Abstract
Introduction and hypothesis
The effect of different abdominal contractions on the position of pelvic organs in parous women during postpartum exercises has not been sufficiently assessed. The aim of this study was to evaluate the displacement of the bladder base (BB) during different pelvic floor and abdominal contractions in parous women compared to nulliparous women. We hypothesised that abdominal and perineal contractions will produce a disparate effect on the position of the BB between groups.
Methods
Cross-sectional study including a convenience sample of 63 volunteers (35 nulliparous vs. 28 postpartum women). Transabdominal ultrasound was used in mode B to image the displacement of the BB. The protocol included six different pelvic floor and abdominal contractions commonly used in postpartum rehabilitation.
Results
The BB elevated significantly more in the postpartum group compared to nulliparous women when performing submaximal contraction of pelvic floor and transversus abdominis muscles simultaneously with axial elongation of the back (0.93 ± 0.55 cm in parous women vs. 0.66 ± 0.46 cm in nulliparous women). In contrast, the BB was found to descend significantly during a curl-up contraction in both groups (0.93 ± 0.55 cm in parous women vs. 0.66 ± 0.46 cm in nulliparous women).
Conclusions
The overall results of this study showed that perineal and superficial abdominal contractions produced different immediate effects compared to deep abdominal contractions on the displacement of BB in parous and nulliparous women. Further research is required to assess the long-term effects of these contractions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is a lack of consensus about the most effective pelvic floor and abdominal contractions during the postpartum period. Besides, there is a considerable community of women asking for early exercise to help restore their figures, starting soon after birth. Postpartum women show important changes in the urethral support system at least 6 months after delivery, as measured by perineal ultrasound [1]: widening of the resting urethral angle, higher compliance during both Valsalva manoeuvres and coughing, and higher hysteresis of the pelvic connective tissue. These changes should be considered to prescribe specific pelvic floor muscles (PFM) and abdominal contractions for the postnatal period. Articles about postpartum contractions mostly deal with the rehabilitation of pelvic floor muscles [2, 3] or the treatment of abdominal diastasis [3,4,5], while the effects of these contractions on the pelvic organs are not discussed. The specific groups of muscles involved in most of the postpartum programmes in the literature are transversus abdominis (TrA), obliquus externus abdominis (OE), obliquus internus abdominis (OI), rectus abdominis (RA), and PFM, while some of the most common studied contractions in parous women are abdominal crunch, abdominal brace, abdominal drawing, and voluntary pelvic floor contraction [2,3,4,5,6,7,8,9]. The potential disparate effect of contractions on the bladder position between nulliparous and parous women can be clinically important to design postpartum rehabilitative programmes, especially in group-based training.
The primary aim of the study was to investigate the immediate effect of different perineal and abdominal contractions on the displacement of the bladder base (BB) using transverse transabdominal ultrasound (TransvTAUS). The secondary aim of the research was to compare the effects of these contractions between continent parous and nulliparous women. We hypothesised that there will be a disparate effect of the abdominal and perineal contractions on the displacement of the BB between the two groups.
Methods and materials
Participants
A convenience sample of 63 volunteers (35 nulliparous women and 28 postpartum women between the 6th and 12th week after birth) participated in this cross-sectional study. Inclusion criteria were willingness to participate in the study, being continent (screened using a validated pelvic floor questionnaire [10]), and having the ability to contract PFM correctly. This ability was assessed by palpation and by superficial biofeedback electromyography (PHENIX® USB NEO, VIVALTIS, France), reflecting the intensity and the length of the pelvic floor contraction on a monitor screen. Exclusion criteria were pregnancy, pelvic surgery including caesarean delivery, known neurological disease, or inability to understand instructions in Spanish.
All participants gave written consent to participate. This study was approved by the Galician Ethics Committee, conformed to the Declaration of Helsinki, and was registered at ClinicalTrials.Gov PRS Protocol Registration and Results System (ID:NCT04154527).
Experimental procedure
All subjects were tested by transvTAUS while lying in a supine position with the hips and knees slightly flexed and abducted, and with the lumbar spine in neutral position. A bladder filling protocol was implemented to ensure that the subjects had moderately full bladders (< 300 ml assessed by abdominal US using the formula described by Poston et al. [11]: height × depth × width × 0.7) to allow clear imaging of the pelvic floor fascia without subjects having an urge to urinate [12]. This protocol involved participants voiding 1 h before the assessment and then consuming 500 ml of water [13, 14].
