Abstract
Substantial evidence exists that diabetes mellitus is associated with an increased risk of osteoporotic fractures. Low bone strength as well as bone extrinsic factors are probably contributing to the increased bone fragility in diabetes. Bone density and quality are important determinants of bone strength. Although bone mineral density (BMD) and the fracture risk assessment tool (FRAX) are very useful clinical tools in assessing bone strength, they may underestimate the fracture risk in diabetes mellitus. Through advances in new technologies such as trabecular bone score (TBS) and peripheral quantitative computed tomography (pQCT), we can better assess the bone quality and fracture risk of patients with diabetes mellitus. Invasive assessments such as microindentation and histomorphometry have been great complement to the existing bone analysis techniques. Bone turnover markers have been found to be altered in diabetes mellitus patients and may be associated with fractures. This review will give a brief summary of the current development and clinical uses of these assessments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a common disease throughout the world [1]. Diabetes-related complications, such as cardiovascular and renal diseases, are becoming a huge health care and financial burden [1]. Osteoporosis is a common skeletal disorder characterized by reduced bone strength predisposing to an increased risk of fracture, which results in pain, impaired function, reduced quality of life, institutionalization, and death [2]. A number of previous studies have revealed the association between diabetes mellitus and osteoporosis, and it is now well established that both type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) are associated with an increased risk of osteoporotic fractures [3,4,5].
The mechanisms underlying increased bone fragility in diabetes mellitus are complex. Low bone turnover, accumulation of advanced glycation endproducts (AGEs), micro- and macro-architecture abnormalities, and tissue material damage lead to abnormal biomechanical properties may contribute to the impaired bone fragility [6]. Other factors associated with bone fragility in patients with diabetes mellitus include inflammation response, oxidative stress, adipokine alterations, WNT dysregulation, and increased marrow fat [6]. Bone extrinsic factors, such as increased frequency of falls, a factor that is closely related to diabetic complications and treatment-induced hypoglycemia, also contribute to the increased fracture risk [6,7,8]. However, after being adjusted for fall frequency, diabetes remains an independent risk factor of increased fracture risk [9,10,11]. Therefore, low bone strength is probably contributing to the increased bone fragility in diabetes. Both bone density and quality are important factors in the determination of bone strength. Multiple methods have been used to assess bone quantity and bone quality of diabetes mellitus patients, including bone mineral density (BMD), trabecular bone score (TBS), quantitative computed tomography (QCT), bone histomorphometry, microindentation, and bone turnover markers. This review will give a brief summary of the current development and clinical uses of these assessments.
We conducted a literature search for English language articles that was published before Mar 15th, 2018 or earlier in the PubMed and Embase online using the following keywords in various combinations: “diabetes”, “diabetes mellitus”, “type 1 diabetes mellitus”, “type 2 diabetes mellitus”, “bone”, “fracture”, “fracture risk”, “skeletal fragility”, “osteoporosis”, “bone mass”, “structure”, “microarchitecture”, “bone quality”, “strength”, “turnover”, “dual x-ray absorptiometry”, “DXA”, “bone mineral density”, “BMD”, “Fracture Risk Assessment Tool”, “FRAX”, “trabecular bone score”, “TBS”, “quantitative computed tomography”, “QCT”, “peripheral quantitative computed tomography”, “pQCT”, “cortical”, “trabecular”, “histomorphometry”, “microindentation”, “cyclic microindentation”, “impact microindentation”, “bone turn over”, “turnover”, “mechanism”, “advanced glycation end-products”, “AGEs”, “insulin”. Approximately 100 relevant articles were reviewed to discuss the current evidence for the use of BMD, FRAX, TBS, QCT, bone histomorphometry, and microindentation in assessment of bone quality in patients with diabetes mellitus. Only publications in English were included.
BMD and FRAX
BMD measured by dual x-ray absorptiometry (DXA) is currently the gold standard for both osteoporosis diagnosis and the monitoring of treatment efficacy.
Research indicates that BMD is lower in patients with T1DM [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. A recent meta-analysis that includes 23 cross-sectional studies and 2 cohort studies shows a significant association between T1DM and decreased BMD values of total body with pooled mean differences of − 0.06 g/cm2 (95% CI − 0.11, − 0.01) [37].
However, patients with T2DM usually show BMD values above average [10, 33, 38,39,40,41,42,43,44,45,46,47,48,49,50]. A meta-analysis which is based on 15 observational studies (3437 T2DM patients and 19,139 control) shows that BMD in patients with T2DM is significantly higher with pooled mean differences of 0.04 g/cm2 (95% CI: 0.02, 0.05) at the femoral neck [51]. Therefore, T2DM may be associated with a reduction of bone quality, which cannot be reflected by BMD measurement.
Fracture risk assessment tool (FRAX) is widely used in estimating individualized 10-year probability of hip and major osteoporotic fracture. The FRAX algorithm consists of femoral neck BMD T-score, age, sex, weight, height, previous history of hip fracture, current smoking, recent use of corticosteroids, presence of rheumatoid arthritis, and ≥ 3 alcoholic beverages per day. FRAX is currently widely used for the estimation of fracture risk in patients with diabetes mellitus. In older patients with T2DM, both femoral neck BMD T-score and FRAX score are significantly related to hip and non-spine fracture risk [52].
Although BMD and FRAX are important in assessment of fracture risk, they are limited in application in patients with diabetes mellitus. As parameters related to diabetes mellitus are not included in FRAX, it may underestimate the fracture risk in specific population. In 2011, using data from three prospective observational studies, the Study of Osteoporotic Fractures, the Osteoporotic Fractures in Men study, and the Health, Aging and Body Composition Study, Schwartz et al. demonstrated that among older adults with T2DM, fracture risk was higher than those without diabetes even with similar BMD T-score and age or FRAX score [52]. For a given hip fracture risk, patients with T2DM have a 0.59 (95% CI, 0.31–0.87) higher T-score for women and 0.38 (95% CI, 0.09–0.66) for men [52]. Therefore, it is suggested that fragility fractures in diabetes mellitus may also be associated with diabetes-related changes in bone quality, which are not reflected in BMD. Although BMD and FRAX are very useful tools for the assessment of fracture risk in older adults, interpretation of T-score of FRAX score in patients with diabetes mellitus should be careful enough to take into account the higher fracture risk associated with diabetes [52].
TBS
TBS is a new texture parameter that analyzes pixel gray-level variations in the DXA image and reflects bone microarchitecture. As TBS is based on DXA, it can be widely accessible without introducing new equipment. A meta-analysis which includes individual-level data from 17,809 subjects in 14 prospective population-based cohorts shows that TBS can serve as a significant predictor of fracture risk independent of FRAX [53]. The gradient of risk (GR; hazard ratio per 1 SD change in risk variable in direction of increased risk) of TBS for major osteoporotic fracture is 1.44 (95% CI 1.35–1.53). When adjusted for FRAX 10-year probability of major osteoporotic fracture, TBS is still an independent predictor of fracture risk (GR = 1.32, 95% CI 1.24–1.41). Moreover, when the FRAX probability is adjusted for TBS, there is a slight increase in the GR (1.76, 95% 1.65–1.87 vs 1.70, 95% CI 1.60–1.81) [53]. The Manitoba BMD Cohort also demonstrated a small but significant improvement in overall net reclassification improvement (NRI) for all individual FRAX interventional criteria (range 0.007 to 0.018) and all three national clinical practice guidelines (CPGs) (range 0.008 to 0.011) [54]. Almost all of the improvement was found in individuals close to the intervention threshold [54].
