Abstract
Diabetes mellitus and depression are comorbid diseases affecting many patients all over the world. The current study was designed to compare the antidepressant effect of some antidiabetic drugs such as vildagliptin, pioglitazone, glyburide, and metformin on depression-related or unrelated to type 2 diabetes mellitus (T2DM). T2DM was induced by high-fat diet and streptozotocin, while diabetes-unrelated depression was induced by reserpine. Antidiabetic agents reduced diabetes-associated depression as indicated by the reduction in the immobility time in the forced swim test, elevation of cortical and hippocampal serotonin and brain-derived neurotrophic factor (BDNF), and the increase in serum β-Amyloid 1–42 (Aβ1–42) levels. Antidiabetic agents also reduced serum corticosterone levels suggesting their inhibitory effect on hypothalamus-pituitary-adrenal axis activity. The antidepressant activity of the tested compounds was associated with reduction of oxidative stress and inflammation in brain. Vildagliptin showed the highest, while glyburide showed the least antidiabetic and antidepressant activity. Antidepressant activities of pioglitazone and metformin were comparable. The difference in antioxidant and anti-inflammatory activities between groups showed the same pattern of the antidepressant effect suggesting that these two pathways may play role in ameliorating depression in diabetic rats. On the other hand, the administration of reserpine in small doses (0.2 mg/kg) induced depression associated with hyperglycemia in non-diabetic rats. Although all treatments improved glycemic parameters to similar levels, vildagliptin showed the greatest effect on Aβ1–42, serotonin, norepinephrine, and BDNF levels. In conclusion, vildagliptin seems to be the leading drug among the tested antidiabetics and may be the most appropriate antidiabetic for managing diabetes-associated depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global prevalence of diabetes mellitus (DM) has been increasing over the last two decades (Sarwar et al. 2010). Long-term diabetes is associated with microvascular and macrovascular complications, as well as psychological complications. Previous studies demonstrated that patients with diabetes have higher incidence of depression than the general population (Ali et al. 2006). Diabetic patients who are depressed have increased rates of mortality, hospitalizations, diabetic complications, and a decreased quality of life compared with non-depressed diabetic patients (Markowitz et al. 2011).
One of the mechanisms that link diabetes to depression is hyperglycemia. The later results in excessive generation of reactive oxygen species (ROS), which activate nuclear factor-kappa B (NF-κB) (Flohé et al. 1997), a transcription factor for different inflammatory mediators. It has been proposed that the proinflammatory cytokines are implicated in the pathogenesis of depression by various mechanisms including the activation of the hypothalamic–pituitary–adrenal (HPA) axis, the increase of oxidative stress in the brain, and the reduction of serotonin production (Hoyo-Becerra et al. 2014). Inflammation may also induce depression via the reduction of brain-derived neurotrophic factor (BDNF), an essential mediator in the neurogenesis, differentiation, and survival of neurons, which are involved in the pathophysiology of depressive disorder (Hritcu and Gorgan 2014). The “neurotrophic theory” hypothesizes that depression is associated with reduced BDNF levels in the brain and that the treatment with antidepressants alleviates depressive behavior and elevates BDNF levels. In addition, increased level of glucocorticoids, due to HPA axis dysfunction in diabetic patients, can reduce BDNF expression in the hippocampus and prefrontal cortex and lead to a depressive state (Autry and Monteggia 2012). Hyperactivity of HPA axis may also provoke a change in β-amyloid peptide 1–42 (Aβ1–42) metabolism, which is associated with the pathophysiology of early-onset depression (Ishijima et al. 2018).
Selective serotonin reuptake inhibitors (SSRIs) are the first-line antidepressants based on their safety profile and efficacy (MacGillivray et al. 2003). Some members such as fluoxetine were found to improve glycemic control besides its antidepressant effect (Goodnick 2001). However, SSRIs are not devoid of side effects such as sexual dysfunction (Gelenberg et al. 2000), withdrawal symptoms upon abrupt discontinuation (Coupland et al. 1996), and increased risk of suicide (Fergusson et al. 2005). Some antidiabetic drugs have been demonstrated to exert antidepressant effects such as metformin (Guo et al. 2014) and pioglitazone (Colle et al. 2017). Nonetheless, the use of antidiabetic drugs as substitutes for conventional antidepressants in treating diabetes-associated depression is ambiguous and needs to be further tackled.
Taken together, the present study was performed to evaluate and compare the antidepressant activity of different antidiabetic drugs against depression escorting diabetes induced by high-fat diet/streptozotocin (STZ) and against reserpine-induced depression in non-diabetic rats.
Materials and methods
Experimental animals
In the present study, adult male Wistar rats (100–115 g) were used. Animals were purchased from the Egyptian Organization for Biological Products and Vaccines (Cairo, Egypt). Rats were acclimatized for 1 week prior to experiments. The animals were kept at controlled temperature (23 ± 2 °C), humidity (60 ± 10%), light/dark cycle (12/12 h), and allowed free access to food and water. All procedures were conducted in accordance with the accepted principles for care and use of laboratory animals and were approved by the animal ethics committee of Faculty of Pharmacy, Zagazig University, Egypt (Approval number: P1-12-2017).
Drugs and chemicals
STZ, metformin hydrochloride, pioglitazone hydrochloride, and glyburide were purchased from Sigma-Aldrich (St. Louis, MO, USA). Vildagliptin was purchased from Novartis (Pharma AG, Basil, Switzerland), and reserpine was purchased from Cayman Chemical (Ann Arbor, MI, USA). On the other hand, fluoxetine hydrochloride was provided as a gift from EIPICO (10th of Ramadan City, Egypt). All drugs were suspended in 10% dimethyl sulfoxide (DMSO) + 10% Tween 80 + 80% distilled water as a vehicle.
Experimental design
Part 1
This part was intended to identify the link between T2DM and the development of depression, as well as evaluating the effect of the studied antidiabetic agents in alleviating diabetes-associated depression. T2DM was induced by feeding rats a high-fat diet (HFD) composed of 25% fat, 48% carbohydrates, and 20% protein for 9 weeks, plus a single intraperitoneal injection of STZ (35 mg/kg) at the beginning of week 5. After 72 h of STZ injection, fasting blood glucose levels of all rats were above 200 mg/dL indicating the induction of diabetes (Wang et al. 2013).
