Abstract
Purpose
One long-held tenet of total knee arthroplasty (TKA) is that post-operative neutral limb alignment promotes implant durability. Recently, the concept of generic safe zone (0° ± 3°) has been challenged. This meta-analysis aimed to evaluate whether neutral alignment was superior to malalignment in long-term survival of TKAs.
Methods
The MEDLINE, Embase, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Chinese Periodical, Google and reference lists of all the included studies were searched. Of the 1512 studies initially identified, ten met the eligibility criteria, including eight case–control studies and two cohort trials. Relative risks of implant failure were compared between post-operative neutrally aligned and malaligned knees.
Results
Post-operative malalignment showed higher failure rate of knee implants compared with neutral alignment (95 % CI 1.00–1.88, P = 0.05). Failure rate in knees with varus alignment was significantly higher than with neutral alignment (95 % CI 1.07–2.55, P = 0.02). There was no significant difference in the likelihood of implant failure between knees with valgus and neutral alignment (95 % CI 0.78–2.41, n.s.). No significant difference of failure rate was noted between neutral alignment and malalignment for fixed-bearing prothesis (95 % CI 0.94–1.95, n.s.) or rotating-platform prothesis (95 % CI 0.75–2.73, n.s.). There was no significant difference of failure rate between knees with neutral alignment and malalignment for studies with a mean follow-up of more than 10 years (95 % CI 0.81–2.01, n.s.) or studies using long-leg weight-bearing radiographs (95 % CI 0.79–1.79, n.s.).
Conclusions
Post-operative varus alignment results in shorter survival rate after TKA. Not only neutral limb alignment but also the valgus alignment promotes implant durability. Neutral or valgus alignment rather than varus alignment is essential to achieve long-term survival of TKAs and patient satisfaction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary total knee arthroplasty (TKA) has been proved to be successful surgery with long-term survival. One long-held tenet of TKA is that post-operative neutral limb alignment promotes implant durability. If incorrect, they can lead to abnormal wear, premature loosening and patellofemoral problems [2]. A series of studies demonstrate that restoring the mechanical axis of the lower extremity in neutral alignment contributes to a more durable implant and, otherwise, increases the incidence of loosening of the knee prothesis [8, 12, 23–26]. Not only prodigious clinical evidences support the concept of neutral coronal alignment favouring long-term survival of prothesis, but also numerous contemporary biomechanical and finite element studies [10, 17, 19] have demonstrated that malalignment, particularly varus, is associated with increased medial tibial surface strain, leading to medial cancellous bone overload and eventual failure through medial tibial collapse.
However, several recently published studies [18–21] demonstrating no significant difference in survivorship when comparing well-aligned versus malaligned TKAs have challenged the concept of generic safe zone, traditionally within 3° of neutral. Parratte et al. [21] found that a post-operative mechanical axis of 0° ± 3° did not improve the survival rate 15 years post-operatively, and concluded that the description of alignment as a dichotomous variable (neutrally aligned vs. malaligned) provided little value in regard to durability. After a review of the available literature, one conventional clinical trial [22] also suggested that knee arthroplasties were unable to confirm the importance of alignment in the long-term survival of knee implants. Thus, whether neutral alignment would contribute to longer survival rate after TKAs has become a controversial new topic.
The traditional main concept in TKAs is aiming the exact mechanical alignment of the lower limb. Recently, however, the concept of anatomical restoration has gained interest among knee surgeons [11]. Howell et al. [11] found that varus alignment of the knee did not adversely affect implant survival or function after kinematically aligned TKA with a mean follow-up of 6.3 years and suggested kinematic alignment as an alternative to mechanical alignment for performing primary TKA. However, whether the varus alignment and oblique joint line would change the stress distribution and affect the long-term survival was questioned [14]. In addition, since constitutional varus alignment of the lower limb was fairly common in normal adults [27], restoration of mechanical alignment to neutral in these cases seemed to be not desirable and would be unnatural for them [3, 30]. Although anatomical restoration of alignment was proposed in these patients with constitutional varus [30], whether post-operative varus alignment would result in short survival rate remained unclear. Moreover, since the severity of pre-operative varus deformity may influence post-operative alignment, some surgeons suggested that ensuring an accurate alignment was important [2], and others argued that correction towards their original status could be a more physiological option [3, 30].
Thus, a meta-analysis of survival of TKAs with post-operative neutral alignment versus malalignment was conducted. Our hypothesis was that restoration of neutral mechanical alignment in theory might lead to longer survival rate compared with malalignment after TKAs; therefore, it could potentially be beneficial to patients. The objectives of our study were: firstly, to examine whether neutral alignment took advantage over either varus or valgus alignment for survival of TKAs, and secondly, to conduct subgroup analysis of TKA survival with neutral alignment versus malalignment according to fixation type of implant, duration of follow-up and measurement method of lower limb alignment. If the hypothesis is confirmed and neutral mechanical alignment indeed shows longer survival rate of TKA than either varus or valgus alignment, it could confirm that malalignment placed a risk of failure after TKA and should be avoided.