Diabetes mellitus is significantly associated with lower TBS in unadjusted and adjusted models [55]. Moreover, TBS is negatively related to levels of HbA1c, fasting plasma glucose, and fasting insulin [56]. Recent studies show the potential of TBS in predicting the fracture risk in diabetes mellitus patients [53,54,55,56,57]. Studies that assess bone quality in DM with TBS are summarized in Table 1. In a recent cross-sectional study in which 119 T1DM patients (mean age 43.4 ± 8.9 years) and 68 gender, age, and BMI matched controls are included, TBS values are significantly lower in T1DM patients with prevalent fractures (1.309 ± 0.125 versus 1.370 ± 0.127, p = 0.04) [57]. In this set-up, a TBS cutoff < 1.42 discriminates the existence of fractures with a sensitivity of 91.7% and a specificity of 43.2% [57]. Another retrospective study which includes 169 postmenopausal women with T2DM evaluates the distinguishing performance of TBS, BMD, original and TBS-adjusted FRAX scores [63]. The result shows that TBS (p = 0.008) are significantly lower and TBS-adjusted FRAX score (OR = 2.0, 95% CI 1.1–2.7) is significantly higher in the group with vertebral fractures compared with the group without vertebral fractures [63]. Moreover, the AUCs of TBS-adjusted major FRAX for overall vertebral fracture risk stratification are significantly higher than that of major FRAX (0.717 versus 0.687; p = 0.043) [63]. There is a lack of clinical study directly comparing differences in TBS between T1DM and T2DM.
Multiple interventional studies have been done to investigate the response of TBS to osteoporosis treatment, though the study population is not limited to patients with DM (reviewed in [74, 75]). To summarize, current studies suggest that TBS tends to increase after treatment in parallel with the change of BMD, but the magnitude of increase of TBS is smaller than that of BMD [74, 75]. There is a lack of evidence in to what extent TBS increase after treatment predicts a reduction of fracture risk. The effect of diabetes treatment on TBS is still not fully known, though some studies demonstrate that HbA1c, fasting glucose, fasting insulin, and homeostasis model assessment for insulin resistance are negatively associated with TBS [56, 62, 66].
QCT
QCT is a noninvasive assessment of bone microarchitecture at the distal radius and tibia [76]. The high resolution of three-dimensional bone images generated by high-resolution peripheral quantitative computed tomography (HRpQCT) allows the measurement of volumetric BMD (vBMD) and other parameters. Mechanical properties of the bone can also be estimated from QCT images using microstructural finite element analysis (μFEA) [77].
QCT has been used in a number of studies to investigate the microarchitecture of bone in patients with diabetes mellitus [78,79,80,81,82]. Studies that assess bone quantity and quality in DM with QCT are summarized in Table 2. A cross-sectional study that includes 17 male T1DM patients aged from 18 to 49 years and 18 sex-matched healthy controls shows that T1DM patients have significant lower cortical vBMD in the femoral neck and significant lower vBMD, cortical thickness, and cortical area in the intertrochanter [78]. The bone strength estimated by pQCT was also lower in T1DM group [78]. Another cross-sectional study that includes 48 adolescents with T1DM also shows that T1DM is associated with reduced bone mineral content and small bone cross-sectional area and cortical strength [79]. In 2015, a cross-sectional study that includes 55 T1DM patients finds that diabetic microvascular disease is associated with deficits in cortical and trabecular vBMD and microarchitecture, while T1DM patients without diabetic microvascular disease show similar HR-pQCT parameters with controls [80]. Further investigation is needed to determine if this relationship between the presence of MVD and bone deficits is causal and impacts fracture risk, and whether diabetic bone disease is an extension of the spectrum of diabetic microvascular diseases.
QCT is also used to assess bone quality in patients with T2DM, but the study results are inconsistent among different studies. In the Framingham HR-pQCT Study which includes 1069 subjects (129 with T2DM, 940 without T2DM) with a mean age of 64 ± 8 years, researchers compare cortical and trabecular microarchitecture, bone density, bone area, and bone strength in T2DM and non-T2DM subjects [81]. After adjusting for age, sex, weight, and height, T2DM group has significantly lower cortical vBMD (p < 0.01), higher cortical porosity (p = 0.02), and smaller cross-sectional area (p = 0.04) at the tibia [81]. Moreover, lower cortical vBMD at the tibia and cortical thickness at the radius is seen in T2DM only among those with a prior fracture [81]. However, in the cross-sectional Gothenburg Study which includes 1053 women (99 with T2DM, 954 without T2DM) aged from 75 to 80 years, ultradistal tibial and radial trabecular volume fraction, distal cortical volumetric BMD, cortical area, and failure load are higher in patients with diabetes than in controls [82]. The different results between two studies may partly be due to the differences in characteristics of subjects and differences in study design [81]. It is also not fully known how well pQCT parameters could predict the fracture risk in T2DM patients.
Microindentation
Microindentation is a technique that can directly assess the mechanical characteristics of cortical bone in vivo. By inserting a probe assembly into a cortical bone’s surface at the anterior tibia and inducing microscopic fractures, microindentation measures bone mechanical strength at the tissue level. There are two approaches of microindentation, cyclic microindentation, and impact microindentation. In cyclic microindentation, relatively low forces (2–10 N) are applied over several seconds, and parameters such as first indentation distance (ID), total indentation distance (TID), indentation distance increase (IDI), creep ID, unloading slope (US) (ave of 3-last cycle), energy (ave of 3-last cycle) are output (reviewed in [104]). Impact microindentation is a single impulse indentation to a higher force within up to 0.25 ms (reviewed in [104]). Using the technique of impact microindentation, a ratio called bone material strength index (BMSi) can be derived, and a lower BMSi indicates lower fracture resistance [105]. The details of the two techniques are reviewed by Allen et al. [104].
Impact microindentation has been used in several clinical studies to investigate the bone quality in DM patients [11, 82, 106]. The Gothenburg Study finds that BMSi is lower in T2DM (74.6 ± 7.6 versus 78.2 ± 7.5, p < 0.01) [82]. In a series of cases and control study, 60 postmenopausal women including 30 patients with a T2DM history for more than 10 years and 30 age-matched non-diabetic controls received impact microindentation. Compared to controls, T2DM patients had significantly lower BMSi while their BMD were similar to controls [11]. This study also finds that the level of glycated hemoglobin over the past 10 years is negatively associated with BMSi (r = − 0.41; p = 0.026) [11]. In another cross-sectional study, BMSi is also found to be negatively associated with T2DM status [106]. Moreover, advanced glycation end product accumulation is negatively related to BMSi [106]. Though the invasive procedure restricts its wide use as a clinical tool, microindentation helps to shed light upon bone quality change in diabetes mellitus population.