Rats were divided into seven groups (n = 6 each). Group 1 (control, CT): normal rats fed standard chow diet and received the vehicle once daily for 4 weeks starting from week 6, group 2 (reserpine, R): normal rats fed standard chow diet and received reserpine (8 mg/kg, IP) once at the end of week 9 serving as positive control group for depression (Huang et al. 2004), group 3 (DM): diabetic rats, group 4 (vildagliptin, V): diabetic rats that received vildagliptin (10 mg/kg, PO) (Refaat et al. 2016), group 5 (pioglitazone, P): diabetic rats that received pioglitazone (10 mg/kg, PO) (Refaat et al. 2016), group 6 (glyburide, G): diabetic rats that received glyburide (5 mg/kg, PO) (Nazaroglu et al. 2009), and group 7 (metformin, M): diabetic rats that received metformin (100 mg/kg, PO) (Arafa et al. 2016). Drugs in groups 4–7 were administered daily starting from week 6 and continued for 4 weeks till the end of the experimental period.
Part 2
This part was intended to evaluate the antidepressant effect of the studied antidiabetic agents in non-diabetic rats. Rats were divided into seven groups (n = 8, each). Group 1 (control, CT): normal rats fed standard chow diet and received the vehicle once daily starting from week 1, group 2 (reserpine, R): chronic depression group in which normal rats received reserpine (0.2 mg/kg, IP) once daily for 14 days (Antkiewicz-Michaluk et al. 2014) followed by an IP injection every 48 h to maintain depression till the end of the experiment (Shyong et al. 2017), group 3 (vildagliptin, V): rats treated as group 2 and received vildagliptin (10 mg/kg, PO), group 4 (pioglitazone, P): rats treated as group 2 and received pioglitazone (10 mg/kg, PO), group 5 (glyburide, G): rats treated as group 2 and received glyburide (5 mg/kg, PO), group 6 (metformin, M): rats treated as group 2 and received metformin (100 mg/kg, PO), and group 7 (fluoxetine, F): rats treated as group 2 and received fluoxetine (20 mg/kg, PO) (Dong et al. 2017). Drug administration in groups 3–7 started from week 3 and continued daily for 4 weeks till the end of the experimental period.
Forced swim test
Forced swim test (FST) was performed according to the original protocol described by Porsolt et al. (1977). Briefly, a pretest session was carried out 24 h prior to the test, where animals were individually placed for 15 min for conditioning in a glass cylinder (45 cm × 35 cm × 60 cm) filled with water to 30 cm and its temperature was adjusted at 24 ± 0.5 °C. Test session was performed 1 day later for 6 min, where the immobility time was recorded (hind legs were no longer moving, and the rat was hunched forward). The last 4 min of the test period was only analyzed because most animals are very active at the beginning of the test, which may obscure the potential effects of the treatment. Manual calculation of the immobility time was carried out by a blind investigator.
Blood and tissue sampling
At the end of experiments, blood was drawn from the retro-orbital sinus of rats using heparinized microcapillary tubes and centrifuged for separation of serum, which was then stored at − 80 °C. Rats were euthanized by cervical dislocation and brain was dissected. One half of the brain was immediately fixed in 10% formalin for histopathology, and the other half was snap-frozen in liquid nitrogen and stored at − 80 °C.
Tissue preparation for neurotransmitter level measurements
The prefrontal cortex (PFC) and the hippocampus were carefully excised as described by Spijker (2011). Brain tissue homogenate was prepared by mixing 1 g of brain tissue in 1 mL phosphate-buffered saline (PBS), which was then homogenized (Con-Torque Tissue Homogenizer, Eberbach Corp., Belleville, MI, USA). The homogenate was centrifuged (10,000 rpm at 5 °C) for 10 min, and the supernatant was separated for the biochemical analyses.
Measurement of glycemic parameters
Fasting serum glucose level was measured colorimetrically using a commercial kit supplied by the Egyptian Company for Biotechnology (Cairo, Egypt). Fasting serum insulin level was measured by sandwich enzyme-linked immunosorbent assay (ELISA) using a rat insulin kit supplied by CUSABIO (Hubei, China). Insulin resistance was calculated using the homeostatic model assessment of insulin resistance (HOMA-IR) as described by Matthews et al. (1985) using the following equation: HOMA-IR = fasting glucose (mg/dL) × fasting insulin (μIU/mL)/405.
Measurement of brain serotonin, norepinephrine, and BDNF levels and serum corticosterone and Aβ 1–42 levels
Brain serotonin, norepinephrine, and BDNF, as well as serum corticosterone and Aβ1–42 levels were measured by ELISA technique using kits supplied by MyBioSource (San Diego, CA, USA), Eagle Biosciences (Amherst, NH, USA), Boster Biological Technology (Pleasanton, CA, USA), Elabscience (Houston, Texas, USA), and Lifespan Biosciences (Seattle, WA, USA), respectively.
Measurement of brain oxidative stress markers
The activities of brain catalase (CAT) and superoxide dismutase (SOD) were measured by ELISA using kits supplied by CUSABIO (Hubei, China). Brain malondialdehyde (MDA) level and reduced glutathione (GSH) level were measured colorimetrically using kits supplied by Eagle Biosciences (Boston, MA, USA).
Measurement of brain inflammatory markers
Brain TNF-α, NF-κB, and phospho-NF-κB (pNF-κB) levels were measured by ELISA technique using kits provided by Sigma Aldrich (St. Louis, MO, USA), Novus Biologicals (Centennial, CO, USA), and Ray Biotech (Peachtree Corners, GA, USA), respectively.