Materials and methods
A meta-analysis of all English and non-English articles identified from electronic databases including MEDLINE, Embase, Cochrane Library, China National Knowledge Infrastructure, Wan Fang Chinese Periodical and Google was conducted. In addition, further relevant studies including those of reference lists of all the included studies were also manually searched. The last search was carried out on 3 December 2014. The following key words: arthroplasty, replacement, knee, total knee arthroplasty, alignment, failure, revision, survival and survivorship, in combination with the Boolean operators AND or OR were used. The search strategy is presented in Fig. 1.
Inclusion and exclusion criteria
All published randomized control trials, non-randomized cohort trials and case–control studies evaluating the survival rate of knee prothesis with neutral alignment and malalignment were included. Inclusion criteria comprised the following: primary TKA; description of limb axial alignment as a dichotomous variable (neutral aligned vs. malaligned, neutral vs. varus or neutral vs. valgus); reporting failure rate, revision rate or survival rate; and reporting post-operative malalignment (malaligned, varus or valgus). Exclusion criteria comprised the following: not original research, non-consecutive case series, unicompartmental knee arthroplasty, revision TKA, a zero failure rate of TKA, older-design TKAs with high failure rates and duplicate records within the same functional centre.
Data extraction
For each eligible study, two of the authors independently extracted all relevant data. Disagreement was resolved by discussion with a third investigator. The following variables were abstracted: authors, year of publication, country, study design, sample size, patient gender, mean age, TKA system, measurement method of alignment, evaluating time of implant failure or mean duration of follow-up, and failure rates in all groups (neutral, varus and valgus alignments). When data were incomplete or unclear, attempts were made to contact the investigators for clarification. Regarding the cause of knee replacement failure, only mechanical failure was included, such as aseptic loosening, radiographic wear and patellar complications [5, 21]. Neutral alignment was within 0° ± 3° in reference to mechanical axis or 2.4°–7.2° of valgus in anatomical femoral–tibial angle. Several studies describing slightly different criteria for neutral alignments, such as 3°–7.5° of valgus in femoral-tibial angle, were also included.
Quality criteria
The quality assessment of included studies was based on the Newcastle–Ottawa scale (NOS) [28]. Using the tool, each study was judged on eight items, categorized into three groups: the selection of the study groups; the comparability of the groups; and the ascertainment of either the exposure or outcome of interest for case–control or cohort studies, respectively. Stars awarded for each quality item serve as a quick visual assessment. Stars are awarded as such that the highest quality studies are awarded up to nine stars.
Analysis of data
This meta-analysis was undertaken using RevMan 5.0 (Cochrane Collaboration, Oxford, UK). We assessed the statistical heterogeneity using a standard Chi-square test (statistical heterogeneity was considered to be present at P < 0.1 and I 2 values >50 %). Pooled data were meta-analysed using a fixation effects model as no heterogeneity exhibited comparing these trials. Adjusted risk ratio (RR) and 95 % CIs were calculated for generic inverse variance outcomes. Where an adjusted RR of <1 favoured malalignment, an adjusted RR of 1 suggested no difference between neutral alignment and malalignment, and an adjusted RR >1 favoured neutral alignment. For the publication with zero events in one group, each cell in the contingency table was inflated by adding 0.5.
Results
There were 1512 potentially relevant papers. By screening titles and reading the abstracts and entire articles, ten studies with 12,278 knees were included in the final meta-analysis (Fig. 1). All of these trials were published in English. The sample sizes ranged from 168 to 6070 knees. There were eight case–control studies [5, 8, 15, 16, 18, 20, 21, 26] and two cohort trials [12, 13]. Fixed-bearing protheses for TKAs were used in seven studies, and rotating-platform protheses were used in three studies. There were four studies with a mean follow-up of more than 10 years. Long-leg weight-bearing radiographs were used for alignment measurement in seven studies and anteroposterior knee radiographs in three studies. Table 1 summarizes the key characteristics of the included trials. The methodology quality of the ten included studies is presented in Table 2.
