Abstract
Rationale
Depression is highly prevalent in diabetes (DM). Brain-derived neurotrophic factor (BDNF) which is mainly regulated by the endoplasmic reticulum chaperon sigma-1 receptor (S1R) plays a relevant role in the development of depression.
Objectives
We studied the dose-dependent efficacy of S1R agonist fluvoxamine (FLU) in the prevention of DM-induced depression and investigated the significance of the S1R-BDNF pathway.
Methods
We used streptozotocin to induce DM in adult male rats that were treated for 2 weeks p.o. with either different doses of FLU (2 or 20 mg/bwkg) or FLU + S1R antagonist NE100 (1 mg/bwkg) or vehicle. Healthy controls were also enrolled. Metabolic, behaviour, and neuroendocrine changes were determined, and S1R and BDNF levels were measured in the different brain regions.
Results
In DM rats, immobility time was increased, adrenal glands were enlarged, and thymuses were involuted. FLU in 20 mg/bwkg, but not in 2 mg/bwkg dosage, ameliorated depression-like behaviour. S1R and BDNF protein levels were decreased in DM, while FLU induced SIR-BDNF production. NE100 suspended all effects of FLU.
Conclusions
We suggest that disturbed S1R-BDNF signaling in the brain plays a relevant role in DM-induced depression. The activation of this cascade serves as an additional target in the prevention of DM-associated depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) and depression are both highly prevalent chronic diseases of the modern era. The International Diabetes Federation predicts that 382 million people suffer from DM worldwide and the number of cases will exceed 592 million in less than 25 years (Federation 2013). Similarly to DM, depression also affects more than 350 million people globally (WHO 2014).
The two diseases often occur together. The prevalence of depression is three times higher in people with type 1 DM (DM1) and two times higher in type 2 diabetic (DM2) patients (Roy and Lloyd 2012). The co-occurrence is associated with elevated risk of DM-induced complications and higher mortality and treatment costs (Park et al. 2013; Shrestha et al. 2013).
Although the causal effect of DM seems to be obvious, the link is rather bi-directional (Chen et al. 2013; Golden et al. 2008). In the pathogenesis of DM and depression, several common pathways have already been identified including immune-inflammatory mediators as well as endocrinological and neurobiological factors. Among them, the role of brain-derived neurotrophic factor (BDNF) has already been highlighted (Korczak et al. 2011).
BDNF belongs to the neurotrophin subfamily and is mainly involved in neurogenesis, neuronal apoptosis, regeneration, and synaptic plasticity (Noble et al. 2011). It also plays a crucial role in the pathophysiology of various neurodegenerative (Durany et al. 2000) and psychiatric disorders including depression (Autry and Monteggia 2012). In the brain of depressive patients, BDNF level is lower and correlates with reduced hippocampus and prefrontal cortex size (Pandey et al. 2008; Thompson Ray et al. 2011). BDNF is decreased not only in the brain but also in the serum of patients with bipolar disorders and depression (Cunha et al. 2006; Palomino et al. 2006). Long-term treatment with various antidepressants could normalize serum BDNF levels (Duman and Monteggia 2006; Sen et al. 2008).
Selective serotonin reuptake inhibitors (SSRIs) are the first choice antidepressive treatment option both in the diabetic and non-diabetic population (Coplan et al. 2014). Besides their antidepressant properties, SSRIs, especially fluvoxamine (FLU), are potent Sigma-1 receptor (S1R) agonists. S1R is an endoplasmic reticulum (ER)-resident chaperon, which is mainly expressed in the central nervous system and to a lesser extent in the peripheral organs. S1R regulates several cellular functions including protein folding, neurotransmitter release, cellular differentiation, and survival (Hayashi and Su 2007; Hayashi et al. 2011). Decreased S1R activity has been observed in the development of depression (Kourrich et al. 2012). SSRIs with S1R agonist properties can modulate hippocampal BDNF levels resulting in an antidepressive effect (Hayashi and Su 2004; Yagasaki et al. 2006).
Although all these data underline the importance of S1R and BDNF in the pathomechanism of depression, this pathway has not been investigated in DM yet. Since SSRIs are the most common antidepressants, we tested the importance of the S1R-BDNF pathway in FLU treated diabetic rats.
Materials and methods
Animals
Six-week-old male Wistar rats weighing 175∼200 g were obtained from Toxi-Coop Ltd (Dunakeszi, Hungary). Rats were housed in plastic cages in groups of three under a 12-h light-dark cycle at room temperature (22 ± 2 °C) with free access to standard rodent diet and tap water. Animal handling and experimental procedures followed the National Institutes of Health guidelines and were approved by the Committee on the Care and Use of Laboratory Animals of the Council on Animal Care at the Semmelweis University of Budapest, Hungary (PEI/001/380-4/2013).
