Abstract
The aims of the study were (1) to assess the reliability of transabdominal (TA) and transperineal (TP) ultrasound during a pelvic floor muscle (PFM) contraction and Valsalva manoeuvre and (2) to compare TA ultrasound with TP ultrasound for predicting the direction and magnitude of bladder neck movement in a mixed subject population. A qualified sonographer assessed 120 women using both TA and TP ultrasound. Ten women were tested on two occasions for reliability. The reliability during PFM was excellent for both methods. TP ultrasound was more reliable than TA ultrasound during Valsalva. The percentage agreement between TA and TP ultrasound for assessing the direction of movement was 85% during PFM contraction, 100% during Valsalva. There were significant correlations between the magnitude of the measurements taken using TA and TP ultrasound and significant correlations with PFM strength assessed by digital palpation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A correct pelvic floor muscle (PFM) contraction has been described as an inward lift and squeeze around the urethra with resultant urethral closure, stabilization and resistance to downward movement [1]. As elevation of the bladder neck is critical for the maintenance of continence, PFM exercises must emphasise elevation and not depression of the pelvic floor (PF). Many women find it difficult to perform a correct PFM contraction that results in an inward lift of the PF [2–4]. Studies have shown that only 36–49% of women with incontinence and prolapse can produce a correct PFM contraction [4–6] and 25–38% of subjects use a Valsalva or straining effort [4, 5]. In a study using transabdominal ultrasound to observe PF movement, PF depression was observed in 43% of women with incontinence and prolapse when attempting to elevate the PFM [7].
Ultrasound gives direct visualization of PFM contraction and can be used as an adjunct to the standard physiotherapy assessment of women with PFM dysfunction to assess PF elevation. The most common methods of ultrasound used by physiotherapists are transperineal ultrasound (TP) and transabdominal (TA) ultrasound. Transperineal ultrasound was established as a reliable method of evaluating women with incontinence [8–15]. More recently, TA ultrasound has been used by physiotherapists to assess the “lifting” aspect of the pelvic floor by observing movement of the bladder base during PFM exercises [16–20] and good intra and inter-rater reliability for the measurement of displacement of the bladder base during a PFM contraction was reported [21].
To date, the reliability of TA ultrasound during other manoeuvres has not been reported and there are no reports comparing TA with TP ultrasound as a method of assessment for women with PFM dysfunction. As these two methods assess the PFM at different anatomical sites, it is important to establish whether elevation of the bladder base as measured using TA ultrasound reflects elevation of the bladder neck measured using TP ultrasound.
The aims of the study were (1) to assess the reliability of TA and TP ultrasound during a PFM contraction and a Valsalva manoeuvre and (2) to compare TA ultrasound with TP ultrasound for predicting the direction and magnitude of bladder neck movement in a mixed subject population.
Method
A cross sectional study design was used to compare TA with TP ultrasound. One hundred and twenty women were recruited from the local Perth metropolitan community. All gave written informed consent. A cross section of women were recruited to include nulliparous and parous asymptomatic women who had not previously had any PFM training and women with incontinence who had not undergone any PFM training during the last 2 years. The aim of the study was not to correct the technique of performing PFM contractions but to assess the two methods of ultrasound at measuring the movement; therefore, women performing an incorrect technique of PFM contraction were still included. Other inclusion criteria were age 20–55 years and pre menopausal or on hormone replacement therapy. Exclusion criteria were pregnancy, urinary tract infection, vaginal infection, known neurological disorders and an inability to understand English. The study received ethical approval from the Human Research Ethics Committee, Curtin University of Technology. All women were interviewed by telephone and questioned regarding any urinary leakage using the incontinence severity index (ISI) questionnaire [22]. Sixty women (30 nulliparous and 30 parous) had no symptoms of incontinence (ISI score=0) and 60 women reported symptoms of incontinence (ISI score > 0). Urinary incontinence was assessed using a urinary symptoms questionnaire [23]. Thirty women had stress incontinence and 30 women had urge incontinence.
