Abstract
Introduction and hypothesis
We used clinical examination and transperineal 3D/4D ultrasound (US) to evaluate pelvic floor muscles (PFM) after different delivery modes.
Methods
Women were surveyed using validated questionnaires. PFM were evaluated and classified according to the Modified Oxford Scale following 3D/4D transperineal US. For statistical analysis, Kruskal–Wallis, Mann–Whitney, chi-square, and Fisher exact tests were used.
Results
Fifty-three women were evaluated: 32 with previous vaginal delivery (VD) and 21 with cesarean section (CS) (8 nonelective and 13 elective). No significant difference among groups was observed regarding urinary incontinence (UI) after delivery (p = 0.39), loss of muscle strength referred by the patient (p = 0.48), or evaluated through digital examination (p = 0.87). No patient with elective CS had avulsion, with difference between VD and elective CS (p = 0.008). US evaluation identified no differences in bladder-neck elevation (p = 0.69) or descent (p = 0.65) , and no difference in genital hiatus size (p = 0.35), levator ani thickness (p = 0.35 –0.44), or presence of major or minor levator ani avulsion (p = 0.10).
Conclusions
We evaluated primiparous women within 12 to 24 months of delivery and found that VD was associated with PFM avulsion. There was no difference among VD and nonelective or elective CS in symptomatology or other anatomic alterations evaluated through 3D/4D transperineal US.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic floor dysfunction (PFD) is a disorder that includes pelvic organ prolapse (POP), urinary incontinence (UI), fecal incontinence (FI), and overactive bladder (OAB) syndrome [1]. The prevalence of these dysfunctions is elevated and has a great impact on women’s quality of life (QoL). In 2010, 28 million women in the United States presented with PFD, and it is believed that this number may increase to 43 million by 2050 [2]. Of the various risk factors associated with the incidence of PFD, vaginal delivery (VD) is considered to be the main contributor to pelvic floor dysfunction compared with cesarean section (CS) [3]. A systematic review and metanalysis of women with UI, with a follow-up period longer than 1 year after delivery, showed that VD was associated with a two-fold risk of developing stress urinary incontinence (SUI) compared with CS and a three-fold risk compared with elective CS, showing a 10% increase in risk [4].
VD appears to have a considerable impact on pelvic floor muscles (PFM). During labor and delivery, excessive stretching of the PFM, especially the levator ani, with direct injury to the muscle, might have an important impact on pelvic muscle support [2]. Pelvic denervation may also contribute to levator ani inefficiency, which would diminish urethral support and consequently induce UI with or without pelvic organ prolapse [5]. Therefore, it is believed that CS, especially elective CS, could have a protective effect on the perineal trauma associated with labor and delivery [6].
The 3D/4D ultrasound is used as a tool to evaluate patients with PFD. It is a simple and accessible method, radiation-free, minimally invasive, cost-effective and has the benefit of providing a real-time and dynamic appraisal of the pelvic floor [7].
Despite growing evidence in the literature, there is still great controversy on the real impact of labor and delivery mode on the occurrence of pelvic floor dysfunctions and anatomic recovery in the long run. The objective of this study was to evaluate, through clinical examination and transperineal 3D/4D US, the ,s after the different delivery modes.
Materials and methods
This is a cross-section study of primiparous women with a history of delivery at the Women’s Hospital Professor Doctor José Aristodemo Pinotti-CAISM-UNICAMP. The period of data collection was between November/2015 to December/2016, after approval of the Ethics Committee at our institution (CAAE: 45,792,115.6.0000.5404).
The sample power was calculated based on avulsion (major and minor) in three groups (VD, nonelective and elective CS) and it was established in 93.7%.
Fifty-three primiparous women with an interval after delivery of 12 to 24 months were included in this study. Women with neurologic or muscular conditions and those with previous pelvic surgery were excluded. The women were divided in three groups: VD (n = 32), nonelective CS (CS during labor, n = 8), and elective CS (planned CS, n = 13). The primary outcome evaluated was the levator ani avulsion by 3D/4D transperineal US. Secondary outcomes were urinary and vaginal symptoms before, during, and after delivery; loss of muscle strength; PFM strength; bladder-neck (BN) mobility; and hiatal area dimensions.
