Abstract
Purpose
The influence of residual malalignment on biomechanical analysis after total knee arthroplasty (TKA) is currently uncertain. The hypothesis is that postoperative alignment would influence the in vivo kinematics after TKA, under weight-bearing conditions but not under non-weight-bearing condition. The purpose of the present study was to compare weight-bearing and non-weight-bearing conditions and to evaluate the effect of the postoperative alignment on the in vivo kinematics after posterior cruciate ligament-retaining TKA during midflexion using 2-dimensional/3-dimensional registration.
Methods
Thirty knees of 30 patients with pre-operative varus deformity were divided into 2 groups according to their postoperative alignment: the normal alignment group (N = 21) and the varus alignment group (N = 9).
Results
Under weight-bearing conditions, the varus alignment group showed a significant posterior displacement of the medial femoral condyle (flexion: 80°, 90° P < 0.05) and a significant anterior displacement of the lateral femoral condyle (flexion: 10° P < 0.01, 20° P < 0.05, and extension: 10°, 20° P < 0.01, 30°, 40° P < 0.05) as compared with the normal alignment group. In contrast, no significant difference in the medial and lateral femoral condyle positions under non-weight-bearing conditions was observed between the normal and varus alignment groups.
Conclusion
The postoperative alignment influenced knee kinematics under weight-bearing conditions. The weight load influenced knee kinematics through posterior tibial slope and induced greater lateral femoral condyle mobility, which might explain the better clinical and functional outcome. These findings contribute to gaining a proper understanding of the in vivo kinematics of the postoperative varus alignment and might be useful for orthopaedic surgeons in the achievement of patient satisfaction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The alignment of the knee following total knee replacement as seen on anteroposterior radiographs may be the most important factor determining the long-term survival of the prosthesis [2, 5, 11, 13, 20, 25, 28–33]. The many studies reported that malalignment leads to unfavourable mediolateral force distribution, which overloads the bone–implant interface as well as the bone itself, resulting in loosening of the implant [38]. The majority of studies reported greater contact force on the medial compartment. Even with neutral alignment, medial load shares between 55 and 70 % were calculated [6, 38]. Halder reported in vivo loads related to the alignment after implantation of an instrumented tibial baseplate and concluded that the medial load shares in neutral alignment were about 60 % [14]. In varus alignment, finite element model analysis studies revealed a nearly 150 % increase in maximum contact stresses with a varus tilt of only 5° [24]. Halder also reported medial load shares with a 3° varus alignment of 70–77 % in an in vivo study [14]. While the effect of alignment on force distribution is relatively well understood, the effect of residual malalignment on clinical and functional outcomes is less well known. Some authors have suggested that a slight undercorrection of the deformity could be beneficial from clinical and functional perspectives [18, 19, 36]. However, current literature lacks a precise in vivo kinematic view of varus alignment in postoperative total knee replacement.
Over the past 15 years, in vivo fluoroscopic analyses have been performed on subjects with various types of knee conditions. These studies involved normal knees [9, 10, 22, 26], and patients with many types of knee arthroplasties. The results from these studies on subjects with normal knees revealed that the lateral condyle experiences significantly more posterior motion than the medial condyle throughout knee flexion [10, 22, 26]. This kinematic pattern where the lateral condyle translates more posteriorly than the medial condyle also creates an external femoral rotation pattern with increasing flexion that has been documented [9]. In vivo kinematic analyses suggest that total knee arthroplasty (TKA) patients often display a different pattern than normal subjects [1, 8, 9, 17, 21, 40]. These abnormal kinematic patterns could lead to a decrease in both ROM and function after TKA [37].
Cruciate-retaining (CR) TKA is designed for the control of both posterior cruciate and bilateral collateral ligaments. This prosthesis has a relaxed geometry and does not restrict the femoral component movement. Therefore, the kinematics of posterior CR TKA are influenced by many factors [23]. The posterior tibial slope (PTS) is an important surgical factor affecting the postoperative knee flexion angle and the kinematics of CR TKA [3, 4, 27]. Our in vivo kinematic studies have revealed that PTS significantly affects the anteroposterior position under weight-bearing condition after CR TKA [12]. Large PTS induced posterior forces on the femur through weight load under weight-bearing conditions, and the femur was forced to shift posteriorly. We concluded that weight load could affect knee kinematics under weight-bearing conditions through impacts on the PTS.
