Abstract
Purpose
This study aimed to investigate the natural morphology of the femoral trochlear groove based on quantitative measurement.
Methods
Computed tomographic femur models of 50 male and 50 female healthy Chinese adults (30–60 years) were analysed using three-dimensional software. Coaxial cutting planes (15° increments) rotating about the trochlear groove axis from the proximal to distal point were created, followed by the deepest point of the trochlear groove marked at each cross section. The shape, position, and orientation of the trochlear groove were analysed.
Results
The trochlear groove was located laterally relative to the mechanical axis and consisted of the laterally oriented proximal part and medially oriented distal part. Based on the turning points located on different cross sections, the trochlear groove was classified into four types: types 45°, 60°, 75°, and 90°. The mediolateral position relative to the mechanical axis was types 45°, 60°, 75°, and 90°, from the lateral to medial side, while the distal parts of them extended along the same path. The orientation of the trochlear groove was relatively consistent and smooth, which oriented at approximately 1° medially between two adjacent segments, except at approximately 10° medially at the turning point.
Conclusion
The trochlear groove tracking varies greatly amongst a population that is mainly categorized into four types. This study may be helpful for better understanding of the natural trochlear groove anatomy, prosthetic design modification, and provide the reference value for studying patellofemoral diseases such as patellar maltracking and trochlear dysplasia.
Level of evidence
Prospective study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is effective for improving knee functions, yet postoperative patellofemoral complications, such as chronic pain, patellar component dislocation, and patellar component loosening/wearing, are commonly observed postoperatively and considered a major cause for revision surgeries [8, 10, 16, 17]. Biomechanical studies by three-dimensional computer models of various TKA designs found that, when other influential factors were controlled (i.e. soft tissue balancing, component positioning, alignment, patellar resurfacing), the anatomical patellofemoral kinematics was not fully restored to physiological values [21, 23]. The asymmetrically designed femoral component with laterally orientated trochlear groove did not provide more anatomical patellar kinematics and patellar stability compared with the older design with symmetrical trochlear groove [3, 21]. The prosthetic trochlear groove may still be different from the normal trochlea, which may partly explain the cause of postoperative patellofemoral complications.
The geometry of the trochlea is the main determinant of patellar position at flexion angles higher than 30° [3, 5]. In addition, the bony structure was reported as an important determinant of patellar kinematics at end-range knee extension (0°–30°) [18]. It is acceptable to assume that the patellar tracking will be very similar to the anatomy of the trochlear groove [5]. Therefore, whether patellofemoral mechanisms could be restored after TKA greatly depends on the design of the prosthetic trochlear groove [6, 12]. A systematic evaluation of the morphological features (shape, position, and orientation) of the natural trochlear groove is necessary for the prosthesis design to be more compatible with the physiological anatomy.
There is a general consensus that the natural trochlear groove orientation follows a path that could be approximated by two consecutive straight lines: a bilinear approximation, with different orientations in its proximal and distal parts [4, 11, 22]. It was hypothesized that there may be a turning point where the two parts connect, and that the turning points of individuals may be located at different zones of the trochlear groove with variations in morphological features of the trochlear groove. Therefore, this study aimed to investigate the geometry of the natural knee trochlear groove in terms of its shape, position, and orientation and to test the hypothesis that the bilinear-shaped trochlear groove could be classified into different types based on various locations of the turning point. The geometry of the trochlear groove tracking was just briefly described in previous studies; the mediolateral position, orientation, and thus different types of the trochlear groove tracking based on these parameters have not been systematically evaluated in the literature. Importantly, the evaluation of the trochlear groove morphology is the theoretical foundation to investigate the difference between natural and prosthetic knees or between natural and pathological knees in trochlear groove morphology. This study may contribute to prosthetic design modification to obtain improved patellofemoral performance.