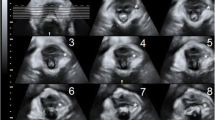
To image the pelvic floor, a 3.5-MHz curved linear array US transducer was used (LOGIQe Ultrasound, GE Healthcare, USA) with the US unit set in B mode. The same researcher, a qualified US technician and women’s health physiotherapist, examined all the participants. transvTAUS of the bladder was performed via the abdominal wall by placing the probe suprapubically on the lower abdomen in a transverse plane to the linea alba. The transducer was angled at 15–30 degrees from the vertical in a caudal posterior direction to obtain a clear image of the inferior-posterior aspect of the bladder [15] (see Fig. 1) and the midline pelvic floor structures (urethra, perineal body, rectum, etc.). The marker to measure the displacement was situated in the middle of the BB on the junction of the hyper- and hypo-echoic areas corresponding to the deep layer of PFM [16] (see Fig. 2c). A customized holder was used to achieve consistent transducer position and to ensure that the field remained constant during the whole exercising programme (see Fig. 1). A clasp locking mechanism was used as a holder, attached to an articulated arm and secured by a fastening strap. This arm was joined to a tripod by a swivel and secured by three locking knobs.
a Graphical User Interface of MATLAB software developed for the offline analysis of the displacement of the bladder base. b Display of the ultrasound video in 15 frames. c Displacement of the bladder base in cm. Position of the ultrasound marker at the beginning of the contraction (left side) compared to the position during the contraction (right side)
Both groups were instructed to randomly perform a series of six different PFM and abdominal contractions, all of them viable with the simultaneous assessment by the transabdominal ultrasound. Those contractions are quite common in the rehabilitation context in programmes of pilates and stabilization exercises, which have proved effective in reducing back pain and improving postural dysfunctions [17]. Table 1 describes the six types of contractions: contraction A requiring submaximal recruitment of PFM; contractions B, C, and F involving deep abdominal muscles (TrA and OI); and contractions D and E involving superficial abdominal muscles (OE and RA). Particularly contraction C meant an axial elongation of the whole spine (neutral position of the pelvic girdle, neutral spine, and the whole alignment of the posture). Contraction F, also known as the “abdominal vacuum exercise” or “stomach vacuum exercise”, involves exhaling all the air out of the lungs, bringing the stomach in as much as possible, and holding it while expanding the lower ribcage. Finally, contractions D and E involve the recruitment of the superficial abdominal muscles. For this reason, the intrabdominal pressure might be too high for the PFM contraction to lift the pelvic organs, and descent of the bladder might happen.
Subjects were instructed to contract PFM voluntarily at submaximal force prior to commencing contractions B, C, D, and E and to maintain this PFM contraction throughout each manoeuvre (Table 1, PFM_PRECONT = pelvic floor muscles pre-contraction held during the whole contraction). Each contraction (A–F) was repeated twice and the average displacement of the BB was recorded for data analysis. Inappropriate contractions (buttocks, thighs, RA) and Valsalva manoeuvres were corrected.
Electromyography biofeedback with superficial electrodes on the perineum and lower abdominal wall recorded the submaximal contraction of PFM and deep abdominis muscles. The participants were asked to perform maximum voluntary recruitment of PFM and TrA for normalization purposes. Subsequently, they tried submaximal contractions of both groups of muscles at 25–30% of their maximal force following the trajectory displayed on the biofeedback screen. Since the displacement of the posterior bladder wall resulting from PFM contraction was simultaneously being registered in the ultrasound (US) image, the subjects were blinded to the US screen to prevent them from altering their performance, thus avoiding a biofeedback effect of the US [13].
Data processing
A bespoke Graphical User Interface from the MATLAB software (The MathWorks, Inc., Natick, MA) was developed for the offline analysis of BB displacement obtained via TransvTAUS (see Fig. 2a). This application loads the anonymised US videos recorded during each contraction from a directory, removes the frames with no movement, and displays a collage of 15 overlapped representative frames on a horizontal grid (see Fig. 2b). The operator must mark the centre of the BB in two images, at the beginning of the contraction and when the maximum displacement of BB is observed. As US images are interpreted as a pixel-based coordinate system, the application obtains the displacement of BB by converting image coordinates to real-world coordinates (see Fig. 2c). The interface then conceals the results from the operator by directly exporting them into an Excel worksheet (Microsoft Corp., Redmond, WA) for further analysis.