Histomorphometry
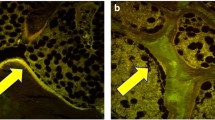
Bone histomorphometric analysis of bone biopsies provides a direct approach to assess bone remodeling rates at tissue level [107]. Moreover, bone microarchitecture can also be evaluated using micro-computed tomography (micro-CT) [107]. A number of studies in rodent models have shown reduced bone turnover rate, worse microstructure, and lower strength in rodent models of T1DM and T2DM [108,109,110,111]. However, as bone biopsy is an invasive test, only a few clinical studies have investigated the bone quality of diabetes mellitus patients using bone histomorphometry. A cross-sectional case-controlled study which includes 23 T1DM subjects (8 males and 15 females) and 23 age- and sex-matched controls does not find deterioration in bone histomorphometric or micro-CT variables in those patients without manifesting complications of T1DM [107]. However, T1DM patients with fracture history may have defects in bone microarchitecture [107]. A histomorphometric study published in 1964 finds an increase of cortical area of ribs in T2DM [112]. Another more recent study obtains iliac crest bone samples from 26 patients (13 male and 13 female) with an average age of 67.42 ± 2.74 years [113]. The control group consists of 20 non-diabetic subjects (11 male and 9 female) with a mean age of 57.95 ± 3.96 years that have suffered sudden or violent death [113]. As a result, significant lower bone volume (p < 0.0001), osteoid volume (p < 0.005), osteoid thickness (p < 0.0001), cortical thickness (p < 0.05), and osteoblast surface (p < 0.05) volume are found in the diabetic group [113]. The discrepancy of different studies may come from the relative low subject volume, the disease course, and complications. More high-quality clinical studies are needed to determine the histologic changes of diabetic bone.
Bone turnover markers
In patients with DM, the levels of multiple bone turnover markers are altered. A meta-analysis that includes 22 studies shows that osteocalcin (OC) and C-terminal telopeptide of type 1 collagen (CTX-1) are significantly lower in people with DM, while alkaline phosphatase (ALP), N-telopeptide of type I collagen (NTX), and hydroxyproline (HYP) do not differ [114]. The meta-analysis also reports decreased OC levels in T1DM compared to controls [114]. Some studies indicate that bone turnover markers are lower in children T1DM or at the onset of the disease [25, 115], but do not differ between T1DM adults and controls [116].
Levels of parathyroid hormone (PTH) tend to be 20–50% lower in T2D subjects than in controls [117,118,119] (reviewed in [120]). Most studies support that bone turnover markers, such as CTX, OC, P1NP, TRAP, and NTX, are reduced in patients with T2DM [11, 118, 119, 121,122,123]. Moreover, low P1NP and OC levels and high CTX, NTX, and sclerostin levels seem to be associated with increased fracture risks in T2DM, while are associated with [118, 121, 124, 125]. Further studies are needed to uncover whether bone turnover markers could predict alterations in bone quality and fracture risk.
Discussion
As is discussed in the introduction, multiple mechanisms contribute to the increased fracture risk in patients with DM. Some of these mechanisms have adverse effects on bone metabolism thus lead to declined bone quantity and quality.
High glucose levels in DM can lead to the accumulation of AGE collagen crosslinks in bone, which leads to biomechanically fragile bone [6]. AGEs can also be specifically recognized by AGE receptors (RAGE), which express in multiple bone-derived cells [126]. The AGE-RAGE interaction induces activation of nuclear factor kB (NF-kB) in RAGE-expressing cells [126]. As a result, the production of proinflammatory cytokines and reactive oxygen species (ROS) are increased in these cells which activate osteoclastogenesis and suppress osteoblast differentiation [127, 128]. Pentosidine is one of the best studied AGEs. Pentosidine levels were significantly higher in DM patients with fractures than those without fractures [129,130,131]. In patients with T2DM, urinary pentosidine levels negatively associate with trabecular bone scores [129]. This indicates that AGEs may play a role in the deterioration in bone microstructure, and this microstructure change can be estimated by methods like TBS.
Although T1DM and T2DM share many mechanisms in inducing osteoporosis and osteoporotic fractures, these mechanisms may affect bone metabolism differently in two diseases, and the two diseases may each have its special mechanisms. As is reviewed, compared those with T1DM, patients with T2DM have higher BMD [132, 133]. Young patients with T1DM, even only a few years after the onset of diabetes mellitus, have a lower BMD score [134,135,136], though decreased BMD are more frequent in patients with longer disease courses [16, 34]. Decreased BMD observed in T1DM is found to be associated with the presence of microvascular complications such as diabetic nephropathy, retinopathy, neuropathy [133]. Also as is reviewed in the main text, the presence of microvascular disease is associated with deficits in bone microstructure. These results indicate that microvascular disease, which may lead to inadequate blood flow in bone tissue, adversely affects bone formation in young T1DM patients and causes the deterioration in both bone quantity and quality. BMI has been found to be significantly greater in patients with T2DM compared to T1DM. BMI is positively associated with BMD and negatively associated with fracture risk [137, 138]. Therefore, high BMI may partly explain the relatively high BMD and low fracture risk in T2DM patients compared with T1DM patients.
Recent studies indicate that T1DM and T2DM differ in levels of bone turnover markers. Recently, Starup-Linde et al. find that compared to T2DM, T1DM has lower levels of P1NP, osteocalcin (OC), and s-receptor activator of nuclear factor kappa beta ligand (RANKL) [139]. The differences between T1DM and T2DM in biomarkers may be interpreted with insulin resistance status in T2DM [139]. How these differences affect bone health has not been fully known.
Patients with T1DM suffer from low levels of insulin and IGF1 since the stage of onset, while T2DM is characterized by insulin resistance, though in the advanced stage of T2DM, there is a relative insulin deficiency. Low levels of insulin and IGF1 have an adverse effect on osteoblasts during growth and can result in low peak bone mass at an early age [124, 140,141,142]. Though insulin mainly plays an anabolic role in the bone formation in physiological concentration, the relationship between hyperinsulinaemia and insulin resistance and bone metabolism is complex, and current clinical studies show conflicting results [45, 143,144,145,146,147]. Moreover, studies also suggest that hyperinsulinaemia and insulin resistance may contribute to reduced bone turnover even in the absence of hyperglycaemia [148].
Conclusion
In summary, diabetes mellitus is closely associated with increased risk of fracture. Therefore, assessment of bone quantity and bone quality may benefit DM patients, especially those with other factors of fractures. Although BMD and FRAX are very useful clinical tools in assessing bone quantity, they may not accurately account for extra fracture risk in diabetes mellitus. Through advances in new technologies, physicians can better assess the bone quality of patients with diabetes mellitus. Apart from BMD and FRAX, recent clinical evidence demonstrates that incorporating TBS brought a moderate improvement to currently used FRAX tool. Therefore, TBS can serve as a useful method in assessing bone quality in patients with DM. As TBS is based on DXA, it can be widely accessible without introducing new equipment. HR-pQCT is also a useful noninvasive method to discriminate bone quality change in DM patients but its association with fracture risk is far from being illustrated. Although the invasive procedures restrict the clinical use of microindentation and bone histomorphometry, they are useful in the research of bone quality in diabetes mellitus. Bone turnover markers have been found to be altered in diabetes mellitus and may be associated with fractures, but more studies are needed. In addition, fracture risk of DM patients is also associated with complications of DM. Further large-scale prospective studies about risk factors of fractures in DM may be needed to bring a special tool for fracture risk assessment in DM patients and identify high-risk population.
