Abstract
Purpose
The aim of this study was to describe the sagittal geometry of the trochlear groove in patients who underwent primary TKA, based on intraoperative data acquired with a navigation system.
Methods
Intraoperative navigation data were collected from 110 patients. All operations were guided by a non-image-based navigation system (BLU-IGS, Orthokey Italia Srl). The trochlear groove has been described on the three anatomical planes; in particular, on the sagittal plane the hypothesis has been verified that the acquired points are referable to a circle. Using the data collected during intraoperative navigation, possible correlation between the radius of the trochlear groove and other femur dimension (length, AP dimension) was analyzed; the orientation of the trochlear sulcus with respect to the mechanical axis and the posterior condyle axis was analyzed too, searching for possible correlation between groove alignment (frontal and axial) or groove radius and the hip–knee–ankle (HKA).
Results
The average radius of curvature of the femoral trochlea was 25.5 ± 5.6 mm; the difference was not statistically significant between the men and women (n.s. p value). No correlation was found between the trochlear groove radius and the femur length (r = − 0.02) or the HKA-phenotypes (r = 0.03) and between the groove alignment and HKA-phenotypes. On axial plane, the trochlear groove was 3.2° ± 4.3° externally rotated, with respect to the posterior condylar axis; on frontal plane, the trochlear groove was 3.9° ± 5.3° externally rotated, with respect to the mechanical axis. In both cases, no statistically significant differences were found between male and female and between left and right limb (p > 0.05).
Conclusion
The present study shows that the sagittal plane geometry of the femoral trochlea in patients affected by osteoarthritis could be described accurately as a circle. The acquisition of the trochlear morphology intraoperatively can lead to more anatomically shape definition, to investigate deeper its radius of curvature and geometry. Trochlear shape could be used as landmarks for femoral component positioning, thus customizing the implant design, optimize the outcomes and improving anterior knee pain after TKA.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patellofemoral complications are a common cause of pain and complications after total knee arthroplasties (TKA). Femoral implant misplacement may generate overstuff, resulting in increased patellar stresses and anterior knee pain [14, 16]. A recent review on mid flexion instability included as technique-specific risk factors the proximalization and anteriorization of femoral implant [6, 20]. Iranpour [9] clearly demonstrates that, in healthy knees, patella follows a circular path. This path is guided by circular shape and orientation of trochlear axis [10].
Given that, a better understanding of the relationship between the femoral component positioning, surgical technique and TKA outcomes, is related to an accurate knowledge of the femoral trochlear geometry itself. However, most of studies focused on the transverse and frontal geometry of the trochlear groove, quantifying its depths and orientation [10], while its radius in the sagittal plane has been mostly neglected [5, 15, 22]. Moreover, the few studies that investigated this aspect were limited to the use of radiological technologies such as MRI or CT-based 3D reconstructions.
During surgery the trochlear groove could be used as reference for femoral implant positioning, because it is less affected by pathology. Despite this, shape of trochlear sulcus on TKA patients has been scarcely investigated. The aim of the study was to verify if pathological trochlear sulcus, collected during intraoperative navigation, is still comparable to what is reported on healthy subjects with other methodologies. Based on literature [5, 10, 15, 22] we wanted to verify if trochlear sulcus, in TKA patients, can still be modeled with a circle, so that it can be modeled and used as intraoperative parameter for implant positioning. Trochlear sulcus was also described on frontal and axial plane and aimed to establish a possible correlation between the radius of the trochlear groove and other femur dimensions.
Materials and methods
Data acquisition
Femoral sulcus was acquired on a cohort of 110 consecutive patients (34 men and 76 women) who underwent navigated TKA between October 2017 and November 2018 by a single experienced surgeon (YV). Patient characteristics such as age, gender, body mass index (BMI) and mechanical axis (HKA) were recorded (Table 1). HKA angle was measured on preoperative standing full-length radiographs and it was divided in phenotypes: neutral alignment was defined between − 1.5° varus and 1.5° valgus, varus alignment < − 1.5° and valgus alignment > 1.5° [7].