Effect of contractions on BB position
The immediate effect of perineal and abdominal contractions on BB displacement was defined as the difference between its position measured during the contraction and its position at rest (see Fig. 2c). Therefore, a positive value represents an elevation of the BB and a negative value a descent of the BB during the contraction.
Statistical analysis
Statistical analysis of the data was performed using SPSS programme version 22. Participant characteristics were presented as frequencies, percentages, and means with standard deviation (SD). Statistical significance was inferred when P < 0.05.
The BB displacement data were grouped based on the contraction (A to F) and the study group (postpartum or nulliparous women). Descriptive statistical analyses (mean, standard deviation, range) were used to quantify the amount of displacement of the BB in cm that occurred for each contraction in each group. According to the Shapiro-Wilk test, normality could be assumed. Hence, a t-test for independent samples was employed for comparing the mean BB displacement during each contraction between groups, while Bonferroni post-hoc comparisons of an ANOVA test were used to compare BB displacement during different contractions within the same group of women.
The validity and reliability of the MATLAB algorithm were checked in a pilot study. In terms of validity, 27 nulliparous volunteers practising contraction A were assessed with the MATLAB algorithm and on the US monitor using electronic callipers. In both cases, the researcher followed the same procedure, placing the marker in the middle of the BB to measure the displacement between its position at rest and its final position in each manoeuvre. The agreement between these two measurements was assessed with a paired t-test, Pearson’s linear correlation coefficient (r), Lin’s concordance correlation coefficient (CCC), and intraclass correlation coefficient (ICC) (A, 2) following the notation according to McGraw K. et al. [13]. Finally, a Bland-Altman plot was constructed with the limits of agreement (LOA) calculated as LOA = d ± 1.96 s, where d is the sample mean of the differences and s the sample standard deviation.
To check the reliability of the algorithm, the interday intra-rater ICC coefficient was obtained by comparing the measurements of contractions A, B, C, and E between two sessions 1 week apart.
Results
Participants characteristics
Sixty-three women of Caucasian origin were included in this study and allocated into two groups: 35 in the nulliparous and 28 in the postpartum group. The mean age was 34.32 (SD = 4.34) years and 22.62 (SD = 3.07) years in the postpartum and nulliparous groups, respectively. The median body mass index was 23.01 (range 17 – 37 kg/m2) and 20.88 (range 17 – 30 kg/m2) in parous and nulliparous women, respectively. The average number of children in the postpartum group was 1.32 (33% had one child and 67% had two children). Only women delivered vaginally, between 6 to 12 weeks after birth, and continent women were included in the research. Any caesarean case and any women with dysfunctions were accepted to participate.
Contractions performance
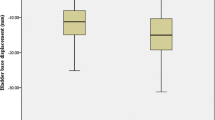
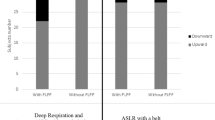
Comparison of BB displacement for the different contractions between parous and nulliparous women
A total of six different abdominal-perineal contractions (A–F) were evaluated in both study groups. Table 2 shows the descriptive statistics (mean, standard deviation, minimum, maximum) of the BB displacement (in cm) for each contraction in postpartum and nulliparous women, with their relevant 95% confidence intervals (CI). There was a significant condition-by-parity effect (P < 0.05) for BB displacement during contractions C, D, and E. Statistical analyses indicated significantly higher BB elevation during contraction C in postpartum participants, while the BB descended more in the postpartum group during contractions D and E compared to nulliparous women. For contractions A, B, and F, no significant differences in the BB displacement between both groups were observed (P = 0.57, P = 0.40, and P = 0.11, respectively).
