Abstract
Rationale
Aberrant prefrontal-hippocampal (PFC-HC) connectivity is disrupted in several psychiatric and at-risk conditions. Advances in rodent functional imaging have opened the possibility that this phenotype could serve as a translational imaging marker for psychiatric research. Recent evidence from functional magnetic resonance imaging (fMRI) studies has indicated an increase in PFC-HC coupling during working-memory tasks in both schizophrenic patients and at-risk populations, in contrast to a decrease in resting-state PFC-HC connectivity. Acute ketamine challenge is widely used in both humans and rats as a pharmacological model to study the mechanisms of N-methyl-d-aspartate (NMDA) receptor hypofunction in the context of psychiatric disorders.
Objectives
We aimed to establish whether acute ketamine challenge has consistent effects in rats and humans by investigating resting-state fMRI PFC-HC connectivity and thus to corroborate its potential utility as a translational probe.
Methods
Twenty-four healthy human subjects (12 females, mean age 25 years) received intravenous doses of either saline (placebo) or ketamine (0.5 mg/kg body weight). Eighteen Sprague-Dawley male rats received either saline or ketamine (25 mg/kg). Resting-state fMRI measurements took place after injections, and the data were analyzed for PFC-HC functional connectivity.
Results
In both species, ketamine induced a robust increase in PFC-HC coupling, in contrast to findings in chronic schizophrenia.
Conclusions
This translational comparison demonstrates a cross-species consistency in pharmacological effect and elucidates ketamine-induced alterations in PFC-HC coupling, a phenotype often disrupted in pathological conditions, which may give clue to understanding of psychiatric disorders and their onset, and help in the development of new treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The dorsolateral prefrontal cortex (DLPFC) is one of the major anatomical hubs implicated in the pathophysiology of schizophrenia (Callicott et al. 2003; Seidman et al. 2006). Recent studies point to a dysregulation of functional coupling between the right DLPFC and left hippocampus in patients suffering from schizophrenia and high-risk individuals (Esslinger et al. 2009; Meyer-Lindenberg et al. 2001; Rasetti et al. 2011). Complementing these task-dependent measures, functional connectivity in the absence of any task, as measured by low-frequency blood oxygenation level-dependent (BOLD) oscillations, has been found to be reduced in schizophrenic patients (Rotarska-Jagiela et al. 2010; Zhou et al. 2008).
We have recently established a homology of prefrontal-hippocampal (PFC-HC) connectivity features in humans and rats (Schwarz et al. 2013); however, the extent to which this circuit can be modulated in a consistent way by the same pharmacological manipulation in both species remains to be established. Here, we focused on resting-state functional magnetic resonance imaging (rs-fMRI) since the construction of a valid translational biomarker in rats is more tractable this way given that n-back tasks are heterogeneous in humans and are hard to translate to anesthetized or restrained rats in the MRI scanner.
Ketamine, a dissociative anesthetic at high doses, acts as an N-methyl-d-aspartate (NMDA) receptor antagonist. At lower, subanesthetic doses, ketamine is widely used in both species to investigate mechanisms underlying psychosis and, more recently, as a potential rapid onset antidepressant (Diamond et al. 2014; Niciu et al. 2014; Salvadore et al. 2010; Scheidegger et al. 2012; Vollenweider et al. 1997; Zarate et al. 2013).
Ketamine has been applied in humans (D’Souza et al. 2012; Krystal et al. 2005; Morgan et al. 2004) and animals (Garcia et al. 2008; Pitsikas et al. 2008; Skoblenick and Everling. 2012) to model translationally relevant behavioral effects. However, in most cases, these studies did not involve explicitly aligned experiments in both humans and animals. Despite the well-validated use of ketamine application as a translational model, there is a lack of data on how acute ketamine treatment affects the functional coupling between prefrontal and subcortical regions. Here, we specifically concentrated on the hippocampus because of its formerly described changes in connectivity pattern in the context of psychosis risk (Meyer-Lindenberg et al. 2001). Besides PFC-HC circuit has been postulated to be important in psychiatric disorders (Godsil et al. 2013).
In our earlier study, we hypothesized that, rather than modeling such a complex and heterogeneous disease as schizophrenia, ketamine challenge may be used to induce a hyperglutamatergic state similar to that of the early (prodromal) stage of the disease (Gass et al. 2014). Ketamine promotes an increased glutamate release in the PFC both in rats (Lorrain et al. 2003; Moghaddam et al. 1997) and in humans (Rowland et al. 2005; Stone et al. 2012) and increases global brain connectivity in healthy humans (Driesen et al. 2013). Another recent study which has investigated ketamine effects on thalamo-cortical connectivity supports this hypothesis (Dawson et al. 2013). In our previous study in rats (Gass et al. 2014), ketamine induced an increase in PFC-HC connectivity and we hypothesized that this increase would translate to humans.
The present study aimed to investigate whether an acute ketamine challenge has analogous effects in rats and humans on PFC-HC connectivity measures derived from rs-fMRI data. This would underscore the value of this phenotype as a translational target for pharmacological studies.
Methods
Subjects
A total of 24 participants completed the study (12 females, mean age 25 years, mean body weight 70 kg). Human fMRI data were acquired in healthy individuals in a subject- and observer-blind, placebo-controlled, randomized, three-period cross-over study. The subjects received counterbalanced single intravenous doses of either saline (placebo condition), ketamine (0.5 mg/kg body weight), or scopolamine (4 μg/kg body weight). In the placebo condition, saline alone was infused for 40 min. For the present study, we only analyzed the ketamine versus placebo conditions.
All participants provided written informed consent for a study approved by the local ethics committee (Medical Faculty Mannheim, University of Heidelberg, Germany). Subjects underwent three consecutive fMRI sessions at the same center over the course of 3 weeks.
Animals
Eighteen Sprague-Dawley male rats (373–447 g; Janvier Laboratories, Le Genest-St-Isle, France) were used for fMRI experiments. Animals were housed under controlled conditions (19–23 °C, 40–60 % humidity) with a 12:12-h light-dark cycle (lights on at 7 a.m.).
All procedures were performed according to the regulations covering animal experimentation within the European Union (European Communities Council Directive 86/609/EEC) and within the German Animal Welfare Act and were approved by the German animal welfare authorities (Regierungspräsidium Karlsruhe).
Ketamine application—humans
On each day of the experiment, subjects received an infusion via a certified intravenous pump (Braun Medical, Melsungen, Germany). To avoid order effects, the sequence of substance applications was randomly permutated across all 24 participants. A ketamine dose of 0.5 mg/kg was used following previously published protocols (Furey et al. 2010; Salvadore et al. 2010). MRI scanning took place after drug administration, with the resting-state measurement starting approximately 20 min after the end of the infusion. The participants were supervised by a certified psychiatrist.
Ketamine application—animals
The experimental design comprised two groups of N = 9 rats each. In one group, S-ketamine (Ketanest®, Pfizer Pharma GmbH, Berlin, Germany) was injected subcutaneously at a dose of 25 mg/kg dissolved in saline (total volume 1 ml/kg). The second group received the same volume of vehicle (saline). The order of ketamine and saline injections was randomized across animals and time of day. The rs-fMRI measurement started at 30 min after the ketamine/vehicle injection.
