Abstract
Purpose
This study was designed to compare clinical, radiological, and general health results of two prostheses (mobile vs. fixed weight-bearing devices) that are used in total knee arthroplasty with a 5-year follow-up.
Methods
This randomized controlled study was conducted from 2004 to 2010 in the Department of Orthopedic Surgery at two university hospitals in Isfahan, Iran. Three hundred patients with expected primary total knee arthroplasty (TKA) without severe deformity (a fixed varus or valgus deformity greater than 20°) received fixed weight-bearing (n = 150) or mobile weight-bearing (n = 150) devices. Clinical, radiological, and quality of life outcomes were compared between the two groups at six-month intervals for the first year, after which the comparisons were made annually for the next 4 years.
Results
Both groups had similar baseline characteristics. Although there was significant improvement in both groups, there was no significant difference between the groups with regard to the means of the Knee Society Scores, which were 92 (SD: 12.1) for the fixed weight-bearing device and 93 (SD: 14.2) for the mobile weight-bearing device (n.s.) at the final follow-up point. Radiographs showed that there was no significant difference in prosthetic alignment and no evidence of loosening. After TKA, the SF-36 score increased in both groups, but there was no statistical difference between the groups in quality of life at the final follow-up (62 (12.2) vs. 64 (14.3), n.s.). There was no revision after 5 years.
Conclusions
In terms of clinical, radiological or general health outcomes for people who underwent TKA, the results of this study showed no clear advantage of mobile weight-bearing over the fixed weight-bearing prosthesis at the five-year follow-up.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has become widely approved for treatment of severe knee functional limitations, such as end-stage osteoarthritis or rheumatoid arthritis [1]. Currently, there are two different designs of the prosthesis devices, that is, fixed weight-bearing and mobile weight-bearing devices, and each design has advantages and disadvantages. Fixed weight-bearing devices, in which the polyethylene tibial insert is locked with the tibial tray, have yielded excellent survival rates of up to 95 % at the 10-year follow-up [16], but problems related to patellofemoral articulation, polyethylene wear, and osteolysis have been reported [4, 8, 10]. The mobile weight-bearing devices, which facilitate movement of the insert relative to the tray [28], reduce contact stress and linear wear of the polyethylene [5, 31], allow reproduction of tibial internal rotation during flexion [6, 9], and improve patellofemoral tracking, which decrease the problems of stability and anterior knee pain [4]. However, the mobile weight-bearing devices have the disadvantages of greater implant costs and potential mechanical failure due to bearing dislocation [13, 35], which may limit their use. Despite the potential advantages that exist for mobile versus fixed weight-bearing devices, some comparative studies have indicated no superiority for the mobile weight-bearing devices over the fixed weight-bearing devices [18, 33].
In a study of 92 bilateral TKAs, Kim et al. [23] showed significantly better Knee Society Scores (KSS) for mobile weight-bearing devices compared to fixed weight-bearing devices. Also, a study by Price et al. [32] of 39 patients who had bilateral TKAs indicated that the mobile weight-bearing devices had higher KSS than the fixed weight-bearing devices. In contrast, available reports showed no significant clinical improvement in the mobile implants compared to the fixed implants [18, 33]. Also, among previous studies, only Lampe et al. [25] succeeded in eliminating the variability in the design of the implant, the surgical technique, and post-operative rehabilitation in short-term follow-up. However, it has not been determined whether these variables have any significant impact on the outcomes in long-term follow-up. As a result of these controversial results, there is a need to better understand the mobile weight-bearing implant and also a need to determine the impact of the variables on follow-up outcomes. Thus, this study was designed to compare clinical, radiological, and general health results of the two types of prostheses at the five-year follow-up assessment. The study hypothesis was that there would be better clinical results with the mobile weight-bearing implant than for the fixed weight-bearing implant at the mid-term follow-up.
Materials and methods
This prospective randomized trial was conducted from June 2004 to November 2010 in the Department of Orthopedic Surgery at two university hospitals (Referral Centers, Isfahan University of Medical Sciences) in Isfahan, Iran. Patients with expected primary total knee arthroplasty without severe deformity (a fixed varus or valgus deformity greater than 20°) participated in the study. Exclusion criteria were mediolateral instability, infective arthritis, severe deformity, and revision. The study was approved by the Ethics Committee of Isfahan University of Medical Sciences, and each patient gave informed consent prior to the study, which was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000. The study was registered at http://www.clinicaltrials.gov (Identifier: NCT01312532).