Comparison of BB displacement in contraction pairs within each study group
The six contractions were compared in pairs within each group (Table 3). Post-hoc analyses indicated no significant differences in the BB displacement between contractions recruiting deep abdominal muscles, specifically A-B-C-F in the nulliparous group and A-B-F in the postpartum group, as in this latter group the BB elevation with contraction C was significantly higher than with contractions A and B (P < 0.05). The BB displacement of the contractions involving superficial abdominal recruitment (D-E) is significantly different to A-B-C-F contractions in both groups, since they are descending the bladder base. The BB decrease with contraction E was significantly higher than with D in both groups.
Validity and reliability of the MATLAB algorithm
To check the validity of the MATLAB algorithm, the absolute error between measurements (collected via electronic callipers on the screen and by the MATLAB algorithm) was calculated. The differences between both methods did not differ statistically from 0 (d = 0.037, P = 0.246) at a 5% significance level. Both the Pearson’s correlation coefficient (r = 0.97, P < 0.001) and Lin’s concordance correlation (CCC = 0.961) indicated a very strong relationship between the algorithm and electronic calliper measurements. The ICC was also high [ICC (A, 2) = 0.96, 95% CI = (0.92, 0.98)], further indicating good agreement between both methods. Figure 3 shows the Bland-Altman plot with LOA = (−0.35, 0.28)
Bland-Altman’s plot (n = 27 volunteers) with the differences between the measurements by the MATLAB algorithm and the ultrasound transducer on the y-axis plotted against the mean of the measures by both methods on the x-axis. Horizontal lines indicate the mean difference (\( \overline{d}=0.037 \)) and 95% confidence limits \( \left(\overline{d}-1.96 SD,\overline{d}+1.96 SD\right)=\left(-0.353,0.279\right) \)
.
In terms of reliability of the MATLAB calculations, the interday intra-rater coefficient obtained by the algorithm for contractions A, B, C, and E was ICC (1, 2) > 0.95 in all four manoeuvres [18] [ICC (1, 2) = 0.96, 0.98, 0.99, and 0.98 in contractions A, B, C, and E, respectively].
Discussion
To our knowledge, this is the first study to assess abdominal and pelvic floor contractions with US imaging in the early postpartum period in continent women, who had higher compliance and hysteresis of the pelvic connective tissue compared to nulliparous women. In our study, both groups were continent and without any pelvic floor dysfunction. Compared to other studies, participants might be incontinent or not at the early postpartum period. These reasons could explain some differences found comparing our results to other studies.
Effect of perineal and abdominal contractions on BB displacement in parous and nulliparous women
The results of the present study showed the immediate effect of specific abdominal and pelvic floor contractions on BB position. Performing a submaximal voluntary contraction of PFM, whether in isolation (contraction A), together with voluntary submaximal TrA (contraction B), or together with axial elongation of the back (contraction C), may provoke a lift effect in the BB in postpartum and nulliparous women. However, statistically significant differences between groups were only observed during contraction C. The study by Junginger et al. [18], which included nine continent women, found a similar lifting effect to that of contractions A and B, where significant bladder neck elevation occurred during concomitant PFM and gentle TrA contraction, with maximal PFM recruitment not recommended because of provocation of high intra-abdominal pressure. Additionally, histological studies reported that the composition of pelvic floor muscles involved mostly type I (slow-twitch) fibres, which are recruited by exercising at 25–30% of maximal force [19, 20]. Therefore, demanding the gentle recruitment of PFM and TrA seems to be appropriate during postpartum exercising.
Contraction C, which provoked the axial elongation of the whole spine, elevated the BB significantly, especially in the postpartum group. As far as we know, this effect of axial elongation on the BB or bladder neck position has not been reported before. Our results indicate that including axial strengthening of the spine might be recommendable in all postpartum exercises to protect pelvic organs from descending. However, further research is needed to assess this effect over time.
On the other hand, performing contraction D may provoke a descending effect in the BB in parous women. This contraction involves an isometric recruitment of all abdominal muscles, both deep (TrA and OI) and superficial (RA and OE), while keeping a submaximal PFM contraction. As far as we know, this contraction has not been studied before in the literature, despite being commonly included in fitness programmes in some western countries. Randomized controlled trials are required to assess the potential prolapsing effect of practising this abdominal contraction D over time.