Demographic data and delivery parameters were collected from medical records. Patients were surveyed about urinary symptoms before and after delivery using the following questionnaires validated to Portuguese: International Consultation on Incontinence Questionnaire–Vaginal Symptoms (ICIQ-VS), which evaluates vaginal, sexual, and QoL issues [8]; the International Consultation on Incontinence Questionnaire–Urinary Incontinence–Short Form (ICIQ-UI-SF), which evaluates urinary symptoms [9].
Physical examination of the PFM was performed by a single physiotherapist specialized in women’s health. Patients were evaluated in the lithotomy position after micturition, without stirrups, and classified according to the Pelvic Organ Prolapse Quantification system (POP-Q) when necessary [10]. Then, digital palpation was undertaken while the patient performed three maximal pelvic floor contractions. The strongest one was graded according to the Modified Oxford Scale (0–5 points) [11]. After a physical examination, participants underwent a 3D/4D transperineal US by the same previous examiner trained and supervised by a physician specialized in gynecologic US with >15 years of experience.
GE Voluson 730 (GE Medical System Kretz-Technik GmbH and Co OHG, Zipf, Austria) US was attached to a RAB4-8 L convex transducer and transversely positioned at the vaginal introitus, protected with a latex condom. Images were captured at rest, during maximum Valsalva maneuver (VM), and during voluntary PFM contraction. Imaging analysis was performed by a second examiner (NM) blinded to evaluation data using 4D View software. BN mobility was measured during VM and PFM contraction to evaluate, respectively, its descent and elevation according to Naranjo–Ortiz et al. methodology [12]. Mobility was calculated based on the distance toward the inferoposterior margin of the pubic symphysis, which was measured using a reference line of its axis (x-axis) and its perpendicular intersection with the inferoposterior margin of the pubic symphysis (y-axis). A negative x coordinate indicates that the bladder is to the right of the reference point and a positive x coordinate indicates that the bladder is to the left. BN descent was calculated based on dislocation at resting position and VM using the following formula: √{(Vy-Ry) [2]+(Vx-Rx) [2]}, describing the difference between coordinates of the x (vertical distance) and y (horizontal distance) points in resting position (R) and Valsalva (V). Similarly, PFM contraction was calculated by the same formula, substituting V values for PFM contraction (C) values, as follows: √{(Cy-Ry) [2]+(Cx-Rx) [2]} [13].
Hiatal dimensions were measured in the axial plane at the level of minimum dimension [14], and three biometrical parameters were evaluated: anteroposterior diameter, laterolateral diameter, and hiatal area. Then, levator ani maximum thickness was measured, moving the plane cranially from the minimum hiatal dimension to the point of maximum muscle thickness, where it was measured at each side, close to the rectus, at 3 and 9 o’clock positions [14].
Levator ani integrity was evaluated through tomographic ultrasound imaging (TUI). Imaging slices were obtained from the minimum hiatal dimension, with 2.5 mm between them, 5 mm under it, and 12.5 mm above the reference plane. The exact location of slices was adjusted according to pubic symphysis position. Muscle avulsion was categorized as complete when abnormal insertion of the muscle to the pubic bone was present in three central images (Fig. 1) and partial when abnormal insertion was present at any three tomographic slices among the eight obtained images [15].
To describe quantitative variables, means were compared according to delivery mode. The Kruskal–Wallis test was used to compare the three possible delivery modes; Mann–Whitney test was used to compare VD and CS, using Bonferroni correction when appropriate. For categorical variables, distribution of frequency was compared using the chi-square or Fisher exact test. SAS version 9.4 for Windows was used, and the p value was set at 5%.,with Freeman–Halton extension.