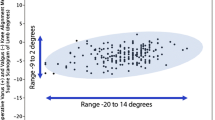
The pooled results indicated that the failure rate of implant was higher in knees with post-operative malalignment compared with neutral alignment (95 % CI 1.00–1.88, P = 0.05, Fig. 2). Failure rate in knees with post-operative varus alignment, reported in five studies, was higher compared with neutral alignment (95 % CI 1.07–2.55, P = 0.02, Fig. 3). Comparison of failure rate between knees with valgus and neutral alignment was conducted in four studies with no significant difference (n.s., Fig. 4). Subgroup analysis was conducted according to the fixation type of prothesis in TKA. No significant difference of failure rate was noted between neutral alignment and malalignment for fixed-bearing protheses (n.s., Fig. 5) or rotating-platform protheses (n.s., Fig. 5). Four studies with a mean follow-up of more than 10 years showed no significant difference of failure rate between knees with neutral alignment and malalignment (n.s., Fig. 6). Seven studies using long-leg weight-bearing radiographs showed no significant difference of failure rate between knees with neutral alignment and malalignment (n.s., Fig. 7). Three studies using anteroposterior knee radiographs showed neutral alignment taking advantage over malalignment (95 % CI 1.03–2.80, P = 0.04, Fig. 7).
Discussion
The most important findings of the present study were the post-operative varus alignment (beyond 3°) indeed, as hypothesized, showing a higher failure rate of knee implants than the neutral alignment in patients undergone primary TKA. However, it was unexpected that no sufficient evidence proved the difference of failure rate between knees with neutral alignment and valgus alignment.
Most surgeons have accepted the premise that the deviation beyond 3° of varus mechanical axis is associated with worse implant survival following total knee arthroplasty [4, 8, 9, 12, 23–26]. This is consistent with the results of current meta-analysis. Clinical evidences show that varus alignment is associated with a significant loss of polyethylene thickness in the medial compartment of the tibial component, which also leads to higher failure rates and poorer outcomes [4, 5, 15]. Moreover, a mechanical axis beyond 3° of varus in the coronal plane remains a less satisfactory target in TKA surgery if the biomechanical evidence, retrieval evidence, computer predictions and clinical evidence are considered together.
When neutral mechanical alignment is restored, the mechanical axis of the leg passes through the centre of the knee, which leads to an even mediolateral load distribution and a minimized risk of implant wear and component loosening [31]. Malalignment of the lower limb could affect load distribution of the medial and lateral regions of the tibial plateau. The load over the medial tibial plateau shares between 70 and 77 % when the limb alignment is left 3° varus [9, 10]. Then, adduction overloads the medial compartment and may cause asymmetrical polyethylene liner wear, tibial component loosening and mechanical failure [11].
Although the neutral mechanical axis is a valuable intraoperative target [1, 13, 16], its achievement does not necessarily confer better implant survival over valgus alignment in current meta-analysis. This could be explained as follows:valgus alignment leads to increased forces passing through the lateral tibial plateau; however, both proximal tibiofibular joint and lateral tibiofemoral joint perform weight-bearing function [6]. Thus, compared with varus alignment, valgus alignment reduces the possibility of tibial collapse and polyethylene thickness loss. Although no statistical difference of failure rate of TKAs is noted between valgus and neutrally aligned knees, the trend is towards fewer revisions in neutral alignment. As few studies report the relative failure rate for TKAs aligned in valgus, it remains for future investigations to determine whether neutral alignment takes advantage over valgus alignment in improving the long-term survival of TKAs.
A number of patients with so-called constitutional varus knees have had varus alignment since they reached skeletal maturity. Some surgeons suggested that correction towards their original constitutional status could be a more physiological option [3, 30] and residual varus alignment did not compromise results of TKAs but improved functional scores in patients with pre-operative varus (more than 10°) [10, 18], while this concept was confirmed in another study, which noted that patients with pre-operative varus had better clinical and functional outcome scores if the alignment was left in mild varus, compared to patients with an alignment correction to neutral [29]. Thus, restoration of constitutional alignment within the “safe zone” of 0° ± 3° during TKA could lead to more physiological peri-articular soft tissue strains and good function. However, excessive varus alignment (>3°) might increase the risk of early failure and should not be a target of post-operative alignment.
Kinematically aligned TKA has gained interest because of its good function and contact kinematics [11]. The goal of kinematically aligned TKA is to position the femoral and tibial components so that the angles and levels of the distal and posterior femoral joint lines and the tibial joint line are each restored to the patient’s natural alignment and not to a neutral limb alignment. The kinematically aligned knee provided neutral limb alignment with mean 0.3° for hip–knee–ankle angle and oblique joint line with mean 1.4° valgus for the femoral component and mean 2.4° varus for the tibial component [7]. In addition, biomechanical study suggested that varus alignment showed a significant posterior displacement of the medial femoral condyle and anterior displacement of the lateral femoral condyle as compared to the normal alignment [9]. Assuming that the principle of aligning the limb on the mechanical axis is important for longevity of the prosthesis, then kinematic alignment method should have similar durability compared with mechanical alignment. However, previously published alignment data for these patients showed that kinematic alignment did not preclude lower limb malalignment [11]. Moreover, excessive oblique tibial joint line angle (>3°) might increase shear stress on the medial proximal tibia, which might place the TKA at a high risk of early failure [14].
