Abstract
Background
Rotational mismatch between femoral and tibial components has been recognized as a risk factor of unsuccessful total knee arthroplasty (TKA), but a main cause of rotational mismatch is uncertain. This study aims to evaluate rotational alignment of the knee by measuring both component rotation and version of the knee in TKA.
Method
Fifty-one TKAs (mean age 73.7 years) were included in this study. The three dimensional, weight-bearing knee alignment was measured before and after TKA. A transepicondylar axis was referenced to femoral component rotation, and an anteroposterior axis of the tibia (middle of posterior cruciate ligament attachment to medial border of patella tendon attachment) was referenced to tibial component rotation. Knee rotational angle was defined as the angle between these two axes.
Result
The mean preoperative knee rotation angle of 9.7° (±8.5°) internal rotation was significantly reduced to 1.8° (±7.3°) external rotation after TKA. Twenty-one of 51 knees (41 %) exhibited rotational mismatch (>10°) preoperatively, and this number was reduced to eight knees (16 %) post-TKA. The femoral component was rotationally aligned within 5° of neutral in all knees, while rotational alignment of the tibial component showed a high degree of variability (range 20.7° internal rotation to 17.2° external rotation).
Conclusion
Rotational malposition of the tibial component was considered to be a main factor of rotational mismatch of the knee after TKA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rotational mismatch between femoral and tibial components is widely recognized as a crucial risk factor that may contribute to unsuccessful total knee arthroplasty (TKA), and may result in possible pain, stiffness, polyethylene wear and patellofemoral dysfunction [1–5]. Rotational mismatch is caused by a rotational malalignment of the components. Many studies have reported techniques to achieve correct rotational alignment [6–8]. Three main reference axes are used to guide the resection of the femur—the transepicondylar axis (TEA), the posterior condylar axis (PCA) with fixed amounts of external rotation of the component, and the trochlear antero-posterior axis (Whiteside’s line). The rotational position of the tibial component is traditionally referenced to the tibial tuberosity, although several alternate reference axes of the proximal tibia have been recently proposed, such as the PCA of the tibia, the transcondylar axis and the mid-sulcus line of the tibial spine [9, 10].
Furthermore, the version of the knee is another potential factor leading to the rotational mismatch of the femoral and tibial components [11–13]. It has been reported that not only is a varus or valgus deformity developed in osteoarthritis (OA), but that a rotational deformity of the knee can also occur as a result of the progression of the degeneration [14, 15]. In these cases, a rotational mismatch between the femoral and the tibial components can occur during TKA when using the measured resection technique since anatomical landmarks determine the alignment of each component separately. Theoretically, to obtain full function according to prosthesis design concept, femur and tibia should align in an anatomically neutral position, and also both femoral and tibial component should be implanted correctly. Thus, rotational alignment should be evaluated quantitatively by taking into account both the version of the knee as an intrinsic factor and the rotational alignment of the components as an extrinsic factor.
Despite an awareness of the rotational mismatch between components, little is known about rotational malalignment during TKA. One possible reason is that the rotational alignment of the tibia relative to the femur, as well as the rotational alignment of the TKA components themselves, cannot be accurately evaluated in routine radiographs. Computed tomography (CT) is used to assess rotational alignment in the transverse plane [2, 16, 17], although its frequent usage is limited because of the radiation dosage and cost. Other concerns with the use of CT are the difficulty in defining the true transverse plane perpendicular to the long axis of the bone in patients with a fixed knee deformity, and the ability to define the same anatomical reference point for the evaluation of a sequence of transverse CT images. We hypothesize that the preoperative rotational malalignment of the knee might persist to some extent after TKA, even though the femoral and tibial components were correctly implanted on each bone. The purpose of this study was to quantitatively measure how rotational alignment of the knee is changed after TKA.