These animals are two groups from the study previously reported (Gass et al. 2014). Both groups were reanalyzed using methods as closely aligned as possible to those used for the human data (see below).
Data acquisition—human fMRI
Functional imaging was performed with a 3-T MR scanner (Siemens Trio, Erlangen, Germany), a 32-channel head-coil, and an echo-planar imaging (EPI) sequence with the following parameters: TR = 1790 ms, TE = 28 ms, 34 oblique slices (aligned to the AC-PC plane), 3-mm slice thickness, FA = 76°, FOV = 192 mm, 64 × 64 matrix, 332 volumes.
Data acquisition—animal fMRI
Experiments were conducted at a 9.4-T MRI scanner (94/20 Bruker BioSpec, Ettlingen, Germany) with Avance III hardware, BGA12S gradient system with the maximum strength of 705 mT/m and Paravision 5.1 software. Transmission and reception were achieved using a linear whole-body volume transmitter coil combined with an anatomically shaped four-channel receive-only coil array for the rat brain.
Rats were anesthetized under 4 % isoflurane (Baxter Deutschland GmbH, Unterschleissheim, Germany) in a mixture of N2 (70 %)/O2 (30 %). After positioning in the scanner (head first, prone), 2.5 % isoflurane was provided for adjustments. Then, a bolus of 0.5-ml medetomidine solution (Domitor®, Janssen-Cilag, Neuss; 0.07 mg/kg s.c.) was administered; isoflurane was slowly discontinued within the next 10 min, after which a continuous infusion of medetomidine solution started at 0.14 mg/kg/h rate.
Breathing and cardiac signals were received using a respiration pad placed beneath the chest (Small Animal Instruments Inc., NY, USA) and a pulse oximeter attached to the hindpaw, respectively. A signal breakout module (Small Animal Instruments Inc., NY, USA) and a four-channel recorder (Velleman® N.V., Gavere, Belgium) were used to record signals (10-ms resolution).
The MRI acquisition protocol for each animal comprised a FieldMap and a rs-fMRI measurement. To acquire the rs-fMRI time series, an echo-planar imaging (EPI) sequence was used with the following parameters: repetition time/echo time (TR/TE) 1700/17.5 ms, flip angle 60°, 1 segment, 29 coronal slices (ascending slice order), 96 × 96 imaging matrix, field of view 35 × 35 mm2, slice thickness 0.5 mm with 0.2 mm inter-slice gap, in-plane voxel dimension 0.365 mm, 300 acquisitions over 8.5 min. The slice stack covered the brain from the cerebellum to the posterior olfactory bulb.
Data processing and analysis—human fMRI
Data were processed using statistical parametric mapping (SPM8) (http://www.fil.ion.ucl.ac.uk/spm/) and the complementary CONN toolbox v13 (Whitfield-Gabrieli and Nieto-Castanon. 2012). Images were realigned, slice-time-corrected, spatially normalized to standard stereotaxic space (Montreal Neurological Institute (MNI) template), resampled to 3-mm isotropic voxels, and smoothed with an 8-mm full-width at half maximum (FWHM) Gaussian kernel. A band-pass filter reduced frequency bands to 0.01–0.1 Hz. Further noise correction included regression of the six motion parameters from the realignment step, their first-order derivatives, and regression of cerebrospinal fluid and white matter signals using an aCompCor-strategy (five dimensions). This method (Behzadi et al. 2007) includes the principal components of white matter/cerebrospinal fluid regions as nuisance regressors and avoids the artificial inflation of anticorrelations related to global signal regression (Chai et al. 2014).
For our seed voxel approach, we extracted the first eigenvariate from masks of the right and left DLPFC (BA9/BA46), respectively. The consecutive correlation map was Fisher-Z-transformed and used for second-level interference. Group statistics (second level) were calculated in SPM8 using flexible factorial models. Drug and order of drug application were modeled as fixed effects. As we were only interested in the ketamine versus placebo comparison, we modeled this contrast alone and treated the other factor levels as nuisance variables. For multiple comparisons correction, we used a region-of-interest mask of the left and right hippocampus as target regions, based on the Harvard-Oxford atlas (http://www.cma.mgh.harvard.edu/) with a probability threshold of 50 % (significance threshold P FWE < 0.05, ROI-corrected). Changes in both cross-hemisphere (left DLPFC to right hippocampus, and right DLPFC to left hippocampus) and unilateral (left DLPFC to left hippocampus, and right DLPFC to right hippocampus) coupling were tested.
Data processing and analysis—animal fMRI
Data were processed using SPM8. The EPI time series were corrected for magnetic field (B0) inhomogeneities using FieldMap sequences. To minimize movement effects on the signal intensities, the estimated movement parameter vectors were regressed out from each voxel (FSL, version 4.1. http://www.fmrib.ox.ac.uk/fsl). Then, respiratory and cardiac signals were filtered out from each voxel using Aztec software (van Buuren et al. 2009). Afterward, a slice-timing correction was applied to the images (SPM8). The time courses were band-pass filtered (0.01–0.1 Hz) (Analysis of Functional Neuroimages (AFNI) version 2) and finally spatially normalized (SPM8) to a rat brain template with co-registered anatomical atlas positioned in the Paxinos stereotactic coordinate system (Schwarz et al. 2006). In the end, the data were filtered to exclude the signal from the cerebrospinal fluid.
For our seed region approach, we extracted the time course from a mask of the right and left prelimbic cortex (PrL). A mean time course of the seed was extracted from each normalized, unsmoothed time series; then, the data were smoothed by 0.8 mm. Correlation coefficients were calculated for these time courses voxel-wise and transformed to Fisher Z-scores. The Z maps were fed into the second-level analyses (SPM8): a two-sample T-test for the dose of 25 mg/kg versus saline using right and left hippocampi as explicit masks (P FWE < 0.05, cluster-level and peak-level correction). Connectivity of the right PrL was tested for both right and left hippocampi, the same was applied to the left PrL.
Pharmacokinetics—humans
Blood samples for measurement of ketamine and its metabolite norketamine were 10 and 80 min after the end of the infusion, respectively. Samples were centrifuged (4000 RPM, 4 °C) and frozen at −80 °C. Analysis was performed by a certified medical laboratory (Labor Limbach, Heidelberg, Germany) using liquid chromatography mass spectrometry. A within-subject average was calculated and used for partial correlation between ketamine and norketamine levels and DLPFC-HC connectivity (peak voxel, adjusted for order effects).
Pharmacokinetics—animals
At the end of each experiment (within 50–80 min after ketamine/vehicle injection) a 4.5–6 ml blood sample was acquired from each rat by cardiac puncture to determine exposure to ketamine and levels of its major metabolite norketamine. Sample analysis was carried out using a mass spectrometry assay by Advion Bioanalytical Labs (Quintiles Company, Indianapolis, IN, USA).