Experimental groups and treatment protocols
DM1 was induced by a single intraperitoneal (i.p.) injection of 65 mg/bwkg streptozotocin (STZ, Sigma Aldrich, Budapest, Hungary) in a freshly prepared 0.1 M citrate buffer (pH 4.5). Rats were considered diabetic if the peripheral blood glucose concentration in three random samples was higher than 15 mmol/L 72 h after the injection of STZ. The age-matched control rats received an equivalent volume of citrate buffer and were used along with diabetic animals.
After 5 weeks, DM1 rats were randomly divided into five groups (n = 6–8/group) and were treated for 2 weeks by oral gavage daily at 10:00 am as follows: group 1—D: D1 rats treated with isotonic saline as vehicle; group 2—FLU20: 20 mg/bwkg fluvoxamine-maleate dissolved in saline (Sigma Aldrich, Budapest, Hungary); group 3—FLU2: 2 mg/bwkg FLU; group 4—FLU20 + NE100: 20 mg/bwkg FLU + 1 mg bwkg−1N,N-dipropyl-2-[4-methoxy-3-(2-phenylethoxy)-phenyl]-ethylamine monohydrochloride (NE100, Tocris Bioscience, Bristol, UK) a specific S1R receptor antagonist; group 5—FLU2 + NE100: 2 mg/bwkg FLU + 1 mg/bwkg NE100.
Age-matched, non-diabetic control rats (C) were treated with saline by oral gavage daily for two 2 weeks at the same time as the diabetic animals.
At the end of the experimental protocol, all rats were anaesthetized with a mixture of 60 mg/bwkg ketamine and 5 mg/bwkg xylazine (rats did not receive drug treatment on this day). Blood samples were taken from the abdominal aorta. The brain and thymus and adrenal glands were collected; the hippocampus and prefrontal area were separated and immediately snap-frozen for further investigation.
Behaviour tests
Treatment protocol is summarized in Suppl. Fig. 1. All behavioural tests were performed after the oral gavage treatment and were conducted in a weakly illuminated room (15 W). Three days before the end of the 7-week experimental period, all animals were tested for locomotor activity by open field test.
Depressive-like behaviour was evaluated by forced swim test (FST); the pre-test was measured 24 h after the open field test, and the test session was conducted 24 h after the pre-test. Rats were sacrificed for tissue collection 24 h after the FST (Online Resource 1).
Open field test
The open field test is a simple sensorimotor test to determine the general and locomotor activity and exploratory behaviour of rodents (Bronikowski et al. 2001). The open field test was performed in a square arena surrounded by a wall (100 × 100 × 60 cm box). The floor was virtually divided into squares (10 × 10 cm). Rats were individually placed into the centre of the field and allowed to explore freely for 10 min. The behaviour was recorded with a Sony DCR-SX21E video camera recorder, and the horizontal locomotory parameter (number of squares crossed) was evaluated manually later by an observer blind to the treatment protocol. The open field box was cleaned between assessments with water.
Forced swim test
FST is the most widely used model for assessing antidepressant-like activity in rats due to its good face and predictive validity (Willner 1984; Slattery and Cryan 2012). This model was described by Porsolt et al. (Porsolt et al. 1978), and it is based on the observation that rodents following initial escape-oriented movements rapidly adopt a characteristic immobile posture in water. Rats were placed in the cylinder (60-cm tall, 14 cm in diameter filled with tap water (24 ± 1 °C) at a height of 30 cm) to ensure that animals could not touch the bottom of the container with their hind paws or their tails. The animals were forced to swim for a 15 min period (pre-test) and 24 h later were subjected to a 5-min test session. After the sessions animals were removed from the water, gently dried with towels, and placed back into their home cages. Water in the tank was changed after each animal. The behaviour of the animals was recorded and later analysed by two observers blind to the treatment protocol using a computer-based time analyser. During the test session, the time spent in mobility (escape-directed behaviour) and immobility was followed and analysed by two independent observers in a blinded fashion.
Measurement of metabolic and neuroendocrine parameters
The development of DM was followed by measurement of serum glucose and fructosamine levels. Additional metabolic serum parameters (triglycerides, total cholesterol, glutamate-oxaloacetate transaminase (GOT) and glutamate-pyruvate transaminase (GPT)) were also evaluated with commercially available kits on a Hitachi 912 photometric chemistry analyser.
Depression is a stress-related disorder and many changes observable in depressive patients resemble a chronic stress state (Duman and Monteggia 2006). In animals, chronic stress is also characterized by lower body weight, adrenal hyperplasia, and thymus involution (Varga et al. 2011). Therefore, we measured these neuroendocrine parameters in the present experiment.