Results
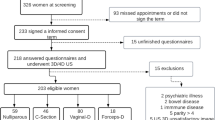
Hospital records showed that 822 primiparous women had a delivery in the 12–24 months before data collection. Among them, 602 could not be included in this study: 72 for a second pregnancy, 30 refused, and 500 had no updated contact number. Among the 220 women who agreed to participate, only 53 attended the evaluation: 32 with previous VD and 21 with CS (eight nonelective and 13 electives) (Fig. 2). Median age at evaluation was 24.8 (±5.7) years in the VD group, 24.3 (±4.4) years in the nonelective CS group, and 29.8 (±5.9) years in the elective CS group. Patients in the last group were significantly older than those in the VD (p = 0.02) and nonelective CS (p = 0.02) groups. No difference in age between VD and nonelective CS was identified (p = 0.93). There was also no statistical difference with regards to body mass index (BMI), ethnicity, smoking, sedentary lifestyle, or profession (Table 1).
Mean length of labor was 10 h (±8.9), with a mean expulsive stage of 39.3 (±32.4) min in the VD group and 16 h (±9.4) of labor in the nonelective CS group, without significant difference between groups (p = 0.10). Episiotomy was performed in more than half of women during VD, and first -and second-grade laceration occurred in 15 patients (46.9%). Mean newborn weight was 3.200 (±0.4) g in the VD group, 3.600 (±0,2) g in the nonelective CS group, and 3.000 (±1.0) g in the elective CS group (p = 0.07); average gestational age was 38 (±2.1) weeks, 39 (±0.9) weeks, and 38 (±2.7) weeks, respectively, for each group (p = 0.14)., and head circumference was 33.9 (±1.1), 35.0 (±0.7), and 34.2 (±5.3) cm, respectively (p = 0.03).
Women were asked about UI symptoms before and after delivery. Prior to pregnancy, 21.9% in the VD group, 25% in the nonelective CS group, and 30.8% in the elective CS group referred incontinence symptoms, without statistically significant differences between groups. After delivery, more than half in the VD group, 50% in the nonelective CS group, and 30.8% in the elective CS group referred symptoms, with no significant difference between groups (p = 0.39).or between referred complaints of muscle strength loss after delivery. Also, there was no difference in reports of these complaints according to the Oxford Modified Scale (p = 0.48 –0.87). Postpartum, no difference was identified in urinary symptoms evaluated on the ICIQ-SF (p = 0.28), vaginal symptoms on the ICIQ-VS (p = 0.29), sexual function (p = 0.36), and QoL (p = 0.24) between groups (Table 1).
In US evaluation, whether in resting position or on VM, no difference in BN elevation (p = 0.69) or descent (p = 0.65) was observed any group. Anteroposterior diameter in the sagittal plane (p = 0.36, p = 0.37), laterolateral diameter (p = 0.12, p = 0.50), hiatal area (p = 0.35, p = 0.68), and levator ani thickness at the right (p = 0.35, p = 0.19) and left (p = 0.44, p = 0.26) showed no significant difference between groups. No patient who underwent elective CS had levator ani avulsion, with a statistical difference among three groups (p 0.05). Levator ani avulsion between VD and elective CS groups showed significant statistical difference (p = 0.008)\.; there was no difference between nonelective CS and VD (p = 0.67) or elective CS (p = 0.19). In the VD group, eight (33.3%) women presented with major and six (25%) with minor avulsion, whereas in nonelective CS, one woman presented with major avulsion and two (28.6%) with minor avulsion (Table 2).
Discussion
This study showed that in a population of women evaluated 12–24 months after delivery, there were no significant differences in PFD symptoms or 3D/4D transperineal US findings according to delivery mode, except that women who had a VD had significantly greater levator ani avulsion than those who chose elective CS.
Levator ani muscle avulsion is defined as the separation of the puborectal/pubococcygeus muscle complex from the tendinous arch of the levator ani muscle and is the most common form of levator trauma [15]. Avulsion may be a causative or aggravating factor for SUI and is an indicator of trauma to the perineal support system, commonly associated with VD. In our study, among women with a VD, one third presented with major avulsion of the levator ani, which is consistent with current literature estimates of 10–35% prevalence [16]. Avulsion was more prevalent in women with VD and was absent in women with elective CS, with a statistically significant difference. There was no significant difference between nonelective CS and the other two groups. This study shows the importance of delivery mode in the pathology of levator ani avulsion. Another study reported similar results: 13% of avulsion in VD (without forceps) and 0% in CS delivery [17]. Others studies found no levator ani muscle defects in women who had a CS [18, 19].