Exclusion criteria of the study were: varus or valgus deformities greater than 15°.
Anatomic data were acquired intraoperatively using a navigation system (BLU-IGS, Orthokey Italia Srl, Firenze, Italy), which also allows verification of bone resections, extension and flexion gaps, ligament balance, and implant positioning. The navigation system’s protocol and accuracy are reported [1, 2], nominal accuracy of the system is 0.5°/mm and inter-tester reliability > 0.8 (intraclass correlation coefficient ICC).
The femoral coordinate reference system was defined as follows: the proximal–distal (PD) axis was aimed along the mechanical axis was defined joining the femoral head center, by leg pivoting, and the most distal part of the femur in the inter-condylar notch. The medio-lateral (ML) axis was defined from the most posterior parts of medial and lateral condyles. Antero-posterior (AP) axis was calculated by cross product of the previous two axes. Additional acquired points were the anterior shaft and the most distal part of the condyles.
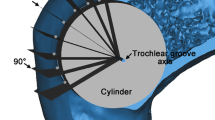
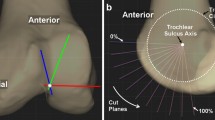
The surgeon acquired also the trochlear groove. These points were expressed and analyzed in the femur reference system to define the sagittal geometry of the sulcus (femur lateral view) (Fig. 1).
Studies demonstrated that in healthy knee, patellofemoral groove closely approximated a circular arc [5, 10, 15, 22]. To evaluate this hypothesis in OA knees, the acquired sulcus has been fitted by two different methods: cubic polynomial and circle. The less-root-mean-square-error-method was chosen to analyse the geometrical features of the groove and it has been reported below. The trochlear groove points were fitted by a circle in a range from 0° to 90°: the 0°-point was lying on the AP axis and the 90°-point was lying on the mechanical axis; measurements were taken at 5° increments (Fig. 2). The best-fit circle was found using a software routine implemented in MATLAB (MathWorks Inc., Natick, USA) that minimized the root mean-square error in relation to the acquired points. The trochlear groove varus-valgus and internal–external orientations as well as the starting and end points of the groove were even evaluated.
Femoral length was defined as the distance between femoral head center to the distal inter-condylar notch and the APk femur dimension as the distance between the anterior femoral cortex and the posterior condyle. No data about medio-lateral femoral dimension were available, since epicondyles were not routinely digitized during navigation.
Navigated TKA represents the standard of care for the senior surgeon; therefore, the present study represents the retrospective analysis of prospectively collected data acquired intraoperatively during a standard procedure. The CNIL *French ethic comitee regarding personal datas* gave the authorization to collect clinical data. Patients signed informed consent for the surgical procedure the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statistical analysis
Data were reported as mean and standard deviation (mean ± SD). Considering the lack of studies in literature with the same methodology, the sample size was calculated with the aim to detect a significant difference between males and females of 2 mm with a standard deviation of 3 mm. Using a power of 80%, an alpha value of 0.05 and considering a male:female ratio of 1:2 base on the senior surgeon experience and volume, a sample of 27 males and 54 females was required. The Student’s t test was performed to compare the patients’ gender with the radius of the trochlear groove and the APk dimension. Comparison between groove alignment (frontal and axial) and HKA-phenotypes were performed using one-way analysis of variance (ANOVA). Correlation between femur length and groove radius was analyzed with Pearson’s linear correlation test. A p value of less than 0.05 was considered statistically significant. Analyse-it software (Analyse-it Software Ltd., Leeds, UK) was used to perform the reported statistical analysis.
Results
The geometry of the trochlear groove could be described accurately as a circle in the sagittal plane. The average radius was 25.5 ± 5.6 mm (range 14.0–37.4 mm) and the 95% CI was from 24.4 to 26.5 mm (Fig. 3). The data points had an average root mean-square error of 0.4 ± 0.2 mm from the fitted radius in each knee.