Materials and methods
One hundred healthy Chinese subjects (50 males and 50 females) were recruited for this study (30–39 age group: 9 males and 8 females; 40–49 age group: 12 males and 35 females; 50–60 age group: 29 males and 7 females). The median age was 46 years (range 30–60 years); height, 165 cm (range 150–190 cm); weight, 65 kg (range 43–90 kg); body mass index (BMI), 23.5 kg/m2 (range 16.5–29.6 kg/m2); mechanical axis of the lower limb, 179.2° (range 174.6°–185.5°). Inclusion criteria were as follows: no anatomical abnormality and no symptoms of soft tissue injuries or osteoarthritis. Individuals with previous knee trauma, knee pain, and other chronic diseases of the musculoskeletal system were excluded from the study.
Three-dimensional knee models
Computed tomography (CT) (Light Speed 16; GE Medical System, General Electric Company, Milwaukee, WI, USA) scanning of both lower extremities was performed in all subjects. The scanning procedure was performed to acquire 0.625-mm CT slices for the knee joint and 2-mm CT slices for the hip joint and ankle joint (resolution 512 × 512 pixels). The femoral and tibial shafts were not scanned to avoid unnecessary radiation exposure. Scanning data were then introduced into the Geomagic Studio 10.0 software program (Geomagic Inc., Research Triangle Park, NC, USA) for use in three-dimensional reconstruction of the geometric pattern of the skeletal knee model.
Trochlear groove morphological measurement
Before measurement, the femur was aligned as follows: the mechanical axis was defined as the line connecting the centre of the femoral head and apex of the intercondylar notch [25]. The coronal plane was parallel to the mechanical axis and was externally rotated at 3° relative to the line connecting the most posterior points of both femoral condyles. The sagittal plane was perpendicular to the coronal plane and passed through the mechanical axis. The transverse plane was perpendicular to both the coronal and sagittal planes.
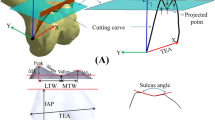
A cylinder was established with its axis parallel to both the coronal and transverse planes, and its radius was adjusted to allow the cylindrical surface to closely fit the trochlear groove; its axis represented the trochlear groove axis. Coaxial cutting planes rotating about the trochlear groove axis from the proximal point to the distal point were created. The plane parallel to the transversal plane represented a 0° cutting plane. Then, with 15° increments towards the distal end of the trochlear groove, cutting planes of 15°, 30°, 45°, 60°, 75°, 90°, and 105° were created, and eight corresponding cross sections were obtained. The deepest points of the trochlear groove were marked on the knee model surface at each cross section, from the proximal to distal end (Fig. 1).
Lateral view of the trochlear groove axis and cutting planes. The medial femoral condyle was removed by the mid-sagittal plane to display the details of the trochlear groove. A cylinder with its axis parallel to both the coronal and transverse planes was established, and its radius was adjusted to allow the cylindrical surface to closely fit the trochlear groove; its axis represented the trochlear groove axis. Coaxial cutting planes rotating about the trochlear groove axis from the most proximal point to the most distal point were created. Starting on a 0° cutting plane parallel to the transversal plane, 15° increments of the cutting plane were created towards the distal end of the trochlear groove; thus, 15°, 30°, 45°, 60°, 75°, 90°, and 105° cutting planes were created
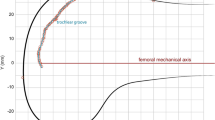
The distance (mediolateral position) from the deepest point of the trochlear groove to the mechanical axis was measured. If the point was located at the medial side of the mechanical axis, the value was positive (d); otherwise, the value was negative (−d) (Fig. 2a). The orientation parameters of the trochlear groove included α and β angles. The angle between every 15° segment on trochlear groove tracking and the mechanical axis was represented by α. α indicated groove orientation at each cross section. Positive values (+α) indicated the lateral orientation of the trochlear groove tracking, and negative values (−α) indicated the medial orientation. The angle between two adjacent 15° segments on the trochlear groove tracking was represented by β (Fig. 2b). Specially, if the groove tracking was beyond the arc of 0°–105°, the most proximal/distal deepest point was defined with cross sections smaller than 0° and larger than 105°.