BDNF ELISA
Blood samples of rats were collected in anticoagulant-free tubes. After a centrifugation at 3600 rpm for 6 min centrifugation, serum was separated and BDNF was measured using commercially available sandwich enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis MN, USA) following manufacturer’s directions. Samples were diluted to 1:10 and were loaded in duplicates. The absorbance was measured at 450 nm with wavelength correction at 570 nm using a Plate Chameleon V Fluorometer-Luminometer-Photom reader (Hidex, Turku, Finland). Relative concentration was calculated using the absorbance values of known concentrations of standard BDNF and was expressed as pg/mL.
BDNF and S1R Western blot analysis
Pro and mature BDNF levels were measured in the hippocampus and most affected by depression (Korczak et al. 2011). Brain samples were homogenized in a lysis buffer containing 50 mmol/L HEPES, 150 mmol/L NaCl, 1 % Triton X-100, 5 mmol/L EDTA, 5 mmol/L EGTA, 20 mmol/L sodium pyrophosphate, 20 mmol/L NaF, 0.2 mg/mL phenylmethylsulfonyl fluoride, 0.01 mg/mL leupeptin, and 0.01 mg/mL aprotinin (pH 7.4). Protein concentration was determined in triplicates by a detergent-compatible protein assay with bovine serum albumin (Sigma Aldrich, Budapest, Hungary) as standard. Samples loaded with 40-μg protein/lane were separated on 12 % SDS polyacrylamide gel and transferred to nitrocellulose membranes. All reagents were purchased from Bio-Rad (Budapest, Hungary). Membranes were stained with Ponceau S, then washed and blocked with 2 % BSA (for BDNF measurement) or 5 % non-fat milk (for S1R measurement) in Tris-buffered saline (TBS) and were incubated overnight at 4 °C with primary antibodies: BDNF (1:1000, Santa Cruz Biotechnology, Heidelberg, Germany) and S1R (1:500, Santa Cruz Biotechnology, Heidelberg, Germany). The membranes were washed in TBS buffer containing 0.05 % Tween-20 and incubated with the corresponding horseradish peroxidase conjugated secondary antibodies (1:6000 anti-goat for BDNF and 1:2000 anti-rabbit for S1R, Santa Cruz Biotechnology, Heidelberg, Germany) for 1 h at room temperature. Bound antibodies were visualized by enhanced chemiluminescence detection Western Blotting Detection kit (GE Healthcare Life Sciences, Budapest, Hungary). Positive immunoreactive bands were quantified densitometrically (Versadoc, Quantity One Analysis software; Bio-Rad, Hungary) as integrated optical density (IOD) after subtraction of background. The IOD was factored for Ponceau S staining to correct for any variations in total protein loading. Protein abundance was represented as IOD/Ponceau S compared to controls.
RNA isolation and qRT-PCR
Total RNA was isolated from the hippocampus and prefrontal area by Total RNA Mini Kit (Geneaid Biotech Ltd., New Taipei City, Taiwan). The quality and quantity of isolated RNA were measured on NanoDrop ND-1000 spectrophotometer (BCM, Huston, TX, USA). To generate the first-stranded cDNA, first Strand cDNA Synthesis Kit for RT-qPCR (Thermo Fisher Scientific, Waltham, MA, USA) was used. The messenger RNA (mRNA) expression of S1R, BDNF, and 18S ribosomal RNA (RN18S) was determined by real-time RT-PCR using LightCycler 480 system (Roche Diagnostics, Mannheim, Germany). Primer pairs were designed by Lasergene PrimerSelect software version 7.1.0 (DNASTAR, Madison, WI, USA) based on nucleotide sequences from NCBI’s nucleotide database (Table 1). The reaction mix contained 10 pmol/μL of each PCR primers (IDT, Coralville, Iowa, USA), 10 μL of LightCycler 480 SYBR Green I Master enzyme mix, and 1 μL of cDNA. Results were analysed by LightCycler 480 software version 1.5.0.39 (Roche Diagnostics, Mannheim, Germany). mRNA expression of S1R and BDNF was determined by comparison with RN18S as an internal control from the same samples.
Statistical analysis
All results are expressed as mean ± SEM. Significances were calculated using one-way ANOVA followed by Bonferroni post hoc tests using Graphpad Prism 5.0 software. For non-parametrical data, the Kruskal–Wallis ANOVA on ranks was evaluated. p < 0.05 was considered significant.
Results
Effect of FLU treatment on metabolic parameters
All investigations were performed after 7 weeks of DM. Metabolic parameters are detailed in Table 2. DM was characterized by lower final body weight (C, 331 ± 6.66 vs. D, 266 ± 11.6; F(5, 37) = 4.2, p < 0.01), less total weight gain (F(5, 41) = 5.4, p < 0.001), elevated serum glucose (F(5, 38) = 21,9, p < 0.001), fructosamine (F(5, 35) = 60.8; p < 0.0001), triglycerides (F(5, 41) = 10.7; p < 0.001), and total cholesterol (F(5, 41) = 19.8; p < 0.001) levels. Neither FLU alone nor in combination with NE100 influenced blood glucose and fructosamine. Both FLU doses decreased hyperlipidaemia (serum triglycerides and total cholesterol) in diabetic rats. NE100 did not suppress the effect of FLU suggesting that the antilipidaemic effect is S1R independent. Serum levels of liver enzymes (GOT, GPT) did not change in any of the groups. FLU treatment in control animals did not influence any of the investigated parameters (Online Resource 2).
