Abstract
Purpose
This study aimed to identify factors associated with rotational mismatch after total knee arthroplasty (TKA) using fixed-bearing posterior stabilized prosthesis and to evaluate the impact of the rotational mismatch on clinical outcomes.
Methods
This retrospective cohort study included 159 cases that underwent TKA. Whole-leg computed tomography images were obtained 2 weeks after TKA, with three-dimensional measures of alignment. Rotational alignment of the femoral and tibial components and rotational mismatch between components and between the femur and tibia bones were evaluated. The new Knee Society Score (KSS) was obtained at the final outpatient visit, which was defined as the final follow-up timepoint. Predictive factors were identified for rotational mismatch of the lower extremity and poor new KSS.
Results
The mean follow-up period was 42 ± 16 months. Rotational mismatch ≥ 10° between bones was identified in 56 cases (35%), with a mean mismatch angle of 5.0° ± 9.1° of external rotation of the tibia relative to the femur. Rotational mismatch ≥ 10° between components was identified in three cases (2%; mean 0.3° ± 3.6° of internal tibial rotation). A multivariate regression analysis showed that component malrotation was predictive of post-operative rotational mismatch between bones (p < 0.01) and rotational mismatch ≥ 10° associated with poor new KSS (odds ratio 4.22; p < 0.01).
Conclusion
Malrotation of the fixed-bearing posterior stabilized TKA causes a rotational mismatch between the femur and tibia bones. Excessive rotational mismatch between bones greater than 10° is a risk factor for poor postoperative functional outcome. Precise component positioning is essential for improving TKA outcomes.
Level of evidence
III
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Precise alignment of the components of a knee prosthesis along the three planes of motion is important for obtaining good clinical results after total knee arthroplasty (TKA). Rotational malposition of the components has been associated with knee pain [17] and stiffness [2], increased pressure at the patellofemoral joint [28], and TKA revision [19]. Therefore, rotational alignment is especially important for successful TKA outcomes.
The rotational parameters of alignment include the position of the components (femur-to-femoral component or tibia-to-tibial component) and rotational mismatch between the long bones and/or components (femur-to-tibia or femoral-to-tibial component). However, the relationship between each parameter of lower limb alignment and rotational alignment of the prosthesis components has not been clearly established. A systematic review of rotational alignment after TKA highlighted the lack of assessments of rotational mismatch between the prosthesis components and between the long bones of the lower extremity [27]; therefore, the cause of rotational mismatch is unclear. Because the prosthetic design could affect rotation alignment [20], it is necessary to assess rotational parameters for the same prosthetic design. A fixed-bearing posterior stabilized (PS) prosthesis is one of the most commonly used TKA prosthesis globally [6, 8, 23]. As such, understanding the factors associated with malrotation of the components of the fixed-bearing PS prosthesis is clinically relevant. The hypotheses were that malrotation of the TKA components would correlate with post-operative rotational mismatch among bones or components, and that the presence of rotational mismatch would lead to poor clinical outcomes. The aims of this study were to clarify factors associated with rotational mismatch after TKA using a fixed-bearing PS prosthesis and to evaluate the impact of rotational mismatch on clinical outcomes.
Materials and methods
Patient selection
Eligible cases were consecutive TKA procedures performed at our institution between December 2012 and April 2017. Patients who underwent fixed-bearing PS TKA for the treatment of primary knee osteoarthritis (OA) with a varus deformity were included. Of the 357 included cases, 198 were excluded based on exclusion criteria, as follows: use of other design prostheses (n = 153); presence of a valgus deformity of the knee (n = 14); and TKA for diseases other than primary knee OA, such as rheumatoid arthritis, osteonecrosis, or post-traumatic knee OA (n = 31). Ultimately, a total of 159 TKAs were analysed in this study (Fig. 1).
