Abstract
Purpose
We report the six year implant survivorship, tibial component alignment and knee and limb function measured by the Oxford Knee Score and Western Ontario and McMaster Universities Osteoarthritis Index ((WOMAC) score after kinematically aligned total knee arthroplasty (TKA) and tested the hypothesis that varus alignment of the tibial component, knee, or limb does not adversely affect implant survival and function.
Methods
We prospectively followed 214 consecutive patients (219 knees) treated with a kinematically aligned TKA in 2007. Kaplan–Meier survival analysis and revision rate per 100 component years determined implant failure. The Oxford Knee Score (0 worst, 48 best) and WOMAC score (0 worst, 100 best) were used to measure function. We categorised tibial component alignment as in-range (≤ 0°) or varus (>0°), knee alignment as in-range (between -2.5° and -7.4°), varus (>-2.5°), or valgus (<-7.4°), and limb alignment as in-range (0° ± 3°), varus (>3°) or valgus (<-3°).
Results
At a mean of 6.3 years (range, 5.8–7.2), implant survivorship was 97.5 % and revision-rate per 100 component years 0.40. Three implants had been revised (deep infection one, loose tibial component one and patella instability [1); two loose patella components were pending revision and considered failures. The average Oxford Knee Score was 43 and WOMAC 91. Function of tibial components (80 %), knees (31 %) and limbs (7 %) that were aligned in varus was similar to patients aligned in-range.
Conclusions
At a mean of 6.3 years after kinematically aligned TKA, varus alignment of the tibial component, knee and limb did not adversely affect implant survival or function, which supports the consideration of kinematic alignment as an alternative to mechanical alignment for performing primary TKA.
Level of evidence, III; therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effects of alignment on implant survivorship and function after total knee arthroplasty (TKA) are of great interest to the surgeon and patient [1–3]. Varus malalignment is mentioned as a major risk factor for implant survivorship, postoperative pain and functional impairments [4–6]. This widespread opinion is based, in part, on historical data derived from implantations performed in the late 1970s and early 1980s with rudimentary implant designs (that is, the Denham knee) [4, 7, 8]. However, results from several studies that used more modern implants and placed the limb or tibial component in varus do not support the opinion that varus alignment adversely affects implant survivorship and function [4, 9, 10].
Kinematically aligned TKA is a new alignment technique with no reports of implant survivorship beyond three years [10]. A Level 1 randomised clinical trial showed that kinematically aligned TKA provided better pain relief, function scores and flexion than mechanically aligned TKA at two years [11]. Kinematic alignment corrects the arthritic deformity to the constitutional alignment of the patient with the intent of positioning the femoral and tibial components, restoring the natural tibial–femoral articular surface, alignment and natural laxities of the knee [11, 12]. However, aligning joint-line components with those of the normal knee also aligns the tibial component in varus, creating concern that varus alignment might result in poor function and early catastrophic failure. Accordingly, there is a need to determine whether varus alignment of the tibial component, knee and limb adversely affects implant survivorship and function at mid-term follow-up.
The purpose of this study was to analyse the six year implant survivorship, alignment of the tibial component, knee, and limb and assess function as measured by the Oxford Knee Score and WOMAC score after kinematically aligned TKA. We also tested the hypothesis that varus alignment of the tibial component, knee or limb does not adversely affect survival and function.
Materials and methods
We prospectively followed 228 consecutive patients treated with 233 primary TKAs with kinematic alignment between January and December 2007 (Table 1). Indications were: (1) disabling knee pain and functional loss unresolved with nonoperative treatment modalities; (2) radiographic evidence of Kellgren-–Lawrence grade 3 or 4 arthritic change or osteonecrosis; (3) and any severity of varus or valgus deformity. We excluded one patient with rheumatoid arthritis, one who became paraplegic from transverse myelitis, one whose knee was mechanically aligned because the wrong patient-specific guide was delivered for surgery, one with a giant-cell tumor of the tibia and ten with a workers’ compensation claim, because they are known to have lower function scores than patients without claims [13]. An institutional review board approved the analysis.
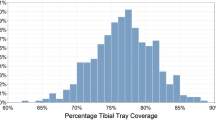
The study cohort consisted of 214 patients (219 knees) with an average age of 68 years (range, 39-93) (Table 2). There were more women (133) than men (81) men, and average body mass index (BMI) for both sexes was 31 kg/m2 (range, 14–49) at the time of surgery. Pre-operative knee diagnoses were degenerative osteoarthritis, 193 knees (88 %), traumatic osteoarthritis, 24 knees (11 %) and osteonecrosis, two knees (1 %). Pre-operative knee alignment was measured from a standing radiograph of the knee and ranged from 34° (-20°) valgus to 14° varus (Fig. 1). Median time to follow-up was 6.3 years (range, 5.8–7.2).