Histopathological examination
Brain tissue samples were collected into PBS and fixed overnight in 10% formalin at 4 °C. Following proper fixation, dehydration of the specimens was done in ascending grades of ethyl alcohol (70%, 90%, and then 100%). The specimens were cleared in xylol, impregnated, and then embedded in paraffin wax. Five-micron sections were cut using a rotatory microtome. Brain sections were stained with hematoxylin and eosin (H&E) for studying the general histological structure of brain tissue giving the cytoplasm a red color and the nucleus a blue color. A semi-quantitative morphometric analysis for the percentage of damaged area was performed using Leica Qwin 500 image analyzer (Leica Microsystems GmbH, Wetzlar, Germany) (Gan et al. 2005). The percentage of damaged brain area was determined based on the dilation and congestion in blood vessels, presence of apoptotic cells (having small darkly stained nuclei surrounded by empty space), shrinkage of pyramidal cells, presence of hemorrhage, and vacuolization.
Statistical analysis
Data are expressed as mean ± standard error of the mean (SEM) unless otherwise stated. Statistical analysis was performed using GraphPad Prism software v.8 (GraphPad Software Inc., La Jolla, CA, USA). The statistical significance of difference between group means was tested using two-way repeated measures analysis of variance (ANOVA) for body weight data or ordinary one-way ANOVA for other data followed by Tukey’s post hoc test. A significant difference was assumed for values of P < 0.05.
Results
Part 1
Diabetes provokes a depressive-like behavior and biochemical alterations that resemble reserpine-induced depression
As depicted in Table 1, diabetic rats had significantly elevated fasting serum glucose level and significantly reduced fasting serum insulin, while reserpine-treated rats showed only significant reduction in fasting serum insulin compared to control rats. The glycemic parameters were significantly higher in diabetic rats compared with reserpine-treated rats.
Diabetic rats and reserpine-treated rats showed a comparable significant increase in the immobility time, which reflects a depressive behavior, compared with control rats. In addition, diabetic rats and reserpine-treated rats exhibited significant reduction in brain serotonin (both cortical and hippocampal), brain BDNF (both cortical and hippocampal), and serum Aβ1–42 levels compared with control rats. The levels of cortical serotonin, cortical BDNF, and hippocampal BDNF were lower in reserpine-treated rats compared with diabetic rats. Moreover, serum corticosterone level was significantly elevated in diabetic rats indicating the activation of HPA.
It is worth mentioning that there was non-significant difference in body weight between control, DM, and reserpine groups. A significant reduction in the activities of the antioxidant enzymes CAT and SOD, as well as total GSH levels, was observed in brain tissue from DM and reserpine groups compared with the control group. On the other hand, both diabetic rats and reserpine-treated rats showed significantly increased brain MDA level, whereas only diabetic rats showed significant increases in TNF-α, total NF-κB, and pNF-κB compared with control group.
Antidiabetic drugs improve glycemic parameters and diabetes-associated depression
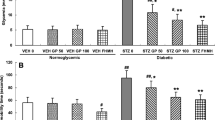
As depicted in Fig. 1a, b, the treatment of diabetic rats with vildagliptin, pioglitazone, glyburide, or metformin significantly reduced fasting serum glucose level, whereas they significantly elevated fasting serum insulin level compared with DM group. Among the treatment groups, vildagliptin induced the largest reduction in serum glucose level compared with pioglitazone, glyburide, or metformin. Similarly, vildagliptin induced the largest increase in serum insulin level compared with other drugs.
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), and metformin (M) on serum blood glucose level (a), insulin level (b), immobility time (c), serum corticosterone level (d), serum Aβ1–42 level (e), and body weight (f) in diabetic rats. Data are expressed as boxplot (1st, 2nd, and 3rd quartiles) for body weight data and mean ± SEM for other data (n = 4–5). Statistical analysis was done using two-way repeated measures ANOVA for body weight data and one-way ANOVA for other data followed by Tukey’s post hoc test. *P < 0.05 vs. diabetic group (DM); $P < 0.05 between designated pairs; ∇P < 0.05 vs. G
The antidiabetic drugs improved diabetes-associated depression. The administration of vildagliptin, pioglitazone, glyburide, or metformin comparably and significantly reduced the immobility time compared with diabetic rats (Fig. 1c). In addition, all drugs significantly reduced serum corticosterone level compared with diabetic rats (Fig. 1d). Furthermore, only vildagliptin, pioglitazone, and metformin significantly elevated serum Aβ1–42 level compared with diabetic rats. The effects of vildagliptin and metformin were comparable and significantly higher compared with pioglitazone (Fig. 1e). Moreover, the body weight of rats increased significantly over time (P < 0.0001); however, there was no significant change in weight among groups at different time point (P = 0.46).
To confirm the antidepressant activity of antidiabetics, depression biomarkers such as serotonin and BDNF have been measured. Drug treatment abolished diabetes-associated reduction in cortical and hippocampal levels of serotonin and BDNF. The administration of vildagliptin, pioglitazone, glyburide, or metformin significantly increased both cortical and hippocampal serotonin level compared with DM group. The effects of the drugs were comparable (Fig. 2a). In addition, all drugs significantly increased cortical BDNF level, while only vildagliptin, glyburide, and metformin significantly increased hippocampal BDNF level compared with diabetic rats (Fig. 2b). The effects of glyburide and metformin were the highest among drugs regarding cortical BDNF, while the effects of vildagliptin and glyburide were the highest among drugs regarding hippocampal BDNF.
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), and metformin (M) on cortical (left axis) and hippocampal (right axis) serotonin level (a) and BDNF level (b) in diabetic rats. Data are expressed as mean ± SEM (n = 3–5). Statistical analysis was done using one-way ANOVA followed by Tukey’s post hoc test. *P < 0.05 vs. diabetic group (DM); $P < 0.05 between designated pairs; ΔP < 0.05 vs. P
Antidiabetic drugs improve oxidative stress and inflammatory markers in the brains of diabetic rats
The administration of vildagliptin, pioglitazone, glyburide, and metformin significantly increased brain CAT and SOD activity compared with diabetic rats. The effects of vildagliptin were the highest among the treatment groups (Fig. 3a, b). On the other hand, drug treatment resulted in significant reductions of MDA level associated with significant increases in GSH level in the brain of diabetic rats. In this regard, the effect of vildagliptin seems to be the highest, while the effect of glyburide seems to be the lowest (Fig. 3c, d).