Neuroendocrine parameters and serum BDNF
In diabetic animals, relative adrenal weight was increased (F(5,37) = 4.5, p < 0.01), while thymus weight (F(5,36) = 11.3, p < 0.001) was decreased compared to controls. Serum BDNF levels were lower in diabetic rats vs. controls (F(5,35) = 13.7, p < 0.0001).
Neither FLU alone nor in combination with NE100 had any effect on organ weights or on serum BDNF levels in diabetic rats vs. controls (Table 3).
FLU ameliorates the depression-like behaviour of diabetic rats
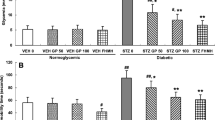
While horizontal locomotor activity was lower in diabetic animals than in controls, neither FLU nor NE100 treatment had any effects confirming that the subsequent behavioural analysis was not distorted by this parameter (Fig. 1).
Effects of fluvoxamine (FLU) on depressive-like behaviour in diabetic rats. Forced swim test and open field test were performed in control and diabetic animals treated for 2 weeks per os with FLU in a dose of 20 mg/bwkg (D + FLU20) or 2 mg/bwkg (D + FLU2) or FLU + 1 mg/bwkg S1R antagonist NE100. Swimming, struggling, and diving represent active parameters, while floating reflects immobility. Each moving pattern of mobility and immobility were calculated in percentage of time. Values are presented as mean ± SEM; n = 6–8/group. * p < 0.05 vs. C; ** p < 0.01 vs. C; *** p < 0.001 vs. C; § p < 0.05 vs. D; # p < 0.05 vs. D + FLU20
Diabetic rats spent more time in immobility/floating (F(5,31) = 10,7; p < 0.001) compared to controls indicating the development of DM-induced depressive-like behaviour. A dose-dependent effect of FLU was observed during the FST. Immobility was decreased in FLU20 rats, while the FLU2 dose was ineffective. Specific S1R antagonist NE100 suspended the beneficial effect of 20 mg/bwkg FLU (Fig. 1).
Protein levels of pro, mature BDNF, and S1R in the hippocampus and prefrontal area
Since FLU2 had no effect on depressive-like behaviour, only the 20 mg/bwkg FLU dose was further used. Protein levels of pro (F hippocampus (3, 28) = 6.88; p < 0.01; F prefrontal area (3, 28) = 7.78; p < 0.001) and mature (F hippocampus (3, 28) = 14; p < 0.001; F prefrontal area (3, 28) = 6; p < 0.01) BDNF and also S1R (F hippocampus (3,32) = 9.69, p < 0.0001; F prefrontal area (3, 28) = 20.9; p < 0.001) were lower in the hippocampus and prefrontal cortex of diabetic rats vs. controls (Fig. 2a-h).
Protein level of pro, mature BDNF, and S1R in the hippocampus and prefrontal area. Top panels (a, b) are representative examples of immunoblots of a 28-kDa precursor BDNF (proBDNF), 14-kDa mature BDNF (mBDNF), and 25-kDa Sigma 1-receptor (S1R) in non-diabetic controls (C) or in diabetic animals (D) or in diabetic rats treated with 20 mg/bwkg fluvoxamine (D + FLU20) and FLU20 + 1 mg/bwkg S1R antagonist NE100 (D + FLU20 + NE100). Lower panels (c–h) show the protein level of proBDNF, mBDNF, and S1R. All data are shown as mean ± SEM; n = 7–8/group. * p < 0.05 vs. C; ** p < 0.01 vs. C; *** p < 0.001 vs. C; § p < 0.05 vs. D; §§ p < 0.01 vs. D; §§§ p < 0.001 vs. D; # p < 0.05 vs. D + FLU20; ### p < 0.01 vs. D + FLU20, ### p < 0.001 vs. D + FLU20. The protein abundance was represented as IOD/Ponceau S vs. controls
FLU treatment increased the level of all proteins (both BDNF forms and S1R), while NE100 suspended the effect of FLU (Fig. 2a-h) in both diabetic brain regions. FLU treatment in control animals did not influence any of the investigated protein levels (Online Resource 3).
RNA expression of BDNF and S1R in the hippocampus and prefrontal area
Total RNA expression of BDNF and S1R did not change in any of the groups in the hippocampus or in the prefrontal area as demonstrated in Fig. 3.