Change between pre-operative and postoperative knee alignment measured on standing radiograph and supine scanogram of the limb. Postoperative knee alignment range (11°) was three times less than pre-operative alignment (34°), which shows the degree of correction achieved with kinematically aligned total knee arthroplasty (TKA). Ellipse covers 99 % of points that represent knee alignment; 114 × 101 mm (300 × 300 DPI)
The lead author (SMH) performed all kinematically aligned TKAs using patient-specific femoral and tibial cutting guides (OtisMed, Alameda, CA, USA), a cemented cruciate-retaining component (Vanguard; Biomet, Inc, Warsaw, IN, USA) and a previously described technique [11, 10, 14, 15]. The basic concept of kinematically aligned TKA is scientifically supported and is not controlled by the US Food and Drug Administration (FDA) or regulatory agencies in other countries [11, 12, 16]. Kinematically aligned TKA is currently performed with manual instruments, which achieves accurate alignment and restores high function [12]. Kinematically aligned TKA can no longer be performed with patient-specific guides, as they are no longer being manufactured. Varus and valgus deformities and flexion contractures were corrected, and the knee was balanced by positioning the bone cuts so the components restored the natural tibial–femoral articular surface without releasing collateral, posterior cruciate or retinacular ligaments [17, 10, 12]. Knee balance and patellar tracking were determined qualitatively by manual and visual examination. The patella was resurfaced. All components were cemented. On the day of discharge, an anteroposterior rotationally controlled long-leg computed tomograph (CT) scanogram of the limb was obtained with the patient supine and non-weight bearing, using a previously described technique [18, 19].
One of the two observers (SP, LRG), blinded to alignment, contacted patients independently of the treating surgeon between October 2013 and March 2014. Whether the patient had further surgery on the knee for any reason, including stiffness, instability, wear, component loosening, fracture, infection and haematoma drainage was recorded, and the operative note was obtained. The source for determining a re-operation on the 203 patients (208 knees) was the patient (n = 178), a family member because the patient was deceased (n = 20) or a family member because the patient was mentally incompetent due to stroke or dementia (n = 5). Mentally competent patients without re-operation and alive at the 6-year follow-up (173; 178 knees) completed the Oxford Knee Score (48 best, 0 worst) and WOMAC questionnaires (100 best, 0 worst).
One observer (KK), blinded to re-operation status and function scores, measured and categorised coronal alignment of the limb, knee and tibial component in 195 patients (200 knees) independent of the treating surgeon using a previously described technique [20, 15, 19]. Alignment of the tibial component was the angle between the joint line of the tibial component and the mechanical axis of the tibia; knee alignment was the angle between the anatomic axes of the femur and tibia; limb alignment was the angle between the mechanical axes of the femur and tibia [8, 5]. We categorised tibial component alignment as in-range (≤ 0°) or varus (>0°) [5]; knee alignment as in-range (between -2.5° and -7.4°), varus (>-2.5°) or valgus (<-7.4°) [5]; and limb alignment as in-range (0° ± 3°), varus (>3°) or valgus (<-3°) [8]. Interclass coefficients for the methods of measuring limb (0.86) and knee (0.87) alignment indicate good reproducibility [19].
Statistical analysis
Pre-operative clinical characteristics, motion, varus–valgus deformity measured on a standing radiograph and function scores were expressed as mean, standard deviation (SD), and 95 % confidence interval (CI) (Table 2). Kaplan–Meier survival analysis of time to failure was performed, including any pending revisions, defined as failure with four endpoints:
1. Revision for any reason
2. Revision for any reason other than infection
3. Revision for tibial collapse
4. Revision due to instability, including patella
Censoring occurred at the date of the last clinical examination, date of death, or date on which implant failure was determined. Implant survival was computed as the rate of revision per 100 component years. This is equivalent to the yearly rate of revision expressed as a percentage and is calculated by dividing the number of implants revised by the observed component years multiplied by 100 [21]. The exact 95 % CI of the revision rate per 100 component years, the overall Oxford Knee Score and the overall WOMAC score were computed. A single-factor, completely randomised analysis of variance (ANOVA) determined whether there were differences in mean scores between patients grouped by in-range, varus and valgus alignment of the tibial component, knee and limb.