References
Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, Cavan D, Shaw JE, Makaroff LE (2017) IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128:40–50
Siris ES, Adler R, Bilezikian J, Bolognese M, Dawson-Hughes B, Favus MJ, Harris ST, Jan de Beur SM, Khosla S, Lane NE, Lindsay R, Nana AD, Orwoll ES, Saag K, Silverman S, Watts NB (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int 25:1439–1443
Fan Y, Wei F, Lang Y, Liu Y (2016) Diabetes mellitus and risk of hip fractures: a meta-analysis. Osteoporos Int 27:219–228
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166:495–505
Majumdar SR, Leslie WD, Lix LM, Morin SN, Johansson H, Oden A, McCloskey EV, Kanis JA (2016) Longer duration of diabetes strongly impacts fracture risk assessment: the Manitoba BMD cohort. J Clin Endocrinol Metab 101:4489–4496
Napoli N, Chandran M, Pierroz DD, Abrahamsen B, Schwartz AV, Ferrari SL (2017) Mechanisms of diabetes mellitus-induced bone fragility. Nat Rev Endocrinol 13:208–219
Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J (2012) Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab 14:634–643
Formiga F, Chivite D, Ruiz D, Navarro M, Perez Castejon JM, Duaso E, Montero A, Lopez-Soto A, Corbella X (2015) Clinical evidence of diabetes mellitus end-organ damage as risk factor for falls complicated by hip fracture: a multi-center study of 1225 patients. Diabetes Res Clin Pract 109:233–237
Schwartz AV, Sellmeyer DE, Ensrud KE, Cauley JA, Tabor HK, Schreiner PJ, Jamal SA, Black DM, Cummings SR (2001) Older women with diabetes have an increased risk of fracture: a prospective study. J Clin Endocrinol Metab 86:32–38
Bonds DE, Larson JC, Schwartz AV, Strotmeyer ES, Robbins J, Rodriguez BL, Johnson KC, Margolis KL (2006) Risk of fracture in women with type 2 diabetes: the Women's Health Initiative observational study. J Clin Endocrinol Metab 91:3404–3410
Farr JN, Drake MT, Amin S, Melton LJ 3rd, McCready LK, Khosla S (2014) In vivo assessment of bone quality in postmenopausal women with type 2 diabetes. J Bone Miner Res 29:787–795
Maggio AB, Ferrari S, Kraenzlin M, Marchand LM, Schwitzgebel V, Beghetti M, Rizzoli R, Farpour-Lambert NJ (2010) Decreased bone turnover in children and adolescents with well controlled type 1 diabetes. J Pediatr Endocrinol Metab 23:697–707
Hadjidakis DJ, Raptis AE, Sfakianakis M, Mylonakis A, Raptis SA (2006) Bone mineral density of both genders in type 1 diabetes according to bone composition. J Diabetes Complicat 20:302–307
Miazgowski T, Czekalski S (1998) A 2-year follow-up study on bone mineral density and markers of bone turnover in patients with long-standing insulin-dependent diabetes mellitus. Osteoporos Int 8:399–403
Neumann T, Samann A, Lodes S, Kastner B, Franke S, Kiehntopf M, Hemmelmann C, Lehmann T, Muller UA, Hein G et al (2011) Glycaemic control is positively associated with prevalent fractures but not with bone mineral density in patients with type 1 diabetes. Diabet Med 28:872–875
Mastrandrea LD, Wactawski-Wende J, Donahue RP, Hovey KM, Clark A, Quattrin T (2008) Young women with type 1 diabetes have lower bone mineral density that persists over time. Diabetes Care 31:1729–1735
AboElAsrar MA, Elbarbary NS, Elshennawy DE, Omar AM (2012) Insulin-like growth factor-1 cytokines cross-talk in type 1 diabetes mellitus: relationship to microvascular complications and bone mineral density. Cytokine 59:86–93
Slade JM, Coe LM, Meyer RA, McCabe LR (2012) Human bone marrow adiposity is linked with serum lipid levels not T1-diabetes. J Diabetes Complicat 26:1–9
Gogas Yavuz D, Keskin L, Kiyici S, Sert M, Yazici D, Sahin I, Yuksel M, Deyneli O, Aydin H, Tuncel E et al (2011) Vitamin D receptor gene BsmI, FokI, ApaI, TaqI polymorphisms and bone mineral density in a group of Turkish type 1 diabetic patients. Acta Diabetol 48:329–336
Abd El Dayem SM, El-Shehaby AM, Abd El Gafar A, Fawzy A, Salama H (2011) Bone density, body composition, and markers of bone remodeling in type 1 diabetic patients. Scand J Clin Lab Invest 71:387–393
Heilman K, Zilmer M, Zilmer K, Tillmann V (2009) Lower bone mineral density in children with type 1 diabetes is associated with poor glycemic control and higher serum ICAM-1 and urinary isoprostane levels. J Bone Miner Metab 27:598–604
Hamilton EJ, Rakic V, Davis WA, Chubb SA, Kamber N, Prince RL, Davis TM (2009) Prevalence and predictors of osteopenia and osteoporosis in adults with type 1 diabetes. Diabet Med 26:45–52
Danielson KK, Elliott ME, LeCaire T, Binkley N, Palta M (2009) Poor glycemic control is associated with low BMD detected in premenopausal women with type 1 diabetes. Osteoporos Int 20:923–933
Miazgowski T, Pynka S, Noworyta-Zietara M, Krzyzanowska-Swiniarska B, Pikul R (2007) Bone mineral density and hip structural analysis in type 1 diabetic men. Eur J Endocrinol 156:123–127
Karaguzel G, Akcurin S, Ozdem S, Boz A, Bircan I (2006) Bone mineral density and alterations of bone metabolism in children and adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 19:805–814
Strotmeyer ES, Cauley JA, Orchard TJ, Steenkiste AR, Dorman JS (2006) Middle-aged premenopausal women with type 1 diabetes have lower bone mineral density and calcaneal quantitative ultrasound than nondiabetic women. Diabetes Care 29:306–311
Salvatoni A, Mancassola G, Biasoli R, Cardani R, Salvatore S, Broggini M, Nespoli L (2004) Bone mineral density in diabetic children and adolescents: a follow-up study. Bone 34:900–904
Ingberg CM, Palmer M, Aman J, Arvidsson B, Schvarcz E, Berne C (2004) Body composition and bone mineral density in long-standing type 1 diabetes. J Intern Med 255:392–398
Heap J, Murray MA, Miller SC, Jalili T, Moyer-Mileur LJ (2004) Alterations in bone characteristics associated with glycemic control in adolescents with type 1 diabetes mellitus. J Pediatr 144:56–62
Liu EY, Wactawski-Wende J, Donahue RP, Dmochowski J, Hovey KM, Quattrin T (2003) Does low bone mineral density start in post-teenage years in women with type 1 diabetes? Diabetes Care 26:2365–2369
Rachon D, Mysliwska J, Suchecka-Rachon K, Semetkowska-Jurkiewicz B, Zorena K, Lysiak-Szydlowska W (2003) Serum interleukin-6 levels and bone mineral density at the femoral neck in post-menopausal women with type 1 diabetes. Diabet Med 20:475–480
Gunczler P, Lanes R, Paoli M, Martinis R, Villaroel O, Weisinger JR (2001) Decreased bone mineral density and bone formation markers shortly after diagnosis of clinical type 1 diabetes mellitus. J Pediatr Endocrinol Metab 14:525–528