RNA expression of BDNF and S1R in the hippocampus and prefrontal area. Total RNA of BDNF and Sigma 1-receptor (S1R) expression was determined in non-diabetic controls (C) or in diabetic animals (D) or in diabetic rats treated with 20 mg/bwkg fluvoxamine (D + FLU20) and FLU20 + 1 mg/bwkgS1R antagonist NE100 (D + FLU20 + NE100). Total RNA was represented by comparison with RN18S as internal control from the same samples. All data are shown as mean ± SEM; n = 7–8/group. NS non-significant
Discussion
Chronic depression is frequent among diabetic patients and negatively impacts disease progression, mortality, and DM-induced complications (Katon et al. 2008; Zhang et al. 2005). Even so, the pathophysiological connections between DM and depression have not been widely studied yet. Here, we showed that DM induces the development of depression-like neuroendocrine and behavioural changes, and we highlighted the importance of the S1R-BDNF pathway in the comorbidity of these diseases.
Previously, we reported (Zelena et al. 2005; Zelena et al. 2006; Zelena et al. 2007) that untreated DM-induced chronic stress per se resulted in adrenal enlargement and thymus involution in mice. In line with these findings and also with other the literature (Reus et al. 2012), here, we also showed that DM-induced chronic mild stress in rats elicited the development of these neuroendocrine changes. In parallel, here, we demonstrated that depression-like behaviour develops in STZ-diabetic rats as well. It is known that during chronic stress induced by various factors including metabolic changes and/or depression, the hypothalamic–pituitary–adrenal (HPA) axis is activated (Chan et al. 2003). Therefore, we postulate that the increased size of adrenal glands and smaller thymus volume could also be the consequence of hyperglycemia and/or chronic stress-induced hyperactivation of the HPA axis further supporting the putative link between DM and depression.
SSRIs are the routinely recommended treatment for depressed patients even with DM due to their high efficacy and tolerability (Markowitz et al. 2011). It is widely accepted that SSRIs reduce depressive-like behaviour in animal models of depression (Sanchez and Meier 1997). Accordingly, treatment with FLU at the dose of 20 mg/bwkg, but not at the dose of 2 mg/bwkg, ameliorated depression-like behaviour in the present animal model of DM. Dose-dependency and chronic administration of FLU in diabetic animals have not been studied as yet.
To our best knowledge, we are the first who used chronic treatment with FLU to treat DM1-associated depressive-like behaviour. We demonstrated that chronic administration of FLU successfully reduced depressive-like behaviour in a dose-dependent manner. While 2 mg/bwkg FLU had no effect, chronic treatment with a higher dose (20 mg/bwkg) reversed the DM-induced depression-like moving pattern.
Our results also suggest that the antidepressant effect of FLU is not only the result of serotonin reuptake inhibition, but S1R activation also plays a significant role. Among SSRIs, FLU is the most potent S1R agonist (Ki, 36 nM) (Narita et al. 1996). S1R agonists promote S1R dissociation from chaperone binding immunoglobulins, thereby stimulating S1R chaperone activity and resulting in neuroprotection (Hashimoto 2015). S1R and its agonists have been implicated in the pathophysiology of depression through the modulation of various neurotransmitters and structural changes in the brain (Fishback et al. 2010).
The relevance of S1R in diabetes was investigated only in one study showing that S1R expression in the brain decreased after 10 weeks of DM, but the effect of FLU was not measured at all (Mardon et al. 1999). Here, we found that the decreased level of S1R after 7 weeks of DM was raised by FLU. Furthermore, we provide evidence that the antidepressant effect of FLU is highly S1R-dependent, since depressive-like behaviour was not reduced in diabetic animals with the addition of NE100. Our observation confirms the result of a genetic model of depression, where the dose-dependent antidepressant effect of FLU was suspended by another S1R antagonist BD1047 (Sugimoto et al. 2012).
S1R regulates the secretion of BDNF, which is initially synthesized as pre-proBDNF in the ER, then, it is transported to the Golgi. ProBDNF is either directly secreted from cells or cleaved intracellularly by furin. The conversion process to mature BDNF may be completed extracellularly by different metalloproteases (Mizoguchi et al. 2011). Both pro- and mature BDNF are biologically active eliciting opposing effects. ProBDNF is pro-apoptotic, while mature BDNF activates pro-survival signaling. The transformation or the relation of the two forms is poorly discussed; in most studies, only total BDNF level was measured (Etemad et al. 2015). Only in studies investigating aging-associated cognitive function, learning, and neuronal plasticity were the two isoforms of BDNF separately measured (Perovic et al. 2013; Wetsel et al. 2013). Depression-related changes of the distinct forms were determined only in the sera, but not in the brain (Niitsu et al. 2014; Yoshimura et al. 2014).