Results
Regarding implant survivorship, re-operation data were available for 208 knees (95 %). At 6 years, implant survivorship was 97.5 % when the endpoint was revision for any reason and per 100 component years was 0.40 (95 % CI 0.18–0.93) (Fig. 2). Three implants were revised for, respectively, deep infection, loose tibial component and patella instability; two loose patella components were pending revision (Table 3) (Fig. 3).
Alignment on computer tomography (CT) scanogram or radiograph of the pertinent projections of failure due to tibial loosening (1A–C), revision due to patella instability (2A–C), one pending revisions due to loose patella component. Tibial loosening may have been associated with tibial component placement in reverse slope due to a poor-fitting tibial component (1B). Revision for patellar instability may have been associated with a difficult-to-treat bilateral congenital lateral patellar instability (2C). Patellar loosening may have been associated with flexed femoral component due to poor-fitting femoral guide (3C). The final case of patellar loosening may have been associated with an overly thin patella remaining after resection (not shown). None of these patients had malalignment of the limb (hip–knee–ankle angle) in the coronal projection (1A, 2A, 3A). Hence, these failures are not associated with the principle of kinematic alignment and are associated with multiple factors that should be preventable with use of manual instruments instead of patient-specific guides; 203 × 101 mm (300 × 300 DPI)
For alignment measurements, a long-leg scanogram of the lower limb was available for 195 patients (200 knees) (Table 1): 80 % of tibial components, 31 % of knees and 7 % of limbs were varus. Tibial component alignment ranged from -7° valgus to 7° varus (mean 1.9° varus, 95 % CI 1.6–2.3°); knee alignment ranged from -9° valgus to 2° varus (mean -3.6° varus, 95 % CI -3.3° to -3.8°); limb alignment ranged from -10° valgus to 8.5° varus (mean -0.8° varus, 95 % CI -0.4° to -1.1°); preoperative knee alignment of 34° (-20° valgus to 14° varus) was corrected to a postoperative knee alignment of 11° (-9° valgus to 2° varus) (Fig. 1).
Function scores were available for 178 knees (81 %) (Table 1). At 6 years, the overall Oxford Knee Score averaged 42.7 (95 % CI 41.6–43.7) and the overall WOMAC score 91.1 (95 % CI 89.0–93.1).
In regards to the effect of alignment category on function, both a long-leg scanogram of the lower limb and a six year function score were available for 175 knees (80 %) (Table 1). Mean Oxford Knee and WOMAC scores were no different for patients grouped as varus, valgus or in-range according to tibial component, knee, limb alignment (Table 4).
Discussion
The most important findings of this study were that kinematically aligned TKA had an acceptable implant survivorship, high average function and varus alignment of the tibial component, knee and limb that did not adversely affect implant survival or function at a mean follow-up of 6.3 years.
Three limitations should be discussed before interpreting the findings of our study. Firstly, these results, of a designer surgeon’s case series, require independent confirmation because designing surgeons tend to report lower failure rates and higher function, which might not be reproducible and applicable to the typical surgeon [22]. However, the study’s 25-point improvement from pre-operative function to an average Oxford Knee Score of 43 at 6 years has been reproduced by nondesigning surgeons, who reported a comparable 20-point improvement from pre-operative function to an average Oxford Knee Score of 40 at 2 years [11]. Secondly, the lack of follow-up of 5 % of patients (11 patients, 11 knees) might have positively biased implant survivorship if some of these patients had revision surgery and were omitted from the revision-rate computation. Such bias would be more likely if these patients were contactable and refused to participate; however, a comprehensive search failed to retrieve reliable contact information from their last listed primary care physician, hospital admission records and multiple people-search websites. The final limitation is that imaging studies were not part of the final follow-up, so we are unable to report on the location and extent of radiolucent lines that indicate reduced implant–bone contact and are suggestive of an implant at risk for loosening.
Our implant survivorship of 97.5 % and revision rate per 100 component years of 0.40 (95 % CI 0.18–0.93) after a mean of 6.3 years for kinematically aligned TKA are comparable with those of mechanically aligned TKA of 0.64 (95 % CI 0.44–1.19) reported by a knee arthroplasty registry for the same implant design at six years (Table 3) [23]. Although patient population, follow-up and methodology of our study and the arthroplasty registry are different, comparable implant survivorship and revision rate suggests that kinematically aligned TKA does not fail prematurely at a mean of 6.3 years’ follow-up.