Tuominen JT, Impivaara O, Puukka P, Ronnemaa T (1999) Bone mineral density in patients with type 1 and type 2 diabetes. Diabetes Care 22:1196–1200
Hampson G, Evans C, Petitt RJ, Evans WD, Woodhead SJ, Peters JR, Ralston SH (1998) Bone mineral density, collagen type 1 alpha 1 genotypes and bone turnover in premenopausal women with diabetes mellitus. Diabetologia 41:1314–1320
Lunt H, Florkowski CM, Cundy T, Kendall D, Brown LJ, Elliot JR, Wells JE, Turner JG (1998) A population-based study of bone mineral density in women with longstanding type 1 (insulin dependent) diabetes. Diabetes Res Clin Pract 40:31–38
Olmos JM, Perez-Castrillon JL, Garcia MT, Garrido JC, Amado JA, Gonzalez-Macias J (1994) Bone densitometry and biochemical bone remodeling markers in type 1 diabetes mellitus. Bone Miner 26:1–8
Pan H, Wu N, Yang T, He W (2014) Association between bone mineral density and type 1 diabetes mellitus: a meta-analysis of cross-sectional studies. Diabetes Metab Res Rev 30:531–542
Yaturu S, Humphrey S, Landry C, Jain SK (2009) Decreased bone mineral density in men with metabolic syndrome alone and with type 2 diabetes. Med Sci Monit 15:Cr5–Cr9
Kao WH, Kammerer CM, Schneider JL, Bauer RL, Mitchell BD (2003) Type 2 diabetes is associated with increased bone mineral density in Mexican-American women. Arch Med Res 34:399–406
Majima T, Komatsu Y, Yamada T, Koike Y, Shigemoto M, Takagi C, Hatanaka I, Nakao K (2005) Decreased bone mineral density at the distal radius, but not at the lumbar spine or the femoral neck, in Japanese type 2 diabetic patients. Osteoporos Int 16:907–913
Barrett-Connor E, Holbrook TL (1992) Sex differences in osteoporosis in older adults with non-insulin-dependent diabetes mellitus. JAMA 268:3333–3337
Gerdhem P, Isaksson A, Akesson K, Obrant KJ (2005) Increased bone density and decreased bone turnover, but no evident alteration of fracture susceptibility in elderly women with diabetes mellitus. Osteoporos Int 16:1506–1512
de Liefde II, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA (2005) Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam study. Osteoporos Int 16:1713–1720
Sosa M, Dominguez M, Navarro MC, Segarra MC, Hernandez D, de Pablos P, Betancor P (1996) Bone mineral metabolism is normal in non-insulin-dependent diabetes mellitus. J Diabetes Complicat 10:201–205
Dennison EM, Syddall HE, Aihie Sayer A, Craighead S, Phillips DI, Cooper C (2004) Type 2 diabetes mellitus is associated with increased axial bone density in men and women from the Hertfordshire cohort study: evidence for an indirect effect of insulin resistance? Diabetologia 47:1963–1968
Bridges MJ, Moochhala SH, Barbour J, Kelly CA (2005) Influence of diabetes on peripheral bone mineral density in men: a controlled study. Acta Diabetol 42:82–86
Schwartz AV, Sellmeyer DE, Strotmeyer ES, Tylavsky FA, Feingold KR, Resnick HE, Shorr RI, Nevitt MC, Black DM, Cauley JA et al (2005) Diabetes and bone loss at the hip in older black and white adults. J Bone Miner Res 20:596–603
Rakic V, Davis WA, Chubb SA, Islam FM, Prince RL, Davis TM (2006) Bone mineral density and its determinants in diabetes: the Fremantle diabetes study. Diabetologia 49:863–871
Hadzibegovic I, Miskic B, Cosic V, Prvulovic D, Bistrovic D (2008) Increased bone mineral density in postmenopausal women with type 2 diabetes mellitus. Ann Saudi Med 28:102–104
Anaforoglu I, Nar-Demirer A, Bascil-Tutuncu N, Ertorer ME (2009) Prevalence of osteoporosis and factors affecting bone mineral density among postmenopausal Turkish women with type 2 diabetes. J Diabetes Complicat 23:12–17
Ma L, Oei L, Jiang L, Estrada K, Chen H, Wang Z, Yu Q, Zillikens MC, Gao X, Rivadeneira F (2012) Association between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studies. Eur J Epidemiol 27:319–332
Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, Donaldson MG, Cauley JA, Harris TB, Koster A, Womack CR, Palermo L, Black DM, Study of Osteoporotic Fractures (SOF) Research Group, Osteoporotic Fractures in Men (MrOS) Research Group, Health, Aging, and Body Composition (Health ABC) Research Group (2011) Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA 305:2184–2192
McCloskey EV, Oden A, Harvey NC, Leslie WD, Hans D, Johansson H, Barkmann R, Boutroy S, Brown J, Chapurlat R et al (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31:940–948
Martineau P, Leslie WD, Johansson H, Oden A, McCloskey EV, Hans D, Kanis JA (2017) Clinical utility of using lumbar spine trabecular bone score to adjust fracture probability: the Manitoba BMD cohort. J Bone Miner Res 32:1568–1574
Leslie WD, Aubry-Rozier B, Lamy O, Hans D (2013) TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98:602–609
Kim JH, Choi HJ, Ku EJ, Kim KM, Kim SW, Cho NH, Shin CS (2015) Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab 100:475–482
Neumann T, Lodes S, Kastner B, Lehmann T, Hans D, Lamy O, Muller UA, Wolf G, Samann A (2016) Trabecular bone score in type 1 diabetes--a cross-sectional study. Osteoporos Int 27:127–133
Shah V, Pyle L, Joshee P, Ostendorf D, Kohrt WM, Alman A, Snell-Bergeon JK (2017) Trabecular bone score is lower in adults with type 1 diabetes and is related to visceral and pericardial fat but not body mass index or subcutaneous fat. Endocr Rev 38:S1
Syversen U, Reseland J, Eriksen EF, Mynarek IM, Iversen TSJ, Basso T, Aasarød KM, Åsvold BO, Mosti MP, Stunes AK (2017) Impaired bone quality, assessed by trabecular bone score and in vivo micro indentation, in men with type 1 diabetes mellitus. Calcif Tissue Int 100:S29
Shah VN, Sippl R, Joshee P, Pyle L, Kohrt WM, Schauer IE, Snell-Bergeon JK (2018) Trabecular bone quality is lower in adults with type 1 diabetes and is negatively associated with insulin resistance. Osteoporos Int 29:733–739
Gilmour J, Colquhoun A, Wu W, Kim S (2018) Type 1 diabetes and bone microarchitecture assessment with trabecular bone score (TBS): a descriptive study. J Clin Densitom 21:27
Dhaliwal R, Cibula D, Ghosh C, Weinstock RS, Moses AM (2014) Bone quality assessment in type 2 diabetes mellitus. Osteoporosis Int 25:1969–1973
Choi YJ, Ock SY, Chung YS (2016) Trabecular bone score (TBS) and TBS-adjusted fracture risk assessment tool are potential supplementary tools for the discrimination of morphometric vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Densitom 19:507–514