All of the women were assessed in supine crook lying, with one pillow underneath the head. The hips and knees were flexed to 60° and the lumbar spine was positioned in neutral. The aim was to assess all the women with a comfortably full bladder. To this end, standardized instructions were given to all the women to void 1 h before testing and then to drink 500 ml of water and not to void again until after the test. All women were assessed by the same qualified sonographer for all the tests using high definition imaging (Philips HDI Sono 5000CT) with two-curved linear array probes (5–2 MHz, 7–4 MHz) using both the TA and TP approach. Ten asymptomatic women were tested on two occasions 1 week apart for reliability.
Transperineal imaging was performed with the ultrasound transducer placed in the mid sagittal plane at the perineum (Fig. 1). A measure of the position of the bladder neck was taken at rest and the change from the resting position was measured (Fig. 2) during the different manoeuvres using the standardized method described by Schaer [9]. The measurements were entered in a computer spread sheet and the cranio ventral (CV) bladder neck lift or dorso-caudal (DC) descent were calculated using the method described by Dietz [24] and shown in Fig. 4. TA ultrasound was performed by placing the probe supra-pubically, on the lower abdomen, in the mid-sagittal plane as shown in Fig. 1. The transducer was angled in a caudal/posterior direction to obtain a clear image of the inferior–posterior aspect of the bladder (Fig. 3). A marker was placed on the bladder base at the region of the greatest displacement visualized during a PFM contraction. A marker was placed on the bladder base at rest and the displacement of the fascia from the resting position at the end of each manoeuvre was measured using the on screen calipers.
Transperineal ultrasound assessment of bladder neck position at rest and during PFM contraction and Valsalva. The measurement graph for calculation of vector length during Valsalva is shown. The displacement is measured by calculating a vector from the resting position (x1y1) to the position at the end of the manoeuvre (x2y2) using the formula: vector length a2=b2 +c2 (where b=y1−y2and c=x1−x2)
Two tasks were performed: a PFM contraction and a Valsalva manoeuvre. The subjects were asked to: (1) draw in and lift the pelvic floor muscles and (2) to perform a maximal Valsalva manoeuvre, the strength was not standardized but subjects were encouraged to perform their maximal straining effort. The measurements were made using the TP approach initially and then were repeated using a TA approach. The subjects were not allowed to observe the ultrasound screen until after the completion of all test measurements as the aim was not to train the PFM, but to measure the test manoeuvres with the two methods. The order in which the test manoeuvres were performed was determined by computer-generated random order selection but the same order was used for a single subject for both methods. The tests were repeated thrice and a mean was taken for each test. The PFM muscles were assessed by digital vaginal palpation and the strength of the PFM contraction was graded using the five point modified Oxford scale as described by Sapsford [25].
Statistical analysis of the data was performed using SPSS (V10). The reliability of both methods was assessed using intraclass correlations (ICC (2,3)) from the duplicate measures on ten volunteers tested one week apart and the standard error of the measurements (SEM) for both methods were calculated.
When assessing for a correct PFM contraction, the direction of the movement is critical. In this study, we wanted to assess the ability of TA ultrasound to predict the direction of movement of the bladder neck as measured by TP ultrasound. The subjects were therefore classified into two categories according to whether they elevated or depressed the bladder neck or pelvic floor. The measure of agreement of both ultrasound methods for direction of movement was assessed using the Kappa statistic. Where a Kappa could not be calculated because the majority of the movements were in the same direction, as during Valsalva, percentage of agreement was reported.
The association between measurements made using the different ultrasound methods was determined using Pearson’s coefficient of correlation. Correlations were also calculated for the subgroups of continent and incontinent women to establish whether the association was comparable in both subgroups. It was not expected that the magnitude of the movement for the two US measures would be the same as different anatomical structures were being measured.
The standard clinical method of PFM assessment is manual muscle testing by digital palpation. The association between the measurements taken during a PFM contraction using both methods of ultrasound and PFM strength assessed by digital palpation was assessed using Spearman’s coefficient of correlation.
