. Second, centrally impaired somatosensory processing might contribute to loss of postural control (Tinazzi et al. 2009). Moreover, CD has been attributed to dysfunction of the basal ganglia and its connections with the cerebellum (Berardelli et al. 1998; Neychev et al. 2011; Quartarone and Hallett 2013; Prudente et al. 2014). As the basal ganglia generate and maintain movement by co-activation of agonist–antagonist muscles to maintain balance (Zahra 2013), impairments in basal ganglia and cerebellum may disturb posture (Takakusaki 2017). We suspect that postural control is inherently affected in CD as there was no correlation observed between the enlarged postural sway and disease severity. Our findings add to the evidence for impaired postural control in CD (Wöber et al. 1999; Bove et al. 2007; Barr et al. 2017).
The presence of dystonic head tremor resulted in larger postural sway amplitude and velocity in patient with a dystonic head tremor compared to patients without head tremor and healthy controls. This might suggest these patients are even more susceptible for balance problems. The larger postural sway might be attributed to alterations in visual input. It is unclear whether gaze stability is impaired in patients with a dystonic head tremor. The vestibulo-ocular reflex (VOR) appears to be intact in patients without head tremor (Rosengren and Colebatch 2010) and suspect that VOR adaptation occurs in long-term dystonic head tremor. Bove and co-workers, however, (Bove et al. 2006) suggested that the inability to focus on one point in patients with essential head tremor might affect postural steadiness. As they observed a larger sway path in patients with essential head tremor compared to patients with essential tremor affecting the arm(s). In this study, however, we did not find a difference in the eyes open and eyes closed condition in patients with head tremor. On the contrary, postural sway tended to decrease in the eyes closed condition. We, therefore, assume that visual dependence is rather low or patients used a stiffening strategy because of the increased difficulty of the task (Field et al. 2008). Second, the enlarged postural sway amplitude and velocity might merely be a reflection of the head tremor. The amplitude and velocity of head movements during the dystonic head tremor might (mechanically) have enlarged the CoP displacements although patients tried to keep the head as still as possible. When patients with CD keep their head still on target, two subtypes of dystonic head tremor have been described by Shaikh et al. (2013). One subtype with a large amplitude and low frequency with a jerky quality caused by slow movement in one direction and a faster corrective movement in the opposite direction. A second subtype showed a small amplitude and high frequency similar to essential tremor. The patients in our sample showed the first subtype: a visible head tremor with a large amplitude. As the corrective phase of the dystonic tremor has a high velocity, part of the higher CoP velocity found in our data might be attributed to the head tremor. Similarly, part of the larger stabilometric parameters (path, area, medio-lateral and antero-posterio range) found in patients with head tremor might be attributed to the tremor and not solely to impaired postural steadiness. Further research might clarify these findings.
The proportion of patients with head tremor in our sample is comparable to other research (van den Dool et al. 2016). The small number of patients in the two subgroups limits the power of the results. Nevertheless, the significantly increased postural sway amplitude and velocity indicate a potential negative impact of CD on postural control.
Gender could be a potential source of bias. Since the prevalence of CD is higher in females with a reported female/male ratio of 2:1 (Steeves et al. 2012; Defazio et al. 2013), a higher percentage of females was included in the patient group compared to the control group. However, no gender differences have been reported for cervical sensorimotor control (Artz et al. 2015; de Vries et al. 2015) and we could not find research reporting gender differences in seated postural control. We, therefore, believe gender did not affect our results.
In conclusion, postural sway is doubled during quiet sitting in patients with CD. Our data add to the yet limited reports on impaired postural control in CD. The alterations in somatosensory input from the neck or somatosensory processing might contribute to a decrease in postural control. Impairments in postural control during sitting might affect everyday life activities, for example the ability to read or working on the computer. Not only the deviated head position but also a decrease in postural steadiness might complicate the task. The findings provide rationale to not limit the physical therapy approach to neck impairments but to explore different modalities such as postural control.