Measurement of the mediolateral position and orientation of the trochlear groove tracking. A positive d value (d) indicated that the point was located at the medial side of the mechanical axis. A negative d value (−d) indicated that the point was located at the lateral side of the mechanical axis. The angle between every 15° segment on the trochlear groove tracking and the mechanical axis was represented by α. Positive values (+α) indicated a lateral orientation of the trochlear groove tracking, while negative values (−α) indicated a medial orientation. The angle between two adjacent 15° segments on the trochlear groove tracking is represented by β
In a pre-experiment with 40 randomly selected samples, 3° increments were used to create cutting planes as in a previous study [23]. The result showed that the average angles of the cutting planes where the turning point was located were 44.4 ± 3.3° (5 samples), 60.2 ± 3.4° (12 samples), 75.5 ± 3.6° (16 samples), and 89.1 ± 2.9° (7 samples). Increments of 6°, 12°, 15°,18°, 24°, and 30° were also tested, and a 15° increment was as effective as a 3° increment to obtain an adequate amount of valid data and improved the research efficiency as well.
All of the measurements were finished by one surgeon to eliminate the interobserver bias. A test–retest analysis was performed to determine intraobserver reliability by measuring the parameters three times in one randomly selected femur, and the assessment was made every month after the first measurement. The standard deviation of the three measuring trials was used to represent measurement accuracy, which was 0.1 mm and 0.1° for the mediolateral location (d) and orientation (α) of the trochlear groove tracking, respectively.
The study was approved by the Institutional Review Board of the Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine (registration number 201532), and informed consent was obtained from all patients.
Statistical analysis
One-way analysis of variance was used to analyse the d values, α/−α, and β angles between different types of groove trackings, as well as age, height, weight, and BMI. Student’s t test was performed to determine whether the α/−α angles between two adjacent 15° segments and β angles between two adjacent deepest points of the groove tracking were significantly different. A p value less than 0.05 was considered statistically significant. This sample size was mainly chosen from the data in the pre-experiment of 42 knees and was calculated using a power analysis. The sample size for a power of ~0.9 (α = 0.05) indicated a minimum sample size of 48 knees. As the mediolateral position parameter indicated by the d value was rather small in value and less than 3.0 mm, a relatively larger sample size was reasonable to decrease the inaccuracy caused by measurement errors.
Results
In the 200 knee models, the trochlear grooves were comprised of two parts (a laterally oriented proximal part and medially oriented distal part) with turning points located at 30°, 45°, 60°, 75°, 90°, and 105° cross sections, respectively, and the corresponding number of cases was 3, 20, 47, 103, 25, and 2, respectively. The data of knee models (5 cases) with turning points located at 30° and 105° cross sections were eliminated from the statistical analysis because of the small sample size. Based on the turning point location in the cross section, the trochlear groove was classified into types 45°, 60°, 75°, and 90°. No significant difference was observed between the four types in terms of average age, weight, height, and BMI (n.s.).
Mediolateral position of the trochlear groove
Generally, the trochlear groove located laterally relative to the mechanical axis. The mediolateral positions of the proximal parts for the four types were different, and according to the d/−d values, the order was types 45°, 60°, 75°, and 90°, from the lateral to medial side; the distal parts extended along the similar path (Table 1, Fig. 3). For the proximal part, the d/−d values of the corresponding points were not significantly different between type 45° and type 60°. For the distal part, the d/−d values at 60° (types 45° vs. 60°), 75° (types 45° vs. 60° vs. 75°), 90° (types 45° vs. 60° vs. 75° vs. 90°), and 105° (types 45° vs. 60° vs. 75° vs. 90°) cross sections were not significantly different between the types (Table 2).
Orientation of the trochlear groove
A significant difference was noted when comparing α between two adjacent 15° segments of the trochlear groove within types 45°, 60°, 75°, and 90° (Table 3). Specifically, there were no significant differences in the comparison of adjacent segments 45°–60° versus 60°–75°, 60°–75° versus 75°–90°, 75°–90° versus 90°–105° in type 45°; and adjacent segments 75°–90° versus 90°–105° in type 60° (Table 4). However, no significant difference was noted when comparing α of the corresponding segment between types 45°, 60°, 75°, and 90°, except when the groups compared were in different directions and in three pairs of comparisons (types 60° vs. 75° in 15°–30° and 45°–60° segments; types 60° vs. 90° in 45°–60° segments) (Table 5). Regarding angle β (excluded β of the turning point), no significant difference was found in comparisons between adjacent groove points except in type 75° (90° vs. 105° cross section, p < 0.05). Furthermore, comparisons of β (excluded β of the turning point) of corresponding groove points between the four types were made with similar results noted, except at the 0° cross section (types 45° vs. 75°, p < 0.05) (Fig. 4).