Zhukouskaya VV, Eller-Vainicher C, Gaudio A, Privitera F, Cairoli E, Ulivieri FM, Palmieri S, Morelli V, Grancini V, Orsi E et al (2016) The utility of lumbar spine trabecular bone score and femoral neck bone mineral density for identifying asymptomatic vertebral fractures in well-compensated type 2 diabetic patients. Osteoporos Int 27:49–56
Bonaccorsi G, Fila E, Messina C, Maietti E, Ulivieri FM, Caudarella R, Greco P, Guglielmi G (2017) Comparison of trabecular bone score and hip structural analysis with FRAX((R)) in postmenopausal women with type 2 diabetes mellitus. Aging Clin Exp Res 29:951–957
Iki M, Fujita Y, Kouda K, Yura A, Tachiki T, Tamaki J, Winzenrieth R, Sato Y, Moon JS, Okamoto N, Kurumatani N (2017) Hyperglycemia is associated with increased bone mineral density and decreased trabecular bone score in elderly Japanese men: the Fujiwara-kyo osteoporosis risk in men (FORMEN) study. Bone 105:18–25
De Araújo I, Salmon C, Nogueira-Barbosa M, Luchini S, De Paula F (2017) Marrow adipose tissue, trabecular bone score and osteocalcin as parameters of bone quality in type 2 diabetes mellitus. J Bone Miner Res 32:S316
Buni M, Ambrose CG, McCormick J, Fisher-Hoch S, Rianon N (2017) The utility of trabecular bone score in evaluating bone quality in Hispanic population with type 2 diabetes. J Bone Miner Res 32:S245
Payer J, Jackuliak P, Kuzma M, Killinger Z (2017) Metabolic compensation of type 2 diabetes and bone quality. Endocr Rev 38:S1
Torres MM, Perez MDA, Martin AG, Rodriguez CN, Córdova RM, Serrano RN (2017) Trabecular bone score in type 2 diabetes mellitus: preliminary data of cross-sectional case-control study. J Bone Miner Res 31:S1
Xue Y, Baker AL, Nader S, Orlander P, Sanchez AJ, Kellam J, Rianon NJ, Ambrose CG (2017) Lumbar spine trabecular bone score (TBS) reflects diminished bone quality in patients with diabetes mellitus and oral glucocorticoid therapy. J Clin Densitom 21:185–192
Jain RK, Zeytinoglu M, Vokes TJ (2017) Diabetes mellitus and trabecular bone score (TBS) in caucasians and African Americans referred for bone densitometry. Endocr Rev 38:S1
Holloway KL, De Abreu LLF, Hans D, Kotowicz MA, Sajjad MA, Hyde NK, Pasco JA (2018) Trabecular bone score in men and women with impaired fasting glucose and diabetes. Calcif Tissue Int 102:32–40
Harvey NC, Gluer CC, Binkley N, McCloskey EV, Brandi ML, Cooper C, Kendler D, Lamy O, Laslop A, Camargos BM et al (2015) Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone 78:216–224
Hans D, Stenova E, Lamy O (2017) The trabecular bone score (TBS) complements DXA and the FRAX as a fracture risk assessment tool in routine clinical practice. Curr Osteoporos Rep 15:521–531
Pawlowska M, Bilezikian JP (2016) Beyond DXA: advances in clinical applications of new bone imaging TECHNOLOGY. Endocr Pract 22:990–998
Macneil JA, Boyd SK (2008) Bone strength at the distal radius can be estimated from high-resolution peripheral quantitative computed tomography and the finite element method. Bone 42:1203–1213
Ishikawa K, Fukui T, Nagai T, Kuroda T, Hara N, Yamamoto T, Inagaki K, Hirano T (2015) Type 1 diabetes patients have lower strength in femoral bone determined by quantitative computed tomography: a cross-sectional study. J Diab Investig 6:726–733
Saha MT, Sievanen H, Salo MK, Tulokas S, Saha HH (2009) Bone mass and structure in adolescents with type 1 diabetes compared to healthy peers. Osteoporos Int 20:1401–1406
Shanbhogue VV, Hansen S, Frost M, Jorgensen NR, Hermann AP, Henriksen JE, Brixen K (2015) Bone geometry, volumetric density, microarchitecture, and estimated bone strength assessed by HR-pQCT in adult patients with type 1 diabetes mellitus. J Bone Miner Res 30:2188–2199
Samelson EJ, Demissie S, Cupples LA, Zhang X, Xu H, Liu CT, Boyd SK, McLean RR, Broe KE, Kiel DP et al (2017) Diabetes and deficits in cortical bone density, microarchitecture, and bone size: Framingham HR-pQCT study. J Bone Miner Res 33:54–62
Nilsson AG, Sundh D, Johansson L, Nilsson M, Mellstrom D, Rudang R, Zoulakis M, Wallander M, Darelid A, Lorentzon M (2017) Type 2 diabetes mellitus is associated with better bone microarchitecture but lower bone material strength and poorer physical function in elderly women: a population-based study. J Bone Miner Res 32:1062–1071
Roe TF, Mora S, Costin G, Kaufman F, Carlson ME, Gilsanz V (1991) Vertebral bone density in insulin-dependent diabetic children. Metabolism 40:967–971
Lettgen B, Hauffa B, Mohlmann C, Jeken C, Reiners C (1995) Bone mineral density in children and adolescents with juvenile diabetes: selective measurement of bone mineral density of trabecular and cortical bone using peripheral quantitative computed tomography. Horm Res 43:173–175
Moyer-Mileur LJ, Dixon SB, Quick JL, Askew EW, Murray MA (2004) Bone mineral acquisition in adolescents with type 1 diabetes. J Pediatr 145:662–669
Bechtold S, Putzker S, Bonfig W, Fuchs O, Dirlenbach I, Schwarz HP (2007) Bone size normalizes with age in children and adolescents with type 1 diabetes. Diabetes Care 30:2046–2050
Roggen I, Gies I, Vanbesien J, Louis O, De Schepper J (2013) Trabecular bone mineral density and bone geometry of the distal radius at completion of pubertal growth in childhood type 1 diabetes. Horm Res Paediatr 79:68–74
Starup-Linde J, Lykkeboe S, Gregersen S, Hauge EM, Langdahl BL, Handberg A, Vestergaard P (2016) Bone structure and predictors of fracture in type 1 and type 2 diabetes. J Clin Endocrinol Metab 101:928–936
Kuroda T, Ishikawa K, Nagai T, Fukui T, Hirano T, Inagaki K (2017) Quadrant analysis of quantitative computed tomography scans of the femoral neck reveals superior region-specific weakness in young and middle-aged men with type 1 diabetes mellitus. J Clin Densitom 21:172–178
Verroken C, Pieters W, Beddeleem L, Goemaere S, Zmierczak HG, Shadid S, Kaufman JM, Lapauw B (2017) Cortical bone size deficit in adult patients with type 1 diabetes mellitus. J Clin Endocrinol Metab 102:2887–2895
Maratova K, Soucek O, Matyskova J, Hlavka Z, Petruzelkova L, Obermannova B, Pruhova S, Kolouskova S, Sumnik Z (2018) Muscle functions and bone strength are impaired in adolescents with type 1 diabetes. Bone 106:22–27
Register TC, Lenchik L, Hsu FC, Lohman KK, Freedman BI, Bowden DW, Carr JJ (2006) Type 2 diabetes is not independently associated with spinal trabecular volumetric bone mineral density measured by QCT in the diabetes heart study. Bone 39:628–633