References
Abbruzzese G, Marchese R, Buccolieri a et al (2001) Abnormalities of sensorimotor integration in focal dystonia: a transcranial magnetic stimulation study. Brain 124:537–545
Albanese A, Asmus F, Bhatia KP et al (2011) EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol 18:5–18. https://doi.org/10.1111/j.1468-1331.2010.03042.x
Antelmi E, Erro R, Rocchi L et al (2016) Neurophysiological correlates of abnormal somatosensory temporal discrimination in dystonia. Mov Disord 0:1–8. https://doi.org/10.1002/mds.26804
Artz NJ, Adams MA, Dolan P (2015) Sensorimotor function of the cervical spine in healthy volunteers. Clin Biomech (Bristol Avon) 30:260–268. https://doi.org/10.1016/j.clinbiomech.2015.01.005
Avanzino L, Martino D, Marchese R et al (2010) Quality of sleep in primary focal dystonia: a case–control study. Eur J Neurol 17:576–581. https://doi.org/10.1111/j.1468-1331.2009.02884.x
Barr C, Barnard R, Edwards L et al (2017) Impairments of balance, stepping reactions and gait in people with cervical dystonia. Gait Posture 55:55–61. https://doi.org/10.1016/j.gaitpost.2017.04.004
Berardelli A, Rothwell JC, Hallett M et al (1998) The pathophysiology of primary dystonia. Brain 121:1195–1212
Bove M, Marinelli L, Avanzino L et al (2006) Posturographic analysis of balance control in patients with essential tremor. Mov Disord 21:192–198. https://doi.org/10.1002/mds.20696
Bove M, Brichetto G, Abbruzzese G et al (2007) Postural responses to continuous unilateral neck muscle vibration in standing patients with cervical dystonia. Mov Disord 22:498–503. https://doi.org/10.1002/mds.21357
Carpenter MG, Frank JS, Winter D, Peysar GW (2001) Sampling duration effects on centre of pressure summary measures. Gait Posture 13:35–40
De Pauw J, Van der Velden K, Meirte J et al (2014) The effectiveness of physiotherapy for cervical dystonia: a systematic literature review. J Neurol 1857–1865. https://doi.org/10.1007/s00415-013-7220-8
de Vries J, Ischebeck BK, Voogt LP et al (2015) Joint position sense error in people with neck pain: a systematic review. Man Ther 20:736–744. https://doi.org/10.1016/j.math.2015.04.015
De Pauw J, Mercelis R, Hallemans A et al (2017a) Cervical sensorimotor control in idiopathic cervical dystonia: a cross-sectional study. Brain Behav. https://doi.org/10.1002/brb3.735
De Pauw J, van der Velden K, Cox R et al (2017b) Measuring disability in patients with cervical dystonia according to the international classification of functioning, disability and health. OTJR Occup Particip Heal. https://doi.org/10.1177/1539449217697043
Defazio G, Jankovic J, Giel JL, et al (2013) Descriptive epidemiology of cervical dystonia. Tremor Other Hyperkinet Mov. https://doi.org/10.7916/D80C4TGJ
Duarte M, Freitas SM (2010) Revision of posturography based on force plate for balance evaluation. Rev Bras Fisioter 14:183–192
Eva-Maj M, Hans W, Per-Anders F et al (2013) Experimentally induced deep cervical muscle pain distorts head on trunk orientation. Eur J Appl Physiol 113:2487–2499. https://doi.org/10.1007/s00421-013-2683-y
Field S, Treleaven J, Jull G (2008) Standing balance: a comparison between idiopathic and whiplash-induced neck pain. Man Ther 13:183–191. https://doi.org/10.1016/j.math.2006.12.005
Fiorio M, Gambarin M, Valente EM et al (2007) Defective temporal processing of sensory stimuli in DYT1 mutation carriers: a new endophenotype of dystonia? Brain 130:134–142. https://doi.org/10.1093/brain/awl283
Gatev P, Thomas S, Kepple T, Hallett M (1999) Feedforward ankle strategy of balance during quiet stance in adults. J Physiol 514:915–928. https://doi.org/10.1111/j.1469-7793.1999.915ad.x
Hill R, Jensen P, Baardsen T et al (2009) Head repositioning accuracy to neutral: a comparative study of error calculation. Man Ther 14:110–114. https://doi.org/10.1016/j.math.2008.02.008
Jinnah HA, Albanese A (2014) The new classification system for the dystonias: why was it needed and how was it developed? Mov Disord Clin Pract 1:280–284. https://doi.org/10.1002/mdc3.12100
Konczak J, Abbruzzese G (2013) Focal dystonia in musicians: linking motor symptoms to somatosensory dysfunction. Front Hum Neurosci 7:297. https://doi.org/10.3389/fnhum.2013.00297
Latash ML, Ferreira SS, Wieczorek SA, Duarte M (2003) Movement sway: changes in postural sway during voluntary shifts of the center of pressure. Exp Brain Res 150:314–324. https://doi.org/10.1007/s00221-003-1419-3
Lekhel H, Popov K, Anastasopoulos D et al (1997) Postural responses to vibration of neck muscles in patients with idiopathic torticollis. Brain 120:583–591
Michiels S, De Hertogh W, Truijen S et al (2013) The assessment of cervical sensory motor control: a systematic review focusing on measuring methods and their clinimetric characteristics. Gait Posture 38:1–7. https://doi.org/10.1016/j.gaitpost.2012.10.007