From this point of view, postoperative alignment will affect in vivo kinematics and physiological varus alignment might lead to a higher medial load and a lower lateral load. This condition might induce medial pivot, lateral condyle posterior translation and physiological rotation patterns (including screw-home movement) and could lead to an increase in both ROM and function after TKA.
The hypothesis of this paper is that the in vivo kinematics after TKA under weight-bearing conditions but not under non-weight-bearing conditions would be influenced by postoperative alignment. Accordingly, we compared the in vivo kinematics during midflexion in the same patients under both weight-bearing and non-weight-bearing conditions and evaluated the effects of their postoperative alignment.
Materials and methods
A total of 30 implants in 30 patients were analysed. All patients underwent implantation of a NRG CR cementless TKA. Of the 30 patients, 25 (83.3 %) were women and 5 (16.7 %) were men. All 30 patients had primary varus osteoarthritis. The average age was 74.6 ± 6.3 years (mean ± SD), and the average postoperative time was 23.2 ± 6.4 months. Thirty patients were selected from our prospective database containing all patients who had received TKAs and were contacted for their consent to be included in this study. All subjects who underwent a successful TKA resulting in more than 90 points on the Knee Society Score, without any measurable ligament laxity or pain, were chosen for this study, thus representing a convenient sample of the best performers.
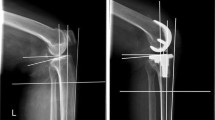
All components were well fixed according to radiographic evaluations during the postoperative follow-up. In this study, we chose exact postoperative anteroposterior (AP) and lateral radiographs and full-length AP radiographs. Mechanical axes of each extremity were defined by straight lines drawn based on Sikorski’s and Vanlommel’s descriptions [33, 36]. The mechanical femoral and tibia angle was measured accordingly. The mechanical axis of femur between the centre of the femoral head and the middle of the intercondylar region and the mechanical axis of tibia between the centre of the tibial component surface and the centre of the talus were made, and the mechanical femoral and tibia angle represents the angle between the mechanical axis of femur and the mechanical axis of tibia (Fig. 1a). Mechanical axis of limb was defined by a straight line drawn from the centres of the femoral head to the centre of the talus. The weight-bearing ratio was calculated by measuring the distance from the medial edge of the proximal tibia to the point where the mechanical axis of limb intersects the proximal tibia, and then dividing that measurement by the entire width of the proximal tibia. A percentage was calculated by multiplying this ratio by 100 % (Fig. 1b).
Mechanical femoral–tibial angle and weight-bearing ratio. a Mechanical axis of femur, tibia, and limb were defined by the use of full-length AP radiographs. The mechanical femoral tibial angle represents the angle between mechanical axis of femur and tibia. b The location where the mechanical axis of limb intersects the tibial component is expressed as a percentage of tibia with (weight-bearing ratio = a/b × 100 %)
These 30 patients were divided into 2 groups according to a discriminatory threshold of 40 % weight-bearing ratio: nine knees were in the varus alignment group (weight-bearing ratio 28.5 ± 10.3 %) (mechanical femoral and tibia angle 184.4° ± 1.5°), and 21 knees were in the normal alignment group (weight-bearing ratio 55.0 ± 7.0 %) (mechanical femoral and tibia angle 178.8° ± 1.8°).
Regarding the posterior slope (PTS), Han reported that the PTS is measured against the fibular shaft and that the angle between the tibial anatomical axis and the fibular shaft axis was 3.0 degrees [16]. This angle between the fibular shaft and the tibial component was measured, and the PTS angle was defined as the measured angle plus 3.0 degrees. The PTS of the varus alignment group was 4.6° ± 4.2° and that of normal alignment group was 6.9° ± 3.4°. No significant deference was detected between the two groups.