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), and metformin (M) on brain catalase (CAT) activity (a), superoxide dismutase (SOD) activity (b), malondialdehyde (MDA) level (c), reduced glutathione (GSH) level (d), total and phospho-nuclear factor-kappa B (tNF-kB, pNF-kB) level (e), and tumor necrosis factor-alpha (TNF-α) level (f) in diabetic rats. Data are expressed as mean ± SEM (n = 3–5). Statistical analysis was done using one-way ANOVA followed by Tukey’s post hoc test. *P < 0.05 vs. diabetic group (DM); $P < 0.05 between designated pairs; ΔP < 0.05 vs. G
On the other hand, drug treatment significantly reduced total and phosphorylated NF-κB levels; whereas only vildagliptin, pioglitazone, and metformin significantly reduced TNF-⍺ level in the brain of diabetic rats. Like other effects, vildagliptin evoked the best effect, while glyburide evoked the minimal effect (Fig. 3e, f).
Effect on the histopathology of the cerebral cortex
As depicted in Fig. 4, cerebral cortex of control rats demonstrated normal pyramidal cells and granular cells with rounded open face nuclei. On the other hand, cerebral cortex of diabetic rats and reserpine-treated rats comparably showed shrunken pyramidal cells surrounded by empty spaces. In addition, dilated congested blood vessels were observed. On the other hand, cerebral cortex of diabetic rats treated with vildagliptin, pioglitazone, glyburide, or metformin showed marked improvement with a histologic picture very close to the control rats. A morphometric analysis for the damaged brain area showed a significant increase in the damaged area in diabetic and rreserpine-treated rats compared with control rats. Treatment of rats with vildagliptin, pioglitazone, glyburide, or metformin significantly abrogated the damage induced by diabetes.
Histopathological examination (H&E) of cerebral cortex of diabetic rats (× 400). Representative photomicrographs are depicted from (a) control rats showing normal pyramidal cells (P), granular cells (G) with rounded open face nuclei, and pink-stained neuropil (N); (b, c) diabetic rats showing shrunken pyramidal cells surrounded by empty space (single arrow) and dilated, congested blood vessels (double arrows); (d) reserpine-treated rats showing shrunken pyramidal cells surrounded with empty space (single arrow) and dilated, congested blood vessel (double arrows); (e–h) vildagliptin-, pioglitazone-, glyburide-, and metformin-treated rats, respectively, showing normal pyramidal cells (P), granular cells (G) with rounded open face nuclei, and pink-stained neuropil (N); and (i) quantitative morphometric analysis showing the percentage of the damaged brain area. *P < 0.05 vs. control (CT); ΔP < 0.05 vs. diabetic group (DM), ∇P < 0.05 vs. R
Part 2
Antidiabetic drugs and fluoxetine improve glycemic parameters comparably in reserpine depression model
As depicted in Fig. 5, the administration of reserpine over 6 weeks impaired glycemic parameters in normal rats. It significantly increased serum glucose level, reduced serum insulin level, and increased HOMA-IR compared with control rats. On the other hand, antidiabetic drugs and fluoxetine significantly decreased serum glucose level and HOMA-IR to a similar degree compared with reserpine-treated rats. However, only metformin significantly increased serum insulin level compared with reserpine-treated rats. Although vildagliptin, pioglitazone, and fluoxetine increased serum insulin compared with reserpine group, albeit such increases were not significant.
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), metformin (M), and fluoxetine (F) on serum blood glucose level (a), insulin level (b), and homeostatic model assessment of insulin resistance (HOMA-IR) (c) in rats treated with reserpine (R). Data are expressed as mean ± SEM (n = 3). Statistical analysis was done using one-way ANOVA followed by Tukey’s post hoc test. *P < 0.05 vs. control group (CT), $P < 0.05 between designated pairs, ΔP < 0.05 vs. R
Antidiabetic drugs and fluoxetine improve reserpine-induced depression comparably
As depicted in Fig. 6, there was a significant increase in immobility time and a significant reduction in serum Aβ1–42 level in reserpinized rats compared with control group. Vildagliptin, pioglitazone, glyburide, metformin, and fluoxetine administration caused comparable, significant decreases in immobility time compared with reserpine group. Similarly, these drugs significantly improved serum Aβ1–42 level except for glyburide. In this regard, the effects of both vildagliptin and fluoxetine were comparable and were the highest among treatment groups.
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), metformin (M), and fluoxetine (F) on immobility time (a) and serum β-amyloid 1–42 (b) in rats treated with reserpine (R). Data are expressed as mean ± SEM (n = 3). Statistical analysis was done using one-way ANOVA followed by Tukey’s post hoc test. *P < 0.05 vs. control group (CT); ΔP < 0.05 vs. R; $P < 0.05 vs. G; @P < 0.05 vs. M; θP < 0.05 vs. P
There were significant reductions in the levels of serotonin, norepinephrine, and BDNF in the cortex and the hippocampus of reserpinized rat compared with control group. The antidiabetic drugs and fluoxetine significantly elevated serotonin level in the cortex and hippocampus compared with reserpine group except for glyburide (Fig. 7a). In a similar way, the treatment of reserpinized rats with vildagliptin, pioglitazone, glyburide, and fluoxetine significantly increased cortical norepinephrine compared with reserpine group. However, all drug treatment significantly increased hippocampal norepinephrine (Fig. 7b). In this regard, the effects of vildagliptin and pioglitazone are the highest and are comparable to that of fluoxetine. Moreover, the treatment of reserpinized rats with vildagliptin, pioglitazone, glyburide, metformin, and fluoxetine significantly increased cortical and hippocampal BDNF compared with reserpine group (Fig. 7c). The effects of vildagliptin and pioglitazone are the highest and are comparable to that of fluoxetine.