Results
Human pharmacological rs-fMRI
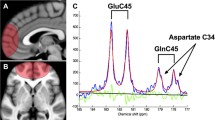
Relative to the placebo condition, ketamine significantly increased the correlation between both the left and right DLPFC and the left hippocampus (T = 3.69, P FWE = 0.027, corrected for left hippocampal ROI, local maximum: x = −30, y = −30, z = −14; T = 3.97, P FWE = 0.013, corrected for left hippocampal ROI, local maximum: x = −26, y = −10, z = −22; Table 1, Figs. 1 and 2). In contrast, there was no significant effect of ketamine on the coupling of the left DLPFC and either the left or right hippocampus (P FWE > 0.05, ROI-corrected).
Connectivity between left (upper row) and right (lower row) seed eigenvariate time course extracted from left/right DLPFC. Coronal (left) and transversal (right) slices showing maximum increase in the connectivity between the left (top) and right (bottom) dorsolateral prefrontal cortex (DLPFC) and the left hippocampus. Maximum increase for the left DLPFC connectivity was T = 3.97 (MNI coordinate [−26, −10, −22] mm) and for the right DLPFC T = 3.69 (MNI coordinate [−30, −30, −14] mm). The results were calculated using a hippocampal mask. The color bar depicts T-values
Barplot of correlation coefficients between left/right DLPFC and left hippocampus after placebo and ketamine application. The y-axis presents Pearson’s correlation coefficient from the hippocampal peak voxel. Left side, connectivity between left DLPFC and right hippocampus; right side, connectivity between right DLPFC and left hippocampus
The concentration of ketamine was 543.78 ng/ml (SD = 391.59 ng/ml) and of norketamine 44.61 ng/ml (SD = 20.35 ng/ml) in the first blood sample. The second blood sample contained 170.66 ng/ml of ketamine (SD = 133.17 ng/ml) and 41.46 ng/ml of norketamine (SD = 14.58 ng/ml). For correlations between plasma levels, we used the within-subject average (ketamine 364.88 ng/ml, SD = 228.48 ng/ml; norketamine 43.24 ng/ml, SD = 16.1 ng/ml). No statistically significant correlations were observed between plasma levels of either ketamine or norketamine and connectivity between DLPFC and hippocampus at the peak voxels (P > 0.19).
Animal pharmacological rs-fMRI
Ketamine significantly elevated the correlation between the left PrL and both the right and left hippocampus, as well as between the right PrL and left hippocampus (Table 2, Figs. 3 and 4). However, there was no significant effect between the right PrL and right hippocampus.
Coronal (left) and transversal (right) slices showing maximum increase in the connectivity between the left prelimbic cortex (PrL) and the right hippocampus (upper row), and the right prelimbic cortex and the left hippocampus (lower row). The results were calculated using a hippocampal mask. The color bar depicts T-values
Barplot of correlation coefficients between left/right prelimbic cortex (PrL) and right/left hippocampus, respectively, after vehicle and ketamine. The y-axis presents Pearson’s correlation coefficient calculated for the mean time courses from hippocampal clusters surviving FWE correction. Left side, connectivity between left PrL and right hippocampus; right side, connectivity between right PrL and left hippocampus
Measured plasma levels of ketamine and norketamine in the ketamine group were 1693.87 ng/ml (SD = 475.92 ng/ml) and 1333.01 ng/ml (SD = 585.78 ng/ml), respectively. Plasma levels of the major metabolite, norketamine, were highly correlated with ketamine levels (r = 0.712). No statistically significant correlations were observed between plasma levels of either ketamine or norketamine and connectivity between left PrL and right hippocampus (where we observed the strongest ketamine effect) at the cluster surviving family-wise error (FWE) correction (P = 0.215 for ketamine; P = 0.241 for norketamine), as well as connectivity between right PrL and left hippocampus at the cluster surviving FWE correction (P = 0.106 for ketamine; P = 0.476 for norketamine).
Discussion
In our rs-fMRI analysis, both humans and rats showed hyperconnectivity between the PFC and the hippocampus after the acute ketamine challenge. In rats, this was found for both left and right hippocampi, whereas in humans, only for the left hippocampus. Our findings indicate that despite the differences in brain anatomy and some details in the protocol, there is a robust cross-species effect of enhanced PFC-HC coupling in response to ketamine. These data add evidence to the utility of functional imaging as a translational biomarker, and builds on other recent findings in which similar cross-species BOLD pharmaco-fMRI amplitude changes were observed (Becerra et al. 2013).
The observed increase in PFC-HC coupling might reflect the neuromodulatory effect of ketamine on this network. NMDA antagonists increase the levels of excitatory neurotransmitters, such as glutamate, acetylcholine, and histamine and disinhibit GABAergic interneurons (Olney and Farber 1995). In a recent study, mice treated with a high dose of ketamine (30 mg/kg) showed a global increase in graph-theory-based connectivity measures (degree and mean clustering coefficient), as well as an increase in thalamo-cortical and cortical-subcortical (PFC to dorsal raphe nuclei and locus coeruleus) connectivity (Dawson et al. 2014). In this study, the authors did not provide specific data on PFC-HC coupling. Nevertheless, the general direction of the ketamine effect on these networks fits well with our data.
Ketamine induces an increase in glucose utilization in the hippocampus (Crosby et al. 1982; Nelson et al. 1980) and cingulate regions (Crosby et al. 1982), as well as regional cerebral blood flow in the hippocampus and cerebral cortex (Burdett et al. 1995). This might provide a neuronal underpinning for our findings. Also, there is a strong correlation between gamma band oscillations and BOLD connectivity in humans (Tagliazucchi et al. 2012). Ketamine consistently increases gamma oscillations both in humans (Hong et al. 2010) and in rats (Kittelberger et al. 2012; Phillips et al. 2012; Pinault 2008), which most likely results from the blockade of NMDA receptors at GABAergic interneurons.
Hippocampal and prefrontal pathophysiology
Both in rats and humans, the increase in connectivity after ketamine was more pronounced in the dorsal portion of the hippocampus. This is in accordance with the higher expression of NMDA receptors in the dorsal hippocampus along a ventral-dorsal axis in both species (Strange et al. 2014). In rats, ketamine has been recently shown (Moran et al. 2015) to suppress the drive from the medial prefrontal cortex (mPFC) to dorsal CA1 (dCA1) through NMDA receptors, while enhancing dCA1-to-mPFC drive through AMPA receptors, which for our study could imply that the direction for the observed increase in coupling came from the dorsal hippocampus, via subiculum outputs. In this respect, we have also accumulated substantial evidence that PFC-HC drive is mediated via AMPA receptors mediating long-term potentiation (LTP). Stress inhibits LTP in this circuit via AMPA receptor phosphorylation (Qi et al. 2009; Rocher et al. 2004; Spedding et al. 2003; Svenningsson et al. 2007). This occurs due to increased AMPA receptor mobility by corticosterone, reducing AMPA synaptic dwell time, which correlates with reduced LTP. These effects can be reversed by the antidepressant tianeptine (Zhang et al. 2013). Ketamine also blocks LTP in this circuit. Indeed, as the dorsal hippocampus mediates cognitive and spatial processing functions, this could partially explain the cognitive impairment observed after acute administration of ketamine.