Subjects and methods
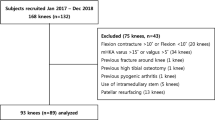
Ninety-five consecutive patients who underwent TKA at our institute during the period from 2005 to 2009 were recruited for this study, and informed consent was obtained. The protocol was approved by our institutional review board. Exclusion criteria included patients younger than 60 years of age, patients with previous knee surgery such as a high tibial osteotomy or osteosynthesis, absence of a complete set of outcome data, knees with a valgus deformity of more than 5°, knees with a severe flexion contracture, and patients with rheumatoid arthritis. Fifty-one osteoarthritic knees in 42 patients were subsequently included in the study. This cohort consisted of five men and 37 women with a mean age of 73.7 years [±5.9 years (±SD); range 61–87 years] at the time of the surgery. The mean preoperative femoro-tibial angle (FTA) was 186.5° (±5.7°), the mean preoperative extension angle (describe bellow) was 15.6° (±8.3°) and the mean preoperative flexion angle was 116° (±8.7°). The mean preoperative knee society score (KSS) was 63.1 (±6.8; range 37–74), and the mean follow-up period was 4.2 years (range 2.5–7 years).
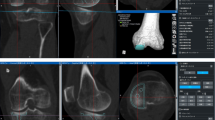
A weight-bearing, three-dimensional (3D), lower extremity alignment assessment system (KneeCAS, LEXI, Inc., Tokyo, Japan) was used for the quantitative measurement of knee alignment [18, 19]. This system consisted of a 2D–3D image matching technique using biplanar computed radiography (CR) and 3D bone models of the full-length lower extremity reconstructed from CT data. Biplanar CR images of each subject’s lower extremity were obtained in the weight-bearing, standing position with the knee fully extended and the toes in the neutral position. 3D digital bone models of each femur and tibia were reconstructed from the transverse CT images of the subject’s entire lower extremity using preoperative planning software (ZedView, LEXI, Inc., Tokyo, Japan). The anatomical coordinate systems and the reference axes used in the present study were established according to the method of Sato et al. [18] (Fig. 1). The 3D digital bone models were then projected onto the biplanar CR images by matching the silhouettes of the digital models to the contours of the respective CR images via 3D rotations and translations. A complete set of alignment parameters were then automatically calculated [20]. The accuracy of this 2D–3D image matching procedure was previously reported—the mean spatial errors were 0.5 mm in distance and 0.7° in rotation [21].
Bony reference points and anatomical coordinate axes defined on the femur and tibia. Solid lines represent the mechanical axes [18]
Component positions and sizes were determined from preoperative planning by applying the ZedView planning software to the CT data sets. In the coronal plane, the femoral component was oriented perpendicular to the femoral mechanical axis. The femoral component was slightly flexed by 2°–3° in the sagittal plane to avoid anterior cortical notching. The rotational position of the femoral component was set to the TEA. The tibial component was oriented perpendicular to the long axis of the tibia in the coronal plane, with a 5° posterior slope in the sagittal plane. The rotational position of the tibial component was determined using the anteroposterior axis described by Akagi et al. [22], which was defined as the line connecting the middle of the posterior cruciate ligament attachment and the medial border of the patellar tendon at its tibial attachment.
The Advance Medial Pivot Knee (Wright Medical Technology, Inc., Memphis, TN, USA) was used in all patients in this study. This knee implant was designed to reproduce the medial pivot motion of the natural knee by allowing a total of 15° of transverse rotation with flexion. A standard medial parapatellar approach was used, the posterior cruciate ligament was retained, the patella was not resurfaced, and no lateral releases were performed. A femoral intramedullary alignment guide was employed, and the valgus and external rotation angles as determined from preoperatively planning were established with a specially designed jig. A tibial extramedullary guide was used, and the anteroposterior axis defined on the proximal cut surface of the tibia was used for tibial rotational alignment. Minimum soft tissue releases were performed only when necessary, using a spacer block technique in extension and 90° flexion. All components were cemented.
Standing biplanar computed radiographic images were again obtained when the patients were able to stand postoperatively without difficulty. The postoperative lower extremity alignment was evaluated following the same technique as was used preoperatively. Note that no postoperative CT scans were needed, since the 3D bone models and anatomical references points and axes that were used for preoperative planning could also be used in these postoperative calculations. The 3D position and alignment of the components were also computed by the image matching technique with computer-aided design data of the femoral and tibial component provided by the manufacturer [19]. Thus, the postoperative lower extremity alignment and component position were measured three dimensionally, and the preoperative and postoperative alignment of the tibia relative to the femur was compared.