The effect of vildagliptin (V), pioglitazone (P), glyburide (G), metformin (M), and fluoxetine (F) on cortical (left axis) and hippocampal (right axis) serotonin level (a), norepinephrine level (b), and BDNF level (c) in rats treated with reserpine (R). Data are expressed as mean ± SEM (n = 3). Statistical analysis was done using one-way ANOVA followed by Tukey’s post hoc test. *P < 0.05 vs. control group (CT); ΔP < 0.05 vs. R; $P < 0.05 vs. G; @P < 0.05 vs. M
Effect on histopathology of the cerebral cortex of reserpine-treated rats
The cerebral cortex of control rats showed normal pyramidal cells and granular cells having rounded open face nuclei. Reserpinized rats exhibited shrunken pyramidal cells surrounded by empty spaces. The administration of vildagliptin, pioglitazone, glyburide, metformin, or fluoxetine markedly improved the histologic cytoarchitecture with nearly normal pyramidal and granular cells. A morphometric analysis for the damaged brain area showed a significant increase in the damaged area in reserpine-treated rats compared with control rats. Treatment of rats with vildagliptin, pioglitazone, glyburide, metformin, or fluoxetine significantly abrogated the damage induced by reserpine (Fig. 8).
Histopathological examination (H&E) of cerebral cortex of rats treated with reserpine (× 400). Representative photomicrographs are depicted from (a) control rats showing normal pyramidal cells (P), granular cells (G) with rounded open face nuclei, and pink-stained neuropil (N); (b) reserpine-treated rats showing shrunken pyramidal cells surrounded by empty space (single arrow); and (c–g) vildagliptin-, pioglitazone-, glyburide-, metformin-, and fluoxetine-treated rats, respectively, showing normal pyramidal cells (P), granular cells (G) with rounded open face nuclei, pink-stained neuropil (N), and (h) quantitative morphometric analysis showing the percentage of the damaged brain area. *P < 0.05 vs. control (CT); ΔP < 0.05 vs. R
Discussion
T2DM is a chronic disease, which is associated with various psychological and physical complications. Depression is considered one of the most psychiatric comorbidities related to diabetes (Rotella and Mannucci 2013). Depression incidence is about two times higher in people diagnosed with T2DM compared to individuals with normal glucose metabolism (Roy and Lloyd 2012). Previous studies have reported that the combined use of antidiabetic and antidepressant drugs was accompanied by increased risk of cardiovascular complications such as myocardial infarction (Rådholm et al. 2016). Therefore, identifying antidiabetic agents, which have antidepressant effects, will potentially benefit patients with T2DM. The present study is the first, to the best of our knowledge, to compare the antidepressant activities of commonly used antidiabetic agents, vildagliptin, pioglitazone, glyburide, and metformin in the presence or absence of T2DM.
In the current study, a well-established T2DM animal model using HFD and STZ was used to induce DM-associated depression in rats (Nankar and Doble 2017). Diabetic rats showed a depressive state similar to that developed in reserpine-treated rats. Increased immobility in FST, reduced brain levels of serotonin and BDNF, and reduced serum level of Aβ1–42 were observed in diabetic and in reserpine-treated rats. In support of our findings, Ye et al. (2017) reported that high-fat diet and a small dose of STZ administration showed typical signs of T2DM and exhibited depressive-like bahaviors, which are manifested by a reduction in the spontaneous activity and the number of crossings in the open field test as well as an increase in immobility in FST.
Dysregulation of serotonin system is a hallmark in diabetes-associated depression. Reduction in central serotonin availability can be mediated by diabetes-induced oxidative stress and inflammation in the brain. Oxidative stress causes impaired glucocorticoid receptor function, loss of negative feedback, and alteration of HPA axis function. Hyperactivity of HPA axis increases glucocorticoids release, which in turn reduces serotonin synhesis (Prabhakar et al. 2015). On the other hand, cytokines released due to brain inflammation in DM reduce the synthesis and increase the reuptake of serotonin and eventually decrease its availability (Felger and Lotrich 2013). Moreover, glucocorticoids and inflammatory cytokines reduce the activity and the exprssion of BDNF, a neurotropic factor that promotes the differentiation and survival of serotonergic neurons (Autry and Monteggia 2012). Herein, we found that diabetic rats showed reduced cortical and hippocampal serotonin and BDNF levels, as well as elevated serum corticosterone indicating hyperactivity of HPA axis. Diabetes was also associated with increased oxidative stress and inflammation in the brain, which may be responsible for serotonin dysregulation and induction of depression.
In the present study, reserpine was used to induce chronic depression in non-diabetic animals. However, we observed that reserpine not only provoked a depressive-like behavior but also increased serum glucose and HOMA-IR and reduced serum insulin. Moreover, improvement of these glycemic parameters by the antidepressant drug, fluoxetine, suggests that diabetes might be produced as a result of depression. These observations concur with previous studies, which demonstrated that chronic, mild stress-induced depression is accompanied by impaired glucose metabolism and insulin sensitivity (Shen et al. 2017). This is not surprising because the association between depression and subsequent development of T2DM has been reported by several meta-analysis studies (Cosgrove et al. 2007).
As pointed out in the results, vildagliptin, pioglitazone, glyburide, and metformin improved glycemic parameters in HFD/STZ-treated animals with different effectiveness. Hereof, vildagliptin showed the best, while glyburide showed the least, ameliorative effect on blood glucose and insulin levels. However, the antidiabetic efficiency of all tested compounds was comparable in reserpine-treated animals, which are considered pre-diabetics according to their fasting blood glucose levels and HOMA-IR. A plausible explanation for this is that these drugs have different mechanisms of action, and their activities may vary according to the stage of DM (Meneses et al. 2015).
Relative to depression, antidiabetic drugs used in the current study ameliorated both diabetes- and reserpine-mediated depression. Planned comparisons revealed that all the tested compounds reduced immobility time in FST, improved histopathological damage, and increased cortical and hippocampal serotonin to comparable levels in DM rats. However, they had variable activities on Aβ1–42, corticosterone, and BDNF levels. In addition, there was no significant change in weight among groups at different time points indicating the independency of the antidepressant effect on body weight change.