Surgical technique
The surgery was performed by the same senior author using a CR TKA (NRG-CR) (Stryker Orthopaedics, Mahwah, NJ). All TKAs were performed using the modified gap-balance technique with a conventional resection block and a commercially available tensor system, the JDK system (Joint Dependent Kinematics) (Stryker Orthopaedics, Mahwah, NJ). Under a tourniquet, we performed a midvastus arthrotomy. A distal femoral osteotomy and then a proximal tibial osteotomy were performed perpendicular to the mechanical axes of the femur and tibia. A proximal tibial osteotomy was then performed with 7° degrees of posterior inclination along the sagittal plane. Next, any osteophytes were removed, and the ligament imbalances in the coronal plane were corrected by releasing the medial soft tissues appropriately. The femoral component was positioned parallel to the resected proximal tibia, with each collateral ligament tensioned as equally as possible with the JDK system. No PCL release was performed in any of these knees. Finally, we removed the osteophytes from the patella without resurfacing and confirmed the appropriate patellar tracking. All of the femoral and tibial components were cementless hydroxyapatite-coated NRG TKA prostheses in this series.
In vivo kinematic analysis
Each patient was asked to perform sequential deep knee bends from the extended position and full extension from the flexed position under both weight-bearing and non-weight-bearing conditions. Both motions from full extension to maximum flexion and from maximum flexion to full extension were monitored fluoroscopically in the sagittal plane. For the non-weight-bearing condition, the patient sat on a chair and was asked to perform active knee bending and extension. We assisted the patient in bending their knee to capture measurements on the flat panel. When obtaining images, the patients stood or lay on their back with their legs in neutral rotation. Successive knee movements were then recorded as serial digital X-ray images (512 × 512 × 12 bits/pixels, 7.5-Hz serial spot images as a DICOM file) using a 9-in digital image intensifier system (BRANSIST Safire, Shimadzu, Japan) and pulsed X-ray beams of 1–2 ms. The 3D positions of the Scorpio NRG CR prosthesis were computed at 10° flexion intervals by a 2D/3D registration technique, which used computer-assisted design (CAD) models to reproduce the positions of the femoral and tibial components from calibrated (including corrections for distortion) single-view fluoroscopic images. The registration algorithm proposed by Zuffi et al. [41] was used in the current study. This algorithm uses a feature-based approach to minimizing distances between lines drawn from a contour found on the 2D image to the X-ray source, and a surface CAD model with iterative computations. Validation of this 2D/3D registration technique was performed by experiments using a phantom of the knee. An Optotrak 3020 system (Northern Digital Inc, Ontario, Canada), which is a 3D optical localizer that tracks infrared light-emitting diode-mounted markers with an accuracy of about 0.1 mm, was used to determine the “grand-truth” positions for comparison with the 2D/3D registration method. The femoral and tibial components were then installed on artificial bones with attached light-emitting diode markers, and then sagittal images were obtained in 10 different poses and digitized using the Optotrak system. The experimental accuracy was assessed by comparing the estimated relative locations of the femoral and tibial components with the grand-truth poses determined by the Optotrak system. The root mean square errors of the relative position of the femoral component in the tibial component coordinate system were 0.2°, 0.6°, and 0.6° for rotation in the coronal, axial, and sagittal planes, respectively, and 0.6, 0.3, and 1.0 mm for translation perpendicular to the coronal, axial, and sagittal planes, respectively. The largest errors in relative position were 0.5°, 0.8°, and 0.8° in the coronal, axial, and sagittal planes, respectively, and 2.1 mm perpendicular to the coronal, axial, and sagittal planes. These values were included in the current kinematic analysis. The errors were smaller than those previously reported, apparently due to the use of higher resolution images.
The range of motion and axial rotation angles between the femoral and tibial components were evaluated, but the angle between the femoral and tibial shafts was not evaluated. In a fixed-bearing TKA, the 3D position of the radiolucent tibial polyethylene insert can be determined from the estimated position of the tibial component [39]. In the femoral coordinate system, the origin was defined as the centre of gravity for the component. In the tibial coordinate system, the origin was defined as the centre of the tibial surface. Anteroposterior translation of the nearest point between the femoral component and the tibial polyethylene insert for the medial and lateral sides was then measured. Axial femoral rotation was defined as positive for external rotation, and negative for internal rotation. On the medial and lateral sides, the nearest point of the femoral component relative to the tibial insert as the centre of the quasi-contact was determined by calculating the nearest distance between the surfaces of the CAD models. The anteroposterior positions of the femoral component anterior to the tibial insert were designated as positive, and the posterior positions were designated as negative.