To our best knowledge, we are the first to show both forms of BDNF in DM-associated depression. We also demonstrated that both in the hippocampus and in the prefrontal cortex FLU increased total and isoform specific BDNF protein levels without changing the mRNA expression, which suggests that the increased protein level of BDNF after FLU treatment is not transcriptionally driven. Our results confirm the findings of Fujimoto et al. showing that cutamesine—another S1R agonist—also potentiates the post-translational processing of BDNF instead of increasing its mRNA transcription (Fujimoto et al. 2012). All these data suggest that S1R agonists have a unique post-translational action on BDNF, and we hypothesize that the lower level of S1R in DM contributes to the decrement of mature BDNF in the brains of diabetic rats. Since mature BDNF activates pro-survival signals, we also postulate that increased secretion of BDNF via enhanced S1R chaperon activity induced by FLU may prevent neuronal cell death in DM.
One should note the possible disadvantages of chronic SSRI treatment. Drug-induced liver injury is one of the most frequently reported adverse effects of SSRIs. In the present study, serum liver enzymes were unaltered supporting the clinical observation that FLU is the least hepatotoxic among SSRIs (Voican et al. 2014).
Antidepressants are also assumed to significantly alter glucose homeostasis. However, there are only two studies saying that FLU induces hyperglycemia; a transient increase in blood glucose level was documented after acute FLU treatment in non-diabetic mice (Yamada et al. 1999). The other study is a case report of a DM2 woman with depression, where FLU elevated the random blood glucose level (Oswald et al. 2003). The effect of FLU in DM1 has not been studied at all. In our study, blood glucose levels tended to be lower in FLU-treated rats than in the untreated ones at the end of the experiments; however, this decrement was not significant. Furthermore, chronic FLU administration did not influence serum fructosamine values suggesting that FLU does not alter glucose homeostasis significantly on the long run.
Abnormalities of lipoprotein metabolism contribute to the development of atherosclerosis and are independent risk factors of cardiovascular mortality in diabetic patients (Reddy et al. 2015). The effect of FLU on serum lipid panel has been poorly investigated. There are only a few studies showing that FLU reduces cholesterol levels and has beneficial effects on the lipid panel (de Zwaan and Nutzinger 1996; Tse et al. 2014). Here, we confirm that FLU decreases DM-induced hyperlipidaemia, which seems to be independent of the S1R pathway.
In conclusion, we are the first to investigate the different forms of BDNF in the type 1 diabetic rat brain. We suggest that the S1R-BDNF pathway is also a possible contributing factor of DM-associated depression which can be effectively influenced by FLU. Altogether, FLU is a promising and safe treatment option; however, population-based larger studies are needed to prove the clinical benefits of S1R agonists in patients suffering from DM-associated depression.
References
Autry AE, Monteggia LM (2012) Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev 64:238–258
Bronikowski AM, Carter PA, Swallow JG, Girard IA, Rhodes JS, Garland T (2001) Open-field behavior of house mice selectively bred for high voluntary wheel-running. Behav Genet 31:309–316
Chan O, Inouye K, Riddell MC, Vranic M, Matthews SG (2003) Diabetes and the hypothalamo-pituitary-adrenal (HPA) axis. Minerva Endocrinol 28:87–102
Chen PC, Chan YT, Chen HF, Ko MC, Li CY (2013) Population-based cohort analyses of the bidirectional relationship between type 2 diabetes and depression. Diabetes Care 36:376–382
Coplan JD, Gopinath S, Abdallah CG, Berry BR (2014) A neurobiological hypothesis of treatment-resistant depression - mechanisms for selective serotonin reuptake inhibitor non-efficacy. Front Behav Neurosci 8:189
Cunha AB, Frey BN, Andreazza AC, Goi JD, Rosa AR, Goncalves CA, Santin A, Kapczinski F (2006) Serum brain-derived neurotrophic factor is decreased in bipolar disorder during depressive and manic episodes. Neurosci Lett 398:215–219
de Zwaan M, Nutzinger DO (1996) Effect of fluvoxamine on total serum cholesterol levels during weight reduction. J Clin Psychiatry 57:346–348
Duman RS, Monteggia LM (2006) A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59:1116–1127
Durany N, Michel T, Kurt J, Cruz-Sanchez FF, Cervas-Navarro J, Riederer P (2000) Brain-derived neurotrophic factor and neurotrophin-3 levels in Alzheimer’s disease brains. Int J Dev Neurosci 18:807–813
Etemad A, Sheikhzadeh F, Asl NA (2015) Evaluation of brain-derived neurotrophic factor in diabetic rats. Neurol Res 37:217–222
Federation ID (2013) International Diabetes Federation. IDF diabetes atlas, 6th edn. Brussels, Belgium: International Diabetes Federation, 2013.