No significant difference was found when comparing α/β between the four types of trackings (except at the turning point); namely, the orientation of groove tracking was relatively consistent. In addition, amongst the 0°–105° of cross sections, the groove orientated medially at approximately 1° (range 0°–3°) along the trochlear groove except at approximately 10° (range 9°–11°) medially when at the turning point; namely, the extension of groove tracking was relatively smooth (Fig. 4).
Discussion
The most important finding of the study was that the trochlear groove tracking was consisted of the laterally orientated proximal and medially orientated distal parts marked by the turning point where the two parts connected. Another important finding was that the groove tracking was categorized into different types based on turning point location and morphological differences (shape, position, and orientation). The evaluation of the trochlear groove tracking in the present study was not only conducive to learn the anatomical landmarks for knee replacement surgery [13, 15], but also may contribute to the modification of current prosthesis. A reference value was also provided in this study for the diagnosis of patellofemoral diseases (patellar maltracking, trochlear dysplasia, etc.) in the clinical setting.
In a study of 100 human femurs, the natural groove orientation was found to follow a path, which could be approximated by two consecutive straight lines: a bilinear approximation [4]. Our finding was consistent with previous studies in that the anatomical morphology of the trochlear groove tracking could be described as bilinear [4, 11, 22]. In a study by Yue et al. [24], no difference in trochlear groove morphology was found between 20 male and 20 female Chinese subjects. Similarly, no significant difference in the position and orientation of trochlear groove tracking was observed between genders in the present study (n.s.). Another finding of the present study was the variation in turning points, with its location at 45°, 60°, 75°, and 90° cross sections. Based on this finding, the femoral trochlear groove was classified into types 45° (10.0 %), 60° (23.5 %), 75° (51.5 %), and 90° (12.5 %) in the present study. As for every 30° of knee flexion, 20° of patellofemoral flexion occurred [14]; hence, the 45°, 60°, 75°, and 90° cross sections of trochlear grooves could be roughly equal to 67.5°, 90°, 112.5°, and 135° knee flexions. Previously, a turning point at about 80° of knee flexion was observed in 100 cadavers by Barink et al. [4]; yet Varadarajan et al. [23] showed that the turning point appeared in 73.9–83.1 % of the trochlear groove tracking.
Compared to the natural knee, the prosthesis showed little variation in groove position through the entire trochlear length or did not have the same curve of groove tracking as a normal knee [3, 23]. A modern asymmetrically designed prosthesis with a groove orientation proximal lateral to distal medial across the anterior flange was thought to be beneficial to patellofemoral kinematics, but this was not supported by some research [3, 21, 23]. Over the proximal 27 % of the trochlea, the prosthetic groove was found to be located on average 2 mm more lateral than in normal knees; distally, the prosthetic groove was located on average 0.8 mm medial relative to its position in normal knees [23]. Intraoperative measurements showed that the prosthetic groove was located on average 2.5 mm medially relative to the normal groove [15]. Non-physiological forces resulting from changes in patellofemoral motion can contribute to patellofemoral pain, and patellar component loosening and wear [2, 5, 7].
