Abstract
Purpose
For years, numerous studies have been performed to determine whether mobile-bearing total knee arthroplasty (MB-TKA) or fixed-bearing total knee arthroplasty (FB-TKA) is the preferential design in total knee arthroplasty. Reviews and meta-analyses on this subject have focused on a relatively small number of randomised controlled trials, possibly missing important results of smaller studies. The goal of this review was to provide a comprehensive overview of all literature comparing MB-TKA and FB-TKA in the treatment of osteoarthritis of the knee.
Methods
An extensive literature search was performed in the PubMed database. All studies that compared MB-TKA with FB-TKA and looked at one of four theorised advantages (insert wear, signs of loosening, survival rate of the prosthesis and clinical outcome) were included.
Results
The initial search yielded 258 articles, of which 127 were included after the first screening. The included studies consisted of 9 meta-analyses, 3 systematic reviews, 48 RCT’s, 44 comparative studies, 10 reviews and 13 studies that examined patients who received bilateral TKA (one MB-TKA and one FB-TKA). Combining the results of all studies showed that almost all studies found no difference between MB-TKA and FB-TKA.
Conclusions
Even when examining all different types of studies on MB-TKA and FB-TKA, the results of this review showed no difference in insert wear, risk of loosening, survivorship or clinical outcome. In daily practice, the choice between MB-TKA and FB-TKA should be based on the experience and judgment of the surgeon, since no clear differences are observed in the scientific literature.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the first mobile-bearing total knee arthroplasty (MB-TKA) procedures have been performed in the 1980s [21], numerous scientific studies have compared MB-TKA with fixed-bearing total knee arthroplasty (FB-TKA) [3, 21, 55, 95, 100, 130, 133]. The mobile-bearing design was developed to allow rotation of the insert around the longitudinal axis (“rotating platform”) or to allow anterior–posterior translation between the insert and the tibial tray of the prosthesis (“meniscal bearing”). Due to the rotational and the translational properties between the insert and the tibial tray, the mobile-bearing insert can be modelled such that they have a better fit with the femoral component without compromising the natural rotation and translation between femur and tibia. This is contrary to the fixed inserts in FB-TKA, which are relatively flat and, therefore, allow some small rotations and translations, but much smaller compared to the MB-TKA [105].
MB-TKA has been theorised in the literature to result in four advantages over FB-TKA: reduced insert wear, less risk of loosening, fewer revisions and better clinical outcome. Firstly, MB-TKA is expected to result in less polyethylene wear because of a larger contact surface between the femoral component and the insert, induced by a more optimal fit of the femoral component and the insert [30]. In addition, the insert can rotate and translate relative to the tibial component, which means that the femoral component slides less on the surface of the insert, which also potentially results in less wear. Secondly, MB-TKA is hypothesised to reduce the chance of loosening of the prosthesis because of less osteolysis [30]. This is thought to be due to the movement of the insert on the tibial tray, resulting in less stress on the bone–cement interface of the tibial component, and less wear-induced osteolysis. The third advantage described in the literature is that less wear and loosening result in a lower number of revisions and, therefore, a better survivorship of the prosthesis [20]. The final theorised advantage of MB-TKA is better clinical outcome. The mobility and design of the insert are hypothesised to result in a more natural movement of the prosthetic knee in daily life. Several disadvantages of MB-TKA have also been described. A known complication of MB-TKA is dislocation of the insert [51, 130]. During surgery, a high level of precision in balancing of the flexion and extension gap is necessary to prevent dislocation or spin-off of the insert. Therefore, MB-TKA is acknowledged to be associated with a prolonged learning curve and an increased risk of soft tissue impingement [30]. Additionally, the fact that in MB-TKA there is a second articulating surface could be a risk for increasing wear as a larger surface of the insert is exposed to friction [30, 130].
In particular, in the last ten years, an increased number of high-quality articles have been published that have studied one or more of the four theorised advantages of MB-TKA. Reviews and meta-analyses have been performed to provide an overview of all the literature available, none finding any significant differences. However, these often include the same studies with a high level of evidence. Several studies have been performed that provide valuable information on MB-TKA and FB-TKA, but are omitted from these overviews because of their methodology. The goal of the present paper is to present an up-to-date overview of the scientific literature that includes studies of different levels of evidence that compare cemented MB-TKA with cemented FB-TKA with respect to insert wear, signs of loosening of the prosthesis, survivorship of the prosthesis and clinical outcome, and to arrive at an evidence-based advise with regard to the preferable type of insert.
Materials and methods
Search strategy
The PubMed MEDLINE database was searched for English language meta-analyses, (systematic) reviews, randomised controlled trials and comparative studies. The search terms used were: mobile bearing, rotating platform, meniscal bearing and anterior–posterior glide rotation. Fixed and total or TKA needed to be present as keywords. Unicompartmental and hemi were excluded in the search. The last search was performed on 17 February 2015. The complete search string can be found in Table 6 in “Appendix”
Eligibility criteria
Two independent reviewers (BF and DD) screened the results of the search, first using the title and abstract of the articles and second using the full text of the remaining articles to identify those eligible for inclusion. Studies comparing clinical, radiological and/or functional results of MB-TKA and FB-TKA were eligible for inclusion. The primary indication for TKA had to be osteoarthritis. In vitro studies, studies with kinematic results or studies that used biomechanical models, were excluded, as well as studies that focused on complete polyethylene tibial components or uncemented prostheses. In the current study, no differentiation was made between meniscal bearing and rotating platform subtypes of MB-TKA or between cruciate retaining and posterior stabilised prostheses.