Melton LJ 3rd, Riggs BL, Leibson CL, Achenbach SJ, Camp JJ, Bouxsein ML, Atkinson EJ, Robb RA, Khosla S (2008) A bone structural basis for fracture risk in diabetes. J Clin Endocrinol Metab 93:4804–4809
Petit MA, Paudel ML, Taylor BC, Hughes JM, Strotmeyer ES, Schwartz AV, Cauley JA, Zmuda JM, Hoffman AR, Ensrud KE (2010) Bone mass and strength in older men with type 2 diabetes: the osteoporotic fractures in men study. J Bone Miner Res 25:285–291
Burghardt AJ, Issever AS, Schwartz AV, Davis KA, Masharani U, Majumdar S, Link TM (2010) High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 95:5045–5055
Shu A, Yin MT, Stein E, Cremers S, Dworakowski E, Ives R, Rubin MR (2012) Bone structure and turnover in type 2 diabetes mellitus. Osteoporos Int 23:635–641
Patsch JM, Burghardt AJ, Yap SP, Baum T, Schwartz AV, Joseph GB, Link TM (2013) Increased cortical porosity in type 2 diabetic postmenopausal women with fragility fractures. J Bone Miner Res 28:313–324
Kiyohara N, Yamamoto M, Sugimoto T (2015) Discordance between prevalent vertebral fracture and vertebral strength estimated by the finite element method based on quantitative computed tomography in patients with type 2 diabetes mellitus. PLoS One 10:e0144496
Yu EW, Putman MS, Derrico N, Abrishamanian-Garcia G, Finkelstein JS, Bouxsein ML (2015) Defects in cortical microarchitecture among African-American women with type 2 diabetes. Osteoporos Int 26:673–679
Heilmeier U, Carpenter DR, Patsch JM, Harnish R, Joseph GB, Burghardt AJ, Baum T, Schwartz AV, Lang TF, Link TM (2015) Volumetric femoral BMD, bone geometry, and serum sclerostin levels differ between type 2 diabetic postmenopausal women with and without fragility fractures. Osteoporos Int 26:1283–1293
Shanbhogue VV, Hansen S, Frost M, Jorgensen NR, Hermann AP, Henriksen JE, Brixen K (2016) Compromised cortical bone compartment in type 2 diabetes mellitus patients with microvascular disease. Eur J Endocrinol 174:115–124
Patsch JM, Rasul S, Huber FA, Leitner K, Thomas A, Kocijan R, Boutroy S, Weber M, Resch H, Kainberger F, Schüller-Weidekamm C, Kautzky-Willer A (2017) Similarities in trabecular hypertrophy with site-specific differences in cortical morphology between men and women with type 2 diabetes mellitus. PLoS One 12:e0174664
Paccou J, Ward KA, Jameson KA, Dennison EM, Cooper C, Edwards MH (2016) Bone microarchitecture in men and women with diabetes: the importance of cortical porosity. Calcif Tissue Int 98:465–473
Allen MR, McNerny EM, Organ JM, Wallace JM (2015) True gold or pyrite: a review of reference point indentation for assessing bone mechanical properties in vivo. J Bone Miner Res 30:1539–1550
Malgo F, Hamdy NA, Papapoulos SE, Appelman-Dijkstra NM (2015) Bone material strength as measured by microindentation in vivo is decreased in patients with fragility fractures independently of bone mineral density. J Clin Endocrinol Metab 100:2039–2045
Furst JR, Bandeira LC, Fan WW, Agarwal S, Nishiyama KK, McMahon DJ, Dworakowski E, Jiang H, Silverberg SJ, Rubin MR (2016) Advanced glycation Endproducts and bone material strength in type 2 diabetes. J Clin Endocrinol Metab 101:2502–2510
Armas LA, Akhter MP, Drincic A, Recker RR (2012) Trabecular bone histomorphometry in humans with type 1 diabetes mellitus. Bone 50:91–96
Hamann C, Goettsch C, Mettelsiefen J, Henkenjohann V, Rauner M, Hempel U, Bernhardt R, Fratzl-Zelman N, Roschger P, Rammelt S, Günther KP, Hofbauer LC (2011) Delayed bone regeneration and low bone mass in a rat model of insulin-resistant type 2 diabetes mellitus is due to impaired osteoblast function. Am J Physiol Endocrinol Metab 301:E1220–E1228
Abbassy MA, Watari I, Soma K (2010) The effect of diabetes mellitus on rat mandibular bone formation and microarchitecture. Eur J Oral Sci 118:364–369
Picke AK, Gordaliza Alaguero I, Campbell GM, Gluer CC, Salbach-Hirsch J, Rauner M, Hofbauer LC, Hofbauer C (2016) Bone defect regeneration and cortical bone parameters of type 2 diabetic rats are improved by insulin therapy. Bone 82:108–115
Follak N, Kloting I, Wolf E, Merk H (2004) Improving metabolic control reverses the histomorphometric and biomechanical abnormalities of an experimentally induced bone defect in spontaneously diabetic rats. Calcif Tissue Int 74:551–560
Klein, Frost HM, Sedlin E (1964) A pilot study of lamellar bone physiology in diabetes mellitus. Henry Ford Hosp Med Bull 12:55–62
Leite Duarte ME, da Silva RD (1996) Histomorphometric analysis of the bone tissue in patients with non-insulin-dependent diabetes (DMNID). Rev Hosp Clin 51:7–11
Starup-Linde J, Eriksen SA, Lykkeboe S, Handberg A, Vestergaard P (2014) Biochemical markers of bone turnover in diabetes patients--a meta-analysis, and a methodological study on the effects of glucose on bone markers. Osteoporos Int 25:1697–1708
Pater A, Sypniewska G, Pilecki O (2010) Biochemical markers of bone cell activity in children with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 23:81–86
Alexopoulou O, Jamart J, Devogelaer JP, Brichard S, de Nayer P, Buysschaert M (2006) Bone density and markers of bone remodeling in type 1 male diabetic patients. Diabete Metab 32:453–458
Dobnig H, Piswanger-Solkner JC, Roth M, Obermayer-Pietsch B, Tiran A, Strele A, Maier E, Maritschnegg P, Sieberer C, Fahrleitner-Pammer A (2006) Type 2 diabetes mellitus in nursing home patients: effects on bone turnover, bone mass, and fracture risk. J Clin Endocrinol Metab 91:3355–3363
Ardawi MS, Akhbar DH, Alshaikh A, Ahmed MM, Qari MH, Rouzi AA, Ali AY, Abdulrafee AA, Saeda MY (2013) Increased serum sclerostin and decreased serum IGF-1 are associated with vertebral fractures among postmenopausal women with type-2 diabetes. Bone 56:355–362
Yamamoto M, Yamaguchi T, Nawata K, Yamauchi M, Sugimoto T (2012) Decreased PTH levels accompanied by low bone formation are associated with vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 97:1277–1284
Rubin MR, Patsch JM (2016) Assessment of bone turnover and bone quality in type 2 diabetic bone disease: current concepts and future directions. Bone Res 4:16001
Jiajue R, Jiang Y, Wang O, Li M, Xing X, Cui L, Yin J, Xu L, Xia W (2014) Suppressed bone turnover was associated with increased osteoporotic fracture risks in non-obese postmenopausal Chinese women with type 2 diabetes mellitus. Osteoporosis Int 25:1999–2005