Statistical analysis
All data in the text are expressed as mean ± SD and as mean ± standard error of the mean (SEM) in the figures. A statistical software package (Statview, Abacus Concepts Inc, Berkeley, CA) was utilized to analyse the data. The Wilcoxon test for comparisons between paired groups, and the Mann–Whitney test between the normal alignment and varus alignment groups were used. P values less than 0.05 were considered statistically significant.
Results
Kinematics under weight-bearing conditions
Under weight-bearing conditions from 0° to 100° of flexion from the extended position, the average nearest medial point was constant for both normal alignment (between −1.2 and 0.1 mm) and varus alignment (between −2.4 and -0.9 mm). The average nearest medial point of varus alignment was more posterior than that of normal alignment, and significant differences were detected at 80° and 90° of knee flexion during flexion from the extended position (P < 0.05) (Fig. 2a).
Normal and varus alignment groups during flexion from the extended position (a–c) and during extension from the flexed position (d–f) under weight-bearing conditions. The average nearest medial point of varus alignment was more posterior than that of normal alignment during both flexion from the extended position (a) and extension from the flexed position (d), and significant differences were detected during flexion from the extended position (a). On the other hand, the average nearest lateral point of varus alignment was significantly more anterior than that of normal alignment during both flexion from the extended position (b) and extension from the flexed position (e). The average external rotation of varus alignment was significantly smaller than that of normal alignment during both flexion from the extended position (c) and extension from the flexed position (f)
At 0° of knee flexion, the average nearest lateral point of the normal alignment group was 3.9 ± 3.2 mm. The average nearest lateral point of the normal alignment group moved 6.0 mm posteriorly from 0° to 100° and reached −9.9 ± 3.3 mm at 100° of knee flexion. The average nearest lateral point of the varus alignment group also moved 9.2 mm posteriorly from 10° to 90°. The average nearest lateral point of the varus alignment group was more anterior than that of the normal alignment group, and significant differences were detected at 10° (P < 0.01) and 20° (P < 0.05) of knee flexion during flexion from the extended position (Fig. 2b).
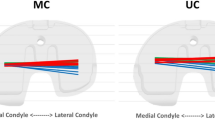
Under weight-bearing conditions for flexion from the extended position, the medial condyle remained motionless. However, the lateral condyle moved 6.0 mm posteriorly from 0° to 100° of knee flexion for the normal alignment group and 9.2 mm posteriorly from 0° to 90° of knee flexion for the varus alignment group. Under weight-bearing conditions, the femoral component displayed a medial pivot pattern.
Regarding axial rotation of the femoral component relative to the tibial component, the mean axial rotation of the normal alignment group was 2.7° ± 4.1° at 0° of knee flexion and 11.1° ± 4.3° at 100° of knee flexion. The femoral component exhibited gradual external rotation from 0° to 100°. In contrast, the mean axial rotation of the varus alignment group was 1.2° ± 1.8° at 0° of knee flexion, 0.1° ± 2.3° at 10° of knee flexion, and 8.2° ± 4.5° at 90° of knee flexion. The femoral component exhibited internal rotation from 0° to 10° and then gradual external rotation from 10° of knee flexion to 90° (Fig. 2c). All knees in varus alignment generally exhibited a combination of internal and external rotation patterns.
Under weight-bearing conditions from 100° to 0° of extension from the flexed position, the average nearest medial point was also constant for both normal alignment and varus alignment. The average nearest medial point of varus alignment was also more posterior than that of normal alignment during extension from the flexed position, although significant differences were not detected (Fig. 2d).