Fishback JA, Robson MJ, Xu YT, Matsumoto RR (2010) Sigma receptors: potential targets for a new class of antidepressant drug. Pharmacol Ther 127:271–282
Fujimoto M, Hayashi T, Urfer R, Mita S, Su TP (2012) Sigma-1 receptor chaperones regulate the secretion of brain-derived neurotrophic factor. Synapse 66:630–639
Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, Lee HB, Lyketsos C (2008) Examining a bidirectional association between depressive symptoms and diabetes. JAMA 299:2751–2759
Hashimoto K (2015) Activation of sigma-1 receptor chaperone in the treatment of neuropsychiatric diseases and its clinical implication. J Pharmacol Sci 127:6–9
Hayashi T, Su TP (2004) Sigma-1 receptor ligands: potential in the treatment of neuropsychiatric disorders. CNS drugs 18:269–284
Hayashi T, Su TP (2007) Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca(2+) signaling and cell survival. Cell 131:596–610
Hayashi T, Tsai SY, Mori T, Fujimoto M, Su TP (2011) Targeting ligand-operated chaperone sigma-1 receptors in the treatment of neuropsychiatric disorders. Expert Opin Ther Targets 15:557–577
Katon W, Fan MY, Unutzer J, Taylor J, Pincus H, Schoenbaum M (2008) Depression and diabetes: a potentially lethal combination. J Gen Intern Med 23:1571–1575
Korczak DJ, Pereira S, Koulajian K, Matejcek A, Giacca A (2011) Type 1 diabetes mellitus and major depressive disorder: evidence for a biological link. Diabetologia 54:2483–2493
Kourrich S, Su TP, Fujimoto M, Bonci A (2012) The sigma-1 receptor: roles in neuronal plasticity and disease. Trends Neurosci 35:762–771
Mardon K, Kassiou M, Donald A (1999) Effects of streptozotocin-induced diabetes on neuronal sigma receptors in the rat brain. Life Sci 65:PL 281–PL 286
Markowitz SM, Gonzalez JS, Wilkinson JL, Safren SA (2011) A review of treating depression in diabetes: emerging findings. Psychosomatics 52:1–18
Mizoguchi H, Nakade J, Tachibana M, Ibi D, Someya E, Koike H, Kamei H, Nabeshima T, Itohara S, Takuma K, Sawada M, Sato J, Yamada K (2011) Matrix metalloproteinase-9 contributes to kindled seizure development in pentylenetetrazole-treated mice by converting pro-BDNF to mature BDNF in the hippocampus. J Neurosci 31:12963–12971
Narita N, Hashimoto K, Tomitaka S, Minabe Y (1996) Interactions of selective serotonin reuptake inhibitors with subtypes of sigma receptors in rat brain. Eur J Pharmacol 307:117–119
Niitsu T, Ishima T, Yoshida T, Hashimoto T, Matsuzawa D, Shirayama Y, Nakazato M, Shimizu E, Hashimoto K, Iyo M (2014) A positive correlation between serum levels of mature brain-derived neurotrophic factor and negative symptoms in schizophrenia. Psychiatry Res 215:268–273
Noble EE, Billington CJ, Kotz CM, Wang C (2011) The lighter side of BDNF. Am J Physiol Regul Integr Comp Physiol 300:R1053–R1069
Oswald P, Souery D, Mendlewicz J (2003) Fluvoxamine-induced hyperglycaemia in a diabetic patient with comorbid depression. Int J Neuropsychopharmacol 6:85–87
Palomino A, Vallejo-Illarramendi A, Gonzalez-Pinto A, Aldama A, Gonzalez-Gomez C, Mosquera F, Gonzalez-Garcia G, Matute C (2006) Decreased levels of plasma BDNF in first-episode schizophrenia and bipolar disorder patients. Schizophr Res 86:321–322
Pandey GN, Ren X, Rizavi HS, Conley RR, Roberts RC, Dwivedi Y (2008) Brain-derived neurotrophic factor and tyrosine kinase B receptor signalling in post-mortem brain of teenage suicide victims. Int J Neuropsychopharmacol 11:1047–1061
Park M, Katon WJ, Wolf FM (2013) Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review. Gen Hosp Psychiatry 35:217–225
Perovic M, Tesic V, Mladenovic Djordjevic A, Smiljanic K, Loncarevic-Vasiljkovic N, Ruzdijic S, Kanazir S (2013) BDNF transcripts, proBDNF and proNGF, in the cortex and hippocampus throughout the life span of the rat. Age 35:2057–2070
Porsolt RD, Anton G, Blavet N, Jalfre M (1978) Behavioural despair in rats: a new model sensitive to antidepressant treatments. Eur J Pharmacol 47:379–391
Reddy VS, Bui QT, Jacobs JR, Begelman SM, Miller DP, French WJ, Investigators of National Registry of Myocardial Infarction b (2015) Relationship between serum low-density lipoprotein cholesterol and in-hospital mortality following acute myocardial infarction (the lipid paradox). Am J Cardiol 115:557–562
Reus GZ, Abelaira HM, Stringari RB, Fries GR, Kapczinski F, Quevedo J (2012) Memantine treatment reverses anhedonia, normalizes corticosterone levels and increases BDNF levels in the prefrontal cortex induced by chronic mild stress in rats. Metab Brain Dis 27:175–182