Radiological parameters
For all patients, whole-leg plane radiographs and computed tomography (CT) images were obtained 2 weeks after TKA, with CT images obtained with patients in a supine position with the knee in full extension. To minimize radiation exposure, the diaphysis of the femur and that of the tibia were excluded from the CT image range. The hip–knee–ankle (HKA) angle was measured using the standing radiographs and SYNAPSE (version 02.03; FUJIFILM Medical Co. Ltd., Tokyo, Japan) [16]. The medial angle between mechanical axis of the femur and the tibia was defined as HKA angle, with a varus deformity defined by an angle < 178.5°, based on a previous report [11]. Coronal, sagittal, and rotational alignment of the components were measured using reconstructed 3-dimensional (3D) CT images (ZedKnee version 10.5; LEXI Co., Ltd., Tokyo, Japan) according to a previous report [25]. Rotational alignment of each component as well as rotational mismatch between the femur and tibia bones and between the femoral and tibial component were measured as the rotational parameters (Fig. 2). The reproducibility of the measurements was confirmed. For intra-observer reliability, each radiological parameter was measured twice, on 20 knees, at an interval ≥ 4 weeks by one orthopedic surgeon. For inter-observer reliability, two orthopedic surgeons measured each radiological parameter twice, on 20 knees, at an interval ≥ 4 weeks. The intra-class and inter-class correlation coefficients for the radiological measurements, respectively, were as follows: coronal alignment of the femur, 0.91 and 0.87; sagittal alignment of the femur, 0.90 and 0.89; rotational alignment of the femur, 0.91 and 0.84; coronal alignment of the tibia, 0.93 and 0.84; sagittal alignment of the tibia, 0.91 and 0.84; rotational alignment of the tibia, 0.93 and 0.92; rotational mismatch between the femur and tibia bones, 0.94 and 0.89; and rotation mismatch between the components, 0.98 and 0.95.
Schema of the three-dimensional (3D) measurement of the rotational parameters. A 3D image reconstructed from whole-leg computed tomography images is shown. Schema indicates the measured rotational alignment of the femoral and tibial components, rotational mismatch between the femur and tibia bones, and rotational mismatch between the femoral and tibial components
Definition of baseline measurements of alignment
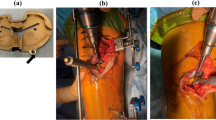
Baseline coronal and sagittal alignment of the prosthesis were measured as the angle of a line (relative to the coronal and sagittal plane) from the centre of the hip or ankle joint to the centre femoral and tibial component, respectively [25]. Rotational parameters were defined relative to the trans-epicondylar axis (TEA) of the femur and Akagi’s line of the tibia [1]. The TEA was drawn from the lateral epicondyle to the most prominent point on the medial epicondyle of the femur [4] (Fig. 3a). The Akagi’s line was drawn from the centre of the attachment of the posterior cruciate ligament to the medial surface of the tibial tuberosity (Fig. 3b). Differences between baseline and component measurements were used to define the alignment of the prosthesis components. Rotation of the femoral component was measured in the plane perpendicular to the femoral baseline (the line from the femoral head to the femoral component centre), and rotation of the tibial component was measured in the plane perpendicular to the tibial baseline (the line from the ankle centre to the tibial component centre). Rotational mismatch between the femur and tibia bones was defined by the angle between the TEA and Akagi’s line (Fig. 3c), with the angle between the centreline of the femoral and tibial components providing the rotational mismatch between components (Fig. 3d). Rotational mismatch between the femoral and tibial bones or between the femoral and tibial components was measured in the same plane. At first, the TEA or the centreline of the femoral component was drawn in the plane perpendicular to the femoral baseline. The drawn TEA or the centreline of the femoral component was then projected parallel onto the plane perpendicular to the tibial baseline automatically using software. Akagi’s line or the centreline of the tibial component was drawn in this plane. Finally, the rotational mismatch angle could be measured in the same plane (i.e., the plane perpendicular to the tibial baseline). A positive value was indicative of varus alignment with the component in the coronal plane, flexion or posterior tilt in the sagittal plane, or external rotation. A positive value of the angle between the TEA and Akagi’s line indicated an external rotation position of the tibia (or tibial component) relative to the femur (or femoral component). Outliers of prosthetic alignment in the coronal and sagittal planes were defined by an angle ≤3° or > 3°, with excessive rotational mismatch defined as an angle ≤10° or > 10°, as previously described [29].