Eligible articles of which the full text could be retrieved and which reported results on one or more of the four theorised advantages of MB-TKA were included. Wear of the insert had to be assessed by measuring the thickness of retrieved inserts, or using the Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System [35], or similar radiological measurement methods. The risk of loosening of the prosthesis had to be reported in the form of radiolucencies or osteolysis around the bone–cement interface. With respect to survivorship and the number of revisions, only those studies were included that reported survival as a result of aseptic loosening. Clinical outcome had to be compared by patient-reported outcome questionnaires looking at pain and functional impairment or by measuring the range of motion by looking at flexion and extension of the knee. In the case of disagreement about an article, this was resolved through a discussion between the reviewers.
Data collection
The following information was extracted from the included studies: author, year of publication, study design (meta-analysis, (systematic) review, randomised controlled trial, comparative study), level of evidence, type of prosthesis, number of prostheses, age of the MB group, age of the FB group and duration of follow-up. In addition, the main results of the articles were studied to see what results they reported for each of the four main outcome categories. For each outcome category that was reported in the article, the result was summarised as either MB = FB (no difference between MB-TKA and FB-TKA), MB (outcome favours MB-TKA) or FB (outcome favours FB-TKA). When several follow-up measurements were reported within a study, the final measurements were used for summarising the results. If a study did not perform a statistical analysis on an outcome category, no result was formulated for that specific category. If a study did not report consistent results within one of the four main outcome categories, there was no final conclusion made for that particular category. If a preference for a type of bearing was reported by patients who participated in bilateral comparative studies, this was also registered.
Data analysis
Final conclusions were based on the studies with the highest level of evidence (LoE), as determined by the reviewers using the criteria reported by several orthopaedic journals [108, 117, 140]. Bilateral comparative studies (where patients received a MB-TKA in one knee and a FB-TKA in the other knee) were considered as level 1 and non-systematic reviews as level 3. If information needed for determining the level of evidence was missing, the level of evidence was reported as one level lower. Because of the large amount of studies included in the current overview, conclusions on the four main categories were primarily drawn by analysing the studies with LoE 1, since these studies are considered to have the highest methodological quality. Afterwards, the results from studies with LoE 2 and 3 were analysed to see whether the results from those studies provided a different view.
Results
Search, Selection and Study characteristics
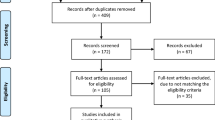
The PubMed search resulted in 258 articles, 121 of which were excluded based on abstract or title (Fig. 1). A full-text version was retrieved of the remaining 137 studies. After reading the full text, another 10 articles were excluded. Six of them did not report on the predetermined outcome variables, two articles had included uncemented prostheses in their analyses, and two articles were excluded because of comparing their own MB-TKA data with literature instead of their own FB-TKA data. All 127 studies are described in Table 1. The included studies consisted of 44 comparative studies (CS), 48 randomised controlled trials (RCT), 13 bilateral studies that compared MB-TKA in one knee and FB-TKA in the other (BiL), 10 reviews (R), three systematic reviews (SR) and nine meta-analyses (MA). No articles from before 2001 were found. Figure 2 shows the number of included papers that was published each year.
Study flow diagram [86]
Insert wear
Results of the LoE 1 studies that reported on insert wear are detailed in Table 2. All five studies, two of which were bilateral studies, did not find a difference between MB-TKA and FB-TKA when looking at the radiological signs of insert wear. When looking at the LoE 2 and 3 studies, all LoE 2 studies and four out of seven LoE 3 studies did not find a difference between MB-TKA and FB-TKA (Table 7 in “Appendix”). Three LoE 3 studies reported a significant difference in wear in favour of MB-TKA.
Signs of loosening of the prosthesis
Twenty-eight LoE 1 studies reported radiolucencies or osteolysis (Table 3). All studies except for 1 reported no difference for any of these variables. The exception was an RCT by Bailey et al. [5], who reported a significantly higher percentage of radiolucencies around the tibial component in MB-TKA. The LoE 2 and 3 studies did not find a difference between MB-TKA and FB-TKA (Table 8 in “Appendix”).
Survivorship
Table 4 shows all results on survival rate and number of revisions. Twenty-five LoE 1 studies were included, and none of these found a significant difference in either survival or revision rate between MB-TKA and FB-TKA. One LoE 2 study and three LoE 3 studies reported a significant difference in favour of FB-TKA for this parameter (Table 9 in “Appendix”).
Clinical outcome
All clinical outcome results can be found in Table 5. Overall conclusion of the 50 LoE 1 studies was that there was no difference between MB-TKA and FB-TKA in almost all studies (n = 47), with 2 studies reporting results in favour of MB-TKA and 1 study reporting results in favour of FB-TKA. One LoE 2 study and four LoE 3 studies showed clinical outcome results in favour of MB-TKA, opposed to only one that showed more benefits of FB-TKA. However, the other 53 LoE 2 and 3 studies reported no differences (Table 10 in “Appendix”).