Compared to other treatments, vildagliptin showed the greatest effect on Aβ1–42, corticosterone, and hippocampal BDNF levels. We speculate that this might be due to its eminent activity on regulating glucose and its profound antioxidant and anti-inflammatory effect. Vildagliptin showed the highest ameliorative effect on oxidative stress and inflammatory markers in the brain. These observations are in line with previous reports indicating that vildagliptin reduced brain MDA level and NF-κB expression in diabetic rats, and this effect was associated with increase in the BDNF (El Batsh et al. 2015). Although vildagliptin cannot pass the blood brain barrier (BBB), its central activity may be mediated by glucagon-like peptide-1 (GLP-1). Vildagliptin inhibits peripheral dipeptidyl peptidase (DPP)-4 enzyme activity resulting in an increase in the GLP-1 level, which can diffuse into the brain (Pintana et al. 2013). GLP-1 acts on GLP-1 receptors located in different areas of the brain such as the hippocampus, frontal cortex, and other areas known to be important for the control of energy homeostasis (Cork et al. 2015). Although non-significant, the effect of vildagliptin on immobility time is stronger than fluoxetine. This finding seems interesting and can be explained somehow by the stronger antioxidant activity of vildagliptin in brain as indicated by the increase in GSH level, as well as the larger elevation of hippocampal BDNF in vildagliptin group when compared to fluoxetine group. However, such an effect needs further studies to be confirmed.
On the other hand, glyburide reduced immobility time in FST and increased serotonin levels in DM-associated depression to extents comparable to other treatment groups. Even though glyburide elevated BDNF to a level similar to vildagliptin in hippocampus and even higher in cortex, it showed minimal change in corticosterone and Aβ1–42 in DM-associated depression and the least effect on serotonin and Aβ1–42 in reserpine-induced depression. There are three possible explanations for these observations: (1) glyburide elicited the least effect on serum glucose and insulin levels, (2) glyburide showed less antioxidant and minimal anti-inflammatory activity in the brain compared with other treatment groups, and (3) the inability of glyburide to pass the blood brain barrier as a result of its high plasma protein binding (Lahmann et al. 2015). Overall, our observations are in accordance with the findings reported by Su et al. (2017) and Esmaeili et al. (2018) indicating that glyburide reduced depression-related symptoms in animal model of Alzheimer’s disease and chronic unpredictable mild stress-induced depression, respectively.
Pioglitazone is an agonist to peroxisome proliferator-activated receptor-gamma (PPAR-γ), which regulates the transcription of genes involved in lipid and carbohydrate metabolism. Previous studies have reported that pioglitazone has the tendency to cross the blood brain barrier and exhibits antidepressant effect through its action on PPAR-γ receptor (Liao et al. 2017). Furthermore, the neuroprotective activity of pioglitazone and other PPAR-γ agonists is mediated by their central antioxidant and anti-inflammatory effect (Kaundal and Sharma 2010). In line with previous reports, the current study showed that pioglitazone elicited an antidepressant effect, which was accompanied by amelioration of serotonin, BDNF, corticosterone, and Aβ1–42 levels in DM-associated depression and restoration of Aβ1–42, serotonin, NE, and BDNF levels in reserpine-induced depression.
We also observed that metformin reduced the depression in DM and reserpine-treated rats. In DM rats, the antidepressant activity of metformin was associated with improvement of serum corticosterone levels and reduction of oxidative stress and inflammation in the brain. In agreement with our observations, Shivavedi et al. (2017) reported that metformin increased brain levels of serotonin and norepinephrine and reduced the activity of HPA axis in depressive animals with DM. Their data also suggested that the effect of metformin on HPA axis is mediated by its antioxidant and anti-inflammatory activity in the brain. In addition, previous studies reported that the antioxidant and anti-inflammatory activity of metformin may be mediated by AMP-activated protein kinase (AMPK)-dependent or independent pathways (Park et al. 2012; Calixto et al. 2013; Saisho 2015). Besides, having the ability to cross the blood brain barrier provides an explanation for the central activity of metformin (Labuzek et al. 2010). It is important to note that both pioglitazone and metformin elicited comparable antioxidant and anti-inflammatory activity in the brain of diabetic rats but to a lesser extent than vildagliptin and higher than glyburide. This may explain why the antidepressant effects of pioglitazone and metformin are less than vildagliptin and higher than glyburide.
The study still has a few limitations. Reserpine was used as a documented model for depression to test the hypothesis that the studied antidiabetic drugs can also elicit antidepressant effect in non-diabetic rats. However, reserpine caused an elevation of blood glucose level. Thus, it was difficult to demonstrate whether the antidepressant activities of these compounds are independent of their antidiabetic effects or not. To address this issue, prospective studies should be conducted using other models of depression such as stress-induced depression. Yet, the results of this study still provide insights into the differences between antidiabetic drugs of different classes regarding their antidepressant effects.
In conclusion, the four tested antidiabetic agents, vildagliptin, glyburide, pioglitazone, and metformin, showed antidepressant effects in DM- and reserpine-induced depression. The difference in their effectiveness in DM rats might be due to their tendency to reach the central nervous system, the extent of their antioxidant and anti-inflammatory effects, and their ability to reduce the activation of HPA axis. In addition, the results seem promising for further evaluating the application of antidiabetic drugs alone as potential alternatives of antidepressant drugs in diabetes-associated depression.