The average nearest lateral point of normal alignment moved 6.4 mm anteriorly from 100° to 20°. The average nearest lateral point of varus alignment group also moved 9.6 mm anteriorly from 90° to 10°. The average nearest lateral point of varus alignment was more anterior than that of normal alignment, and significant differences were detected at 10° (P < 0.01), 20° (P < 0.01), 30° (P < 0.05) and 40° (P < 0.05) of knee flexion during extension from the flexed position (Fig. 2e).
Under weight-bearing conditions during extension from the flexed position, the medial condyle remained motionless and the lateral condyle moved anteriorly in the normal alignment group and the varus alignment group. Under weight-bearing conditions, the femoral component also displayed a medial pivot pattern.
Regarding axial rotation of the femoral component relative to the tibial component, the femoral component exhibited gradual internal rotation from 100° to 0°. In contrast, the femoral component initially exhibited internal rotation from 90° to 10° and gradual external rotation from 10° to 0° (Fig. 2f). All knees in varus alignment generally exhibited a combination of internal and external rotation pattern.
Kinematics under non-weight-bearing conditions
Kinematics under non-weight-bearing conditions were examined from 0° to 100° of flexion from the extended position. At 0° of knee flexion, the average nearest medial point of normal alignment group was −0.6 ± 1.7 mm. The average nearest medial point moved 5.2 mm anteriorly to reach 4.6 ± 2.5 mm at 80° of knee flexion. From 80° to 100°, the average nearest medial point moved 2.8 mm posteriorly and reached 1.8 ± 2.8 mm at 100° of knee flexion (Fig. 3a).
Normal and varus alignment groups during flexion from the extended position (a–c) and during extension from the flexed position (d–f) under non-weight-bearing conditions. No significant difference was detected between normal and varus alignment during both flexion from the extended position (a–c) and extension from the flexed position (d–f) under non-weight-bearing conditions
At 0° of knee flexion, the average nearest lateral point of normal alignment group was −5.4 ± 2.9 mm. Under non-weight-bearing conditions from 0° to 50°, the average nearest lateral point remained constant. Subsequently, the nearest lateral point moved 4.6 mm posteriorly from 50° to 100° and reached −8.1 ± 4.1 mm at 100° of knee flexion (Fig. 3b).
The medial side initially moved 5.2 mm anteriorly from 0° to 80° of knee flexion, but then moved 2.8 mm posteriorly from 80° to 100°. The lateral side remained motionless from 0° to 50° of knee flexion and then moved 4.6 mm posteriorly from 50° to 100° (Fig. 3a, b).
With regard to the axial rotation of the femoral component relative to the tibial component, the mean axial rotation was 4.7° ± 4.1 at 0°, 3.9° ± 3.9° at 10°, and 10.7° ± 5.6° at 100° of knee flexion. The femoral component initially exhibited internal rotation from 0° to 10° and gradual external rotation from 10° to 100°, with mean axial rotation during the knee flexion cycle of 6.8° (Fig. 3c). All knees generally exhibited an external rotation pattern.
Under non-weight-bearing conditions from 100° to 0° of extension from the flexed position, the normal alignment group exhibited the same kinematics as under non-weight-bearing conditions from 0° to 100° of flexion from the extended position (Fig. 3d–f). The varus alignment group also exhibited the same kinematics as the normal alignment group, and no significant difference was detected between the two groups (Fig. 3a–f).
Discussion
The most important finding of the present study was that the kinematics were influenced by weight load (weigh-bearing condition) and the postoperative alignment. High weight loading induced a more posterior position. Under weight-bearing conditions, the varus alignment group showed a more posterior position of the medial condyle and a more anterior position of the lateral condyle than the normal alignment group. In contrast, no significant difference was detected between the normal and varus alignment groups under non-weight-bearing conditions.
Although many previous studies have reported that all TKAs have variable kinematic patterns that can be very different as compared to normal knees [1, 7, 9, 34, 35], no study has evaluated the difference at midflexion between varus and normal alignment kinematics. In our previous study, the PTS effect was evaluated [12]. A large PTS induced posterior placement of the medial femoral condyle under weight-bearing condition. The PTS did affect the postoperative in vivo kinematics through weight load.