Discussion
The most important finding of the present study was an absence in difference between MB-TKA and FB-TKA. When comprehensively reviewing all available literature, type of bearing in TKA did not appear to influence insert wear, signs of loosening, survival rate of the prosthesis and clinical outcome. Both the enlarged contact surface and the reduction in movement of the femoral component on the surface of the insert in MB-TKA were hypothesised to result in less polyethylene wear [30]. The studies with the highest LoE included in this overview did not show differences between MB-TKA and FB-TKA in insert wear. This could be explained by the fact that insert wear is rare altogether and occurs late in the life cycle of a prosthesis. Since the 15-year survival rate of TKA is known to be above 90 % [78], only a very small number of patients have revision surgery because of insert wear. With this in mind, studies with large numbers of patients and a very long follow-up are necessary to be able to determine a difference in insert wear between MB-TKA and FB-TKA. Since in vitro studies also have not been able to produce consistent results on insert wear [28, 39, 41, 82, 88], a possible decrease in insert wear does not appear to be an argument in choosing between MB-TKA and FB-TKA. However, when looking at studies included in this overview with a lower LoE, three out of seven LoE 3 studies showed results in favour of MB-TKA. Studies that include retrieved inserts are essential in assessing actual insert wear, but unfortunately this type of research is categorised in a lower LoE and, therefore, often overlooked. The fact that several LoE 3 studies find that MB-TKA appears to be associated with less insert wear is, therefore, noteworthy, but does not seem to be associated with differences in function, outcome or survival.
Taking the LoE of studies into account, the current study shows that radiolucencies and osteolysis around MB-TKA do not differ significantly from FB-TKA. The only LoE 1 study that found a higher percentage of tibial radiolucencies in MB-TKA also showed that this difference did not influence clinical outcome in their patients [5] and, therefore, this higher percentage seems not to be clinically relevant. It should be noted that the patients in this study were only evaluated at a maximum of 2-year follow-up. Whether the increase in tibial radiolucencies found in their MB-TKA group influences revision rates after 10 or 15 years is, therefore, unknown.
Several studies mentioned the number of revisions, but did not perform a statistical analysis to evaluate the differences. It was often unclear whether the revisions were caused by aseptic loosening or all causes. The LoE 1 studies did not show differences in the number of revisions. It is worth mentioning that three studies with a LoE of 2 or 3 showed a lower survival rate for MB-TKA compared to FB-TKA.
In this literature overview, patient-reported outcomes of questionnaires were included to quantify clinical outcome. The included literature showed that the experienced clinical outcome after undergoing MB-TKA did not differ from patients who underwent FB-TKA. The pain scores and ranges of motion of the knee also did not differ between both types of bearing. Besides, it has been shown that differences found in range of motion and questionnaires are hard to translate to clinically important differences, since these differences can fall within the variation of normal range of knee motion [105]. Furthermore, differences in objective measurements, like range of motion, do not appear to relate directly to the subjectively experienced quality of movement [115]. Based on this reasoning, in combination with the high amount of studies that did not find any differences in both the questionnaire results and the range of motion between MB-TKA and FB-TKA, it can be concluded that there is no difference between MB-TKA and FB-TKA in clinical outcome.
A strength of the current literature overview is the large number of included studies. In the first Cochrane review on this subject in 2004, only 2 articles were of sufficient methodological quality to be included [55]. Scientific research on MB-TKA has increased dramatically after this review, and out of the 127 studies included in the current study, 51 were LoE 1. The present paper provides an overview of both high and lower LoE studies that has not been presented earlier. Another strength is the fact that results were included on four different theorised advantages of MB-TKA, and, therefore, a more complete picture of the results of MB-TKA in comparison with FB-TKA is given.
There are also several limitations to the current study. Included studies were categorised according to their level of evidence [108, 117, 140]. Although this method has proven reliable and has been widely accepted for classifying methodological designs [13, 94], this classification does not fully address the methodological quality [99]. The results of several studies have been included twice, since several RCT and CS studies that were included are also used in the SR and MA studies. It is possible that a small number of studies have not been included because only the PubMed database was searched. However, the chance that these studies would alter the conclusions of this study is small, considering the large amount of included studies and their comparable results. It can be considered a limitation that all different brands of prostheses and the different types (e.g. posterior stabilised/cruciate retaining) in MB-TKA and FB-TKA groups were combined. Because of this heterogeneity, it is possible that better outcome of individual prostheses is not fully addressed. This is inherent to the design of this literature overview and to (systematic) literature studies in general. Based on the consensus amongst LoE 1 studies, it is not to be expected that further differentiation into different types of prostheses would change the conclusions of this literature overview. The number of studies published on MB-TKA and FB-TKA is large and still increasing. However, the recent increase in evidence does not seem to provide new insights. It can, therefore, be argued that the discussion concerning the differences between MB-TKA and FB-TKA is not furthered by additional studies on this subject.
Conclusion
An extensive literature review was performed on studies examining differences between MB-TKA and FB-TKA, including a large number of studies with a lower LoE that are generally overlooked in other reviews. No clear differences were found between MB-TKA and FB-TKA in insert wear, signs of loosening of the prosthesis, survival rate and clinical outcome. Because of this, surgeons deciding between MB-TKA and FB-TKA for use in their day-to-day practice should be guided by different arguments, like surgeon experience with a certain type of prosthesis and financial or logistic advantages of different prostheses.