Definition of the knee axial alignment
The 3D longitudinal anatomic axes of the femur (ALA-f) and tibia (ALA-t) were automatically calculated from the lines connecting the centroids of cross sections along the femoral and tibial shafts, respectively (Fig. 2). The angle between the ALA-f and ALA-t, projected onto the femoral sagittal plane, was defined as the extension angle. The angle between the ALA-f and ALA-t, projected onto the femoral coronal plane, was defined as the varus–valgus (adduction–abduction) angle. The FTA was measured by this method with the patient in the standing position [18].
3D longitudinal anatomical axes (dotted lines) of the femur (ALA-f) and tibia (ALA-t) projected onto the femoral coronal and sagittal planes [18]. The angle between ALA-f and ALA-t was defined as the varus–valgus angle in the coronal plane and the extension angle in the sagittal plane
Definition of the knee rotation angle
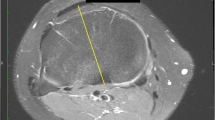
The surgical TEA was identified as the line that connected the lateral epicondylar prominence and the lowest point of the medial sulcus of the medial epicondyle [6]. If the medial sulcus could not be identified, the clinical TEA based on the most prominent point of the medial epicondyle was selected. The line through the midpoint and perpendicular to the TEA was defined as the femoral antero-posterior (AP) axis. The antero-posterior axis described by Akagi et al. [22] was selected as the tibial AP axis. The knee rotation angle was defined as the angle between the femoral AP axis and the tibial AP axis, projected onto the femoral transverse plane (Fig. 3). Based on a CT study of normal knees [22, 23], the target knee rotational angle was taken to be zero degrees. In this present study, negative values were used to indicate internal rotation of the tibia relative to the femur, with positive values as external rotation.
The angle between the tibial AP axis and the perpendicular to the femoral TEA was defined as the knee rotation angle in the femoral transverse plane. TEA transepicondylar axis, P middle of the tibial attachment of the posterior cruciate ligament, A medial border of the patellar tendon attachment at the tibial tuberosity. Dotted lines contour of projected femoral condyle onto the femoral transverse plane. Solid lines contour of projected tibial condyle onto the femoral transverse plane
Recent studies have shown that the optimal rotational alignment of the femoral component is within 5° of the femoral TEA [8, 24]. To our knowledge, however, no consensus has been reached as to the optimal rotational alignment of the tibial component [7, 9, 10, 17, 25–27]. In this present study, the rotational alignment of the tibial component was set to within 5° of its reference axis as described above. Knee rotational mismatch was defined as a knee rotational angle >10°.
3D evaluation of component alignment
The positions of the components relative to the bones were calculated from the spatial relationship between the anatomic coordinate systems and the component coordinate systems. The varus–valgus angle of the components was defined as the angle between the mechanical axis and the component’s Z-axis (proximal–distal) in the anatomical coronal plane. The flexion–extension angle of the components was calculated between the mechanical axis and the component’s Z-axis in the anatomical sagittal plane. The rotational angle of the femoral component was determined with respect to the femoral TEA in the femoral transverse plane. The rotational angle of the tibial component was defined with respect to the tibial AP axis in the tibial transverse plane [19]. The rotational mismatch of the tibial component relative to the femoral component was calculated between the projected femoral component X-axis (medio-lateral) onto the femoral transverse plane and the projected tibial component X-axis onto the femoral transverse plane. In addition to respective rotational alignment of components, the combined rotation of the femoral component and the tibial component was also calculated.