For men, the radius of the curvature of the femoral trochlear groove was 24.7 ± 4.9 mm, while for women it was 25.6 ± 5.8 mm (Fig. 4). The difference was not statistically significant between the men and women (n.s. p value). In the sagittal view, the average center of the fitted trochlear groove was at 24.0 ± 4.6 mm proximally along the mechanical axis and 2.2 ± 5.2 mm posteriorly along the AP axis. A weak correlation was found between the groove radius and the anterior femoral cortex (r = 0.27). No correlation was found between the femur length and the trochlear groove radius (r = − 0.02) (Fig. 5).
On axial plane, the trochlear groove was 3.2° ± 4.3° externally rotated, with respect to the posterior condylar axis (Fig. 6). No statistically significant differences were found between male and female and between left and right limb (Table 2).
On frontal plane, the trochlear groove was 3.9° ± 5.3° externally rotated, with respect to the mechanical axis (Fig. 7). No statistically significant differences were found between male and female and between left and right limb (Table 3).
No statistically significant differences between groove orientation, and HKA-phenotypes (Fig. 8) were found. A varus alignment was present in 66 (60.0%) cases (HKA < − 1.5°), a neutral alignment in 25 (22.7%) (− 1.5° < HKA < 1.5°), and a valgus alignment in 19 (17.3%) (HKA > 1.5°).
A positive moderate correlation was found between the APk dimension and the trochlear groove radius (r = 0.36). The average APk dimension was 60.9 ± 3.4 mm for men and 56.3 ± 3.2 mm for women; the difference was statistically significant (p < 0.05).
Discussion
The most important finding of the present study was that the geometry of the trochlear groove, in patients who underwent a TKA implant, could be described accurately as a circle in the sagittal plane with an average radius of 25.5 ± 5.6 mm centered 2.2 ± 5.2 mm posterior to mechanical axis, and 24.0 ± 4.6 mm proximal to inter-condylar notch. Sulcus line has 3.2° ± 4.3° of external rotation, with respect to the posterior condyles axis and a 3.9° ± 5.3° of external rotation, with respect to the mechanical axis. Moreover, no differences were found between genders and based on femoral length. We also found no differences in sulcus orientation in patients divided according to limb phenotypes.
Despite few studies investigated the trochlear groove geometry in relation to its radius of curvature, several novel findings have been identified in the present study. In fact, this is the first study to evaluate this morphological feature intraoperatively using a navigation system and, moreover, the one with the largest sample size. This allowed to study the patient morphology, independently from the slice orientation of common radiological technologies such as X-ray or MRI. In fact, Monk et al. [13] in 25 healthy subjects, by means of MRI measured an average radius of 21 mm, which is smaller than what reported in the present study. Limitations of their MRI measurement were the spatial resolution with 2.2 mm slice thickness and the manual acquisition of parameters. For these reasons, the value reported in the present study could be considered more reliable and closer to patient’s anatomy. In fact Iranpour, with a 3D CT-based model on 40 healthy knees, described the trochlear groove as a circle with a radius of 23 mm [10]. Considering that CT is able to capture only osseous anatomy, including a cartilage layer of 2 mm [3, 18], it is consistent to the value of 25 mm reported in the present study. While the geometry of the cartilage surface is known to differ from normal to OA knees, the difference is relatively small [8] and thus—this aspect is not expected to affect our conclusions. An inferior value of 19–20 mm was instead found in 100 healthy Chinese subjects, again using 3D CT-based reconstructions [22]. The authors imputed the differences with previous studies to the variation in reference axis, measurement methods and racial differences. Such considerations are valid also for the present study, where European patients were included, similarly to previous studies [10, 13]. On the other hand, a common finding is found in the population evaluated in the present study and the in Chinese population, since in both cases no differences were found between males and females. This is important, because it confirms the hypothesis that femoral groove shape is independent from gender. Furthermore, the patient’s height seems irrelevant as well, since no correlation was found between radius and femoral length. Thus, in the view of patient specific TKA positioning and TKA design, gender and patient’s femoral length does not represent relevant variables to be taken into account to optimize patellofemoral anatomy.