References
Aggarwal AK, Agrawal A (2013) Mobile versus fixed-bearing total knee arthroplasty performed by a single surgeon: a 4- to 6.5-year randomized, prospective, controlled, double-blinded study. J Arthroplasty 28:1712–1716
Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L (2005) Comparison of mobile-bearing and fixed-bearing total knee arthroplasty: a prospective randomized study. J Arthroplasty 20:145–153
Apostolopoulos AP, Michos IV, Mavrogenis AF, Chronopoulos E, Papachristou G, Lallos SN, Efstathopoulos NE (2011) Fixed versus mobile bearing knee arthroplasty: a review of kinematics and results. J Long Term Eff Med Implants 21:197–203
Argenson JN, Boisgard S, Parratte S, Descamps S, Bercovy M, Bonnevialle P, Briard JL, Brilhault J, Chouteau J, Nizard R, Saragaglia D, Servien E, French Society of O, Traumatologic S (2013) Survival analysis of total knee arthroplasty at a minimum 10 years’ follow-up: a multicenter French nationwide study including 846 cases. Orthop Traumatol Surg Res 99:385–390
Bailey O, Ferguson K, Crawfurd E, James P, May PA, Brown S, Blyth M, Leach WJ (2015) No clinical difference between fixed- and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23:1653–1659
Ball ST, Sanchez HB, Mahoney OM, Schmalzried TP (2011) Fixed versus rotating platform total knee arthroplasty: a prospective, randomized, single-blind study. J Arthroplasty 26:531–536
Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA (2003) Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res 410:131–138
Banks SA, Hodge WA (2004) 2003 Hap Paul Award Paper of the International Society for Technology in Arthroplasty. Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplasty 19:809–816
Banks SA, Hodge WA (2004) Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res 426:187–193
Beard DJ, Pandit H, Price AJ, Butler-Manuel PA, Dodd CAF, Murray DW, Goodfellow JW (2007) Introduction of a new mobile-bearing total knee prosthesis: minimum three year follow-up of an RCT comparing it with a fixed-bearing device. Knee 14:448–451
Berry DJ, Currier JH, Mayor MB, Collier JP (2012) Knee wear measured in retrievals: a polished tray reduces insert wear. Clin Orthop Relat Res 470:1860–1868
Bhan S, Malhotra R, Kiran EK, Shukla S, Bijjawara M (2005) A comparison of fixed-bearing and mobile-bearing total knee arthroplasty at a minimum follow-up of 4.5 years. J Bone Joint Surg Am 87:2290–2296
Bhandari M, Swiontkowski MF, Einhorn TA, Tornetta P, Schemitsch EH, Leece P, Sprague S, Wright JG (2004) Interobserver agreement in the application of levels of evidence to scientific papers in the American volume of the Journal of Bone and Joint Surgery. J Bone Joint Surg Am 86-A:1717–1720
Biau D, Mullins MM, Judet T, Piriou P (2006) Mobile versus fixed-bearing total knee arthroplasty: mid-term comparative clinical results of 216 prostheses. Knee Surg Sports Traumatol Arthrosc 14:927–933
Bistolfi A, Lee GC, Deledda D, Rosso F, Berchialla P, Crova M, Massazza G (2014) NexGen((R)) LPS mobile bearing total knee arthroplasty: 10-year results. Knee Surg Sports Traumatol Arthrosc 22:1786–1792
Bo ZD, Liao L, Zhao JM, Wei QJ, Ding XF, Yang B (2014) Mobile bearing or fixed bearing? A meta-analysis of outcomes comparing mobile bearing and fixed bearing bilateral total knee replacements. Knee 21:374–381
Breeman S, Campbell MK, Dakin H, Fiddian N, Fitzpatrick R, Grant A, Gray A, Johnston L, MacLennan GS, Morris RW, Murray DW (2013) Five-year results of a randomised controlled trial comparing mobile and fixed bearings in total knee replacement. Bone Joint J 95-B:486–492
Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, van Dijk CN (2008) Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res 466:1959–1965
Breugem SJ, van Ooij B, Haverkamp D, Sierevelt IN, van Dijk CN (2014) No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc 22:509–516
Buechel FF (2004) Mobile-bearing knee arthroplasty: rotation is our salvation! J Arthroplasty 19:27–30
Buechel FF, Pappas MJ (1986) The New Jersey low-contact-stress knee replacement system: biomechanical rationale and review of the first 123 cemented cases. Arch Orthop Trauma Surg 105:197–204
Catani F, Benedetti MG, De Felice R, Buzzi R, Giannini S, Aglietti P (2003) Mobile and fixed bearing total knee prosthesis functional comparison during stair climbing. Clin Biomech (Bristol, Avon) 18:410–418
Chen LB, Tan Y, Al Aidaros M, Wang H, Wang X, Cai SH (2013) Comparison of functional performance after total knee arthroplasty using rotating platform and fixed-bearing prostheses with or without patellar resurfacing. Orthop Surg 5:112–117
Cheng M, Chen D, Guo Y, Zhu C, Zhang X (2013) Comparison of fixed- and mobile-bearing total knee arthroplasty with a mean five-year follow-up: a meta-analysis. Exp Ther Med 6:45–51
Chiu K, Ng T, Tang W, Lam P (2001) Bilateral total knee arthroplasty: one mobile-bearing and one fixed-bearing. J Orthop Surg (HongKong) 9:45–50
Delport HP (2013) The advantage of a total knee arthroplasty with rotating platform is only theoretical: prospective analysis of 1,152 arthroplasties. Open Orthop J 7:635–640
Delport HP, Banks SA, De Schepper J, Bellemans J (2006) A kinematic comparison of fixed-and mobile-bearing knee replacements. J Bone Joint Surg Br 88:1016–1021