Baseline measurement of each rotational parameter. The Baselines for 3D measurements of each rotational parameter are shown. A positive value indicates the position of the component in external rotation. a, b The trans-epicondylar axis (TEA) of the femur and Akagi’s line of the tibia measured at baseline are shown. The component rotations were measured in the plane perpendicular to each bone baseline. c Change in the angular position of the femur and tibia bones relative to baseline in cases of rotational mismatch between the femur and tibia bones. d Angle between the centreline of the femoral and tibial components indicative of rotational mismatch between components. Rotational mismatches were measured in the same plane. The drawn femoral baseline (TEA or the centreline of the component) in the femoral plane was projected parallel onto the tibial plane automatically using software
Clinical parameters
The conventional Knee Society Score (KSS) was evaluated before surgery and at the final follow-up according to previous methods [12]. The patient reported-outcome measurement portion of the new 2011 version of the KSS (new KSS) and the 12-item Forgotten Joint Score (FJS-12) were evaluated at the final follow-up [3, 21]. The lower quartile of the new KSS subscales was defined as a poor clinical outcome [5]. The following cut-off values were used: symptom score, ≤ 17 points; satisfaction, ≤ 20 points; expectations, ≤ 9 points; and functional activities, ≤ 43 points.
Surgical technique
The same fixed-bearing PS prosthesis (Vanguard PS, Zimmer Biomet, Warsaw, IN, USA) was used for all cases, and all TKA procedures were performed by the same surgical team using a medial para-patellar approach. The target position of the femoral and tibial components in both the coronal and sagittal planes was perpendicular to the mechanical axis. In the rotational plane, the femoral component was aligned to achieve an equal flexion and extension gap, with the position of the tibial component set manually to be parallel to Akagi’s line [15].
Statement of ethics
Informed consent was obtained from all patients before enrolment into the study. The protocol of this study was approved by the Osaka City University Institutional Review Board (ID number: 1280).
Statistical analysis
Continuous variables were described using means and standard deviations. Categorical variables were tabulated with absolute frequencies. All variables were confirmed as parametric using the Kolmogorov–Smirnov test. Baseline lower limb alignment and component alignment measures were compared between patients with and without excessive rotational mismatch using Student’s t test. The rates of excessive rotational mismatch between the femur and tibia bones and between the femoral and tibial components were compared using McNemar’s test, which is appropriate for comparisons of nominal variables within the same population. Correlations between component alignment and rotational mismatch among femorotibial bones and correlations between component rotational alignment and the new KSS subscales were analysed using Pearson’s correlation coefficient. A multivariate linear regression analysis controlling for confounding variables was used to identify factors predictive of rotational mismatch between the femur and tibia. A multivariate logistic regression analysis was used identify factors predictive of poor clinical outcomes according to the new KSS subscales.
The significant digits were set as follows: age, height, weight, follow-up period, the HKA angle, and clinical parameters were reported as integers; radiological parameters, except for the HKA angle, were reported to the first decimal place; the intra- and inter-class correlation coefficients, as well as correlation coefficients (r), standard coefficients, and odd’s ratio are reported to two decimal places.
To determine the adequate sample size, a power analysis was performed for each subscale of the new KSS. According to a previous report regarding the new KSS and rotational parameters, the expected difference between those with and without rotational mismatch for each subscale was as follows: symptoms, 3 ± 4 points; satisfaction, 5 ± 5 points; expectations, 2 ± 2 points; and functional activities, 16 ± 17 points [13]. Based on these differences in subscale scores, a sample size of 28 patients or more was determined to be adequate to provide appropriate power (β = 0.80) with the significance level set at 0.05. Statistical significance was defined as p < 0.05. Statistical analyses were performed using the R software package (version 3.1.1, R core team 2014: R Foundation of Statistical Computing, Vienna).