For the femoral component, the mediolateral position of the trochlear groove varies at different flexion angles, and the design parameters are different amongst prosthesis systems [6]. Additionally, when assessing the changes in trochlear groove, individual patient anatomy was always ignored instead of average parameters [3, 21, 23]. Previously, the mediolateral position of the trochlear groove in 33 cadavers was found to be at 49.0 ± 3.7 % of the femur width in a study by Shih et al. [20]. As in our study, the variation of the position of the trochlear groove was found mainly in the proximal parts. The position order was types 45°, 60°, 75°, and 90° from the lateral to medial side, with the corresponding turning points located at −3.1, −2.8, −2.5, and −1.6 mm from the mechanical axis, respectively, and varied at different cross-sectional angles along the trochlear groove trackings. This difference changed substantially from proximal to distal on the trochlea and indicated the need for implants with anatomically designed trochlear grooves [23], while considering the natural anatomical variation. Additionally, the implanted position of the femoral component may vary between surgeons with different skills and may affect the postoperative trochlear groove position [15].
The orientation of the trochlear groove was relatively consistent and smooth amongst different types, which oriented at approximately 1° (range 0°–3°) medially from 0° to 105° cross sections except at approximately 10° (range 9°–11°) medially at the turning points in the present study. Based on the hypothesis that the motion of the patella would follow the articular geometry of the trochlea [10], 1° of medial orientation in the trochlear groove could partly explain patellar kinematics with the distal pole moving medially through 0°–90° of knee flexion [21]. A previous study found that the patella may rotate as much as 12°–15° with respect to the femur [19], with the rotation angle being similar to the total degree of medial orientation across its whole sector in the trochlear groove of the present study. In addition, 10° of orientation shift at the turning point would also provide determinant clues for patellar kinematics and the change of direct force on the patella. In a review of the literature, the reversal of the ‘screw home mechanism’ during the initial 30° of knee flexion derotated the tibia [19]. In addition, tibial internal rotation produced a ‘medial pivot’ motion in the mid-range extension [1, 9]. There would be an implicit idea that both 10° of medial orientation shift and tibia internal rotation had a ‘coupling effect’. However, the effect would be differed as the profile of the four types varied, and this needs to be further investigated. Although the mediolateral variation between types 45° and 60° was not significantly different, these knees were not classified into a same type.
In addition, the current protocol of TKA involves placement of the femoral component at 3° of external rotation to create a balanced flexion–extension gap and to favour patellar tracking [6, 21, 23]. It was reported that the femoral component rotation has a notable effect on the trochlear groove position and orientation [6, 23]. Therefore, following the current protocol, to facilitate the comparison between our results with parameters of prosthetic trochlear groove as in previous studies [21, 23], the three-dimensional coordinate in the present study was set at 3° of external rotation to the posterior condylar line in the axial alignment.
A main limitation of the present study was that physiological features (e.g. the width and height of the lateral and medial femoral condylar facet, and trochlear bisector angle) which are also important in prosthetic design and patellofemoral kinematics [6, 23] were not evaluated. Some anatomical differences between the types might be identified by further studies. Second, the bony morphology of the knee model was used, neglecting the geometry of the articular cartilage. Although the geometry of the cartilage surface differed from that of the bone in the trochlea, the difference was small [11, 20]. Third, the present study lacks clinical translational value in that there is no reference to current arthroplasty design; thus, further studies are needed.
Conclusions
The trochlear groove tracking varies greatly amongst a population that is categorized into four different types based on morphological differences, such as mediolateral positions of the proximal parts and angles of cutting planes for turning points. This study may be helpful for a better understanding of the natural trochlear groove anatomy, prosthetic design modification, and provide the reference value for studying patellofemoral diseases such as patellar maltracking and trochlear dysplasia.