Delport HP, Sloten JV, Bellemans J (2010) Comparative gravimetric wear analysis in mobile versus fixed-bearing posterior stabilized total knee prostheses. Acta Orthop Belg 76:367–373
Dennis DA, Komistek RD (2005) Kinematics of mobile-bearing total knee arthroplasty. Instr Course Lect 54:207–220
Dennis DA, Komistek RD (2006) Mobile-bearing total knee arthroplasty: design factors in minimizing wear. Clin Orthop Relat Res 452:70–77
Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res 416:37–57
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Engh CA Jr, Zimmerman RL, Hopper RH Jr, Engh GA (2013) Can microcomputed tomography measure retrieved polyethylene wear? Comparing fixed-bearing and rotating-platform knees. Clin Orthop Relat Res 471:86–93
Evans MC, Parsons EM, Scott RD, Thornhill TS, Zurakowski D (2006) Comparative flexion after rotating-platform versus fixed-bearing total knee arthroplasty. J Arthroplasty 21:985–991
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Ferguson KB, Bailey O, Anthony I, James PJ, Stother IG, Blyth MJ (2014) A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design–outcomes at 2 year follow-up. Knee 21:151–155
Geiger F, Mau H, Kruger M, Thomsen M (2008) Comparison of a new mobile-bearing total knee prosthesis with a fixed-bearing prosthesis: a matched pair analysis. Arch Orthop Trauma Surg 128:285–291
Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, Hallan G, Furnes O (2013) Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J 95-B:636–642
Grupp TM, Kaddick C, Schwiesau J, Maas A, Stulberg SD (2009) Fixed and mobile bearing total knee arthroplasty—influence on wear generation, corresponding wear areas, knee kinematics and particle composition. Clin Biomech (Bristol, Avon) 24:210–217
Gupta RR, Bloom KJ, Caravella JW, Shishani YF, Klika AK, Barsoum WK (2014) Role of primary bearing type in revision total knee arthroplasty. J Knee Surg 27:59–66
Haider H, Garvin K (2008) Rotating platform versus fixed-bearing total knees: an in vitro study of wear. Clin Orthop Relat Res 466:2677–2685
Hansson U, Toksvig-Larsen S, Jorn LP, Ryd L (2005) Mobile versus fixed meniscal bearing in total knee replacement: a randomised radiostereometric study. Knee 12:414–418
Hanusch B, Lou TN, Warriner G, Hui A, Gregg P (2010) Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomised controlled trial. Int Orthop 34:349–354
Harrington MA, Hopkinson WJ, Hsu P, Manion L (2009) Fixed- versus mobile-bearing total knee arthroplasty: Does it make a difference?–a prospective randomized study. J Arthroplasty 24:24–27
Hasegawa M, Sudo A, Uchida A (2009) Staged bilateral mobile-bearing and fixed-bearing total knee arthroplasty in the same patients: a prospective comparison of a posterior-stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc 17:237–243
Henricson A, Dalen T, Nilsson KG (2006) Mobile bearings do not improve fixation in cemented total knee arthroplasty. Clin Orthop Relat Res 448:114–121
Higuchi H, Hatayama K, Shimizu M, Kobayashi A, Kobayashi T, Takagishi K (2009) Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. Int Orthop 33:997–1000
Ho FY, Ma HM, Liau JJ, Yeh CR, Huang CH (2007) Mobile-bearing knees reduce rotational asymmetric wear. Clin Orthop Relat Res 462:143–149
Hofstede SN, Nouta KA, Jacobs W, van Hooff ML, Wymenga AB, Pijls BG, Nelissen RG, Marang-van de Mheen PJ (2015) Mobile bearing versus fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev 2:CD003130
Huang CH, Liau JJ, Cheng CK (2007) Fixed or mobile-bearing total knee arthroplasty. J Orthop Surg Res 2:1–8
Huang CH, Liau JJ, Lu YC, Chang TK, Cheng CK (2009) Specific complications of the mobile-bearing total knee prosthesis. J Long Term Eff Med Implants 19:1–11
Huang CH, Liau JJ, Lung CY, Lan CT, Cheng CK (2002) The incidence of revision of the metal component of total knee arthroplasties in different tibial-insert designs. Knee 9:331–334
Huang CH, Ma HM, Liau JJ, Ho FY, Cheng CK (2002) Osteolysis in failed total knee arthroplasty: a comparison of mobile-bearing and fixed-bearing knees. J Bone Joint Surg Am 84-A:2224–2229
Huang ZM, Ouyang GL, Xiao LB (2011) Rotating-platform knee arthroplasty: a review and update. Orthop Surg 3:224–228
Jacobs W, Anderson P, Limbeek J, Wymenga A (2004) Mobile bearing versus fixed bearing prostheses for total knee arthroplasty for post-operative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev 2:CD003130
Jacobs WC, Christen B, Wymenga AB, Schuster A, van der Schaaf DB, Ten Ham A, Wehrli U (2011) Functional performance of mobile versus fixed bearing total knee prostheses: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 20:1450–1455
Jawed A, Kumar V, Malhotra R, Yadav CS, Bhan S (2012) A comparative analysis between fixed bearing total knee arthroplasty (PFC Sigma) and rotating platform total knee arthroplasty (PFC-RP) with minimum 3-year follow-up. Arch Orthop Trauma Surg 132:875–881
Jolles BM, Grzesiak A, Eudier A, Dejnabadi H, Voracek C, Pichonnaz C, Aminian K, Martin E (2012) A randomised controlled clinical trial and gait analysis of fixed- and mobile-bearing total knee replacements with a five-year follow-up. J Bone Joint Surg Br 94:648–655
Kalisvaart MM, Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD (2012) Randomized clinical trial of rotating-platform and fixed-bearing total knee arthroplasty: no clinically detectable differences at 5 years. J Bone Joint Surg Am 94:481–489