Both postmortem and neuroimaging studies reveal disrupted hippocampal function in schizophrenic patients (Heckers and Konradi 2014; Konradi et al. 2011; Schobel et al. 2013). This might underlie abnormal recruitment of hippocampal circuits during cognitive tasks (Meyer-Lindenberg et al. 2001; Suazo et al. 2013). As schizophrenia is most often discussed in the context of dopamine dysregulation, it has to be noted that the rat equivalent of the primate anterior hippocampus regulates the activity of striatal dopaminergic neurons (Floresco et al. 2001). Our ketamine challenge in humans was not designed to induce psychotic effects per se. Our participants experienced mild perceptual changes, nausea, and dissociation (Table S1). These side effects were almost exactly the same as previously described for the same infusion protocol (Zarate et al. 2012).
Therefore, the subanesthetic ketamine administration used in humans in the present study probably has more relevance to the cognitive deficits associated with disorders such as schizophrenia, rather than plain psychosis.
In a previous paper, we considered the PFC-HC system and its functional connectivity in the rat and discussed at length the homology (and the limitations of the homology) with humans (Schwarz et al. 2013). For example, we found that in the rat, the posterior (subiculum) region of the hippocampal formation correlates more strongly with the mPFC than the anterior dorsal hippocampus, and that a homologous relationship exists in human. This dominant posterior hippocampal-prefrontal connectivity is consistent with the anatomical connectivity. Since the human PFC is much larger and more differentiated than that in the rat, in the present study we selected the DLPFC as a region of the human cortex that has been previously demonstrated as exhibiting aberrant functional connectivity with the hippocampus in disease and at-risk states (Esslinger et al. 2009; Meyer-Lindenberg et al. 2005). Since granular prefrontal cortex (including DLPFC) appeared during primate evolution, the rat brain lacks a granular cortex, thus making it difficult to confidently establish an area homologous the primate DLPFC (Preuss 1995; Uylings et al. 2003). The closest homolog of human DLPFC in rats is the PrL in terms of anatomical connections and electrophysiological and computational properties (Seamans et al. 2008). Functional aspects like spatial delay reaction and working memory typically recruit the human DLPFC and seem to be connected to the rat mPFC (Jung et al. 1998; Yang et al. 2014). The PrL plays a similar role in spatial working memory as the human DLPFC (Chudasama 2011; Kesner and Churchwell 2011). Taken together, from anatomical and functional perspective, the rat mPFC fuses elements of both the dorsal anterior cingulate cortex (Brodmann area 32) and the DLPFC (Seamans et al. 2008; Wise. 2008), making our seed regions comparable.
Hemispheric lateralization of the effects
We have found a lateralization of the response to ketamine in the left hippocampus in humans. Laterality was observed only in the hippocampus and not in the DLPFC. Reasons for the asymmetrical hippocampal response to ketamine could include asymmetries in NMDA/AMPA receptor density, subunit composition profile defining the functional properties of receptors, and expression of glutamate transporters. Also, the left and right hippocampi might not have equivalent connections to DLPFC. For example, a difference in the participation of the left and right hippocampi in episodic memory encoding is well-established (Igloi et al. 2010), with the right hippocampus providing place-learning navigation using environmental cues and the left hippocampus mediating self-navigation based on body movements.
Additionally, it is interesting to note that the left hippocampus seems to be more affected in schizophrenic patients, compared to the right: basal metabolic activity in the left hippocampus is increased in schizophrenia and predicts psychosis and positive symptom severity (Schobel et al. 2013). Also, hippocampal laterality in NMDA receptor distribution and function has been reported in schizophrenia with a left-sided loss of glutamate receptors (Harrison et al. 2003; Kerwin et al. 1988). Most importantly, both disease phenotype (Meyer-Lindenberg et al. 2005) and at-risk effects (Esslinger et al. 2009) have been observed to be left-lateralized with regard to the connectivity pattern.
In rats, both left and right hippocampi showed an increased coupling with the PrL. It is noteworthy that brain lateralization per se is not a characteristic unique only for humans. It has been found in several animal species including rats at morphological, functional, and biochemical levels (Glick and Ross 1981; Rogers 1989). For example, rats have left-right asymmetry in nigrostriatal regions as well as in the frontal cortex as indicated by difference in cortical thickness, effects of lesions and frontal cortical metabolism. The fact that, unlike in humans, both left and right hippocampi responded to ketamine could be due to a reduced laterality in terms of connections, NMDA/AMPA receptor profile and/or glutamate transporters. This proposal requires further investigation.
Apart from species effects on lateralization, asymmetries in ketamine response patterns have been described before. A study looking at ketamine effects in depressive patients found a decreased post-ketamine metabolism (as measured by glucose-PET) in the right DLPFC and increased in the left parahippocampal region. Ketamine gives rise to a hyperconnectivity between the hippocampus and cingulate cortex, as well as several other regions, similar to our results (Khalili-Mahani et al. 2015). The hippocampal hyperconnectivity might be linked to a hypoperfusion of the hippocampus as has been shown by using arterial spin labeling (Khalili-Mahani et al. 2015).
Differences between human and rat experiments
An important difference between the human and rat experiments was a requirement for anesthesia during rat fMRI. However, under medetomidine, a sedative alpha-2 adrenergic agonist, we obtained robust functional connectivity patterns in the PFC-HC circuit in the rat that closely reflect known anatomical connectivity and are comparable to those in humans (Schwarz et al. 2013); this may reflect the fact that medetomidine does not strongly interfere with neural activity (Williams et al. 2010). Also, an anesthetized rat brain still preserves global network properties of the awake brain (in terms of graph theory: global clustering coefficient, mean shortest path length, small-worldness, and modularity) (Liang et al. 2012). Also, for medetomidine, there is no evidence for specific mPFC-HC connectivity effects (Grandjean et al. 2014).
In this study, the human subjects had lower plasma levels of ketamine than the rats, reflecting the lower dose administered. Lower ketamine doses in rats (5 and 10 mg/kg) were additionally tested using identical analytical procedures as applied to the 25 mg/kg group, but they did not produce any significant effects on PrL-hippocampal connectivity (data not shown). Thus, it seems that a higher exposure of ketamine is required in the rat to reach an effect comparable to that observed in humans. However, it should be noted that in rats, ketamine was administered as one-time subcutaneous injection, while this procedure is not possible in humans, and conversely, it was not practicable to administer ketamine to the rats in a long intravenous application via an infusion pump. The human participants received a lower dose but in a continuous way, a standard procedure established in clinical trials of ketamine in depression. While we cannot quantitatively align the human and rat exposure-response relationships, the ketamine-induced hyperconnectivity in both species was comparable at different, species-specific, dose and exposure levels.