Results
Patient characteristics are presented in Table 1 and radiological parameters in Table 2. The histograms of rotational mismatches (Fig. 4c, d; Table 3) indicated that the incidence of excessive rotational mismatch was more frequent between the femur and tibia bones than between the femoral and tibial components. The functional activity subscore of the new KSS was significantly lower among patients with than without excessive rotational mismatch between the femur and tibia bones (Table 3). A significant positive correlation was identified between a rotational mismatch of the femur and tibia bones and the rotational alignment of the femoral and tibial components (Fig. 5c, f). On multivariate linear regression analysis, malrotation of the femoral and tibial components was an independent risk factor of rotational mismatch between the femur and tibia bones after surgery (Table 4). Moreover, excessive rotational mismatch between the femur and tibia bones was an independent risk factor for a poor functional activity score after surgery, with an odds ratio of 4.22 (Table 5; Fig. 6).
Histograms for each of the measured rotational parameters. The distribution of values for each rotational parameter is shown. a, b The alignments of femoral and tibial components tended to be an internal rotation. c, d The distribution of rotational mismatch between the femur and tibia bones shows a tendency for an external position of the tibia relative to the femur. The distribution shows the near absence of rotational mismatch between components. The frequency of cases of excessive rotational mismatch ( >|10°|) between the femur and tibia bones (n = 56) was significantly greater than that for excessive rotational mismatch between the components (n = 3, p < 0.01)
Correlation between the alignment of each prosthetic component and rotational mismatch between the femur and tibia bones. A significant positive correlation was identified between rotational mismatch of the femur and tibia bones and rotational alignment of the femoral (r = 0.43; p < 0.01) and tibial (r = 0.87; p < 0.01) components. Rotational mismatch between the femur and tibia bones was not correlated with any other alignment parameter of the components
Discussion
The most important finding of the present study was that malrotation of the femoral and tibial components resulted in rotational mismatch between the femur and tibia bones after TKA using a fixed-bearing PS prosthesis. Moreover, the resulting excessive rotational mismatch between the femur and tibia bones was an independent risk factor for a low functional activity KSS after TKA.
The use of 3D measurements is desirable for an accurate assessment of prosthetic alignment in the rotational plane [18]. To the best of our knowledge, no previous reports have measured rotational mismatch between the femur and tibia bones using 3D measurements and analysed the correlation between rotational mismatch and the clinical outcomes after TKA using fixed-bearing prosthesis in detail. Therefore, the findings of a greater incidence of excessive rotational mismatch between the femur and tibia bones than that between the femoral and tibial component and of a significant positive correlation between malrotation of femoral and tibial components and rotational mismatch of the lower extremity is clinically meaningful. It was also important that there were few rotational mismatches between the femoral and tibial components of the fixed-bearing PS prosthesis. This finding suggested that the fixed-bearing PS prosthesis itself does not have any capacity to absorb rotation mismatch of the lower extremity after TKA, despite the statement in the product manual of a ~ 15° tolerance of rotation between the femoral and tibial components. This study highlights the importance of precisely setting the femoral and tibial components when using a fixed-bearing PS TKA to prevent post-operative rotational mismatch between the femur and tibia bones.
The association of internal femoral malrotation and post-operative new KSS for functional activities has been reported [13]. Internal malrotation of the femoral component caused restriction of the natural knee kinematics in a cadaver study; however, its external malrotation caused few changes [10]. A recent systematic review showed that excessive internal rotation of the tibial component is a risk factor for poor functional outcomes after TKA, but that external rotation does not affect the results [19]. Rotational mismatch of more than 10° among the femoral and tibial components resulted in worse functional scores because of abnormal knee kinematics [14]. However, the association of rotational mismatch between the femur and tibia bones has been unclear until this study. Considering previous results and this study findings, post-operative functional activities could be relatively easily affected by component malrotation and rotational mismatch.