Kim D, Seong SC, Lee M, Lee S (2012) Comparison of the tibiofemoral rotational alignment after mobile and fixed bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:337–345
Kim TK, Chang CB, Kang YG, Chung BJ, Cho HJ, Seong SC (2010) Early clinical outcomes of floating platform mobile-bearing TKA: longitudinal comparison with fixed-bearing TKA. Knee Surg Sports Traumatol Arthrosc 18:879–888
Kim TW, Park SH, Suh JT (2012) Comparison of mobile-bearing and fixed-bearing designs in high flexion total knee arthroplasty: using a navigation system. Knee Surg Relat Res 24:25–33
Kim YH, Choi Y, Kim JS (2010) Osteolysis in well-functioning fixed- and mobile-bearing TKAs in younger patients. Clin Orthop Relat Res 468:3084–3093
Kim YH, Kim DY, Kim JS (2007) Simultaneous mobile- and fixed-bearing total knee replacement in the same patients. A prospective comparison of mid-term outcomes using a similar design of prosthesis. J Bone Joint Surg Br 89:904–910
Kim YH, Kim JS (2009) Prevalence of osteolysis after simultaneous bilateral fixed- and mobile-bearing total knee arthroplasties in young patients. J Arthroplasty 24:932–940
Kim YH, Kim JS, Choe JW, Kim HJ (2012) Long-term comparison of fixed-bearing and mobile-bearing total knee replacements in patients younger than 51 years of age with osteoarthritis. J Bone Joint Surg Am 94:866–873
Kim YH, Kook HK, Kim JS (2001) Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res 392:101–115
Kim YH, Yoon SH, Kim JS (2007) The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg Br 89:1317–1323
Kim YH, Yoon SH, Kim JS (2009) Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 467:493–503
Kotani A, Yonekura A, Bourne RB (2005) Factors influencing range of motion after contemporary total knee arthroplasty. J Arthroplasty 20:850–856
Ladermann A, Lubbeke A, Stern R, Riand N, Fritschy D (2008) Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomised, clinical and radiological study with mid-term results at 7 years. Knee 15:206–210
Lampe F, Sufi-Siavach A, Bohlen KE, Hille E, Dries SP (2011) One year after navigated total knee replacement, no clinically relevant difference found between fixed bearing and mobile bearing knee replacement in a double-blind randomized controlled trial. Open Orthop J 5:201–208
Li YL, Wu Q, Ning GZ, Feng SQ, Wu QL, Li Y, Hao Y (2014) No difference in clinical outcome between fixed- and mobile-bearing TKA: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22:565–575
Liu F, Ohdera T, Miyamoto H, Wasielewski RC, Komistek RD, Mahfouz MR (2009) In vivo kinematic determination of total knee arthroplasty from squatting to standing. Knee 16:116–120
Lizaur-Utrilla A, Sanz-Reig J, Trigueros-Rentero MA (2012) Greater satisfaction in older patients with a mobile-bearing compared with fixed-bearing total knee arthroplasty. J Arthroplasty 27:207–212
Lu YC, Huang CH, Chang TK, Ho FY, Cheng CK (2010) Wear-pattern analysis in retrieved tibial inserts of mobile-bearing and fixed-bearing total knee prostheses. J Bone Joint Surg Br 92:500–507
Luring C, Bathis H, Oczipka F, Trepte C, Lufen H, Perlick L, Grifka J (2006) Two-year follow-up on joint stability and muscular function comparing rotating versus fixed bearing TKR. Knee Surg Sports Traumatol Arthrosc 14:605–611
Lygre SHL, Espehaug B, Havelin LI, Vollset SE, Furnes O (2011) Failure of total knee arthroplasty with or without patella resurfacing. Acta Orthop 82:282–292
Mahoney OM, Kinsey TL, D’Errico TJ, Shen J (2012) The John Insall Award: no functional advantage of a mobile bearing posterior stabilized TKA. Clin Orthop Relat Res 470:33–44
Marques CJ, Daniel S, Sufi-Siavach A, Lampe F (2014) No differences in clinical outcomes between fixed- and mobile-bearing computer-assisted total knee arthroplasties and no correlations between navigation data and clinical scores. Knee Surg Sports Traumatol Arthrosc 23:1660–1668
Matsuda S, Mizu-uchi H, Fukagawa S, Miura H, Okazaki K, Matsuda H, Iwamoto Y (2010) Mobile-bearing prosthesis did not improve mid-term clinical results of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 18:1311–1316
McEwen HM, Barnett PI, Bell CJ, Farrar R, Auger DD, Stone MH, Fisher J (2005) The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J Biomech 38:357–365
McGonagle L, Bethell L, Byrne N, Bolton-Maggs BG (2014) The Rotaglide + total knee replacement: a comparison of mobile versus fixed bearings. Knee Surg Sports Traumatol Arthrosc 22:1626–1631
Minoda Y, Ikebuchi M, Kobayashi A, Iwaki H, Inori F, Nakamura H (2010) A cemented mobile-bearing total knee replacement prevents periprosthetic loss of bone mineral density around the femoral component: a matched cohort study. J Bone Joint Surg Br 92:794–798
Minoda Y, Iwaki H, Ikebuchi M, Yoshida T, Mizokawa S, Itokazu M, Nakamura H (2015) Mobile-bearing prosthesis and intraoperative gap balancing are not predictors of superior knee flexion: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23:1986–1992
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Moskal JT, Capps SG (2014) Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res 472:2185–2193
Mueller-Rath R, Kleffner B, Andereya S, Mumme T, Wirtz DC (2007) Measures for reducing ultra-high-molecular-weight polyethylene wear in total knee replacement: a simulator study. Biomed Tech (Berl) 52:295–300