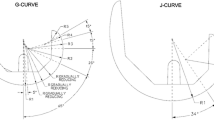
Here, we propose an explanation for this mechanism under weight-bearing conditions (Fig. 4). Standard gravity produces a posterior force on the femur through PTS and locates the femur posteriorly to some extent. A CR TKA does not contain an ACL, and therefore, the prosthesis cannot positively resist this posterior force, and the femur moves posteriorly to the equilibrium position (Fig. 4b). Regarding the medial condyle in varus alignment, large weight loading generates a large posterior force, and the femur is forced to locate posteriorly to maintain its equilibrium position (Fig. 4c). Regarding the lateral condyle in varus alignment, little weight loading generates little posterior force on the femur (Fig. 4a).
Posterior translation force on the femur generated by weight load and the posterior tibial slope. a A small weight load generates a small posterior force on the femur, and the femur is translated anteriorly relative to the tibia (The lateral condyle of the varus alignment group). b A standard weight load generates posterior force on the femur, and the femur is located in it normal position relative to the tibia. c A large weight load produces a large posterior force, and the femur is translated posteriorly relative to the tibia. (The medial condyle of the varus alignment group)
Recently, Howell suggested that a slight undercorrection of the deformity was beneficial from functional perspective [19], and Vanlommel reported better clinical and functional outcome score in postoperative mild varus with pre-operative varus knees [36]. We also kept the same idea in mind and started to study midresidual varus deformity with pre-operative varus knees. Screw-home movement was first clearly described by Hallen in 1966. Hallen stated that the medial (internal) rotation of the femur on the tibia on full extension stabilizes the joint [15]. In vivo kinematics on terminal extension from the flex position was also evaluated in this study. Our results revealed that varus alignment induced posterior displacement of the lateral femoral condyle on the tibia and led to external rotation of the femur on full extension. Although this rotation is in the opposite direction as screw-home movement, the lateral femoral condyle mobility might be physiological and lead to better functional condition around full extension.
There are some limitations to the current study. One limitation was that the component positions and rotations for the femoral and tibial bones were not taken into consideration. Only the angle between the femoral and tibial components was evaluated. It should be kept in mind that several degrees of difference exist between the component angle and the femoral–tibial shaft angle. Additional detail comparison about clinical outcome between varus and normal alignment groups was not carried out in this study. It is still unclear whether the greater mobility of the lateral femoral condyle will enhance the clinical and functional outcome. Further study is necessary for the direct explanation.
Conclusion
In conclusion, under weight-bearing conditions, both the medial and lateral condyles moved posteriorly as compared with the situation under non-weight-bearing conditions. Under weight-bearing conditions, the varus alignment group showed a more posterior position of the medial condyle and more anterior position of the lateral condyle compared to the normal alignment group. Under non-weight-bearing conditions, no significant difference was detected between the normal and varus alignment groups. In other words, weight load created a posterior shift in both the medial and lateral condyle positions. The weight load influenced knee kinematics through PTS, and greater lateral femoral condyle mobility might explain the better clinical and functional outcome. These findings contribute to gaining a proper understanding of the in vivo kinematics of the postoperative varus alignment and might be useful for orthopaedic surgeons in achieving patient satisfaction.