There are three approaches to address the issue of post-operative rotational mismatch. The first is improving the accuracy of aligning the components at the time of implantation by using computer-assisted navigation and patient-specific instrumentation to reduce the risk of excessive rotational mismatch [9, 22, 30]. The second is the adjustment of tibial component rotation according to the rotation of the femur after multiple extension-flexion movements with trial implants (i.e., range of motion technique) [7]. This might help to improve the accuracy of setting the implant rotation. The third is to increase the tolerance of the prosthesis itself to absorb rotational mismatch, as is possible when using a mobile-bearing prosthesis [24]. Therefore, selecting an adequate strategy to prevent post-operative rotational mismatch to improve clinical outcomes after TKA would be advantageous.
The advantages of this study are as follows. First, all radiological parameters of alignment were assessed using 3D measurements with high accuracy [26]. Second, all procedures were performed by the same surgical team using the same surgical approach and the same TKA prosthesis. Third, we evaluated the relationship between radiological findings and clinical outcomes at the final follow-up.
The clinical relevance of this study is to clarify the importance of avoiding malrotation of fixed-baring PS prosthesis for preventing rotational mismatch between the femur and tibia bones and postoperative poor functional activities.
The limitations of this study should also be acknowledged. First, this study findings are the result of analysing the fixed-bearing PS prosthesis used for knee osteoarthritis with varus deformity; therefore, they may not be applicable to other prosthesis designs, diseases, or deformities. Second, CT images used for 3D measurements were obtained with patients in the supine position with the knee in full (non-weight-bearing) extension. Because the rotational mismatch between the femoral and tibial components of the fixed-bearing PS TKA was not identified, the same results would be anticipated in the standing position with weight bearing because the constraint between the components of the prosthesis would only increase under vertical loading during weight bearing. However, this study was not designed to evaluate the rotational parameters in knee flexion; a further study would be warranted to clarify this issue. Third, pre-operative rotational mismatch was not measured in this study. The variations in pre-operative rotational mismatch or anatomical variance could possibly affect the post-operative results.
In conclusion, this study highlights the importance of accurate alignment of the femoral and tibial components of the fixed-bearing PS TKA to prevent post-operative rotational mismatch of the lower extremity. This study findings of a significant positive correlation between rotational mismatch between the femur and tibia bones after TKA and lower patient-reported functional score (measured using the new KSS) are the clinical importance. Precise component positioning is essential for improving TKA outcomes.
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Bédard M, Vince KG, Redfern J, Collen SR (2011) Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 469:2346–2355
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “Forgotten Joint” as the ultimate goal in joint arthroplasty. validation of a new patient-reported outcome measure. J Arthroplasty 27:430–436
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Black MM, Tilton N, Bento S, Cureton P, Feigelman S (2016) Recovery in young children with weight faltering: child and household risk factors. J Pediatr 170:301–306
Comfort T, Baste V, Froufe MA, Namba R, Bordini B, Robertsson O, Cafri G, Paxton E, Sedrakyan A, Graves S (2014) International comparative evaluation of fixed-bearing non-posterior-stabilized and posterior-stabilized total knee replacements. J Bone Joint Surg Am 96:65–72
Feczko PZ, Pijls BG, van Steijn MJ, van Rhijn LW, Arts JJ, Emans PJ (2016) Tibial component rotation in total knee arthroplasty. BMC Musculoskelet Disord 17:87
Graves S, Sedrakyan A, Baste V, Gioe TJ, Namba R, Cruz OM, Stea S, Paxton E, Banerjee S, Isaacs AJ, Robertsson O (2014) International comparative evaluation of knee replacement with fixed or mobile-bearing posterior-stabilized prostheses. J Bone Joint Surg Am 96:59–64