Munro JT, Pandit S, Walker CG, Clatworthy M, Pitto RP (2010) Loss of tibial bone density in patients with rotating- or fixed-platform TKA. Clin Orthop Relat Res 468:775–781
Namba RS, Inacio MC, Paxton EW, Ake CF, Wang C, Gross TP, Marinac-Dabic D, Sedrakyan A (2012) Risk of revision for fixed versus mobile-bearing primary total knee replacements. J Bone Joint Surg Am 94:1929–1935
Namba RS, Inacio MC, Paxton EW, Robertsson O, Graves SE (2011) The role of registry data in the evaluation of mobile-bearing total knee arthroplasty. J Bone Joint Surg Am 93:48–50
Nieuwenhuijse MJ, van der Voort P, Kaptein BL, Valstar ER, Nelissen RG (2013) Fixation of high-flexion total knee prostheses: five-year follow-up results of a four-arm randomized controlled clinical and roentgen stereophotogrammetric analysis study. J Bone Joint Surg Am 95:e1411
Nutton RW, Wade FA, Coutts FJ, van der Linden ML (2012) Does a mobile-bearing, high-flexion design increase knee flexion after total knee replacement? J Bone Joint Surg Br 94:1051–1057
Obremskey WT, Pappas N, Attallah-Wasif E, Tornetta P, Bhandari M (2005) Level of evidence in orthopaedic journals. J Bone Joint Surg Am 87:2632–2638
Oh KJ, Pandher DS, Lee SH, Sung Joon SD Jr, Lee ST (2009) Meta-analysis comparing outcomes of fixed-bearing and mobile-bearing prostheses in total knee arthroplasty. J Arthroplasty 24:873–884
Okamoto N, Nakamura E, Nishioka H, Karasugi T, Okada T, Mizuta H (2014) In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplasty 29:2393–2396
Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ (2004) Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res 428:221–227
Pijls BG, Valstar ER, Kaptein BL, Nelissen RG (2012) Differences in long-term fixation between mobile-bearing and fixed-bearing knee prostheses at ten to 12 years’ follow-up: a single-blinded randomised controlled radiostereometric trial. J Bone Joint Surg Br 94:1366–1371
Poolman RW, Struijs PA, Krips R, Sierevelt IN, Lutz KH, Bhandari M (2006) Does a “Level I Evidence” rating imply high quality of reporting in orthopaedic randomised controlled trials? BMC Med Res Methodol 6:44
Post ZD, Matar WY, van de Leur T, Grossman EL, Austin MS (2010) Mobile-bearing total knee arthroplasty: better than a fixed-bearing? J Arthroplasty 25:998–1003
Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, de Steiger R, Dodd CAF, Gibbons M, McLardy-Smith P, Goodfellow JW, Murray DW (2003) A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br 85:62–67
Radetzki F, Wienke A, Mendel T, Gutteck N, Delank KS, Wohlrab D (2013) High flex total knee arthroplasty–a prospective, randomized study with results after 10 years. Acta Orthop Belg 79:536–540
Rahman WA, Garbuz DS, Masri BA (2010) Randomized controlled trial of radiographic and patient-assessed outcomes following fixed versus rotating platform total knee arthroplasty. J Arthroplasty 25:1201–1208
Ranawat AS, Rossi R, Loreti I, Rasquinha VJ, Rodriguez JA, Ranawat CS (2004) Comparison of the PFC Sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: short-term results. J Arthroplasty 19:35–39
Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M (2004) In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res 418:184–190
Rees JL, Beard DJ, Price AJ, Gill HS, McLardy-Smith P, Dodd CAF, Murray DW (2005) Real in vivo kinematic differences between mobile-bearing and fixed-bearing total knee arthroplasties. Clin Orthop Relat Res 432:204–209
Saari T, Uvehammer J, Carlsson LV, Herberts P, Regner L, Karrholm J (2003) Kinematics of three variations of the Freeman-Samuelson total knee prosthesis. Clin Orthop Relat Res 410:235–247
Sackett DL (1986) Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 89:2S–3S
Sawaguchi N, Majima T, Ishigaki T, Mori N, Terashima T, Minami A (2010) Mobile-bearing total knee arthroplasty improves patellar tracking and patellofemoral contact stress: in vivo measurements in the same patients. J Arthroplasty 25:920–925
Schuster AJ, von Roll AL, Pfluger D, Wyss T (2011) Anteroposterior stability after posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1113–1120
Scuderi GR, Hedden DR, Maltry JA, Traina SM, Sheinkop MB, Hartzband MA (2012) Early clinical results of a high-flexion, posterior-stabilized, mobile-bearing total knee arthroplasty a US investigational device exemption trial. J Arthroplasty 27:421–429
Shemshaki H, Dehghani M, Eshaghi MA, Esfahani MF (2012) Fixed versus mobile weight-bearing prosthesis in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:2519–2527
Shi K, Hayashida K, Umeda N, Yamamoto K, Kawai H (2008) Kinematic comparison between mobile-bearing and fixed-bearing inserts in NexGen legacy posterior stabilized flex total knee arthroplasty. J Arthroplasty 23:164–169
Shi X, Shen B, Yang J, Kang P, Zhou Z, Pei F (2014) In vivo kinematics comparison of fixed-and mobile-bearing total knee arthroplasty during deep knee bending motion. Knee Surg Sports Traumatol Arthrosc 22:1612–1618
Siebold R, Louisia S, Canty J, Bartlett RJ (2007) Posterior stability in fixed-bearing versus mobile-bearing total knee replacement: a radiological comparison of two implants. Arch Orthop Trauma Surg 127:97–104
Silvestre Munoz A, Almeida Herrero F, Lopez Lozano R, Arguelles Linares F (2008) Comparison of mobile- and fixed-bearing cemented total knee arthroplasty. Acta Orthop Belg 74:801–808