References
Banks SA, Markovich GD, Hodge WA (1997) In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplast 12(3):297–304
Bargren JH, Blaha JD, Freeman MA (1983) Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res 173:178–183
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84(1):50–53
Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13(3):193–196
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Chong DY, Hansen UN, Amis AA (2010) Analysis of bone-prosthesis interface micromotion for cementless tibial prosthesis fixation and the influence of loading conditions. J Biomech 43(6):1074–1080
Dennis DA, Komistek RD, Colwell CE Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 356:47–57
Dennis DA, Komistek RD, Mahfouz MR (2003) In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res 410:114–130
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Dennis DA, Mahfouz MR, Komistek RD, Hoff W (2005) In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38(2):241–253
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplast 24(6 Suppl):39–43
Fujimoto E, Sasashige Y, Tomita T, Iwamoto K, Masuda Y, Hisatome T (2013) Significant effect of the posterior tibial slope on the weight-bearing, midflexion in vivo kinematics after cruciate-retaining total knee arthroplasty. J Arthroplast. doi:10.1016/j.arth.2013.10.018
Green GV, Berend KR, Berend ME, Glisson RR, Vail TP (2002) The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: the posteromedial hot spot. J Arthroplast 17(8):1033–1039
Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, Bergmann G (2012) Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am 94(11):1023–1029
Hallen LG, Lindahl O (1966) The “screw-home” movement in the knee-joint. Acta Orthop Scand 37(1):97–106
Han HS, Chang CB, Seong SC, Lee S, Lee MC (2008) Evaluation of anatomic references for tibial sagittal alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16(4):373–377
Horiuchi H, Akizuki S, Tomita T, Sugamoto K, Yamazaki T, Shimizu N (2012) In vivo kinematic analysis of cruciate-retaining total knee arthroplasty during weight-bearing and non-weight-bearing deep knee bending. J Arthroplast 27(6):1196–1202
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21(10):2271–2280
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73(5):709–714
Kitagawa A, Tsumura N, Chin T, Gamada K, Banks SA, Kurosaka M (2010) In vivo comparison of knee kinematics before and after high-flexion posterior cruciate-retaining total knee arthroplasty. J Arthroplast 25(6):964–969
Komistek RD, Dennis DA, Mahfouz M (2003) In vivo fluoroscopic analysis of the normal human knee. Clin Orthop Relat Res 410:69–81
Komistek RD, Mahfouz MR, Bertin KC, Rosenberg A, Kennedy W (2008) In vivo determination of total knee arthroplasty kinematics: a multicenter analysis of an asymmetrical posterior cruciate retaining total knee arthroplasty. J Arthroplast 23(1):41–50
Liau JJ, Cheng CK, Huang CH, Lo WH (2002) The effect of malalignment on stresses in polyethylene component of total knee prostheses–a finite element analysis. Clin Biomech 17(2):140–146
Lotke PA, Ecker ML (1977) Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 59(1):77–79
Mahfouz MR, Komistek RD, Dennis DA, Hoff WA (2004) In vivo assessment of the kinematics in normal and anterior cruciate ligament-deficient knees. J Bone Joint Surg Am 86-A(Suppl 2):56–61
Massin P, Gournay A (2006) Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplast 21(6):889–896
Moreland JR (1988) Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res 226:49–64
Panel NIHC (2004) NIH Consensus Statement on total knee replacement December 8-10, 2003. J Bone Joint Surg Am 86(6):1328–1335
Ritter MA (2009) The Anatomical Graduated Component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg Br 91(6):745–749
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93(17):1588–1596
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Sikorski JM (2008) Alignment in total knee replacement. J Bone Joint Surg Br 90(9):1121–1127
Stiehl JB, Komistek RD, Dennis DA (1999) Detrimental kinematics of a flat on flat total condylar knee arthroplasty. Clin Orthop Relat Res 365:139–148
Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA (1995) Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 77(6):884–889
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21(10):2325–2330
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87(5):646–655
Wong J, Steklov N, Patil S, Flores-Hernandez C, Kester M, Colwell CW Jr, D’Lima DD (2011) Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J Orthop Res 29(3):347–353
Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Maeda D, Sato Y, Yoshikawa H, Tamura S (2005) Development of three-dimensional kinematic analysis system for artificial knee implants using X-ray fluoroscopic imaging. Nihon Hoshasen Gijutsu Gakkai Zasshi 61(1):79–87
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplast 20(6):777–783
Zuffi S, Leardini A, Catani F, Fantozzi S, Cappello A (1999) A model-based method for the reconstruction of total knee replacement kinematics. IEEE Trans Med Imaging 18(10):981–991
Acknowledgments
The authors would like to thank Kenji Iwami and Takeshi Fujii for their excellent assistance in the photographing.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujimoto, E., Sasashige, Y., Tomita, T. et al. Different femorotibial contact on the weight-bearing: midflexion between normal and varus aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23, 1720–1728 (2015). https://doi.org/10.1007/s00167-014-3194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3194-z