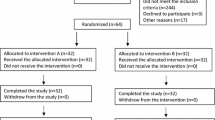
Of the 322 patients initially enrolled in the study, 22 were not included in the final analysis. Of the 15 patients who did not meet the inclusion criteria, five patients had mediolateral instability, eight patients had severe deformity, and two patients had infective arthritis. Seven patients were unable to get the anaesthesiologist’s permission for the operation. Of the remaining 300 patients in the final sample, 150 received fixed weight-bearing implants and 150 received mobile weight-bearing implants for total knee arthroplasty.
Based on a table of random numbers generated by random allocation software in regard to simple random allocation [34], the principal investigator (HSh) assigned patients to either the fixed weight-bearing group or the mobile weight-bearing group, and the surgeries were conducted by the same orthopaedic surgeon. The fixed weight-bearing prosthesis (P.F.C.® Sigma, DePuy, Johnson & Johnson, Leeds, UK) and the mobile weight-bearing prosthesis (P.F.C.® Sigma RP, DePuy, Johnson & Johnson, Leeds, UK) were used in this study. These are both posterior-stabilized prostheses, and they are identical with respect to the femoral component. The pre-operative, baseline characteristics of the two groups are shown in Table 1.
Eligible patients underwent regional (spinal or epidural) anaesthesia, and the surgical procedures were performed with tourniquet control via a midline skin incision and a medial parapatellar approach to the knee. Intramedullary and extramedullary alignment was done for the femur and tibia. Realignment of the knee was performed in the two groups by appropriate soft-tissue procedures. In order to remove a volume of bone equal to the volume of the component to be implanted, all patellae were resurfaced, and patellar thickness was measured before the resection. All devices were cemented after inflation of the tourniquet, pulsatile lavage of the bone, drying, and pressurization of the cement. Prophylactic intravenous antibiotic (cefazolin, 2 g) was administered to all patients 30 min before making the incision, and an additional quantity of 1 g was administered every 8 h for 3 days. Anti-thrombotic prophylaxis (subcutaneous enoxaparin or deltiparin) was begun 6 h post-operatively and continued until day five after surgery. The standard TKA rehabilitation protocol, including self-controlled epidural analgesia, non-steroidal oral analgesia, anti-thrombotics, physical therapy, and continuous passive motion, was the same for both groups. Continuous passive motion began on the first post-operative day, and full weight-bearing ambulation began on the second day, assisted by crutches for the first 6 weeks and a cane for an additional 6 weeks. Patients were discharged either to their own home or to a temporary rehabilitation facility when they were able to actively flex the knee to at least 90° and walk independently. Clinical and radiographic follow-up was performed at one, three, and 6 months; 1 year after the operation; and yearly thereafter until year five. The radiographs were taken during weight-bearing in all the patients, and they were taken at 3 months, 1 year, and then every 2 years. There was no difference between the two groups in additional soft-tissue procedures.
Knee Society Scoring (KSS) as a primary outcome was obtained pre-operatively and during the follow-up until year five. KSS was used for evaluating the function of the knee, with the higher scores indicating better knee function [17]. Our secondary outcomes included pain, patellofemoral joint function, quality of life, and radiological outcomes (alignment angles in the knee, positions of the femoral and tibial components, the position of the patella, and radiolucency).
Pain was evaluated with a visual analogue scale (VAS) with scores ranging from zero to 10 (0 for no pain and 10 for intolerable pain). Patellofemoral joint function was evaluated by a scoring system developed by Kim et al. [20], which considers pain in the anterior knee, the strength of the quadriceps, the ability to rise from a chair, and the ability to walk upstairs, with a final score that ranged from a minimum of one to a maximum of 30 points. Radiological outcomes were assessed by the Knee Society’s roentgenographic evaluation system. Long-standing roentgenograms of the knee were obtained to determine overall limb alignment before and after surgery. The components’ interfaces for radiolucent lines were investigated by fluoroscopic positioning in the anteroposterior and lateral views. Skyline views of the patellofemoral joint were obtained at 45° of flexion, using the technique developed by Merchant et al. [29].