Results
One hundred and twenty women with a mean (SD) age of 43 (7) years, BMI 24 (4) kg.m2 and a median parity of 2 (range 0–5) were assessed. The reliability of TP compared with TA ultrasound for the ten subjects between trial 1 and 2 for both test manoeuvres is presented in Table 1 showing the intraclass correlations (ICC) and SEM. Transperineal ultrasound showed good reliability ICC (SEM) for both PFM contractions (0.91(0.11)) and Valsalva (0.87(0.16)). TA ultrasound showed good reliability for measurements taken with PFM contraction (0.93 (0.13)) but it was found to be less reliable than TP ultrasound for measurement made during Valsalva manoeuvre and had larger measurement errors (0.51(0.35)).
When the movement of the pelvic floor or bladder neck was classified as “elevation” or “depression”, the measure of agreement of both ultrasound methods for direction of movement is shown in Table 2. There was a significant agreement between TA and TP ultrasound for assessing the direction of movement during PFM contraction (Kappa=0.56 P<0.0001). The percentage agreement between TA and TP ultrasound was 85% during PFM contraction and 100% during Valsalva.
During PFM contraction, there were divergent measures in 18 subjects, 10 subjects depressed the bladder neck on TP ultrasound with elevation of the bladder base on TA ultrasound, and eight subjects elevated the bladder neck on TP ultrasound and depressed the bladder base on TA ultrasound. These divergent measures were distributed across asymptomatic and incontinent subjects as shown in Table 3.
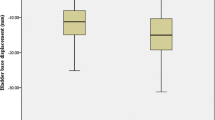
The measurements taken using both methods of ultrasound during PFM contraction and Valsalva manoeuvre and the strength of the PFM assessed by digital palpation for all subjects is summarized in Table 4. There were significant correlations between TA and TP ultrasound for PFM contraction (r=0.63, P<0.0001) and Valsalva (r=0.69, P<0.0001) (Table 5, Fig. 5). The correlations were significant in both the continent (PFM contraction (r=0.58, P< 0.0001) and Valsalva (r=0.73, P<0.0001)) and incontinent (PFM contraction (r=0.64, P<0.0001) and Valsalva (r=0.60, P<0.0001)) groups (Table 5, Fig. 5).
There was also a significant correlation between manual muscle testing and both TA (rho=0.49, P<0.0001) and TP (rho=0.58, P<0.0001) ultrasound measurements.
Discussion
Real time ultrasound provides direct visualization of the PFM contraction to both the therapist and patient and therefore provides a useful biofeedback method to teach the correct technique of performing PFM exercises that result in a “lifting” contraction also it allows the amount of movement of the bladder neck and/or bladder base during PFM contraction to be quantified.
In our study, the reliability of TA ultrasound was excellent and comparable to TP ultrasound for measuring PF movement during PFM contraction. TP ultrasound was found to be more reliable than TA ultrasound for measuring movement of the pelvic floor during Valsalva manoeuvre. The reduced reliability during Valsalva using TA ultrasound may have been due to greater movement of the probe over the abdomen or the fact that the inferior posterior aspect of the bladder is susceptible to changes in intra-abdominal pressure (IAP) [26]. The intra and inter-rater reliability of both methods of ultrasound have previously been investigated separately and good reliability for TP ultrasound during PFM contraction and Valsalva manoeuvre [9, 27, 28] were reported. Previous studies of reliability for TP ultrasound during Valsalva have controlled for IAP [9, 28]. Intra abdominal pressure was not measured in the current study as the intention of this study was to assess the clinical utility of both methods of ultrasound.
In a previous study of the intra and inter-rater reliability of TA ultrasound, good inter-rater reliability for measurement made during PFM contraction was reported [21]. In the same study, the sagittal and transverse views were compared and the sagittal view was found to be more reliable for measurements made during PFM contraction [21]. In our study, only the intra-rater reliability of TA ultrasound in the sagittal view was investigated. Thus, inter-rater reliability and comparison of the transverse and sagittal views for Valsalva manoeuvre warrant further investigation.