References
Atzori F, Salama W, Sabatini L, Mousa S, Khalefa A (2016) Medial pivot knee in primary total knee arthroplasty. Ann Transl Med 4:6
Baldini A, Anderson JA, Cerulli-Mariani P, Kalyvas J, Pavlov H, Sculco TP (2007) Patellofemoral evaluation after total knee arthroplasty. Validation of a new weight-bearing axial radiographic view. J Bone Joint Surg Am 89:1810–1817
Barink M, Meijerink H, Verdonschot N, van Kampen A, de Waal Malefijt M (2007) Asymmetrical total knee arthroplasty does not improve patella tracking: a study without patella resurfacing. Knee Surg Sports Traumatol Arthrosc 15:184–191
Barink M, Van de Groes S, Verdonschot N, de Waal Malefijt M (2003) The trochlea is bilinear and oriented medially. Clin Orthop Relat Res 411:288–295
Barink M, Van de Groes S, Verdonschot N, De Waal Malefijt M (2006) The difference in trochlear orientation between the natural knee and current prosthetic knee designs; towards a truly physiological prosthetic groove orientation. J Biomech 39:1708–1715
Dejour D, Ntagiopoulos PG, Saffarini M (2014) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 22:2599–2607
D’Lima DD, Chen PC, Kester MA, Colwell CW Jr (2003) Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. J Bone Joint Surg Am Suppl 4:85–93
Eisenhuth SA, Saleh KJ, Cui Q, Clark CR, Brown TE (2006) Patellofemoral instability after total knee arthroplasty. Clin Orthop Relat Res 446:149–160
Freeman MA, Pinskerova V (2005) The movement of the normal tibio-femoral joint. J Biomech 38:197–208
Iranpour F, Merican AM, Baena FR, Cobb JP, Amis AA (2010) Patellofemoral joint kinematics: the circular path of the patella around the trochlear axis. J Orthop Res 28:589–594
Iranpour F, Merican AM, Dandachli W, Amis AA, Cobb JP (2010) The geometry of the trochlear groove. Clin Orthop Relat Res 468:782–788
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? J Arthroplast 15:424–429
Kuriyama S, Hyakuna K, Inoue S, Tanaka Y, Tamaki Y, Ito H, Matsuda S (2014) Is a “sulcus cut” technique effective for determining the level of distal femoral resection in total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 22:3060–3066
Lee TQ, Gerken AP, Glaser FE, Kim WC, Anzel SH (1997) Patellofemoral joint kinematics and contact pressures in total knee arthroplasty. Clin Orthop Relat Res 340:257–266
Meijerink HJ, Barink M, van Loon CJ, Schwering PJ, Donk RD, Verdonschot N, de Waal Malefijt MC (2007) The trochlea is medialized by total knee arthroplasty: an intraoperative assessment in 61 patients. Acta Orthop 78:123–127
Patel J, Ries MD, Bozic KJ (2008) Extensor mechanism complications after total knee arthroplasty. Instr Course Lect 57:283–294
Post WR (1999) Clinical evaluation of patients with patellofemoral disorders. Arthroscopy 15:841–851
Powers CM (2000) Patellar kinematics, Part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther 80:965–978
Schindler OS, Scott WN (2011) Basic kinematics and biomechanics of the patello-femoral joint. Part 1: the native patella. Acta Orthop Belg 77:421–431
Shih YF, Bull AM, Amis AA (2004) The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc 12:300–306
Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA (2014) No difference in patellar tracking between symmetrical and asymmetrical femoral component designs in TKA. Knee Surg Sports Traumatol Arthrosc 22:534–542
Varadarajan KM, Gill TJ, Freiberg AA, Rubash HE, Li G (2009) Gender differences in trochlear groove orientation and rotational kinematics of human knees. J Orthop Res 27:871–878
Varadarajan KM, Rubash HE, Li G (2011) Are current total knee arthroplasty implants designed to restore normal trochlear groove anatomy? J Arthroplast 26:274–281
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Gender differences in the knees of Chinese population. Knee Surg Sports Traumatol Arthrosc 19:80–88
Yue B, Wang J, Wang Y, Yan M, Zhang J, Zeng Y (2015) The intercondylar notch ceiling: an accurate reference for distal femoral resection in total knee arthroplasty for severely degenerated varus knees. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3792-4
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 81272037).
Author information
Authors and Affiliations
Corresponding author
Additional information
Shichang Chen and Zhe Du are joint first author and contributed by equal contribution.
Rights and permissions
About this article
Cite this article
Chen, S., Du, Z., Yan, M. et al. Morphological classification of the femoral trochlear groove based on a quantitative measurement of computed tomographic models. Knee Surg Sports Traumatol Arthrosc 25, 3163–3170 (2017). https://doi.org/10.1007/s00167-016-4236-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4236-5