Sarkar PD, Choudhury AB (2013) Relationships between serum osteocalcin levels versus blood glucose, insulin resistance and markers of systemic inflammation in central Indian type 2 diabetic patients. Eur Rev Med Pharmacol Sci 17:1631–1635
Movahed A, Larijani B, Nabipour I, Kalantarhormozi M, Asadipooya K, Vahdat K, Akbarzadeh S, Farrokhnia M, Assadi M, Amirinejad R, Bargahi A, Sanjdideh Z (2012) Reduced serum osteocalcin concentrations are associated with type 2 diabetes mellitus and the metabolic syndrome components in postmenopausal women: the crosstalk between bone and energy metabolism. J Bone Miner Metab 30:683–691
Kanazawa I, Yamaguchi T, Sugimoto T (2011) Serum insulin-like growth factor-I is a marker for assessing the severity of vertebral fractures in postmenopausal women with type 2 diabetes mellitus. Osteoporos Int 22:1191–1198
Kanazawa I, Yamaguchi T, Yamamoto M, Sugimoto T (2010) Relationship between treatments with insulin and oral hypoglycemic agents versus the presence of vertebral fractures in type 2 diabetes mellitus. J Bone Miner Metab 28:554–560
Hein GE (2006) Glycation endproducts in osteoporosis--is there a pathophysiologic importance? Clin Chim Acta 371:32–36
Gilbert L, He X, Farmer P, Boden S, Kozlowski M, Rubin J, Nanes MS (2000) Inhibition of osteoblast differentiation by tumor necrosis factor-alpha. Endocrinology 141:3956–3964
Glantschnig H, Fisher JE, Wesolowski G, Rodan GA, Reszka AA (2003) M-CSF, TNFalpha and RANK ligand promote osteoclast survival by signaling through mTOR/S6 kinase. Cell Death Differ 10:1165–1177
Choi YJ, Ock SY, Jin Y, Lee JS, Kim SH, Chung Y (2018) Urinary Pentosidine levels negatively associates with trabecular bone scores in patients with type 2 diabetes mellitus. Osteoporos Int 29:907–915
Saito M, Fujii K, Marumo K (2006) Degree of mineralization-related collagen crosslinking in the femoral neck cancellous bone in cases of hip fracture and controls. Calcif Tissue Int 79:160–168
Schwartz AV, Garnero P, Hillier TA, Sellmeyer DE, Strotmeyer ES, Feingold KR, Resnick HE, Tylavsky FA, Black DM, Cummings SR, Harris TB, Bauer DC, Health, Aging, and Body Composition Study (2009) Pentosidine and increased fracture risk in older adults with type 2 diabetes. J Clin Endocrinol Metab 94:2380–2386
DeShields SC, Cunningham TD (2018) Comparison of osteoporosis in US adults with type 1 and type 2 diabetes mellitus. J Endocrinol Investig. https://doi.org/10.1007/s40618-018-0828-x
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int 18:427–444
Thrailkill KM, Lumpkin CK, Bunn RC, Kemp SF, Fowlkes JL (2005) Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Phys Endocrinol Metab 289:E735–E745
Hofbauer LC, Brueck CC, Singh SK, Dobnig H (2007) Osteoporosis in patients with diabetes mellitus. J Bone Miner Res 22:1317–1328
Compston JE, Flahive J, Hosmer DW, Watts NB, Siris ES, Silverman S, Saag KG, Roux C, Rossini M, Pfeilschifter J, Nieves JW, Netelenbos JC, March L, LaCroix AZ, Hooven FH, Greenspan SL, Gehlbach SH, Díez-Pérez A, Cooper C, Chapurlat RD, Boonen S, Anderson FA Jr, Adami S, Adachi JD, for the GLOW Investigators (2014) Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: the global longitudinal study of osteoporosis in women (GLOW). J Bone Miner Res 29:487–493
Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, Ensrud K, Stefanick ML, Barrett-Connor E, Orwoll ES (2011) BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res 26:496–502
Chan MY, Frost SA, Center JR, Eisman JA, Nguyen TV (2014) Relationship between body mass index and fracture risk is mediated by bone mineral density. J Bone Miner Res 29:2327–2335
Starup-Linde J, Lykkeboe S, Gregersen S, Hauge EM, Langdahl BL, Handberg A, Vestergaard P (2016) Differences in biochemical bone markers by diabetes type and the impact of glucose. Bone 83:149–155
Gandhi A, Beam HA, O'Connor JP, Parsons JR, Lin SS (2005) The effects of local insulin delivery on diabetic fracture healing. Bone 37:482–490
Fulzele K, DiGirolamo DJ, Liu Z, Xu J, Messina JL, Clemens TL (2007) Disruption of the insulin-like growth factor type 1 receptor in osteoblasts enhances insulin signaling and action. J Biol Chem 282:25649–25658
Miyake H, Kanazawa I, Sugimoto T (2017) Decreased Serum Insulin-like Growth Factor-I is a Risk Factor for Non-vertebral Fractures in Diabetic Postmenopausal Women. Intern Med 56:269–273
Abrahamsen B, Rohold A, Henriksen JE, Beck-Nielsen H (2000) Correlations between insulin sensitivity and bone mineral density in non-diabetic men. Diabet Med 17:124–129
Shanbhogue VV, Finkelstein JS, Bouxsein ML, Yu EW (2016) Association between insulin resistance and bone structure in nondiabetic postmenopausal women. J Clin Endocrinol Metab 101:3114–3122
Hernandez JL, Olmos JM, Pariente E, Martinez J, Valero C, Garcia-Velasco P, Nan D, Llorca J, Gonzalez-Macias J (2010) Metabolic syndrome and bone metabolism: the Camargo Cohort study. Menopause 17:955–961
Verroken C, Zmierczak HG, Goemaere S, Kaufman JM, Lapauw B (2017) Insulin resistance is associated with smaller cortical bone size in nondiabetic men at the age of peak bone mass. J Clin Endocrinol Metab 102:1807–1815
von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E (2007) Associations between the metabolic syndrome and bone health in older men and women: the rancho Bernardo study. Osteoporos Int 18:1337–1344
Tonks KT, White CP, Center JR, Samocha-Bonet D, Greenfield JR (2017) Bone turnover is suppressed in insulin resistance, independent of adiposity. J Clin Endocrinol Metab 102:1112–1121
Acknowledgments
This study was supported by a grant from The Ministry of Science and Technology of the Peoples Republic of China (National Science and Technology Major Projects for Major New Drugs Innovation and Development 2008ZX09312-016), National Natural Science Foundation of China (No. 81070687,81170805 and 81670714), Beijing Natural Science Foundation (No. 7121012) and Scientific Research Foundation of Beijing Medical Development (No. 2007-3029), National Key Program of Clinical Science (WBYZ2011-873), CAMS Innovation Fund for Medical Sciences (No. 2016-I2M-3-003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Ning Jiang and Weibo Xia declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Jiang, N., Xia, W. Assessment of bone quality in patients with diabetes mellitus. Osteoporos Int 29, 1721–1736 (2018). https://doi.org/10.1007/s00198-018-4532-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4532-7