Urinary symptoms were more prevalent among women with VD. One meta-analysis demonstrated a twofold increase in the risk of developing long-term SUI, comparing VD with CS [4]. Nevertheless, results of that article did not reach statistical significance. Regarding vaginal symptoms, there was also no difference. These findings endorse a study that evaluated women prior to and 1 and 4 years after delivery using the same questionnaires as in our study [20]. This could be due to long-term PFM recovery [21]. Another randomized study reinforces these findings, showing a lower rate of SUI among women assigned to elective CS compared with VD at 3 months after delivery. However, it showed no difference 2 years after delivery [22]. BN descent has been associated with the pathogenesis of SUI [12]. Among the methods used to evaluate urethral mobility, the most frequently recommended are BN descent assessed using US [12]. There is an association between VD and greater descent [23]. Staer–Jensen et al. identified greater mobility some weeks after delivery, with recovery on subsequent months [21]. One study evaluated BN descent 4 years after delivery and found no differences between VD and elective CS. These results are resonant with our data, which found no difference in BN descent between delivery modes. These findings may be due to recovery, as urethral mobility recovery 1 year after delivery has been reported [21], which corroborates our findings at a mean of 18 months after delivery.
Our results did not identify a difference in hiatal area between VD and elective CS. One study associated VD with an increase in hiatal area and genital prolapse [24], whereas one third of women might have a 20% increase in hiatal area after the first VD [25]. However, a recent study presents results similar to ours, showing significant hiatal area reduction months after delivery [26]. During pregnancy, physiological changes in the pelvic floor increase perineal distensibility [27]. Twelve months after delivery, an increase in elastin and collagen restores pelvic floor tonus to pregestational status.
The strengths of this analysis are the use of validated questionnaires to evaluate symptoms of pelvic floor dysfunction and the evaluation period of between 12 and 24 months, since many symptoms may resolve 6 months after birth [21]. Only 30 women refused to participate, but attendance rates were low. Acceptance to participate (21%) were similar to surveys available in the literature (20–30%) [28]. Limitations of this study are the small sample size and the possibility of recall bias. Size limitation may lead to increased type 2 errors due to the difficulty for women to return to the hospital at which they delivered and, clearly, obstacles to research in countries like Brazil, where offering financial compensation to participants is not permitted. Evidence in the literature marks a positive association between reward and participation rates in such studies, independent of the amount of remuneration [29]. With regard to symptom evaluation, although questionnaire assessment was prospective, evaluation of previous symptoms may influence results. Prospective studies with more robust samples may further elucidate the role of delivery mode on symptoms and anatomic alterations of the pelvic floor.
Conclusions
In this study, which evaluated primiparous women over 12–24 months after delivery, VD was associated with levator ani avulsion. There was no difference among VD, nonelective CS, and elective CS groups regarding symptomatology or other anatomic alterations evaluated through 3D/4D transperineal US.
Abbreviations
- PFD:
-
Pelvic floor dysfunction
- VD:
-
Vaginal delivery
- PFM:
-
Pelvic floor muscle
- US:
-
Ultrasound
- CS:
-
Cesarean section
- ICIQ-VS:
-
International Consultation on Incontinence Questionnaire–Vaginal Symptoms
- ICIQ-SF:
-
International Consultation on Incontinence Questionnaire–Short Form
- POP-Q:
-
Pelvic Organ Prolapse Quantification system
- BN:
-
Bladder neck
- TUI:
-
Tomographic ultrasound imaging
References
Haylen BT, Ridder DD, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20.
Memon H, Handa VL. Pelvic floor disorders following vaginal or cesarean delivery. Curr Opin Obstet Gynecol. 2012;24(5):349–54.
Huser M, Janku P, Hudecek R, Zbozinkova Z, Bursa M, Unzeitig V, et al. Pelvic floor dysfunction after vaginal and cesarean delivery among singleton primiparas. Int J Gynecol Obstet. 2017;137(2):170–3.
Tähtinen RM, Cartwright R, Tsui JF, Aaltonen RL, Aoki Y, Cárdenas JL, et al. Long-term impact of mode of delivery on stress urinary incontinence and urgency urinary incontinence: a systematic review and meta-analysis. Eur Urol. 2016;70(1):148–58.