Whereas humans received racemic ketamine (mixture of S(+) and R(−) enantiomers) according to a well-established protocol (Salvadore et al. 2010), rats received S-ketamine, the S(+)-enantiomer of ketamine which is discussed as the main compound responsible for the NMDA-antagonistic effect. As both R- and S-ketamine exhibit a voltage- and use-dependent blockade of NMDA receptor currents in cell culture (Zeilhofer et al. 1992), there is no evidence of a strong difference between the effect of racemic or S-ketamine. Nevertheless, a direct analogy between pharmacokinetics and pharmacodynamics in both species was not possible. Therefore, we are not able to make assumptions about quantitative cross-species differences. The lack of a significant exposure-response relationship in both species is likely due to the fact that only a single dose was administered. We have previously shown significant exposure-response relationships for functional connectivity measures in the rat when modeling over a wide range of doses and exposures (Gass et al. 2014).
Comparison with schizophrenia
The directionality of the effect we observed (increased functional coupling) stands in contrast to the observations of reduced PFC-HC coupling during resting-state in chronic schizophrenia (Rotarska-Jagiela et al. 2010; Zhou et al. 2008). We have recently suggested that ketamine effects rather resemble a hyperglutamatergic state and cognitive disruption as observed in prodromal stage of schizophrenia (Gass et al. 2014). Other papers have debated on the grounds of neurobiological findings whether hypofrontality or decreased thalamo-cortical connectivity as markers for schizophrenia are mirrored in the acute ketamine effect. For example, acute ketamine induces increased intra-PFC connectivity (reduced in schizophrenia), increased thalamo-cortical connectivity (reduced in schizophrenia), a general increase in number of connections (versus fewer connections in schizophrenia) and increased clustering coefficient (versus decreased mean clustering in schizophrenia) (Dawson et al. 2013, 2014; Gass et al. 2014; Liu et al. 2008; Lynall et al. 2010; Micheloyannis et al. 2006).
While it is attractive to discuss the PFC-HC connectivity as a marker for schizophrenia, we are aware of problems of an analogy to ketamine-induced psychosis. From a psychopathological perspective, ketamine captures psychosis only broadly, but when looking at the exact changes in mind states (Vollenweider and Kometer 2010), it certainly does not mirror symptoms seen in schizophrenia. Recent clinical observations corroborated that ketamine anesthesia does not induce acute exacerbation of schizophrenia, thus ketamine’s profile is unique (Corlett et al. 2011; Mion and Villevieille 2013), which makes it even more interesting than seeing it solely as a “psychosis model,” e.g., it would be interesting to study the amount of dissociation in dependence of cortical-subcortical coupling, something our own sample was too small to conduct.
Future questions
Several questions remain open for future studies. For example, what is the reason for the asymmetry of ketamine response? The spatiotemporally heterogeneous connectivity pattern in both humans and rats would be greatly informed by measuring local NMDA receptor density. Such a technique might be available with combined PET-fMRI and a specific NMDA receptor ligand. Also, what are the crossing steps in the transition from prodromal to chronic schizophrenia? While we did not assess these questions empirically, we encourage others to consider these issues in future research.
We would expect that due to abundant expression of NMDA receptors all over the brain, ketamine effects might also be observed in other regions and networks. Indeed, graph-theoretic-based approaches mapping the global connectivity of brain regions in humans (Driesen et al. 2013; Joules et al. 2015) suggest that increases in connectivity may not be limited to the PFC-HC network. However, these studies do not elucidate the links or circuits in which the connectivity is most strongly increased, and in future, it would be interesting to compare the strength of the ketamine effects between affected networks.
Conclusion
Overall, our data suggest that the systems-level alterations induced by ketamine treatment are comparable across species. In conjunction with previous pharmaco-fMRI studies in rats and humans, our results provide further evidence of the utility of fMRI across species as a translational tool in neuroscience. Characterizing homologous mechanisms in humans and rats in this way may help in the development of novel treatment interventions by presenting both a translational biomarker and drug model. More specifically, our data elucidate ketamine-induced alterations in PFC-HC coupling, a phenotype often disrupted in pathological conditions, which may give clue to understanding of psychiatric disorders and their onset, and help in the development of new treatments.
References
Becerra L, Upadhyay J, Chang PC, Bishop J, Anderson J, Baumgartner R, Schwarz AJ, Coimbra A, Wallin D, Nutile L, George E, Maier G, Sunkaraneni S, Iyengar S, Evelhoch JL, Bleakman D, Hargreaves R, Borsook D (2013) Parallel buprenorphine phMRI responses in conscious rodents and healthy human subjects. J Pharmacol Exp Ther 345:41–51. doi:10.1124/jpet.112.201145
Behzadi Y, Restom K, Liau J, Liu TT (2007) A component based noise correction method (CompCor) for BOLD and perfusion based fMRI. Neuroimage 37:90–101
Burdett NG, Menon DK, Carpenter TA, Jones JG, Hall LD (1995) Visualisation of changes in regional cerebral blood flow (rCBF) produced by ketamine using long TE gradient-echo sequences: preliminary results. Magn Reson Imaging 13:549–553
Callicott JH, Egan MF, Mattay VS, Bertolino A, Bone AD, Verchinksi B, Weinberger DR (2003) Abnormal fMRI response of the dorsolateral prefrontal cortex in cognitively intact siblings of patients with schizophrenia. Am J Psychiatry 160:709–719
Chai XJ, Ofen N, Gabrieli JD, Whitfield-Gabrieli S (2014) Selective development of anticorrelated networks in the intrinsic functional organization of the human brain. J Cogn Neurosci 26:501–513. doi:10.1162/jocn_a_00517
Chudasama Y (2011) Animal models of prefrontal-executive function. Behav Neurosci 125:327–343. doi:10.1037/a0023766