Abbreviations
- Aβ40/42:
-
β-Amyloid 40/42
- Aβ1–42:
-
β-Amyloid 1-42
- AGEs:
-
Advanced glycation end products
- AMPK:
-
Adenosine monophosphate-activated protein kinase
- ANOVA:
-
Analysis of variance
- BBB:
-
Blood brain barrier
- BDNF:
-
Brain-derived neurotrophic factor
- CAT:
-
Catalase
- CT:
-
Control
- DM:
-
Diabetes mellitus
- DMSO:
-
Dimethyl sulfoxide
- DPP-4:
-
Dipeptidyl peptidase-4 inhibitor
- ELISA:
-
Enzyme-linked immunosorbent assay
- F:
-
Fluoxetine
- FST:
-
Forced swim test
- G:
-
Glyburide
- GLP-1:
-
Glucagon-like peptide 1
- GSH:
-
Reduced glutathione
- H&E:
-
Hematoxylin and eosin
- HFD:
-
High-fat diet
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- HPA:
-
Hypothalamic–pituitary–adrenal
- IDO:
-
Indoleamine 2,3-dioxygenase
- M:
-
Metformin
- MDA:
-
Malondialdehyde
- NF-kB:
-
Nuclear factor-kappa B
- P:
-
Pioglitazone
- PBS:
-
Phosphate-buffered saline
- PKC:
-
Protein kinase C
- p.NF-KB:
-
Phospho-nuclear factor-kappa B
- PPAR-γ:
-
Peroxisome proliferator activated receptor-gamma
- ROS:
-
Reactive oxygen species
- SEM:
-
Standard error of the mean
- SOD:
-
Superoxide dismutase
- SSRIs:
-
Selective serotonin reuptake inhibitors
- STZ:
-
Streptozotocin
- T2DM:
-
Type 2 diabetes mellitus
- TNF-α:
-
Tumor necrosis factor-alpha
- V:
-
Vildagliptin
References
Ali S, Stone MA, Peters JL, Davies MJ, Khunti K (2006) The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet Med 23:1165–1173
Antkiewicz-Michaluk L, Wąsik A, Możdżeń E, Romańska I, Michaluk J (2014) Antidepressant-like effect of tetrahydroisoquinoline amines in the animal model of depressive disorder induced by repeated administration of a low dose of reserpine: behavioral and neurochemical studies in the rat. Neurotox Res 26:85–98
Arafa NM, Marie MA, AlAzimi SA (2016) Effect of canagliflozin and metformin on cortical neurotransmitters in a diabetic rat model. Chem Biol Interact 258:79–88
Autry AE, Monteggia LM (2012) Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev 64:238–258
Calixto MC, Lintomen L, Andre DM, Leiria LO, Ferreira D, Lellis-Santos C, Anhe GF, Bordin S, Landgraf RG, Antunes E (2013) Metformin attenuates the exacerbation of the allergic eosinophilic inflammation in high fat-diet-induced obesity in mice. PLoS One 8:e76786
Colle R, de Larminat D, Rotenberg S, Hozer F, Hardy P, Verstuyft C, Fève B, Corruble E (2017) Pioglitazone could induce remission in major depression: a meta-analysis. Neuropsychiatr Dis Treat 13:9–16
Cork SC, Richards JE, Holt MK, Gribble FM, Reimann F, Trapp S (2015) Distribution and characterisation of glucagon-like peptide-1 receptor expressing cells in the mouse brain. Molec Metabol 4:718–731
Cosgrove MP, Sargeant LA, Griffin SJ (2007) Does depression increase the risk of developing type 2 diabetes? Occup Med 58:7–14
Coupland NJ, Bell CJ, Potokar JP (1996) Serotonin reuptake inhibitor withdrawal. J Clin Psychopharmacol 16:356–362
Dong XZ, Wang DX, Lu YP, Yuan S, Liu P, Hu Y (2017) Antidepressant effects of Kai-Xin-San in fluoxetine-resistant depression rats. Braz J Med Biol Res 50(10):e6161
El Batsh MM, Manal M, Shafik NM, Younos IH (2015) Favorable effects of vildagliptin on metabolic and cognitive dysfunctions in streptozotocin-induced diabetic rats. Eur J Pharmacol 769:297–305
Esmaeili MH, Bahari B, Salari AA (2018) ATP-sensitive potassium-channel inhibitor glibenclamide attenuates HPA axis hyperactivity, depression- and anxiety-related symptoms in a rat model of Alzheimer’s disease. Brain Res Bull 137:265–276
Felger JC, Lotrich FE (2013) Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 246:199–229
Fergusson D, Doucette S, Glass KC, Shapiro S, Healy D, Hebert P, Hutton B (2005) Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. BMJ 330:396
Flohé L, Brigelius-Flohé R, Saliou C, Traber MG, Packer L (1997) Redox regulation of NF-kappa B activation. Free Radic Biol Med 22:1115–1126
Gan P, Cheng JS, Ng YK, Ling EA (2005) Role of GABA in electro-acupuncture therapy on cerebral ischemia induced by occlusion of the middle cerebral artery in rats. Neurosci Lett 383:317–321
Gelenberg AJ, Delgado P, Nurnberg HG (2000) Sexual side effects of antidepressant drugs. Curr Psychiatry Rep 2:223–227
Goodnick PJ (2001) Use of antidepressants in treatment of comorbid diabetes mellitus and depression as well as in diabetic neuropathy. Ann Clin Psychiatry 13:31–41
Guo M, Mi J, Jiang QM, Xu JM, Tang YY, Tian G, Wang B (2014) Metformin may produce antidepressant effects through improvement of cognitive function among depressed patients with diabetes mellitus. Clin Exp Pharmacol Physiol 41:650–656
Hoyo-Becerra C, Schlaak JF, Hermann DM (2014) Insights from interferon-alpha-related depression for the pathogenesis of depression associated with inflammation. Brain Behav Immun 42:222–231
Hritcu L, Gorgan LD (2014) Intranigral lipopolysaccharide induced anxiety and depression by altered BDNF mRNA expression in rat hippocampus. Prog Neuro-Psychopharmacol Biol Psychiatry 51:126–132
Huang Q-j, Jiang H, Hao X-l, Minor TR (2004) Brain IL-1beta was involved in reserpine-induced behavioral depression in rats. Acta Pharmacol Sin 25:293–296
Ishijima S, Baba H, Maeshima H, Shimano T, Inoue M, Suzuki T, Arai H (2018) Glucocorticoid may influence amyloid β metabolism in patients with depression. Psychiatry Res 259:191–196
Kaundal RK, Sharma SS (2010) Peroxisome proliferator-activated receptor gamma agonists as neuroprotective agents. Drug News Perspect 23:241–256
Labuzek K, Suchy D, Gabryel B, Bielecka A, Liber S, Okopien B (2010) Quantification of metformin by the HPLC method in brain regions, cerebrospinal fluid and plasma of rats treated with lipopolysaccharide. Pharmacol Rep 62:956–965