Our results confirm that the orientation of trochlear sulcus on axial plane is about 3° externally rotated with respect to posterior condylar tangent. This confirms what expressed by Riviere et al. [17], kinematically aligned implants my lead to overstuff of lateral trochlea, and also in works of Talbot et al. [19].
Our data regarding native HKA and groove alignment and radius are in line with those from Maillot et al. [11] reported that TF and trochlear anatomies are relatively independent from one another.
From a clinical perspective, the present study offers important insights. First of all, it confirms that intraoperatively it is still possible to map the trochlear groove shape with a circle, in a similar fashion to what reported in other research [10, 13, 22]. Thus, a simple circle model can be used to identify portions of trochlear sulcus to use as reference to customize implant positioning based on arches of that circle, to avoid potential patellofemoral overstuff [12] or mid flexion instability [6]. Further studies should be performed in this direction to assess its reliability and its clinical implications in optimizing the outcomes and reducing anterior knee pain after TKA. Moreover, instrumentations and software could be developed for this purpose. Another insight is represented using these measurements in the development of patellar-friendly TKA designs. It was in fact demonstrated that several actual TKA designs exhibit characteristics of trochlear dysplasia [4], that manufacturer’s definition of anatomical groove geometry may not imply exact replication of normal anatomy, and that exact restoration of physiologic patellar tracking may not be feasible with current designs [17, 21].
The present study has several limitations. First, the measurements were not obtained in healthy patients but in those with OA requiring TKA, without considering the amount of patellofemoral disease that could bias the results. If from one side this could not allow to generalize the findings to general population, on the other hand those are applicable to osteoarthritic patients, which are those that effectively need knee replacement and thus represent the ideal population to investigate the patellofemoral anatomy. Secondly, all measurements were obtained manually by a single examiner. However, the small average root mean square error demonstrates a good reliability in such measurements, thus discarding bias in the method of measurement. Finally, the lack of MRI or CT evaluation did not allow to correlate and validate the navigation measurement with common radiological methods. However, it was not the aim of the study, which was instead designed to assess the in vivo trochlear shape and its correlation with gender and femoral dimension.
Conclusions
The geometry of the trochlear groove in patients with osteoarthritis could be described accurately as a circle in the sagittal plane with an average radius of 25.5 ± 5.6 mm and a 3.2° ± 4.3° of external rotation, with respect to the posterior condyle axis and a 3.9° ± 5.3° of external rotation, with respect to the mechanical axis. Moreover, no differences are present between the genders and based on femoral length; differences are present instead between gender and femoral AP dimension. No correlation was found between groove alignment (frontal and axial) or groove radius and the HKA-phenotypes.