Furthermore, the included curl-up contraction (Contraction E) showed a descending displacement of the BB in both groups (postpartum women −1.31 ± 0.57 cm, nulliparous women −0.66 ± 0.51 cm). Even when participants in both groups were continent, the BB descent was higher in postpartum women (P < 0.01), maybe due to the higher compliance observed in that group. Therefore, postpartum women may be at risk of pelvic organ prolapse when performing curl-up abdominal exercises repeatedly, but further research is needed to demonstrate their prolapsing effect in postpartum women when performed regularly. These findings in curl-up contraction were similar to those obtained by Barton et al. 2015 [13], where parous women displayed significantly more BB descent on average than nulliparous women (1.55 ± 0.73 cm vs. 1.14 ± 0.58 cm, P = 0.009). Of note, 60% of the participants in Barton’s study were incontinent, potentially explaining the greater difference observed.
Contraction F is commonly practised in fitness programmes but it has not yet been studied in the scientific literature. This contraction elevated the BB (0.78 ± 0.46 cm in postpartum women vs. 0.61 ± 0.47 cm in nulliparous women), but it was not statistically different from Contraction A (submaximal PFM contraction) in the nulliparous (P = 0.94) or the postpartum (P = 0.25) groups. However, Contraction F required high coordination to perform it properly. A lifting effect of the BB was also obtained by Navarro et al. [21] (0.68 cm, interquartile range = 0.37 cm) practising a similar abdominal manoeuvre called the hypopressive abdominal exercise in nulliparous women, as assessed by transabdominal US. Further research is needed to assess the potential protective effect of this contraction on the BB overtime.
Reliability and validation of TransvTAUS
In this study, a TransvTAUS was performed via the abdominal wall in a transverse view. Using this method to assess BB position in the course of contractions presents several clinical advantages compared to perineal US, as the patient does not need to undress and it is a completely non-invasive technique. TransvTAUS has showed to be a reliable method to measure the displacement of the BB during PFM contraction [22]. Murphy et al. [23] also obtained good intra-rater reliability for BB displacement measurements in the transverse plane during PFM contraction when using transabdominal US [ICC = 0.85, 95% CI = (0.72, 0.96)].
Sherburn et al. [22] and Murphy et al. [23] also found TransvTAUS to be a valid tool to assess the lifting or descending effect of PFM on the BB confirmed by digital palpation. They showed that the direction of the imaged displacement was in agreement with the direction of movement palpated by the investigator. Therefore, the direction of the displacement of the BB seems to be validated, but not the length of this displacement.
Besides, transperineal US is considered to be the gold standard due to its validation with lateral chain of urethrocystography [24] and video cystourethrography [25]. It also has the advantage of taking the measurements from a fixed bony landmark, while transabdominal US may reflect movement of the abdominal wall due to the lack of a bony reference point. To avoid any abdominal effect and minimize measurement errors in this trial, a customized holder was designed to secure the US probe throughout the measuring process. However, the reliability of this holder has not been studied yet, so further research is needed.
Validity and reliability of the MATLAB algorithm
Nearly all former studies assessing BB displacement through the abdominal wall used electronic callipers on the US screen [14, 15, 24], a method that can be very time-consuming during clinical sessions. In contrast, our research team developed a new MATLAB algorithm (Ecolab) for improving the measurement process. High agreement [ICC = 0.96, 95% CI = (0.92, 0.98)] was found between the newly designed algorithm and the conventional manual procedure, indicating good precision for the algorithm for measuring BB displacement compared to electronic callipers on the US screen. The good correlation observed between both procedures and high reliability during contractions A, B, C, and E (ICC > 0.90 in all four manoeuvres) makes the MATLAB algorithm a valid and reliable tool for measuring BB displacement. Implementing this new algorithm in the clinical setting could provide several advantages, including the automatic saving of the results in a spreadsheet and the ability to perform the measurement offline, which overcomes the need for the patient to be present during the measurement.
Limitations
There are some potential limitations to this study. First, compared to transperineal US, which has been considered the gold standard for assessing bladder neck displacement in functional activities [24], the employed US technique does not have a fixed reference point. Hence, BB displacement can only be expressed relative to a potentially mobile starting point. To achieve accurate and repeatable measurements, the transducer position needs to be consistent. In line with this recommendation, Whittaker et al. 2009 [26] showed that non-statistically significant (P > 0.05) changes in measurements of the BB position occur if the transducer motion is kept below approximately 5 to 10 degrees of angular motion or 10 mm of inward/outward motion. These findings provide guidance on acceptable amounts of transducer motion relative to the pelvis when recording measurements of BB displacement.