The knee rotational angle was compared between pre-TKA and post-TKA states. Knees with a rotational angle of <10° were considered to be properly aligned and were included in the ‘rotationally matched’ group, while knees with a rotational angle >10° were considered to be malaligned and were included in the ‘rotationally mismatched’ group. Statistical analysis was performed using SPSS 14.0 J (SPSS, Inc., Chicago, IL, USA). Normality of the data was checked using the Shapiro–Wilk test, and the Student’s t test or Mann–Whitney U test was appropriately selected. The Fisher’s exact test was used to compare frequencies of component malposition between the rotationally matched and mismatched knee groups after TKA. The level of statistical significance was set at a p value ≤0.05.
Results
There were no complications clinically, and the mean KSS significantly improved to 94.8 (±4.5) postoperatively (p < 0.01). The mean postoperative FTA was 175.7° (±3.3°) (p < 0.01), the mean postoperative extension angle was 14.6° (±7.6°) (p = 0.24), and the mean postoperative flexion angle was 116.8° (±12.4°) (p = 0.67). The mean knee rotational angle pre-TKA was −9.7° (±8.5°; range −30.7° to 5.6°), with 21 knees (41 %) falling within the mismatched group. After TKA, knee rotational malalignment was significantly improved (p = 0.002), with a mean knee rotational angle of +1.8° (±7.0°; range −14.2° to +15.3°). Figure 4 showed the distribution of both preoperative and postoperative FTA and knee rotational angle, and a weak association was found between preoperative FTA and the knee rotational angle (correlate coefficient 0.33). Forty-three knees (84 %) were included in the rotationally matched group, while eight knees (16 %) fell within the mismatched group. Seventeen of the 21 knees (81 %) that exhibited preoperative rotational malalignment were improved with surgery, while four knees remained rotationally malaligned and in the mismatched group. Twenty-six of the 30 knees (87 %) that did not demonstrate preoperative rotational malalignment preserved their rotational alignment after TKA, while four knees lost their rotational alignment postoperatively and fell within the mismatched group.
The axial alignment of the components is summarized in Table 1. There were no significant differences in alignment of the femoral and tibial components between the matched and mismatched groups in both coronal and sagittal planes. The rotational alignment of the components is summarized in Table 2. All femoral components were rotationally aligned to within 5° of neutral in both groups. However, the rotational position of the tibial components exhibited a high degree of variability, ranging from −20.7° to +17.2°. In the mismatched group, four knees showed excessive (>10°) external rotation of the tibia relative to the femur, and all of these demonstrated more than 5° of internal rotation of the tibial component (mean −12.1°; range −5.2° to −17.2°). The remaining four knees in the mismatched group showed excessive (>10°) internal rotation of the tibia relative to the femur, and all of these exhibited external rotation of the tibial component (mean 8.9°; range +0.3° to +17.2°). The rotational position of the tibial components in two of the four excessive internally rotated knees were within 5° from neutral, while the remaining two mismatched knees had tibial components that were in more than 5° of external rotation. There was no significant difference in the number of tibial components with rotational malalignment of more than 5° between the two groups (p = 0.26). However, if the cutoff value for normalcy was set to more than 8°, a significant difference in the frequency of tibial component rotational malalignment was found (p = 0.03). There was no significant difference in the rotational alignment of the tibial component relative to the femoral component between the matched and mismatched groups (p = 0.41). Three of four excessive externally rotated knees showed small external rotation of femoral component with large internal rotation of tibial component, while the one remaining knee showed both components internal rotation. All of four excessive internally rotated knees showed a small internal rotation of the femoral component with external rotation of the tibial component.
Discussion
Rotational mismatch of the knee causes several clinical problems. The excessive internal rotation of the tibia causes toe-in gait. The excessive external rotation of the tibia causes lateral translation of the tibial tuberosity, resulting in increased Q-angle and maltracking of the patella. Rotational mismatch of the knee also restricts rotation of the tibiofemoral joint, and it may limit to obtain full knee joint kinematics according to prosthesis design concept.