Corlett PR, Honey GD, Krystal JH, Fletcher PC (2011) Glutamatergic model psychoses: prediction error, learning, and inference. Neuropsychopharmacology 36:294–315. doi:10.1038/npp.2010.163
Crosby G, Crane AM, Sokoloff L (1982) Local changes in cerebral glucose utilization during ketamine anesthesia. Anesthesiology 56:437–443
D’Souza DC, Singh N, Elander J, Carbuto M, Pittman B, Udo de Haes J, Sjogren M, Peeters P, Ranganathan M, Schipper J (2012) Glycine transporter inhibitor attenuates the psychotomimetic effects of ketamine in healthy males: preliminary evidence. Neuropsychopharmacology 37:1036–1046. doi:10.1038/npp.2011.295
Dawson N, Morris BJ, Pratt JA (2013) Subanaesthetic ketamine treatment alters prefrontal cortex connectivity with thalamus and ascending subcortical systems. Schizophr Bull 39:366–377. doi:10.1093/schbul/sbr144; 10.1093/schbul/sbr144
Dawson N, McDonald M, Higham DJ, Morris BJ, Pratt JA (2014) Subanesthetic ketamine treatment promotes abnormal interactions between neural subsystems and alters the properties of functional brain networks. Neuropsychopharmacology 39:1786–1798. doi:10.1038/npp.2014.26
Diamond PR, Farmery AD, Atkinson S, Haldar J, Williams N, Cowen PJ, Geddes JR, McShane R (2014) Ketamine infusions for treatment resistant depression: a series of 28 patients treated weekly or twice weekly in an ECT clinic. J Psychopharmacol 28:536–544
Driesen NR, McCarthy G, Bhagwagar Z, Bloch M, Calhoun V, D’Souza DC, Gueorguieva R, He G, Ramachandran R, Suckow RF, Anticevic A, Morgan PT, Krystal JH (2013) Relationship of resting brain hyperconnectivity and schizophrenia-like symptoms produced by the NMDA receptor antagonist ketamine in humans. Mol Psychiatry. doi:10.1038/mp.2012.194
Esslinger C, Walter H, Kirsch P, Erk S, Schnell K, Arnold C, Haddad L, Mier D, Opitz von Boberfeld C, Raab K, Witt SH, Rietschel M, Cichon S, Meyer-Lindenberg A (2009) Neural mechanisms of a genome-wide supported psychosis variant. Science 324:605. doi:10.1126/science.1167768
Floresco SB, Todd CL, Grace AA (2001) Glutamatergic afferents from the hippocampus to the nucleus accumbens regulate activity of ventral tegmental area dopamine neurons. J Neurosci 21:4915–4922
Furey ML, Khanna A, Hoffman EM, Drevets WC (2010) Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology 35:2479–2488. doi:10.1038/npp.2010.131
Garcia LS, Comim CM, Valvassori SS, Reus GZ, Andreazza AC, Stertz L, Fries GR, Gavioli EC, Kapczinski F, Quevedo J (2008) Chronic administration of ketamine elicits antidepressant-like effects in rats without affecting hippocampal brain-derived neurotrophic factor protein levels. Basic Clin Pharmacol Toxicol 103:502–506. doi:10.1111/j.1742-7843.2008.00210.x
Gass N, Schwarz AJ, Sartorius A, Schenker E, Risterucci C, Spedding M, Zheng L, Meyer-Lindenberg A, Weber-Fahr W (2014) Sub-anesthetic ketamine modulates intrinsic BOLD connectivity within the hippocampal-prefrontal circuit in the rat. Neuropsychopharmacology 39:895–906. doi:10.1038/npp.2013.290
Glick SD, Ross DA (1981) Lateralization of function in the rat brain. Trends Neurosci. 4:196–199
Godsil BP, Kiss JP, Spedding M, Jay TM (2013) The hippocampal-prefrontal pathway: the weak link in psychiatric disorders? Eur Neuropsychopharmacol. doi:10.1016/j.euroneuro.2012.10.018
Grandjean J, Schroeter A, Batata I, Rudin M (2014) Optimization of anesthesia protocol for resting-state fMRI in mice based on differential effects of anesthetics on functional connectivity patterns. Neuroimage 102(Pt 2):838–847. doi:10.1016/j.neuroimage.2014.08.043
Harrison PJ, Law AJ, Eastwood SL (2003) Glutamate receptors and transporters in the hippocampus in schizophrenia. Ann N Y Acad Sci 1003:94–101
Heckers S, Konradi C (2014) GABAergic mechanisms of hippocampal hyperactivity in schizophrenia. Schizophr Res. doi:10.1016/j.schres.2014.09.041
Hong LE, Summerfelt A, Buchanan RW, O’Donnell P, Thaker GK, Weiler MA, Lahti AC (2010) Gamma and delta neural oscillations and association with clinical symptoms under subanesthetic ketamine. Neuropsychopharmacology 35:632–640. doi:10.1038/npp.2009.168
Igloi K, Doeller CF, Berthoz A, Rondi-Reig L, Burgess N (2010) Lateralized human hippocampal activity predicts navigation based on sequence or place memory. Proc Natl Acad Sci U S A 107:14466–14471. doi:10.1073/pnas.1004243107
Joules R, Doyle OM, Schwarz AJ, O’Daly OG, Brammer M, Williams SC, Mehta MA (2015) Ketamine induces a robust whole-brain connectivity pattern that can be differentially modulated by drugs of different mechanism and clinical profile. Psychopharmacology (Berl). doi:10.1007/s00213-015-3951-9
Jung MW, Qin Y, McNaughton BL, Barnes CA (1998) Firing characteristics of deep layer neurons in prefrontal cortex in rats performing spatial working memory tasks. Cereb Cortex 8:437–450
Kerwin RW, Patel S, Meldrum BS, Czudek C, Reynolds GP (1988) Asymmetrical loss of glutamate receptor subtype in left hippocampus in schizophrenia. Lancet 1:583–584
Kesner RP, Churchwell JC (2011) An analysis of rat prefrontal cortex in mediating executive function. Neurobiol Learn Mem 96:417–431. doi:10.1016/j.nlm.2011.07.002
Khalili-Mahani N, Niesters M, van Osch MJ, Oitzl M, Veer I, de Rooij M, van Gerven J, van Buchem MA, Beckmann CF, Rombouts SA, Dahan A (2015) Ketamine interactions with biomarkers of stress: a randomized placebo-controlled repeated measures resting-state fMRI and PCASL pilot study in healthy men. Neuroimage 108:396–409. doi:10.1016/j.neuroimage.2014.12.050
Kittelberger K, Hur EE, Sazegar S, Keshavan V, Kocsis B (2012) Comparison of the effects of acute and chronic administration of ketamine on hippocampal oscillations: relevance for the NMDA receptor hypofunction model of schizophrenia. Brain Struct Funct 217:395–409. doi:10.1007/s00429-011-0351-8
Konradi C, Yang CK, Zimmerman EI, Lohmann KM, Gresch P, Pantazopoulos H, Berretta S, Heckers S (2011) Hippocampal interneurons are abnormal in schizophrenia. Schizophr Res 131:165–173. doi:10.1016/j.schres.2011.06.007
Krystal JH, Abi-Saab W, Perry E, D’Souza DC, Liu N, Gueorguieva R, McDougall L, Hunsberger T, Belger A, Levine L, Breier A (2005) Preliminary evidence of attenuation of the disruptive effects of the NMDA glutamate receptor antagonist, ketamine, on working memory by pretreatment with the group II metabotropic glutamate receptor agonist, LY354740, in healthy human subjects. Psychopharmacology (Berl) 179:303–309. doi:10.1007/s00213-004-1982-8