Another limitation stems from using surface electromyogram electrodes in perineal and abdominal registration, as these electrodes are supposed to be less accurate and cannot differentiate between OI and TrA. Only one study was found to use a combination of surface and fine-wire recordings [19], a potentially more accurate method. Muscle recruitment parameters are unclear in most studies. In our study, participants were asked to achieve 25–30% of maximal recruitment during abdominal and PFM contractions as registered by electromyography feedback with surface electrodes and visualized on a monitor screen.
Implications for clinical practice
These results revealed which contractions appear to be safer and appropriate for training PFM and abdominal muscles at the early postnatal period, which can help therapists to design evidence-based exercising programmes for parous women taking into consideration the high postpartum compliance in the connective tissue and also help prevent the practice of exercises harmful for the pelvic organs. However, future research is needed to compare these effects between vaginal and caesarean parous women as well as for assessing long-term effects.
Conclusions
The overall results of this study showed different immediate effects of the perineal and superficial abdominal versus deep abdominal contractions on BB displacement in parous and nulliparous women. Performing perineal and deep abdominal muscle contractions led to a lifting effect on the BB, while perineal and superficial abdominal muscle contractions provoked an immediate descent of the BB in both groups.
Comparing parous and nulliparous women, the BB was observed to elevate significantly in the postpartum group when performing submaximal PFM and TrA contraction simultaneously with axial elongation of the back. Therefore, including this contraction in postpartum programmes is recommendable. In contrast, the BB was found to descend significantly during a curl-up contraction in both groups and therefore must be avoided in postpartum programmes as it may ease prolapse. Although these results provide guidelines on the adequacy of postpartum exercises, only the immediate effects on the displacement of the BB were measured. Further randomized clinical trials assessing the effect of perineal and abdominal contractions in postpartum women are warranted to demonstrate their long-term effectiveness.
In addition, the MATLAB algorithm proved to be a highly reliable tool and therefore is likely to be useful for further studies in pelvic floor and abdominal contractions.
Abbreviations
- BB:
-
Bladder base
- ICC:
-
Intraclass correlation coefficient
- OI:
-
Obliquus internus muscle
- OE:
-
Obliquus externus muscle
- PFM:
-
Pelvic floor muscles
- RA:
-
Rectus abdominis muscle
- TrA:
-
Transversus abdominis muscle
- US:
-
Ultrasound
- TransvTAUS:
-
Transverse transabdominal ultrasound
References
Wijma J, Weis Potters AE, van der Mark T, Tinga D, Aarnoudse J. Displacement and recovery of the vesical neck position during pregnancy and after childbirth. Neurol Urodyn. 2008;26:372–6.
Woodley SJ, Lawrenson P, Boyle R, Cody JD, Morkved S, Kernohan A, et al. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD007471.pub4.
Deffieux X, Vieillefosse S, Billecocq S, Battut A, Nizard J, Coulm B, et al. Postpartum pelvic floor muscle training and abdominal rehabilitation: guidelines. Gynecol Obstet Biol Reprod. 2015;44(10):1141–6. https://doi.org/10.1016/j.jgyn.2015.09.023.
Gluppe SL, Hilde G, Tennfjord MK, Engh MA, Bo K. Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: a randomized controlled trial. Phys Ther. 2018;98(4):260–8.
Guillard S, Ryan C, Stokes M, Warner M, Ewings S, Dixon J. Immediate effects on lateral abdominal muscle exercises in different postural positions on the inter-recti distance in parous women. Physiotherapy. 2018;105(suppl 1):E14. https://doi.org/10.1016/j.physio.2018.11.253.
Coldron Y, Stokes MJ, Di J, Newham KC. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. 2008;13(2):112–21.
Weis CA, Triano JJ, Barrett J, Campbell MB, et al. Ultrasound assessment of abdominal muscle thickness in postpartum vs nulliparous women. J Manip Physiol Ther. 2015;38(5):352–7.
Okamoto M, Murayama R, Haruna M, Matsuzaki M. Evaluation of pelvic floor function by transabdominal ultrasound in postpartum women. JMU. 2010;37:187–93.