Moreau MS, Cauquil SA, Costes Salon M (1999) Static and dynamic balance function in spasmodic torticollis. Mov Disord 14:87–94
Neychev VK, Gross RE, Lehéricy S et al (2011) The functional neuroanatomy of dystonia. Neurobiol Dis 42:185–201. https://doi.org/10.1016/j.nbd.2011.01.026
Patel N, Jankovic J, Hallett M (2014a) Sensory aspects of movement disorders. Lancet Neurol 13:583–592. https://doi.org/10.1016/S1474-4422(13)70213-8
Patel N, Hanfelt J, Marsh L et al (2014b) Alleviating manoeuvres (sensory tricks) in cervical dystonia. J Neurol Neurosurg Psychiatry 85:882–884. https://doi.org/10.1136/jnnp-2013-307316
Peterka RJ (2002) Sensorimotor integration in human postural control. J Neurophysiol 88:1097–1118. https://doi.org/10.1152/jn.00605.2001
Pettorossi VE, Schieppati M (2014) Neck proprioception shapes body orientation and perception of motion. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2014.00895
Prieto TE, Myklebust JB, Hoffmann RG et al (1996) Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng 43:956–966. https://doi.org/10.1109/10.532130
Prudente CN, Hess EJ, Jinnah HA (2014) Dystonia as a network disorder: what is the role of the cerebellum? Neuroscience 260:23–35. https://doi.org/10.1016/j.neuroscience.2013.11.062
Putzki N, Stude P, Konczak J et al (2006) Kinethesia is impaired in focal dystonia. Mov Disord 21:754–760. https://doi.org/10.1002/mds.20799
Quartarone A, Hallett M (2013) Emerging concepts in the physiological basis of dystonia. Mov Disord 28:958–967. https://doi.org/10.1002/mds.25532
Revel M, Andre-Deshays C, Minguet M (1991) Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil 72:288–291
Revel M, Minguet M, Gregoy P, Vaillant JMJ (1994) Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Arch Phys Med Rehabil 75:895–899
Röijezon U, Clark NC, Treleaven J (2015) Proprioception in musculoskeletal rehabilitation. Part 1: basic science and principles of assessment and clinical interventions. Man Ther 20:368–377. https://doi.org/10.1016/j.math.2015.01.008
Rosengren SM, Colebatch JG (2010) Vestibular evoked myogenic potentials are intact in cervical dystonia. Mov Disord 25:2845–2853. https://doi.org/10.1002/mds.23422
Shaikh AG, Wong AL, Zee DS, Jinnah HA (2013) Keeping your head on target. J Neurosci 33:11281–11295. https://doi.org/10.1523/JNEUROSCI.3415-12.2013
Steeves TD, Day L, Dykeman J et al (2012) The prevalence of primary dystonia: a systematic review and meta-analysis. Mov Disord 27:1789–1796. https://doi.org/10.1002/mds.25244
Takakusaki K (2017) Functional neuroanatomy for posture and gait control. J Mov Disord 10:1–17. https://doi.org/10.14802/jmd.16062
Tinazzi M, Rosso T, Fiaschi A (2003) Role of the somatosensory system in primary dystonia. Mov Disord 18:605–622. https://doi.org/10.1002/mds.10398
Tinazzi M, Fiorio M, Fiaschi A et al (2009) Sensory functions in dystonia: insights from behavioral studies. Mov Disord 24:1427–1436. https://doi.org/10.1002/mds.22490
Treleaven J, Jull G, Sterling M (2003) Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med 35:36–43
Treleaven J, Jull G, LowChoy N (2006) The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Man Ther 11:99–106. https://doi.org/10.1016/j.math.2005.04.003
van den Dool J, Tijssen MAJ, Koelman JHTM et al (2016) Determinants of disability in cervical dystonia. Park Relat Disord 32:48–53. https://doi.org/10.1016/j.parkreldis.2016.08.014
Vuillerme N, Pinsault N (2009) Experimental neck muscle pain impairs standing balance in humans. Exp Brain Res 192:723–729. https://doi.org/10.1007/s00221-008-1639-7
Wöber E, Schnider P, Steinhoff N et al (1999) Posturographic findings in patients with idiopathic cervical dystonia before and after local injections with botulinum toxin. Eur Neurol 41:194–200
Zahra HHM (2013) A model of the basal ganglia in voluntary movement and postural reactions. Comput Methods Biomech Biomech Eng 17:1432–1446. https://doi.org/10.1080/10255842.2012.751983
Acknowledgements
This study is funded by a research grant from the University of Antwerp (Academic project Antwerp University G815). Assessments were performed at and with support from the Multidisciplinary Motor Centre Antwerp (M2OCEAN) that was established by means of a Hercules Grant type 2 for medium sized research infrastructure from the Flemish Research Council (AUHA/09/006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
De Pauw, J., Mercelis, R., Hallemans, A. et al. Postural control and the relation with cervical sensorimotor control in patients with idiopathic adult-onset cervical dystonia. Exp Brain Res 236, 803–811 (2018). https://doi.org/10.1007/s00221-018-5174-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-018-5174-x