Liang Z, King J, Zhang N (2012) Intrinsic organization of the anesthetized brain. J Neurosci 32:10191. doi:10.1523/JNEUROSCI.1020-12.2012
Liu Y, Liang M, Zhou Y, He Y, Hao Y, Song M, Yu C, Liu H, Liu Z, Jiang T (2008) Disrupted small-world networks in schizophrenia. Brain 131:945–961. doi:10.1093/brain/awn018
Lorrain DS, Baccei CS, Bristow LJ, Anderson JJ, Varney MA (2003) Effects of ketamine and N-methyl-D-aspartate on glutamate and dopamine release in the rat prefrontal cortex: modulation by a group II selective metabotropic glutamate receptor agonist LY379268. Neuroscience 117:697–706
Lynall ME, Bassett DS, Kerwin R, McKenna PJ, Kitzbichler M, Muller U, Bullmore E (2010) Functional connectivity and brain networks in schizophrenia. J Neurosci 30:9477–9487. doi:10.1523/JNEUROSCI.0333-10.2010
Meyer-Lindenberg A, Poline JB, Kohn PD, Holt JL, Egan MF, Weinberger DR, Berman KF (2001) Evidence for abnormal cortical functional connectivity during working memory in schizophrenia. Am J Psychiatry 158:1809–1817
Meyer-Lindenberg AS, Olsen RK, Kohn PD, Brown T, Egan MF, Weinberger DR, Berman KF (2005) Regionally specific disturbance of dorsolateral prefrontal-hippocampal functional connectivity in schizophrenia. Arch Gen Psychiatry 62:379–386. doi:10.1001/archpsyc.62.4.379
Micheloyannis S, Pachou E, Stam CJ, Breakspear M, Bitsios P, Vourkas M, Erimaki S, Zervakis M (2006) Small-world networks and disturbed functional connectivity in schizophrenia. Schizophr Res 87:60–66
Mion G, Villevieille T (2013) Ketamine pharmacology: an update (pharmacodynamics and molecular aspects, recent findings). CNS Neurosci Ther 19:370–380. doi:10.1111/cns.12099
Moghaddam B, Adams B, Verma A, Daly D (1997) Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17:2921–2927
Moran RJ, Jones MW, Blockeel AJ, Adams RA, Stephan KE, Friston KJ (2015) Losing control under ketamine: suppressed cortico-hippocampal drive following acute ketamine in rats. Neuropsychopharmacology 40:268–277. doi:10.1038/npp.2014.184
Morgan CJ, Mofeez A, Brandner B, Bromley L, Curran HV (2004) Ketamine impairs response inhibition and is positively reinforcing in healthy volunteers: a dose-response study. Psychopharmacology (Berl) 172:298–308. doi:10.1007/s00213-003-1656-y
Nelson SR, Howard RB, Cross RS, Samson F (1980) Ketamine-induced changes in regional glucose utilization in the rat brain. Anesthesiology 52:330–334
Niciu MJ, Luckenbaugh DA, Ionescu DF, Richards EM, Vande Voort JL, Ballard ED, Brutsche NE, Furey ML, Zarate CA, Jr (2014) Ketamine’s antidepressant efficacy is extended for at least four weeks in subjects with a family history of an alcohol use disorder. Int J Neuropsychopharmacol 18:doi: 10.1093/ijnp/pyu039
Olney JW, Farber NB (1995) NMDA antagonists as neurotherapeutic drugs, psychotogens, neurotoxins, and research tools for studying schizophrenia. Neuropsychopharmacology 13:335–345. doi:10.1016/0893-133X(95)00079-S
Phillips KG, Cotel MC, McCarthy AP, Edgar DM, Tricklebank M, O’Neill MJ, Jones MW, Wafford KA (2012) Differential effects of NMDA antagonists on high frequency and gamma EEG oscillations in a neurodevelopmental model of schizophrenia. Neuropharmacology 62:1359–1370. doi:10.1016/j.neuropharm.2011.04.006
Pinault D (2008) N-methyl d-aspartate receptor antagonists ketamine and MK-801 induce wake-related aberrant gamma oscillations in the rat neocortex. Biol Psychiatry 63:730–735. doi:10.1016/j.biopsych.2007.10.006
Pitsikas N, Boultadakis A, Sakellaridis N (2008) Effects of sub-anesthetic doses of ketamine on rats’ spatial and non-spatial recognition memory. Neuroscience 154:454–460. doi:10.1016/j.neuroscience.2008.04.001
Preuss TM (1995) Do rats have prefrontal cortex? The rose-woolsey-akert program reconsidered. J Cogn Neurosci 7:1–24. doi:10.1162/jocn.1995.7.1.1
Qi H, Mailliet F, Spedding M, Rocher C, Zhang X, Delagrange P, McEwen B, Jay TM, Svenningsson P (2009) Antidepressants reverse the attenuation of the neurotrophic MEK/MAPK cascade in frontal cortex by elevated platform stress; reversal of effects on LTP is associated with GluA1 phosphorylation. Neuropharmacology 56:37–46. doi:10.1016/j.neuropharm.2008.06.068
Rasetti R, Sambataro F, Chen Q, Callicott JH, Mattay VS, Weinberger DR (2011) Altered cortical network dynamics: a potential intermediate phenotype for schizophrenia and association with ZNF804A. Arch Gen Psychiatry 68:1207–1217. doi:10.1001/archgenpsychiatry.2011.103
Rocher C, Spedding M, Munoz C, Jay TM (2004) Acute stress-induced changes in hippocampal/prefrontal circuits in rats: effects of antidepressants. Cereb Cortex 14:224–229
Rogers LJ (1989) Laterality in animals. Int J Comp Psychol 3(1):5–25
Rotarska-Jagiela A, van de Ven V, Oertel-Knochel V, Uhlhaas PJ, Vogeley K, Linden DE (2010) Resting-state functional network correlates of psychotic symptoms in schizophrenia. Schizophr Res 117:21–30. doi:10.1016/j.schres.2010.01.001
Rowland LM, Bustillo JR, Mullins PG, Jung RE, Lenroot R, Landgraf E, Barrow R, Yeo R, Lauriello J, Brooks WM (2005) Effects of ketamine on anterior cingulate glutamate metabolism in healthy humans: a 4-T proton MRS study. Am J Psychiatry 162:394–396
Salvadore G, Cornwell BR, Sambataro F, Latov D, Colon-Rosario V, Carver F, Holroyd T, DiazGranados N, Machado-Vieira R, Grillon C, Drevets WC, Zarate CA Jr (2010) Anterior cingulate desynchronization and functional connectivity with the amygdala during a working memory task predict rapid antidepressant response to ketamine. Neuropsychopharmacology 35:1415–1422. doi:10.1038/npp.2010.24
Scheidegger M, Walter M, Lehmann M, Metzger C, Grimm S, Boeker H, Boesiger P, Henning A, Seifritz E (2012) Ketamine decreases resting state functional network connectivity in healthy subjects: implications for antidepressant drug action. PLoS One 7:e44799. doi:10.1371/journal.pone.0044799
Schobel SA, Chaudhury NH, Khan UA, Paniagua B, Styner MA, Asllani I, Inbar BP, Corcoran CM, Lieberman JA, Moore H, Small SA (2013) Imaging patients with psychosis and a mouse model establishes a spreading pattern of hippocampal dysfunction and implicates glutamate as a driver. Neuron 78:81–93. doi:10.1016/j.neuron.2013.02.011
Schwarz AJ, Danckaert A, Reese T, Gozzi A, Paxinos G, Watson C, Merlo-Pich EV, Bifone A (2006) A stereotaxic MRI template set for the rat brain with tissue class distribution maps and co-registered anatomical atlas: application to pharmacological MRI. Neuroimage 32:538–550