Mota P, Pascoal A, Carita AI, Bo K. The immediate effects on inter-rectus distance of abdominal crunch and drawing-in exercises during pregnancy and the postpartum period. J Orthop Sports Phys Ther. 2015;45(10):781–8.
Busquets M, Serra R. Validation of a Spanish version of the international consultation on incontinence questionnaire short-form (ICIQ-SF). Rev Med Chil. 2012;140:340–6.
Poston GJ, Joseph AEA, Riddle PT. The accuracy of ultrasound in measurement of changes in bladder volume. Br J Urol. 1983;55(4):361–3.
Baessler K, Junginger B. Traditional gymnastic exercises for the pelvic floor often Lead to bladder neck descent -a study using perineal ultrasound. Geburtshilfe Frauenheilkd. 2017;77(07):765–70.
Barton A, Serrao C, Thompson T, Briffa K. Transabdominal ultrasound to assess pelvic floor muscle performance during abdominal curl in exercising women. Int Urogynecol J. 2015;26(12):1789–95.
Thompson JA, O’Sullivan PB, Briffa K, Neumann P, Court S. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(4):285–92.
Bo K, Sherburn M, Allen T. Transabdominal ultrasound measurement of pelvic floor muscle activity when activated directly or via a TrA contraction. Neurourol Urodyn. 2003;22(6):582–8.
Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional maneuvers in continent and incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:779–86.
Yamato TP, Maher CG, Saragiotto BT. Pilates for low back pain. Cochrane Database Syst Rev. 2015;7:CD010265.
Martínez-Bustelo S (2016) Transabdominal functional echography of the pelvic floor. Dissertation, International Symposium on Rehabilitative Ultrasound Imaging, Madrid.
Junginger B, Baessler K, Sapsford R, Hodges P. Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J Pelvic Floor Dysfunct. 2010. https://doi.org/10.1007/s00192-009-0981-z.
Gilpin SA, Gosling JA, Smith ARB, Warrel DW. The pathogenesis of genitourinary prolapse and stress incontinence of urine. A histological and histochemical study. BJOG. 1989;96(1):15–23.
Navarro B, Torres M, Arranz B, Sanchez O. Muscle response during a hypopressive contraction after pelvic floor physiotherapy: Assesssment with transabdominal ultrasound. Fisioterapia. 2017;39(5):187–94.
Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP. Investigation of transabdominal real-time ultrasound to visualise the muscles of the pelvic floor. Aust J Physiother. 2005;51:167–70.
Murphy C, Sherburn M, Allen T (2002) Investigation of transabdominal diagnostic ultrasound as a clinical tool and outcome measure in the conservative measurement of pelvic floor muscle dysfunction. In: Proceedings of the International Continence Society Meeting, Heidelberg, Abstract 129, p 61.
Schaer GN, Koechli OR, Shuessler B, Haller U. Perineal ultrasound for evaluating the bladder neck in urinary stress incontinence. Obstet Gynaecol. 1995;85:220–4.
Dietz H, Wilson P. Anatomical assessment of the bladder outlet and proximal urethra using ultrasound and video-cystourethrography. Int Urogynecol J. 1998;9:365–9.
Whittaker JL, Warner MB, Stokes MJ. Induced transducer orientation during ultrasound imaging: effects on abdominal muscle thickness and bladder position. Ultrasound Med Biol. 2009;35:1803–11.
Acknowledgments
The authors acknowledge PRIM S.A. (Spain) for their support by providing the US logiq-E equipment and PHENIX®, VIVALTIS (France) for providing the PHENIX USB NEO Biofeedback apparatus for the data collection of this research.
The authors also acknowledge the midwives from San José Health Center, Galician Healthcare Service (A Coruña, Spain), for their contribution to recruiting subjects and providing the clinical setting during the data collection.
Funding
The authors thank COFIGA (Colegio Oficial de Fisioterapeutas de Galicia) for funding this research (Research Grant 2018–2019 modality B).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martínez-Bustelo, S., Ferri-Morales, A., Corral-Gómez, L. et al. Transabdominal ultrasound to assess the displacement of the bladder base during abdominal and pelvic floor contractions in continent parous versus nulliparous women. Int Urogynecol J 33, 2257–2266 (2022). https://doi.org/10.1007/s00192-021-04756-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04756-4