Slobogean G, Bhandari M (2012) Introducing levels of evidence to the journal of orthopaedic trauma: implementation and future directions. J Orthop Trauma 26:127–128
Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R (2011) Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty 26:1205–1213
Smith TO, Ejtehadi F, Nichols R, Davies L, Donell ST, Hing CB (2010) Clinical and radiological outcomes of fixed- versus mobile-bearing total knee replacement: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 18:325–340
Stoner K, Jerabek SA, Tow S, Wright TM, Padgett DE (2013) Rotating-platform has no surface damage advantage over fixed-bearing TKA. Clin Orthop Relat Res 471:76–85
Tibesku CO, Daniilidis K, Skwara A, Dierkes T, Rosenbaum D, Fuchs-Winkelmann S (2011) Gait analysis and electromyography in fixed- and mobile-bearing total knee replacement: a prospective, comparative study. Knee Surg Sports Traumatol Arthrosc 19:2052–2059
Tibesku CO, Daniilidis K, Vieth V, Skwara A, Heindel W, Fuchs-Winkelmann S (2011) Sagittal plane kinematics of fixed- and mobile-bearing total knee replacements. Knee Surg Sports Traumatol Arthrosc 19:1488–1495
Tienboon P, Jaruwangsanti N, Laohasinnurak P (2012) A prospective study comparing mobile-bearing versus fixed-bearing type in total knee arthroplasty using the free-hand-cutting technique. J Med Assoc Thai 95:S77–S86
Tjørnild M, Søballe K, Hansen PM, Holm C, Stilling M (2015) Mobile- versus fixed-bearing total knee replacement. Acta Orthop 86:208–214
Urwin SG, Kader DF, Caplan N, St Clair Gibson A, Stewart S (2014) Gait analysis of fixed bearing and mobile bearing total knee prostheses during walking: Do mobile bearings offer functional advantages? Knee 21:391–395
Van der Bracht H, Van Maele G, Verdonk P, Almqvist KF, Verdonk R, Freeman M (2010) Is there any superiority in the clinical outcome of mobile-bearing knee prosthesis designs compared to fixed-bearing total knee prosthesis designs in the treatment of osteoarthritis of the knee joint? A review of the literature. Knee Surg Sports Traumatol Arthrosc 18:367–374
van der Voort P, Pijls BG, Nouta KA, Valstar ER, Jacobs WC, Nelissen RG (2013) A systematic review and meta-regression of mobile-bearing versus fixed-bearing total knee replacement in 41 studies. Bone Joint J 95-B:1209–1216
van Stralen RA, Heesterbeek PJ, Wymenga AB (2015) Different femorotibial contact points between fixed- and mobile-bearing TKAs do not show clinical impact. Knee Surg Sports Traumatol Arthrosc 23:3368–3374
Vasdev A, Kumar S, Chadha G, Mandal SP (2009) Fixed- versus mobile-bearing total knee arthroplasty in Indian patients. J Orthop Surg (HongKong) 17:179–182
Vertullo CJ, Easley ME, Scott WN, Insall JN (2001) Mobile bearings in primary knee arthroplasty. J Am Acad Orthop Surg 9:355–364
Watanabe T, Ishizuki M, Muneta T, Banks SA (2012) Matched comparison of kinematics in knees with mild and severe varus deformity using fixed- and mobile-bearing total knee arthroplasty. Clin Biomech (Bristol, Avon) 27:924–928
Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H (2005) Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop 29:179–181
Wen Y, Liu D, Huang Y, Li B (2011) A meta-analysis of the fixed-bearing and mobile-bearing prostheses in total knee arthroplasty. Arch Orthop Trauma Surg 131:1341–1350
Wohlrab D, Hube R, Zeh A, Hein W (2009) Clinical and radiological results of high flex total knee arthroplasty: a 5 year follow-up. Arch Orthop Trauma Surg 129:21–24
Wolterbeek N, Garling EH, Mertens BJ, Nelissen RG, Valstar ER (2012) Kinematics and early migration in single-radius mobile- and fixed-bearing total knee prostheses. Clin Biomech (Bristol, Avon) 27:398–402
Wolterbeek N, Nelissen RGHH, Valstar ER (2012) No differences in in vivo kinematics between six different types of knee prostheses. Knee Surg Sports Traumatol Arthrosc 20:559–564
Wonglertsiri S, Uthaicharatratsame C (2013) Comparison of fixed bearing and mobile bearing total knee arthroplasty using identical femoral component. J Med Assoc Thail 96:203–208
Woolson ST, Epstein NJ, Huddleston JI (2011) Long-term comparison of mobile-bearing versus fixed-bearing total knee arthroplasty. J Arthroplasty 26:1219–1223
Woolson ST, Northrop GD (2004) Mobile- versus fixed-bearing total knee arthroplasty: a clinical and radiologic study. J Arthroplasty 19:135–140
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A:1–3
Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E (2008) Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 90:1172–1179
Zeng Y, Shen B, Yang J, Zhou ZK, Kang PD, Pei FX (2013) Is there reduced polyethylene wear and longer survival when using a mobile-bearing design in total knee replacement? A meta-analysis of randomised and non-randomised controlled trials. Bone Joint J 95-B:1057–1063
Zurcher AW, van Hutten K, Harlaar J, Terwee CB, Rob Albers GH, Poll RG (2014) Mobile-bearing total knee arthroplasty: more rotation is evident during more demanding tasks. Knee 21:960–963
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fransen, B.L., van Duijvenbode, D.C., Hoozemans, M.J.M. et al. No differences between fixed- and mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 1757–1777 (2017). https://doi.org/10.1007/s00167-016-4195-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4195-x