Hernandez-Vaquero D, Noriega-Fernandez A, Fernandez-Carreira JM, Fernandez-Simon JM, Llorens de los Rios J (2014) Computer-assisted surgery improves rotational positioning of the femoral component but not the tibial component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3127–3134
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Fuchs-Winkelmann S, Labey L (2018) Internal femoral component malrotation in TKA significantly alters tibiofemoral kinematics. Knee Surg Sports Traumatol Arthrosc 26:1767–1775
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip–knee–ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale for the knee society clinical rating system. Clin Orthop 248:13–14
Kawahara S, Okazaki K, Matsuda S, Nakahara H, Okamoto S, Iwamoto Y (2014) Internal rotation of femoral component affects functional activities after TKA-survey with the 2011 knee society score. J Arthroplasty 29:2319–2323
Lützner J, Kirschner S, Günther K-P, Harman MK (2012) Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop 36:1841–1847
Minoda Y, Iwaki H, Ikebuchi M, Yoshida T, Nakamura H (2012) The flexion gap preparation does not disturb the modified gap technique in posterior stabilized total knee arthroplasty. Knee 19:832–835
Mullaji AB, Shetty GM, Lingaraju AP, Bhayde S (2013) Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA? Clin Orthop Relat Res 471:134–141
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92:1238–1244
Okamoto S, Mizu-uchi H, Okazaki K, Hamai S, Tashiro Y, Nakahara H, Iwamoto Y (2016) Two-dimensional planning can result in internal rotation of the femoral component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:229–235
Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, Hirschmann MT (2018) Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1636–1644
Rhee SJ, Cho JY, Jeung SH, Poon KB, Choi YY, Suh JT (2018) Combined rotational alignment change after total knee arthroplasty in different tibial component designs: implications for optimal tibial component rotational alignment. Knee Surg Relat Res 30:74–83
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2012) The new knee society knee scoring system. Clin Orthop Relat Res 470:3–19
Silva A, Sampaio R, Pinto E (2014) Patient-specific instrumentation improves tibial component rotation in TKA. Knee Surg Sports Traumatol Arthrosc 22:636–642
Spekenbrink-Spooren A, Van Steenbergen LN, Denissen GAW, Swierstra BA, Poolman RW, Nelissen RGHH (2018) Higher mid-term revision rates of posterior stabilized compared with cruciate retaining total knee arthroplasties: 133,841 cemented arthroplasties for osteoarthritis in the Netherlands in 2007–2016. Acta Orthop 89:640–645
Tjørnild M, Søballe K, Møller Hansen P, Holm C, Stilling M (2015) Mobile-vs. Fixed-bearing total knee replacement: a randomized radiostereometric and bone mineral density study. Acta Orthop 86:208–214
Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K, Nakamura S, Takemura S, Nakamura H (2019) Two-dimensional measurement misidentifies alignment outliers in total knee arthroplasty: a comparison of two- and three-dimensional measurements. Knee Surg Sports Traumatol Arthrosc 27:1497–1503
Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K, Nakamura S, Takemura S, Nakamura H (2019) An accelerometer-based portable navigation system improved prosthetic alignment after total knee arthroplasty in 3D measurements. Knee Surg Sports Traumatol Arthrosc 27:1580–1586
Valkering KP, Breugem SJ, Van Den Bekerom MPJ, Tuinebreijer WE, Van Geenen RCI (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86:432–439
Verlinden C, Uvin P, Labey L, Luyckx JP, Bellemans J, Vandenneucker H (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait: an in vitro biomechanical study. J Bone Joint Surg Br 92:737–742
Watanabe S, Sato T, Omori G, Koga Y, Endo N (2014) Change in tibiofemoral rotational alignment during total knee arthroplasty. J Orthop Sci 19:571–578
Yamamura K, Minoda Y, Sugama R, Ohta Y, Nakamura S, Ueyama H, Nakamura H (2019) Design improvement in patient-specific instrumentation for total knee arthroplasty improved the accuracy of the tibial prosthetic alignment in the coronal and axial planes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05571-7
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ueyama, H., Minoda, Y., Sugama, R. et al. Malrotation of the fixed-bearing posterior stabilized total knee prosthesis causes a postoperative rotational mismatch between the femur and tibia. Knee Surg Sports Traumatol Arthrosc 28, 3810–3820 (2020). https://doi.org/10.1007/s00167-020-05864-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05864-2