To determine quality of life, we used the Iranian version of the short-form health survey (SF-36) questionnaire [30] before and after the operation, since its validity and reliability has been established. The questionnaires showed that the internal consistency (to test reliability) among all eight SF-36 scales met the minimum reliability standard, with Cronbach’s alpha coefficients ranging from 0.7 to 0.9 except for the vitality scale, for which the alpha coefficient was 0.6. In their study, convergent validity (to test scaling assumptions) using each item’s correlation with its hypothesized scale showed satisfactory results, with all correlations above 0.4 and in the range of 0.5 to 0.9. The SF-36 questionnaire, a generic measure of health, was used to measure quality of life. It consists of 36 questions (items), each of which was assigned a score ranging from 0 to 100.
Statistical analysis
Considering α = 0.05, study power = 80 %, d = 5.8 points as the minimal expected difference between the two groups in KSS [18] with standard deviations (SDs) of 12.7 and 15.5 and a 30 % possibility of failure, a sample size of 122 patients was considered for each group. In an effort to minimize the chance of type 2 error, we decided to recruit 150 patients per group. Neither the examiner nor the patient knew the type of implant during the evaluation, and the data recorded for each follow-up evaluation were double blind.
SPSS software (Windows version 18.0) was used to analyse the data using the independent t test (if the data were normally distributed) and the chi-squared test for comparing means and categorical data, respectively, between the two groups. Values of P < 0.05 were considered to be statistically significant.
Results
The flow of participants is shown in the CONSORT diagram in Fig 1. The results of each parameter of the KSS system during follow-up are shown in Table 2. Pre-operatively, the means of KSS in the fixed weight-bearing and mobile weight-bearing groups were 40 (SD: 18.2) and 41 (SD: 16.1) (n.s.), respectively, and the means improved to 92 (SD: 12.1) and 93 (SD: 14.2), respectively, at the final follow-up, that is, 5 years after surgery, but there was no difference between the two groups in this regard (CI 95 % = −3.9 to 1.9, n.s.).
Post-operative results improved similarly in both groups. Pain gradually diminished over the follow-up period, and there were 120 (80 %) and 132 (88 %) pain-free patients, respectively, at the end of follow-up (n.s.). The means of the functional scores were not statistically different between the two groups before surgery (47 (SD: 22.1) vs. 45 (SD: 21.3), CI 95 % = −2.9 to 6.9, n.s.) and 5 years after surgery (85 (SD: 23.4) vs. 86 (SD: 24.6), CI 95 % = −6.4 to 4.4, n.s.) (Table 2).
The walking distance, level of support, and stairs are shown in Table 2. The results showed that the ability to walk improved similarly in the two groups. The mean of patellar score was not significantly different between the groups before follow-up (11 (SD: 4.4) vs. 12 (SD: 4.6), CI 95 % = −2.0 to 0.02, n.s.) and at the final follow-up (26 (SD: 5.0) vs. 27 (SD: 4.5), CI 95 % = −2.08 to 0.08, n.s.).
The total scores of the SF-36 questionnaires are shown in Table 2. The results showed that the SF-36 scores increased after TKA in both groups, but there was no statistical difference between the groups in quality of life at final follow-up (62 (SD: 12.2) vs. 64 (SD: 14.3), CI 95 % = −5.0 to 1.0, n.s.).
The radiological results are shown in Table 3. There were no statistical differences in overall alignment between the two groups pre-operatively or post-operatively. According to the chi-squared test, there were no statistical differences between the groups in the positions of the femoral and tibial components, the position of the patella, or radiolucency. There were no intra-operative complications in either group, and there were no revisions or osteolysis during follow-up.
With the multi-variate regression analysis, gender (n.s.), age (n.s.), and kind of prosthesis (n.s.) had no impact on total KSS score at the five-year follow-up.
Discussion
The most important finding of this study was the lack of improvement when mobile weight-bearing devices were used instead of fixed weight-bearing devices with regard to clinical, radiological, and general health outcomes. The variables of gender, age, and kind of prosthesis had no impact on the final outcomes at the 5-year follow-up. The Knee Society Score improved in the patients after TKA, but there was no statistical difference between the two groups. Our results are in agreement with previous studies [1, 2, 19, 21, 37]. In a prospective study, Matsuda et al. [27] compared the clinical and radiological results of mobile weight-bearing implants and fixed weight-bearing implants for 61 total knee arthroplasties and found no improvement for mobile weight-bearing implants, with specific attention to rotational alignment and range of motion in the mid-term follow-up. Our results agreed with their results, but we have called attention to some limitations in their study, such as inadequate randomization and only using KSS to evaluate patients’ symptoms.