In this study, it is important to note that the scans were performed by a qualified sonographer with considerable experience using high quality equipment. It may be that health professionals who are not specifically trained in ultrasound scanning, using less sophisticated equipment commonly found in physiotherapy practices, may not obtain such reliable results.
In a previous study, we reported depression of the PF during PFM contraction observed using TA ultrasound [18] but this is the first study to report women depressing the bladder neck on PFM contraction using TP ultrasound. In previous studies using TP ultrasound, the subjects were able to observe the PFM contraction and the best contraction was used for assessment [11, 13, 14, 27, 29]. In some studies, subjects were coached to ensure a PFM contraction that resulted in bladder neck elevation [13, 27]. These strategies may have resulted in the exclusion of subjects performing PFM contractions incorrectly, whereas they were included in our study.
We have shown that TA ultrasound was able to predict the direction of bladder neck movement measured by TP ultrasound in the great majority of cases, but divergent measures did occur during PFM contraction in both the continent and incontinent groups. There may be several reasons for these divergent measures during PFM contraction such as measurement error, inconsistent subject performance or the lack of a fixed reference point for TA ultrasound. Outward movement of the abdominal wall moves the US transducer away from the structures of interest and may give the impression of depression of the bladder base. In this study, the US probe was held firmly against the abdominal wall with the aim of limiting movement of the probe, but error due to outward abdominal movement cannot be ruled out as a possible confounding factor.
Divergent measures may also reflect genuine divergent movement of the PF at the two anatomical sites. A “squeezing” contraction of the PFM may result in an anterior movement of the pubo-rectal sling without elevation of the bladder neck. Conversely, it is possible that elevation of the bladder neck may be observed in TP ultrasound with depression of the bladder base on TA ultrasound because of raised IAP. Our recent research has shown depression of the bladder base as measured by TA ultrasound occurs secondary to large increases in IAP and is associated with co-contraction of the PFM, chest wall and abdominal wall muscles [26]. To clarify these issues, simultaneous measures using both TA and TP ultrasound would have to be made. This methodological issue is a limitation of the current study design but technological issues with ultrasound would preclude simultaneous measurement.
There was good agreement between the two methods for assessing the magnitude of the movement during PFM contraction and Valsalva and a significant correlation between manual muscle testing and the measurements made with both methods of ultrasound. The correlation of manual muscle testing with TP ultrasound was slightly less than that reported by Dietz et al. [30] This could be explained by our inclusion of all women performing correct and incorrect levator contractions. It appears that the strength of muscle contraction and the ability to perform an elevating contraction, although correlated, assess two different aspects of a PFM contraction. The PFM muscles can contract strongly but incorrectly or conversely an elevating PFM contraction can be performed correctly even if the muscles are weak.
In the clinical physiotherapy setting, when using ultrasound for biofeedback, TP ultrasound has the advantage of allowing good visualization of bladder neck and taking all measurements from a fixed bony landmark, this makes it more reliable for comparisons between subjects. The disadvantages of TP ultrasound are that it requires specific training and practice to perform the technique consistently, the measures are more complex and time consuming to calculate, the images rendered require experience to interpret and the location of the probe on the perineum is more invasive and may limit some functional manoeuvres.