The current meta-analysis has several limitations. Firstly, like most studies of alignment after TKA, the present study focused on the static, coronal plane alignment and did not specifically evaluate either sagittal plane or rotational alignment or the dynamic impact of gait on alignment. Secondly, one study [26] did not state the reasons for implant failure. Apart from aseptic mechanical failure, if other reasons, such as fracture and infection, were presented, which could possibly bias the results. Thirdly, as no consensus whether the anatomical or mechanical axis was used to describe overall coronal alignment, both 2.4°–7.2° of valgus in anatomical tibiofemoral angle and mechanical axis within 0° ± 3° were considered to be neutral alignment that could possibly bias the results. Since each subgroup analysis shows no significant difference of failure rate between neutral alignment and malalignment (fixed-bearing prothesis, rotating-platform prothesis, follow-up of more than 10 years, long-leg weight-bearing radiographs for alignment measurement), further researches on these matter are necessary to support the conclusion.
The post-operative alignment of the knee is still the most important factor affecting the survival rate of knee implants. These findings contribute to gaining a proper understanding that more than 3° post-operative varus alignment should be avoided in both mechanically and kinematically aligned TKAs, including patients with pre-operative severe varus deformity or constitutional varus. It might be useful for orthopaedic surgeons in achieving long-term survival of TKAs and patient satisfaction.
Conclusion
More than 3° post-operative varus alignment results in shorter survival rate after TKA compared with neutral alignment. Both neutral limb alignment and valgus alignment promote implant durability.
References
Alden KJ, Pagnano MW (2008) Computer-assisted surgery: a wine before its time. Orthopedics 31:936–939
Bae DK, Song SJ, Heo DB et al (2013) Does the severity of preoperative varus deformity influence postoperative alignment in both conventional and computer-assisted total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 21(10):2248–2254
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) Is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53
Berend ME, Ritter MA, Meding JB et al (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
BonnerTJ Eardley WG, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg (Br) 93:1217–1222
Boya H, Ozcan O, Oztekin HH (2008) Radiological evaluation of the proximal tibiofibular joint in knees with severe primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 16(2):157–159
Dossett HG, Estrada NA, Swartz GJ et al (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 96-B(7):907–913
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24:39–43
Fujimoto E, Sasahige Y, Tomita T et al (2015) Different femorotibial contact on the weight-bearing: midflexion between normal and varus aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1720–1728
Halder A, Kutzner I, Graichen F et al (2012) Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am 94:1023–1029
Howell SM, Papadopoulos S, Kuznik K et al (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. doi:10.1007/s00264-015-2743-5
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38:379–385
Kim YH, Park JW, Kim JS (2012) Computer-navigated versus conventional total knee arthroplasty a prospective randomized trial. J Bone Joint Surg (Am) 94:2017–2024
Klatt BA, Goyal N, Austin MS, Hozack WJ (2008) Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty 23(1):26–29
Lee BS, Lee SJ, Kim JM et al (2011) No impact of severe varus deformity on clinical outcome after posterior stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:960–966
Lee HJ, Jung HJ, Jung YB (2014) Time-dependent clinical results of rotating-platform total knee arthroplasty according to mechanical axis deviation. Knee Surg Relat Res 26:141–148
Lombardi AV Jr, Berend KR, Ng VY (2011) Neutral mechanical alignment: a requirement for successful TKA: affirms. Orthopedics 34(9):504–506
Magnussen RA, Weppe F, Demey G (2011) Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 469:3443–3450
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130:1487–1491
Morgan SS, Bonshahi A, Pradhan N (2008) The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop 32:639–642
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg (Am) 92:2143–2149
Rand JA, Coventry MB (1988) Ten-year evaluation of geometric total knee arthroplasty. Clin Orthop Relat Res 232:168–173
Ritter MA (2009) The Anatomical Graduated Component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg [Br] 91:745–749
Ritter MA, Davis KE, Davis P et al (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg [Am] 95:126–131
Ritter MA, Davis KE, Meding JB et al (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg (Am) 93:1588–1596
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Shetty GM, Mullaji A, Bhayde S, Nha KW, Oh HK (2014) Factors contributing to inherent varus alignment of lower limb in normal Asian adults: role of tibial plateau inclination. Knee 21(2):544–548
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight under correction following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Victor JM, Bassens D, Bellemans J et al (2014) Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 472(1):98–104
Zhao D, Banks SA, D’Lima DD et al (2007) In vivo medial and lateral tibial loads during dynamic and high flexion activities. J Orthop Res 25(5):593–602
Author information
Authors and Affiliations
Corresponding author
Additional information
Hai-xiao Liu and Ping Shang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Liu, Hx., Shang, P., Ying, XZ. et al. Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 2663–2671 (2016). https://doi.org/10.1007/s00167-015-3781-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3781-7