This study measured the transverse rotation angle between the femur and tibia pre-TKA and post-TKA, and the rotational alignment of the femoral and tibial components relative to their respective bones. Twenty-one of 51 knees (41 %) demonstrated more than 10° of rotational malalignment preoperatively, whereas only eight knees (16 %) showed rotational malalignment after TKA. TKA significantly improved the rotational alignment of 84 % of the knees (p = 0.002). The alignment of the femoral and tibial components relative to their respective bones in the matched group were at an average of 0.4° of internal rotation and 2.9° of internal rotation, respectively. The components were also well aligned in the coronal and sagittal planes, suggesting that proper component placement corrected knee rotational malalignment.
Uehara et al. [13] reported that 11 % of the knees of patients who had TKA demonstrated more than 10° of rotational mismatch, as measured by CT. Matsui et al. [15] reported that the rotational deformity of the knees increased proportionally with the grade of OA. In the present study, the preoperative incidence of knee rotational malalignment was relatively high. Under the weight-bearing condition, knees with medial OA were likely in more varus due to the lateral thrust. Weight-bearing may have also enhanced the rotational malalignment.
Eckhoff et al. [11] reported that the intrinsic rotational deformity should be addressed in order for a TKA to succeed. In spite of our best efforts with TKA surgery, in this study we found that preoperative rotational mismatch persisted in two of 51 cases, suggesting that even with correct component placement relative to the anatomical landmarks, rotational mismatch of the knee could still occur. The risk of persistent rotational mismatch of the knee might be higher with a low conformity or mobile bearing implant design. With a high conformity implant design, on the other hand, rotational incongruity between the femoral and tibial components would result in increased contact stresses when rotational malposition of the components existed.
The most important factor causing rotational mismatch after TKA was found to be rotational malpositioning of the tibial component. Recent studies reported a large variation in tibial rotational position, even when evaluated using computer assisted surgery [17]. Nicoll and Rowley [27] reported that internal malposition of the tibial component led to residual pain after TKA, and that their threshold value of tibial component rotational position was 9°. Barrack et al. [4] reported that TKAs with anterior knee pain showed an average of 6.2° of internal rotation of the tibial component. Bedard et al. [26] reported increased stiffness after TKA that was related to internal malpositioning of the components, especially on the tibial side. In the present study, eight knees showed rotational mismatch after TKA, and six of these knees exhibited rotational malpositioning of the tibial component. Since there is no clear definition of optimal rotational alignment of the tibial component, we set a criterion for rotational alignment of the tibial component to be within 5° of neutral. If a threshold value of tibial component rotation was set to within 8°, we found a significant difference between the matched group and mismatched group (p = 0.03), which was comparable to previous reports. During the follow-up period, there were no symptomatic complications such as patellofemoral dysfunction or loosening of the component in the mismatched group. It is necessary to evaluate long-term results to elucidate if or how rotational mismatch relates to modes of TKA failure.
The limitation of this study was the relatively small number of subjects and that all subjects were of Asian descent. The results in this study may not be applicable to all types of TKA designs. Our selection of anatomical references may have affected the results. Reported reproducibility of defining the femoral TEA is controversial [8, 24], and relatively large anatomical variability and poor reproducibility has been recognized when locating the tibial AP axis [10]. Based on the same method as in this present study, the knee rotational angle, as measured in 82 normal knees, was previously reported to be an average of 4.3° external rotation of the tibia relative to the femur [20], with a large variation ranging from −25.1° to 16°. In this study, rotational alignment of the components was set by referencing the femoral TEA and the tibial AP axis, and neutral rotation of the knee was set at 0° [22, 23]. It is difficult to compare knee rotational alignment between subjects with different stages of OA and axial alignment. However, the current study focused mainly on how knee rotational alignment changed after TKA. We directly compared knee rotational angle between pre-TKA and post-TKA using the same anatomical reference points and axis definitions. Therefore, any errors related to the selection of the reference points were minimized. The presence of a flexion contracture and/or varus/valgus deformity affects the calculated value of rotational alignment. In this study, however, knees with severe flexion contractures were excluded. We have also thoroughly documented the errors associated with this measurement technique, and found that a slight flexion contracture and varus deformity had only a small affect on the measured rotational values (e.g., a 10° flexion contracture with a 15° varus deformity yielded an apparent internal rotation of 2.6°). Thus, we believe that these measurement errors did not change the main results of this study.