References
Bignozzi S, Lopomo N, Zaffagnini S, Martelli S, Bruni D, Marcacci M (2008) Accuracy, reliability, and repeatability of navigation systems in clinical practice. Oper Tech Orthop 18:154–157
Casino D, Zaffagnini S, Martelli S, Lopomo N, Bignozzi S, Iacono F, Russo A, Marcacci M (2009) Intraoperative evaluation of total knee replacement: kinematic assessment with a navigation system. Knee Surg Sports Traumatol Arthrosc 17:369–373
Culvenor AG, Eckstein F, Wirth W, Lohmander LS, Frobell R (2019) Loss of patellofemoral cartilage thickness over 5 years following ACL injury depends on the initial treatment strategy: results from the KANON trial. Br J Sports Med 53:1168–1173
Dejour D, Ntagiopoulos PG, Saffarini M (2014) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 22:2599–2607
Du Z, Chen S, Yan M, Yue B, Zeng Y, Wang Y (2017) Do size, shape, and alignment parameters of the femoral condyle affect the trochlear groove tracking? A morphometric study based on 3D- computed tomography models in Chinese people. BMC Musculoskelet Disord 18:1–7
Evangelista PJ, Laster SK, Lenz NM, Sheth NP, Schwarzkopf R (2018) A computer model of mid-flexion instability in a balanced total knee arthroplasty. J Arthroplasty 33:S265–S269
Hochreiter B, Hirschmann MT, Amsler F, Behrend H (2019) Highly variable tibial tubercle–trochlear groove distance (TT–TG) in osteoarthritic knees should be considered when performing TKA. Knee Surg Sports Traumatol Arthrosc 27:1403–1409
Iagnocco A, Coari G, Zoppini A (1992) Sonographic evaluation of femoral condylar cartilage in osteoarthritis and rheumatoid arthritis. Scand J Rheumatol 21:201–203
Iranpour F, Merican AM, Baena FRY, Cobb JP, Amis AA (2010) Patellofemoral joint kinematics: the circular path of the patella around the trochlear axis. J Orthop Res 28:589–594
Iranpour F, Merican AM, Dandachli W, Amis AA, Cobb JP (2010) The geometry of the trochlear groove. Clin Orthop Relat Res 468:782–788
Maillot C, Leong A, Harman C, Morelli A, Mospan R, Cobb J, Rivière C (2019) Poor relationship between frontal tibiofemoral and trochlear anatomic parameters: implications for designing a trochlea for kinematic alignment. Knee 26:106–114
Mihalko W, Fishkin Z, Krakow K (2006) Patellofemoral overstuff and its relationship to flexion after total knee arthroplasty. Clin Orthop Relat Res 449:283–287
Monk AP, Choji K, O’Connor JJ, Goodfellow JW, Murray DW (2014) The shape of the distal femur: a geometrical study using MRI. Bone Jt J 96B:1623–1630
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Jt J 96B:96–100
O’Connor JJ, Shercliff TL, Biden E, Goodfellow JW (1989) The geometry of the knee in the sagittal plane. Proc Inst Mech Eng Part H J Eng Med 203:223–233
Petersen W, Rembitzki IV, Brüggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Rivière C, Dhaif F, Shah H, Ali A, Auvinet E, Aframian A, Cobb J, Howell S, Harris S (2018) Kinematic alignment of current TKA implants does not restore the native trochlear anatomy. Orthop Traumatol Surg Res 104:983–995
Schub DL, Frisch NC, Bachmann KR, Winalski C, Saluan PM (2013) Mapping of cartilage depth in the knee and elbow for use in osteochondral autograft procedures. Am J Sports Med 41:903–907
Talbot S, Dimitriou P, Radic R, Zordan R, Bartlett J (2015) The sulcus line of the trochlear groove is more accurate than Whiteside’s Line in determining femoral component rotation. Knee Surg Sports Traumatol Arthrosc 23:3306–3316
Vajapey SP, Pettit RJ, Li M, Chen AF, Spitzer AI, Glassman AH (2020) Risk factors for mid-flexion instability after total knee arthroplasty: a systematic review. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.05.026
Varadarajan KM, Rubash HE, Li G (2011) Are current total knee arthroplasty implants designed to restore normal trochlear groove anatomy? J Arthroplasty 26:274–281
Wang J, Yue B, Wang Y, Yan M, Zeng Y (2012) The 3D analysis of the sagittal curvature of the femoral trochlea in the Chinese population. Knee Surg Sports Traumatol Arthrosc 20:957–963
Acknowledgements
We would like to thank Mr. David Burlot for his precious contribution in data collection and management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Simone Bignozzi is an employee of Orthokey Italia srl. Other authors have no conflict of interest.
Funding
No fundings have been received for this work.
Ethical approval
Clinical data were collected under authorization of CNIL.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grassi, A., Asmonti, I., Bignozzi, S. et al. The sagittal geometry of the trochlear groove could be described as a circle: an intraoperative assessment with navigation. Knee Surg Sports Traumatol Arthrosc 29, 1769–1776 (2021). https://doi.org/10.1007/s00167-020-06224-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06224-w