Schwarz AJ, Gass N, Sartorius A, Zheng L, Spedding M, Schenker E, Risterucci C, Meyer-Lindenberg A, Weber-Fahr W (2013) The low-frequency blood oxygenation level-dependent functional connectivity signature of the hippocampal-prefrontal network in the rat brain. Neuroscience 228:243–258. doi:10.1016/j. neuroscience .2012.10.032
Seamans JK, Lapish CC, Durstewitz D (2008) Comparing the prefrontal cortex of rats and primates: insights from electrophysiology. Neurotox Res 14:249–262. doi:10.1007/BF03033814
Seidman LJ, Thermenos HW, Poldrack RA, Peace NK, Koch JK, Faraone SV, Tsuang MT (2006) Altered brain activation in dorsolateral prefrontal cortex in adolescents and young adults at genetic risk for schizophrenia: an fMRI study of working memory. Schizophr Res 85:58–72
Skoblenick K, Everling S (2012) NMDA antagonist ketamine reduces task selectivity in macaque dorsolateral prefrontal neurons and impairs performance of randomly interleaved prosaccades and antisaccades. J Neurosci 32:12018–12027. doi:10.1523/JNEUROSCI.1510-12.2012
Spedding M, Neau I, Harsing L (2003) Brain plasticity and pathology in psychiatric disease: sites of action for potential therapy. Curr Opin Pharmacol 3:33–40
Stone JM, Dietrich C, Edden R, Mehta MA, De Simoni S, Reed LJ, Krystal JH, Nutt D, Barker GJ (2012) Ketamine effects on brain GABA and glutamate levels with 1H-MRS: relationship to ketamine-induced psychopathology. Mol Psychiatry 17:664–665. doi:10.1038/mp.2011.171
Strange BA, Witter MP, Lein ES, Moser EI (2014) Functional organization of the hippocampal longitudinal axis. Nat Rev Neurosci 15:655–669. doi:10.1038/nrn3785
Suazo V, Diez A, Tamayo P, Montes C, Molina V (2013) Limbic hyperactivity associated to verbal memory deficit in schizophrenia. J Psychiatr Res 47:843–850. doi:10.1016/j.jpsychires.2013.02.007
Svenningsson P, Bateup H, Qi H, Takamiya K, Huganir RL, Spedding M, Roth BL, McEwen BS, Greengard P (2007) Involvement of AMPA receptor phosphorylation in antidepressant actions with special reference to tianeptine. Eur J Neurosci 26:3509–3517
Tagliazucchi E, von Wegner F, Morzelewski A, Brodbeck V, Laufs H (2012) Dynamic BOLD functional connectivity in humans and its electrophysiological correlates. Front Hum Neurosci 6:339. doi:10.3389/fnhum.2012.00339
Uylings HB, Groenewegen HJ, Kolb B (2003) Do rats have a prefrontal cortex? Behav Brain Res 146:3–17
van Buuren M, Gladwin TE, Zandbelt BB, van den Heuvel M, Ramsey NF, Kahn RS, Vink M (2009) Cardiorespiratory effects on default-mode network activity as measured with fMRI. Hum Brain Mapp 30:3031–3042. doi:10.1002/hbm.20729
Vollenweider FX, Kometer M (2010) The neurobiology of psychedelic drugs: implications for the treatment of mood disorders. Nat Rev Neurosci 11:642–651. doi:10.1038/nrn2884
Vollenweider FX, Leenders KL, Scharfetter C, Antonini A, Maguire P, Missimer J, Angst J (1997) Metabolic hyperfrontality and psychopathology in the ketamine model of psychosis using positron emission tomography (PET) and [18F]fluorodeoxyglucose (FDG). Eur Neuropsychopharmacol 7:9–24
Whitfield-Gabrieli S, Nieto-Castanon A (2012) Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect 2:125–141. doi:10.1089/brain.2012.0073
Williams KA, Magnuson M, Majeed W, LaConte SM, Peltier SJ, Hu X, Keilholz SD (2010) Comparison of alpha-chloralose, medetomidine and isoflurane anesthesia for functional connectivity mapping in the rat. Magn Reson Imaging 28:995–1003. doi:10.1016/j.mri.2010.03.007
Wise SP (2008) Forward frontal fields: phylogeny and fundamental function. Trends Neurosci 31:599–608. doi:10.1016/j.tins.2008.08.008
Yang ST, Shi Y, Wang Q, Peng JY, Li BM (2014) Neuronal representation of working memory in the medial prefrontal cortex of rats. Mol Brain 7:61. doi:10.1186/s13041-014-0061-2
Zarate CA Jr, Brutsche N, Laje G, Luckenbaugh DA, Venkata SL, Ramamoorthy A, Moaddel R, Wainer IW (2012) Relationship of ketamine's plasma metabolites with response, diagnosis, and side effects in major depression. Biol Psychiatry 72:331–338. doi:10.1016/j.biopsych.2012.03.004
Zarate CA Jr, Mathews DC, Furey ML (2013) Human biomarkers of rapid antidepressant effects. Biol Psychiatry 73:1142–1155. doi:10.1016/j.biopsych.2012.11.031
Zeilhofer HU, Swandulla D, Geisslinger G, Brune K (1992) Differential effects of ketamine enantiomers on NMDA receptor currents in cultured neurons. Eur J Pharmacol 213:155–158
Zhang H, Etherington LA, Hafner AS, Belelli D, Coussen F, Delagrange P, Chaouloff F, Spedding M, Lambert JJ, Choquet D, Groc L (2013) Regulation of AMPA receptor surface trafficking and synaptic plasticity by a cognitive enhancer and antidepressant molecule. Mol Psychiatry 18:471–484. doi:10.1038/mp.2012.80
Zhou Y, Shu N, Liu Y, Song M, Hao Y, Liu H, Yu C, Liu Z, Jiang T (2008) Altered resting-state functional connectivity and anatomical connectivity of hippocampus in schizophrenia. Schizophr Res 100:120–132. doi:10.1016/j.schres.2007.11.039
Acknowledgments
The authors thank Felix Hörner and Claudia Falfan-Melgoza for their excellent technical assistance.
Conflict of interest
NEWMEDS—the research leading to these results, has received support from the Innovative Medicine Initiative Joint Undertaking under Grant Agreement No. 115008 of which resources are composed of the European Federation of Pharmaceutical Industries and Associations (EFPIA) in-kind contribution and financial contribution from the European Union’s Seventh Framework Program (FP7/2007–2013). Also the work was supported by the BMBF (01EW1110) in the frame of ERA-Net NEURON. AJS is an employee and shareholder of Eli Lilly and Company; ES is an employee of Instituts de Recherches Servier; MS is an employee of Spedding Research Solutions; and CR is an employee of F. Hoffman-La Roche.
Author information
Authors and Affiliations
Corresponding author
Additional information
Oliver Grimm and Natalia Gass shared first authorship.
Adam J. Schwarz and Andreas Meyer-Lindenberg shared last authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table S1
(DOC 26 kb)
Rights and permissions
About this article
Cite this article
Grimm, O., Gass, N., Weber-Fahr, W. et al. Acute ketamine challenge increases resting state prefrontal-hippocampal connectivity in both humans and rats. Psychopharmacology 232, 4231–4241 (2015). https://doi.org/10.1007/s00213-015-4022-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-015-4022-y