In contrast, a study by Kim et al. [23] of 92 bilateral TKAs reported significantly better KSS for mobile weight-bearing implants. The difference may be that a different kind of prosthesis was used. In their study, the excessive constraint of the Medial Pivot fixed weight-bearing prosthesis imposed by the fully congruent medial tibiofemoral articulation may not restore normal kinematics of the knee and inhibit posterior rolling and sliding of the lateral femoral condyle around a medial femoral condyle during knee flexion. This subtle disturbance of kinematics of the Medial Pivot fixed weight-bearing prosthesis may contribute to less favourable clinical outcomes than the PFC Sigma mobile weight-bearing prosthesis. Price et al. [32] conducted a study of 39 patients requiring bilateral TKA and also reported higher KSS for mobile weight-bearing implants compared to fixed weight-bearing implants. The difference may be due to the fact that, in the study conducted by Price et al. [32], the blinding protocol was broken for nine of the 39 patients, and some of the clinical measurements were made by an examiner who could have known which implant was in which knee. Also, our results agree with the results of a meta-analysis conducted by Smith et al. [36]. They reported that statistical pooling of the data clearly indicates that no significant difference exists between clinical outcomes of mobile weight-bearing implants and fixed weight-bearing implants in TKA.
Our study showed that the pain levels were the same for the fixed weight-bearing group and the mobile weight-bearing group. This finding is in agreement with many previous studies [12, 15, 22, 38]. In contrast, there are three studies that found lower levels of pain with the mobile weight-bearing implants [3, 23, 32]. It should be noted that all three studies that showed a difference in pain levels at the final follow-up had a relatively short follow-up periods (1–2.6 years). Short-term results are not always indicative of mid-term and long-term outcomes, so the results of these studies should be interpreted with caution. Results at the end of follow-up showed that 88 % of the patients in the mobile weight-bearing group were pain free. This finding agreed with the results of a study conducted by Aglietti et al. in which it was reported that 84 % of patients were pain free in the mobile weight-bearing group [1].
Stair climbing was reported as the percentage of patients requiring aids to climb stairs versus those able to climb stairs normally [7]. Our results showed that post-operative stair-climbing ability was greatly improved when compared to the pre-operative results. However, no significant difference existed between the groups. Our findings agreed with previous studies [1, 3, 22].
In the present study, the safety of the fixed and mobile weight-bearing devices was demonstrated, and no complications were found in any of the cases at the 5-year follow-up. Our results were in agreements with the findings in the study performed by Hasegawa et al. [15], which indicated that there was no loosening of parts, revision, or infection in any patient. However, in some studies, complications requiring a revision in the mobile weight-bearing group, such as bearing dislocation, instability requiring revision, and early component loosening [12, 23, 24], were reported. The surgeon-specific factor could be a contributing factor in complications. In this study, one experienced knee surgeon (MDe) performed all of the TKAs. However, this property limited us to design a multi-centric study. A review study with adequate power to determine the risk of complications with mobile weight-bearing devices is warranted. In our study, we eliminated the variability in implant design, surgical technique, and post-operative rehabilitation. Until now, only Lampe et al. [25] had succeeded in eliminating these factors to such an extent. But they followed their patients only for a year, and our study confirmed their results in longer follow-up.
Also, quality of life was improved significantly post-operatively, but no statistical difference was found between the groups. This finding agrees with previous studies [14, 26].
In this study, radiological findings are in agreement with those from the study conducted by Aglietti et al., in which no difference in radiological outcomes was found between groups [1]. This study also supports the results obtained by Smith et al.’s meta-analysis study [36], which indicated that there is no statistically significant difference in radiological outcomes between fixed versus mobile weight-bearing knee prostheses. Garling et al. [11] also reported no significant difference in radiostereometric analysis component anterior–posterior tilting between fixed and mobile weight-bearing TKAs.