Alperin M, Cook M, Tuttle LJ, Esparza MC, Lieber RL. Impact of vaginal parity and aging on the architectural design of pelvic floor muscles. Am J Obstet Gynecol. 2016;215(3):312 e–1-9.
Dietz HP. Pelvic floor trauma following vaginal delivery. Curr Opin Obstet Gynecol. 2006;18:528–37.
Tan L, Shek KL, Atan IK, Rojas RG, Dietz HP. The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J. 2015;26(11):1667–72.
de Oliveira MS, Tamanini JTN, de Aguiar Cavalcanti G. Validation of the prolapse quality-of-life questionnaire (P-QoL) in Portuguese version in Brazilian women. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(10):1191–202.
Nunes Tamanini JT, Dambros M, D’Ancona CAL, Rodrigues Palma PC, Rodrigues NN. Validação para o português do “International Consultation on Incontinence Questionnaire - Short Form” (ICIQ-SF). Rev Saude Publica. 2004;38(3):438–44.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87(12):631–42.
Naranjo-Ortiz C, Shek KL, Martin AJ, Dietz HP. What is normal bladder neck anatomy? Int Urogynecol J. 2016;27(6):945–50.
Shek KL, Dietz HP. The urethral motion profile: a novel method to evaluate urethral support and mobility. Aust New Zeal J Obstet Gynecol. 2008;48(3):337–42.
Albrich S, Laterza RM, Skala C, Salvatore S, Koelbl H, Naumann G. Impact of the mode of delivery on levator morphology: a prospective observational study with three-dimensional ultrasound early in the postpartum period. BJOG. 2012;119(1):51–60.
Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011;22(6):699–704.
Dietz HP. Pelvic floor trauma in childbirth. Aust N Z J Obstet Gynaecol. 2013;53(3):220–30.
Cassadó Garriga J, Pessarrodona Isern A, Espuña Pons M, Duran Retamal M, Felgueroso Fabrega A, Rodriguez Carballeira M, et al. Four-dimensional sonographic evaluation of avulsion of the levator ani according to delivery mode. Ultrasound Obstet Gynecol. 2011;38(6):701–6.
van Delft K, Sultan AH, Thakar R, Schwertner-Tiepelmann N, Kluivers K. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG. 2014;121(9):1164–71.
Siafarikas F, Staer-Jensen J, Hilde G, Bø K, Ellström Engh M. The levator ani muscle during pregnancy and major levator ani muscle defects diagnosed postpartum: a three- and four-dimensional transperineal ultrasound study. BJOG. 2015;122(8):1083–91.
Volløyhaug I, van Grutin I, van Delft K, Sultan AH, Thakar R. Is bladder neck and urethral mobility associated with urinary incontinence and mode of delivery 4 years after childbirth? Neurourol Urodyn. 2016;9999:1–8.
Staer-Jensen J, Siafarikas F, Hilde G, Benth JS, Bo K, Engh ME. Postpartum recovery of levator hiatus and bladder neck mobility in relation to pregnancy. Obstet Gynecol. 2015;125(3):531–9.
Hannah M, Whyte H, Hewson S. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized term breech trial. Am J Obstet Gynecol. 2004;191:917–27.
Jundt K, Scheer I, Schiessl B, Karl K, Friese K, Peschers U. Incontinence, bladder neck mobility, and sphincter ruptures in primiparous women. Eur J Med Res. 2010;15(6):246–52.
Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25(6):580–5.
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12):1485–92.
Ferreira CW, Atan IK, Martin A, Shek KL, Dietz HP. Pelvic organ support several years after a first birth. Int Urogynecol J. 2017;28(10):1499–1505.
Ashton-Miller JA, DeLancey JOL. On the biomechanics of vaginal birth and common aequelae. Annu Rev Biomed Eng. 2009;11:163–76.
Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–36.
Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Araujo, C.C., Coelho, S.S.A., Martinho, N. et al. Clinical and ultrasonographic evaluation of the pelvic floor in primiparous women: a cross-sectional study. Int Urogynecol J 29, 1543–1549 (2018). https://doi.org/10.1007/s00192-018-3581-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3581-y