By comparison, the advantages of TA ultrasound are the relative ease to learn the technique, take measures and interpret the images for biofeedback purposes. Furthermore, the probe placement does not restrict movement of the lower limbs, which is important when assessing subjects with lumbo-pelvic pain [17]. The technique is totally non-invasive and the patient does not need to get undressed. This may be important in specific populations where internal examination may not be desirable, e.g. children, adolescents, men, victims of sexual abuse and some ethnic groups. TA ultrasound gives an alternative approach to learning PFM exercises in some women where the reluctance to undergo internal examination may be a barrier to them seeking professional help for incontinence. However, TA ultrasound does not allow visualisation of the bladder neck directly. It requires a full bladder, which may be difficult in women with a reduced functional bladder capacity or bladder urgency, and it may be difficult to obtain a clear image in women with dense abdominal scar tissue. Furthermore, movement of the bladder base does not always reflect movement at the bladder neck; in some instances, it may reflect outward movement of the abdominal wall instead due to lack of a bony reference point. Difficulty visualizing the bladder in obese women using the TA technique was previously reported [31]. But we were able to visualize the inferior posterior aspect of the bladder clearly in all women (BMI range 17–39).
As a clinical tool, TA ultrasound is vastly more expensive than the standard practice of digital vaginal examination and requires training in the use of the ultrasound equipment. If TA ultrasound is used alone, without local assessment of the vulval skin and vaginal walls, it does not allow for assessment of vaginal atrophy, vaginal wall prolapse, size of the uro-genital hiatus, sensory deficit, PFM tone, symmetry of PFM contraction and PFM muscle strength. As there is no bony landmark, it is not possible to assess the resting tone or starting position of a pelvic floor muscle contraction. Limited movement of the PFM may represent high resting tone as well as poor pelvic muscle elevation/movement.
Conclusion
Both transperineal and transabdominal ultrasound were shown to be reliable at measuring movement during a PFM contraction. Transperineal ultrasound is more reliable than TA ultrasound for measuring movement during Valsalva. Transperineal ultrasound is more reliable for inter subject comparisons as it measures from a fixed bony landmark; however, the technique is more complicated to learn and the measurements are more time consuming to calculate in a clinical setting. The location of the probe on the perineum may limit some functional manoeuvres. Transabdominal ultrasound is totally non-invasive and the patient does not need to undress, the technique is quick to perform and is relatively easy to learn. Transabdominal ultrasound predicts the direction bladder neck movement in the majority of women and correlates with TP ultrasound for measuring the magnitude of the movement of the pelvic floor. Transabdominal ultrasound gives an alternative approach to PFM assessment in specific populations where internal examination may not be appropriate or desirable. Clinically, it may be a useful tool for the functional assessment and physiotherapy management of women with incontinence and prolapse as it gives good visual feedback to therapist and patient for retraining the pelvic floor muscles.
References
Bo K et al (2001) Dynamic MRI of the pelvic floor muscles in upright sitting. Neurourol Urodyn 20:167–174
Bo K et al (1988) Knowledge about and ability to correct pelvic floor muscle exercises in women with urinary stress incontinence. Neurourol Urodyn 7:261–262
Benvenuti F et al (1987) Re-educative treatment of genuine stress incontinence. Am J Phys Med 66:155–168
Bump RC et al (1991) Assessment of Kegel pelvic muscle exercise performance after brief verbal instruction. Am J Obstet Gynecol 165(2):322–327; discussion 327–329
Theofrastous JP et al (1997) Relationship between urethral and vaginal pressures during pelvic muscle contraction. The Continence Program for Women Research Group. Neurourol Urodyn 16(6):553–558
Van Loenen N, Vierhout M (1997) Augmentation of urethral pressure profile by voluntary pelvic floor contraction. Int Urogynecol J 8:284–287