In the present study with the multi-variate regression analysis, the results showed the variables, including gender, age, and kind of prosthesis, had no impact on total KSS score at the five-year follow-up. To the best of our knowledge, this study is the only study that has determined this result in the mid-term follow-up.
This study has several strengths. The trial attempted to exclude “observer-dependent” bias in clinician-based outcome (KSS), with the examiner blinded to which implant was in which knee. A statistical power study was performed to obtain the required population for a meaningful statistical analysis. Surgical procedures were standardized, and they were all performed by the same surgeon. Post-operative recovery, rehabilitation protocol, and medical prophylaxes were the same for both groups. All patients were evaluated for each follow-up with all patients participating through the final follow-up. Also, we compared two similar prostheses from the same manufacturer.
One limitation of this study might be the 5-year follow-up. An even longer follow-up period may be necessary to ascertain the long-term outcomes of mobile weight-bearing devices [24].
The primary interest of the study was KSS, which is clinically relevant within the first year after the operation. However, long-term outcome is also important, especially because it is believed that contact stresses, and therefore loosening, could be improved by the mobile weight-bearing implant and may affect the quality of life and KSS. For that reason, the patients will be followed-up until 10 years after the operation.
Conclusions
Mid-term follow-up does not show any advantages for mobile versus fixed weight-bearing implants in clinical outcomes. The variables, including gender, age, and kind of prosthesis, had no impact on the total KSS score at the 5-year follow-up.
References
Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L (2005) Comparison of mobile-bearing and fixed-bearing total knee arthroplasty: a prospective randomized study. J Arthroplast 20(2):145–153
Bhan S, Malhotra R, Kiran EK, Shukla S, Bijjawara M (2005) A comparison of fixed-bearing and mobile-bearing total knee arthroplasty at a minimum follow-up of 4.5 years. J Bone Joint Surg Am 87(10):2290–2296
Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, van Dijk CN (2008) Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res 466:1959–1965
Buechel FF, Pappas MJ (1989) New Jersey low contact stress knee replacement system. Ten-year evaluation of meniscal bearings. Orthop Clin N Am 20(2):147–177
Buechel FFPM (1990) Long-term survivorship analysis of cruciate-sparing versus cruciate-sacrificing knee prostheses using meniscal bearings. Clin Orthop Relat Res 260:162–169
Callaghan JJ, Insall JN, Greenwald AS, Dennis DA, Komistek RD, Murray DW, Bourne RB, Rorabeck CH, Dorr LD (2001) Mobile-bearing knee replacement: concepts and results. Instr Course Lect 50:431–449
Catani F, Benedetti MG, De Felice R, Buzzi R, Giannini S, Aglietti P (2003) Mobile and fixed bearing total knee prosthesis functional comparison during stair climbing. Clin Biomech (Bristol, Avon) 18(5):410–418
Colizza WA, Insall JN, Scuderi GR (1995) The posterior stabilized total knee prosthesis. Assessment of polyethylene damage and osteolysis after a ten-year-minimum follow-up. J Bone Joint Surg Am 77(11):1713–1720
Delport HP, Banks SA, De Schepper J, Bellemans J (2006) A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br 88(8):1016–1021
Engh GA (1988) Failure of the polyethylene bearing surface of a total knee replacement within four years. A case report. J Bone Joint Surg Am 70:1093–1096
Garling EH, Valstar ER, Nelissen RG (2005) Comparison of micromotion in mobile bearing and posterior stabilized total knee prostheses: a randomized RSA study of 40 knees followed for 2 years. Acta Orthop 76(3):353–361
Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J (2009) Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs. A prospective randomized trial. J Bone Joint Surg Am 91(9):2104–2112
Grupp TM, Kaddick C, Schwiesau J, Maas A, Stulberg SD (2009) Fixed and mobile bearing total knee arthroplasty–influence on wear generation, corresponding wear areas, knee kinematics and particle composition. Clin Biomech (Bristol, Avon) 24(2):210–217
Harrington MA, Hopkinson WJ, Hsu P, Manion L (2009) Fixed- vs mobile-bearing total knee arthroplasty: does it make a difference?—a prospective randomized study. J Arthroplast 24(6 Suppl):24–27
Hasegawa M, Sudo A, Uchida A (2009) Staged bilateral mobile-bearing and fixed-bearing total knee arthroplasty in the same patients: a prospective comparison of a posterior-stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc 17(3):237–243