Roy T, Lloyd CE (2012) Epidemiology of depression and diabetes: a systematic review. J Affect Disord 142(Suppl):S8–S21
Sanchez C, Meier E (1997) Behavioral profiles of SSRIs in animal models of depression, anxiety and aggression. Are they all alike? Psychopharmacology 129:197–205
Sen S, Duman R, Sanacora G (2008) Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biol Psychiatry 64:527–532
Shrestha SS, Zhang P, Li R, Thompson TJ, Chapman DP, Barker L (2013) Medical expenditures associated with major depressive disorder among privately insured working-age adults with diagnosed diabetes in the United States, 2008. Diabetes Res Clin Pract 100:102–110
Slattery DA, Cryan JF (2012) Using the rat forced swim test to assess antidepressant-like activity in rodents. Nat Protoc 7:1009–1014
Sugimoto Y, Tagawa N, Kobayashi Y, Mitsui-Saito K, Hotta Y, Yamada J (2012) Involvement of the sigma1 receptor in the antidepressant-like effects of fluvoxamine in the forced swimming test in comparison with the effects elicited by paroxetine. Eur J Pharmacol 696:96–100
Thompson Ray M, Weickert CS, Wyatt E, Webster MJ (2011) Decreased BDNF, trkB-TK+ and GAD67 mRNA expression in the hippocampus of individuals with schizophrenia and mood disorders. J Psychiatry Neurosci : JPN 36:195–203
Tse L, Procyshyn RM, Fredrikson DH, Boyda HN, Honer WG, Barr AM (2014) Pharmacological treatment of antipsychotic-induced dyslipidemia and hypertension. Int Clin Psychopharmacol 29:125–137
Varga J, Domokos A, Barna I, Jankord R, Bagdy G, Zelena D (2011) Lack of vasopressin does not prevent the behavioural and endocrine changes induced by chronic unpredictable stress. Brain Res Bull 84:45–52
Voican CS, Corruble E, Naveau S, Perlemuter G (2014) Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry 171:404–415
Wetsel WC, Rodriguiz RM, Guillemot J, Rousselet E, Essalmani R, Kim IH, Bryant JC, Marcinkiewicz J, Desjardins R, Day R, Constam DB, Prat A, Seidah NG (2013) Disruption of the expression of the proprotein convertase PC7 reduces BDNF production and affects learning and memory in mice. Proc Natl Acad Sci U S A 110:17362–17367
Willner P (1984) The validity of animal models of depression. Psychopharmacology 83:1–16
World Health Organization, pp Facts sheet No 369 - Depression. Accessed on the 18th of May 2014, Available from: http://www.who.int/mediacentre/factsheets/fs369/en/.
Yagasaki Y, Numakawa T, Kumamaru E, Hayashi T, Su TP, Kunugi H (2006) Chronic antidepressants potentiate via sigma-1 receptors the brain-derived neurotrophic factor-induced signaling for glutamate release. J Biol Chem 281:12941–12949
Yamada J, Sugimoto Y, Inoue K (1999) Selective serotonin reuptake inhibitors fluoxetine and fluvoxamine induce hyperglycemia by different mechanisms. Eur J Pharmacol 382:211–215
Yoshimura R, Kishi T, Hori H, Atake K, Katsuki A, Nakano-Umene W, Ikenouchi-Sugita A, Iwata N, Nakamura J (2014) Serum proBDNF/BDNF and response to fluvoxamine in drug-naive first-episode major depressive disorder patients. Ann Gen Psychiatry 13:19
Zelena D, Barna I, Mlynarik M, Gupta OP, Jezova D, Makara GB (2005) Stress symptoms induced by repeated morphine withdrawal in comparison to other chronic stress models in mice. Neuroendocrinology 81:205–215
Zelena D, Filaretova L, Mergl Z, Barna I, Tóth ZE, Makara GB (2006) Hypothalamic paraventricular nucleus, but not vasopressin, participates in chronic hyperactivity of the HPA axis in diabetic rats. Am J Physiol Endocrinol Metab 290:E243–E250
Zelena D, Domokos A, Barna I, Csabail K, Bagdy G, Makara GB (2007) The role of vasopressin in chronic stress studied in a chronic mild stress model of depression. Ideggyogy Sz 60:196–200
Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles G, Kahn HS (2005) Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol 161:652–660
Acknowledgments
This study was funded by grants of OTKA K112629-K116928-K108688-PD105361-NN114607. It was also supported by MTA-SE “Lendület” Research Grant (LP-008/2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Lenart, L., Hodrea, J., Hosszu, A. et al. The role of sigma-1 receptor and brain-derived neurotrophic factor in the development of diabetes and comorbid depression in streptozotocin-induced diabetic rats. Psychopharmacology 233, 1269–1278 (2016). https://doi.org/10.1007/s00213-016-4209-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-016-4209-x