Thompson J, O’Sullivan P (2003) Levator plate movement during voluntary pelvic floor muscle contraction in subjects with incontinence and prolapse: a cross sectional study and review. Int Urogynecol J 12(4):84–88
Koelbl H, Bernaschek G (1989) A new method for sonographic urethrocystography and simultaneous pressure-flow measurements. Obstet Gynecol 74(3 Pt 1):417–422
Schaer G et al (1995) Perineal ultrasound for evaluating the bladder neck in urinary stress incontinence. Obstet Gynaecol 85:220–224
Schaer GN et al (1996) Perineal ultrasound: determination of reliable examination procedures. Ultrasound Obstet Gynecol 7(5):347–352
Peschers U et al (1996) Changes in vesical neck mobility following vaginal delivery. Obstet Gynaecol 88:1001–1006
Dietz H, Wilson P (1998) Anatomical assessment of the bladder outlet and proximal urethra using ultrasound and video-cystourethrography. Int Urogynecol J 9:365–369
Dietz HP, Wilson PD, Clarke B (2001) The use of perineal ultrasound to quantify levator activity and teach pelvic floor muscle exercises. Int Urogynecol J Pelvic Floor Dysfunct. 12(3):166–168; discussion 168–9
Dietz HP, Steensma AB, Vancaillie TG (2003) Levator function in nulliparous women. Int Urogynecol J Pelvic Floor Dysfunct 14(1):24–26; discussion 26
Brandt F et al (2000) Perineal assessment of the urethrovesical junction mobility in young continent females. Int Urogynecol J 11:18–22
Bo K, Sherburn M, Allen T (2003) Transabdominal ultrasound measurement of pelvic floor muscle activity when activated directly or via a transversus abdominis muscle contraction. Neurourol Urodyn 22(6):582–588
O’Sullivan PB et al (2002) Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine 27(1):E1–E8
Thompson J, O’Sullivan P (2003) Levator plate movement during voluntary pelvic floor muscle contraction in subjects with incontinence and prolapse: a cross sectional study and review. Int Urogynecol J 12(4):84–88
Thompson J et al (2003) A comparison between transabdominal and transperineal ultrasound in the assessment of women performing pelvic floor exercises. Aust N Z Continence J 9(4):92–93
Thompson J et al (2004) Pelvic floor elevation during pelvic floor muscle contraction in women with incontinence and normal controls. ICS web site. In: Proceedings of the joint ICS/ IUGA meeting, August, Paris
Murphy C, Sherburn M, Allen T (2002) Investigation of transabdominal diagnostic ultrasound as a clinical tool and outcome measure in the conservative measurement of pelvic floor muscle dysfunction. In: Proceedings of the international continence society meeting, Heidelberg, Abstract 129, p 61
Sandvik H et al (1993) Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health 47(6):497–499
Ishiko O et al (2000) The urinary incontinence score in the diagnosis of female urinary incontinence. Int J Gynaecol Obstet 68:131–137
Dietz H, Wilson P, Clarke B (2001) The use of perineal ultrasound to quantify levator activity and teach pelvic floor muscle exercises. Int Urogynecol J 12:166–169
Sapsford R, Bullock-Saxton J, Markwell S (1998) Women’s health. A textbook for physiotherapists. WB Saunders, London
Thompson J et al (2004) Motor control strategies involved in pelvic floor elevation and depression. ICS web site. In: Proceedings of the joint ICS/ IUGA meeting, August, Paris
Dietz HP (2004) Levator function before and after childbirth. Aust N Z J Obstet Gynaecol 44(1):19–23
Peschers UM et al (2001) Bladder neck mobility in continent nulliparous women. BJOG 108(3):320–324
Peschers UM et al (1997) Levator ani function before and after childbirth. Br J Obstet Gynaecol 104(9):1004–1008
Dietz HP, Jarvis SK, Vancaillie TG (2002) The assessment of levator muscle strength: a validation of three ultrasound techniques. Int Urogynecol J Pelvic Floor Dysfunct 13(3):156–159; discussion 159
White R et al (1980) Real-time ultrasonography in the evaluation of urinary stress incontinence. Am J Obstet Gynecol 138:235–239
Acknowledgements
The authors thank Curtin University Postgraduate Scholarship Awards and the Physiotherapy Research Foundation of Australia for financial assistance. The support from Dr Anthony Murphy for use of ultrasound equipment, Nicole David for the preparation of the graphics and Ritu Gupta for statistical advice is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thompson, J.A., O’Sullivan, P.B., Briffa, K. et al. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. Int Urogynecol J 16, 285–292 (2005). https://doi.org/10.1007/s00192-005-1308-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-005-1308-3