Lahmann C, Kramer HB, Ashcroft FM (2015) Systemic administration of glibenclamide fails to achieve therapeutic levels in the brain and cerebrospinal fluid of rodents. PLoS One 10:e0134476
Liao L, Zhang X, Li J, Zhang Z, Yang C, Rao C, Zhou C, Zeng L, Zhao L, Fang L (2017) Pioglitazone attenuates lipopolysaccharide-induced depression-like behaviors, modulates NF-κB/IL-6/STAT3, CREB/BDNF pathways and central serotonergic neurotransmission in mice. Int Immunopharmacol 49:178–186
MacGillivray S, Arroll B, Hatcher S, Ogston S, Reid I, Sullivan F, Williams B, Crombie I (2003) Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ 326:1014
Markowitz SM, Gonzalez JS, Wilkinson JL, Safren SA (2011) A review of treating depression in diabetes: emerging findings. Psychosomatics 52:1–18
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Meneses JM, Silva MB, Sousa M, Sa R, Oliveira FP, Alves GM (2015) Antidiabetic drugs: mechanisms of action and potential outcomes on cellular metabolism. Curr Pharm Des 21:3606–3620
Nankar RP, Doble M (2017) Hybrid drug combination: anti-diabetic treatment of type 2 diabetic Wistar rats with combination of ellagic acid and pioglitazone. Phytomedicine 37:4–9
Nazaroglu NK, Sepici-Dincel A, Altan N (2009) The effects of sulfonylurea glyburide on superoxide dismutase, catalase, and glutathione peroxidase activities in the brain tissue of streptozotocin-induced diabetic rat. J Diabetes Complicat 23:209–213
Park CS, Bang BR, Kwon HS, Moon KA, Kim TB, Lee KY, Moon HB, Cho YS (2012) Metformin reduces airway inflammation and remodeling via activation of AMP-activated protein kinase. Biochem Pharmacol 84:1660–1670
Pintana H, Apaijai N, Chattipakorn N, Chattipakorn SC (2013) DPP-4 inhibitors improve cognition and brain mitochondrial function of insulin-resistant rats. J Endocrinol 218:1–11
Porsolt RD, Le Pichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatments. Nature 266:730–732
Prabhakar V, Gupta D, Kanade P, Radhakrishnan M (2015) Diabetes-associated depression: the serotonergic system as a novel multifunctional target. Indian J Pharm 47:4
Rådholm K, Wiréhn AB, Chalmers J, Östgren CJ (2016) Use of antidiabetic and antidepressant drugs is associated with increased risk of myocardial infarction: a nationwide register study. Diabet Med 33:218–223
Refaat R, Sakr A, Salama M, El Sarha A (2016) Combination of vildagliptin and pioglitazone in experimental type 2 diabetes in male rats. Drug Dev Res 77:300–309
Rotella F, Mannucci E (2013) Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry 74(1):31–37
Roy T, Lloyd CE (2012) Epidemiology of depression and diabetes: a systematic review. J Affect Disord 142(Suppl):S8–S21
Saisho Y (2015) Metformin and inflammation: its potential beyond glucose-lowering effect. Endocr Metab Immune Disord Drug Targets 15:196–205
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J, Collaboration ERF (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375:2215–2222
Shen J-D, Wei Y, Li Y-J, Qiao J-Y, Li Y-C (2017) Curcumin reverses the depressive-like behavior and insulin resistance induced by chronic mild stress. Metab Brain Dis 32:1163–1172
Shivavedi N, Kumar M, Tej G, Nayak PK (2017) Metformin and ascorbic acid combination therapy ameliorates type 2 diabetes mellitus and comorbid depression in rats. Brain Res 1674:1–9
Shyong Y-J, Wang M-H, Kuo L-W, Su C-F, Kuo W-T, Chang K-C, Lin F-H (2017) Mesoporous hydroxyapatite as a carrier of olanzapine for long-acting antidepression treatment in rats with induced depression. J Control Release 255:62–72
Spijker S (2011) Dissection of rodent brain regions. In: Li KW (ed) Neuroproteomics. Humana Press, Totowa, pp 13–26
Su WJ, Peng W, Gong H, Liu YZ, Zhang Y, Lian YJ, Cao ZY, Wu R, Liu LL, Wang B, Wang YX, Jiang CL (2017) Antidiabetic drug glyburide modulates depressive-like behavior comorbid with insulin resistance. J Neuroinflammation 14:210
Wang L, Duan G, Lu Y, Pang S, Huang X, Jiang Q, Dang N (2013) The effect of simvastatin on glucose homeostasis in streptozotocin induced type 2 diabetic rats. J Diabetes Res 2013:274986
Ye M, Ke Y, Liu B, Yuan Y, Wang F, Bu S, Zhang Y (2017) Root bark of Morus alba ameliorates the depressive-like behaviors in diabetic rats. Neurosci Lett 637:136–141
Acknowledgments
The authors acknowledge Dr. Rehab Hasan, Department of Histology, Faculty of Medicine, Al-Azhar University, Egypt, for her great effort in the histopathological examination. The authors would like also to thank Dr. Tracey L. Woodlief, Department of Pharmacology and Toxicology, East Carolina University, USA, for the English language review.
Author information
Authors and Affiliations
Contributions
MFM and AAAM conceived and designed research. NE conducted the experiments. NE, AAAM, and ES analyzed the data. NE, AAAM, and ES wrote the first draft of manuscript. MFM and AAAM revised and edited the manuscript. All the authors read and approved the manuscript.
Corresponding author
Ethics declarations
All procedures were conducted in accordance with the accepted principles for care and use of laboratory animals and were approved by the animal ethics committee of Faculty of Pharmacy, Zagazig University, Egypt (Approval number: P1-12-2017).
Conflict of interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Soliman, E., Essmat, N., Mahmoud, M.F. et al. Impact of some oral hypoglycemic agents on type 2 diabetes-associated depression and reserpine-induced depression in rats: the role of brain oxidative stress and inflammation. Naunyn-Schmiedeberg's Arch Pharmacol 393, 1391–1404 (2020). https://doi.org/10.1007/s00210-020-01838-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-020-01838-w