In summary, we used a 3D lower limb alignment assessment system to evaluate rotational alignment of the knee before and after TKA, taking into account both component alignment and version of the knee. Rotational malalignment after TKA was significantly improved. Rotational malposition of the tibial component was the main factor related to post-TKA rotational mismatch of the knee.
References
Eckhoff DG, Metzger RG, Vandewalle MV. Malrotation associated with implant alignment technique in total knee arthroplasty. Clin Orthop Relat Res. 1995;321:28–31.
Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–53.
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007;458:131–6.
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:46–55.
Wasielewski R, Galante J, Leighty R, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43.
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–7.
Incavo SJ, Coughlin KM, Pappas C, Beynnon BD. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty. 2003;18:643–8.
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Jt Surg Am. 2005;87:2276–80.
Huddleston JI, Scott RD, Wimberley DW. Determination of neutral tibial rotational alignment in rotating platform TKA. Clin Orthop Relat Res. 2005;440:101–6.
Siston RA, Goodman SB, Patel JJ, Delp SD, Giori NJ. The high variability of tibial rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:65–9.
Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD. Version of the osteoarthritic knee. J Arthroplasty. 1994;9:73–9.
Nagamine R, Miyanishi K, Miura H, Urabe K, Matsuda S, Iwamoto Y. Medial torsion of the tibia in Japanese patients with osteoarthritis of the knee. Clin Orthop Relat Res. 2003;408:218–24.
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamamoto Y. Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2002;402:196–201.
Yagi T. Tibial torsion in patients with medial-type osteoarthritic knees. Clin Orthop Relat Res. 1994;302:52–6.
Matsui Y, Kadoya Y, Uehara K, Kobayashi A, Takaoka K. Rotational deformity in varus osteoarthritis of the knee. Clin Orthop Relat Res. 2005;433:147–51.
Jazrawi L, Birdzell L, Kummer J, Di Cesare PE. The accuracy of computed tomography for determining femoral and tibial total knee arthroplasty component rotation. J Arthroplasty. 2000;15:761–6.
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty: three-dimensional evaluation of implant alignment and rotation. J Bone Jt Surg Am. 2007;89:236–43.
Sato T, Koga Y, Omori G. Three-dimensional lower extremity alignment assessment system: application to evaluation of component position after total knee arthroplasty. J Arthroplasty. 2004;19:620–8.
Sato T, Koga Y, Sobue T, Omori G, Tanabe Y, Sakamoto M. Quantitative 3-dimensional analysis of preoperative and postoperative joint lines in total knee arthroplasty: a new concept for evaluation of component alignment. J Arthroplasty. 2007;22:560–8.
Ariumi A, Sato T, Kobayashi K, Koga Y, Omori G, Minato I, Endo N. Three-dimensional lower extremity alignment in the weight-bearing standing position in healthy elderly subjects. J Orthop Sci. 2010;15:64–70.
Kobayashi K, Sakamoto M, Tanabe Y, Ariumi A, Sato T, Omori G, Koga Y. Automated image registration for assessing three-dimensional alignment of entire lower extremity and implant position using bi-plane radiography. J Biomech. 2009;42:2818–22.
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. 2004;420:213–9.
Aglietti P, Sensi L, Cuomo P, Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008;466:2751–5.
Yau W, Chiu K, Tang W. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty. 2007;22:1042–8.
Ikeuchi M, Yamanaka N, Okanoue Y, Ueta E, Tani T. Determining the rotational alignment of the tibial component at total knee replacement. J Bone Jt Surg Br. 2007;89:45–9.
Bedard M, Vince K, Redfern J, Collen SR. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res. 2011;469:2346–55.
Nicoll D, Rowley D. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Jt Surg Br. 2010;92:1238–44.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Watanabe, S., Sato, T., Omori, G. et al. Change in tibiofemoral rotational alignment during total knee arthroplasty. J Orthop Sci 19, 571–578 (2014). https://doi.org/10.1007/s00776-014-0565-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0565-8