Huang CH, Ma HM, Liau JJ, Ho FY, Cheng CK (2002) Osteolysis in failed total knee arthroplasty: a comparison of mobile-bearing and fixed-bearing knees. J Bone Joint Surg Am 84-A(12):2224–2229
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jacobs W, Anderson P, Limbeek J, Wymenga A (2004) Mobile bearing vs fixed bearing prostheses for total knee arthroplasty for post-operative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev (2):CD003130
Jacobs WCH, Christen B, Wymenga AB, Schuster A, van der Schaaf DB, Ten Ham A, Wehrli U (2011) Functional performance of mobile versus fixed bearing total knee prostheses: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-011-1684-9
Kim BS, Reitman RD, Schai PA, Scott RD (1999) Selective patellar nonresurfacing in total knee arthroplasty. 10 year results. Clin Orthop Relat Res 367:81–88
Kim YH, Kim DY, Kim JS (2007) Simultaneous mobile- and fixed-bearing total knee replacement in the same patients. A prospective comparison of mid-term outcomes using a similar design of prosthesis. J Bone Joint Surg Br 89(7):904–910
Kim YH, Kook HK, Kim JS (2001) Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res 392:101–115
Kim YH, Yoon SH, Kim JS (2009) Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 467:493–503
Ladermann A, Lubbeke A, Stern R, Riand N, Fritschy D (2008) Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomised, clinical and radiological study with mid-term results at 7 years. Knee 15(3):206–210
Lampe F, Sufi-Siavach A, Bohlen KE, Hille E, Dries SP (2011) One year after navigated total knee replacement, no clinically relevant difference found between fixed bearing and mobile bearing knee replacement in a double-blind randomized controlled trial. Open Orthop J 5:201–208
Luna JT, Sembrano JN, Gioe TJ (2010) Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs: surgical technique. J Bone Joint Surg Am 92(Suppl 1 Pt 2):240–249
Matsuda S, Mizu-uchi H, Fukagawa S, Miura H, Okazaki K, Matsuda H, Iwamoto Y (2010) Mobile-bearing prosthesis did not improve mid-term clinical results of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 18(10):1311–1316
McEwen HM, Barnett PI, Bell CJ, Farrar R, Auger DD, Stone MH, Fisher J (2005) The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J Biomech 38(2):357–365
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56(7):1391–1396
Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B (2005) The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res 14(3):875–882
O’Connor JJ, Goodfellow JW (1996) Theory and practice of meniscal knee replacement: designing against wear. Proc Inst Mech Eng H 210(3):217–222
Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, de Steiger R, Dodd CA, Gibbons M, McLardy-Smith P, Goodfellow JW, Murray DW (2003) A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br 85(1):62–67
Ranawat CS, Luessenhop CP, Rodriguez JA (1997) The press-fit condylar modular total knee system. Four-to-six-year results with a posterior-cruciate-substituting design. J Bone Joint Surg Am 79(3):342–348
Saghaei M (2004) Random allocation software for parallel group randomized trials. BMC Med Res Methodol 4:26
Sehat K, Devan P, Horne G (2007) Fixed bearing or mobile bearing total knee arthroplasty? A review of the recent literature. Curr Opin Orthop 18:66–70
Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R (2011) Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplast 26(8):1205–1213
Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H (2005) Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop 29(3):179–181
Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E (2008) Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 90(9):1172–1179
Acknowledgments
We thank all the staff nurses of the Orthopedic Department at Al-Zahra and Kashani University Hospitals for their valuable help. Also, we are all thankful for the editing assistance that Professor Jagodzinski (Hannover University of Medical Sciences, Germany) provided. This research was supported financially by the Vice-Chancellery of Research at Isfahan University of Medical Sciences (Isfahan University of Medical Sciences Research Project No. 187263).
Conflict of interest
All author confirmed that no conflict of interest is existed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical Trial Registration: The study was registered at http://www.clinicaltrials.gov (Identifier: NCT01312532).
Rights and permissions
About this article
Cite this article
Shemshaki, H., Dehghani, M., Eshaghi, M.A. et al. Fixed versus mobile weight-bearing prosthesis in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20, 2519–2527 (2012). https://doi.org/10.1007/s00167-012-1946-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1946-1