Three reasons explain why a kinematically aligned TKA that restores the natural constitutional alignment of the limb and knee resulted in an acceptable implant survival and revision rate per 100 component years at a mean of 6.3 years, even though 80 % of tibial components, 31 % of knees and 3 % of limbs were categorised as varus: (1) Kinematically aligned TKA avoids the wide range of collateral ligament imbalances that are complex, cumulative and not correctable by collateral ligament release, and the wide range of change in the natural alignment of the limb and knee, which are caused by mechanically aligned TKA. The -9° valgus to 2° varus range of knee alignment of the kinematically aligned TKAs is comparable with the -9° valgus to 0° varus range of the natural knee alignment, which indicates an average correction of the constitutional alignment [24]. (2) Kinematically aligned TKA that restores constitutional alignment of the limb and joint line of the knee has more physiological strain in collateral ligaments than does mechanically aligned TKA that is unnaturally aligned to a neutral mechanical alignment [25]. (3) There is new evidence suggesting that primary osteoarthritis is not caused by the patient’s constitutional alignment, which would suggest that restoring this alignment does not predispose the implant to premature failure. The primary cause of osteoarthritis is hypothesised to be adverse changes in cartilage metabolism associated with aging and obesity. Articular cartilage is a mechanosensitive tissue that, when healthy, increases anabolic activity and thickens when loaded. Chondrocytes experience age-related declines in their anabolic activity and thickening response and cause osteoarthritis because of gradual loss of the ability to respond and compensate for high loads from activity and obesity [26]. Clinical findings of bilateral osteoarthritis with a varus deformity in one knee and a valgus deformity in the other (wind-swept), lack of osteoarthritis in the majority of elderly Asian patients with severe constitutional varus, and the report that patients with pre-operative varus have better clinical outcome and function scores and no revisions when alignment is left in mild constitutional varus—compared with patients with alignment correction to neutral—at a mean follow-up of 7.2 years, support the indication that adverse change in cartilage metabolism is the primary cause of osteoarthritis [9].
Finally, the high function scores reported in this study are comparable with a Level 1 randomised clinical trial. That trial reported that the kinematically aligned group had a 7-point better Oxford Knee Score, 26-point better WOMAC score, 8° better flexion and 1.7 higher odds ratio of having a pain-free knee at 2 years’ follow-up [11]. Similarly, the average Oxford Knee Score of 43 (95 % CI 41.6—43.7) at 6 years in the study reported here is 10 points higher than the average of 33 (95 % CI 31.9–33.4) reported for a case series of mechanically aligned TKA at 6 years [27]. Although patient population, follow-up and methodology of our study and the case series of mechanically aligned TKA are different, our study and the Level 1 randomised clinical trial of kinematically aligned TKA report encouraging functional and clinical results.
In summary, the acceptable implant survivorship and correction of knee alignment associated with a varus alignment of the tibial component and/or knee, and the high patient function at a mean follow-up of 6.3 years, support the consideration of kinematic alignment as an alternative to mechanical alignment for performing primary TKA.
References
Maderbacher G, Schaumburger J, Keshmiri A, Barthel M, Springorum HR, Craiovan B, Grifka J, Baier C (2014) Pinless navigation in total knee arthroplasty: Navigation reduced by the maximum? International orthopaedics:1–6. doi:10.1007/s00264-014-2529-1
Iorio R, Mazza D, Drogo P, Bolle G, Conteduca F, Redler A, Valeo L, Conteduca J, Ferretti A (2014) Clinical and radiographic outcomes of an accelerometer-based system for the tibial resection in total knee arthroplasty. International orthopaedics:1–6. doi:10.1007/s00264-014-2541-5
Manzotti A, Cerveri P, Pullen C, Confalonieri N (2014) Computer-assisted unicompartmental knee arthroplasty using dedicated software versus a conventional technique. Int Orthop 38(2):457–463. doi:10.1007/s00264-013-2215-8
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130(12):1487–1491. doi:10.1007/s00402-010-1064-9
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) the effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93-A(17):1588–1596
Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, Meding JB (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95(2):126–131. doi:10.2106/JBJS.K.00607
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg British 73(5):709–714
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92(12):2143–2149. doi:10.2106/JBJS.I.01398
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc:1–6. doi:10.1007/s00167-013-2481-4
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007. doi:10.1007/s11999-012-2613-z
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 96-B(7):907–913. doi:10.1302/0301-620X.96B7.32812
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21(10):2271–2280. doi:10.1007/s00167-013-2621-x
de Beer J, Petruccelli D, Gandhi R, Winemaker M (2005) Primary total knee arthroplasty in patients receiving workers’ compensation benefits. Can J Surg 48(2):100–105
Howell SM, Hull ML (2012) Principles of kinematic alignment in total knee arthroplasty with and without patient specific cutting blocks (OtisKnee). In: Scott S (ed) Insall and Scott surgery of the knee, vol 1, 5th edn. Elsevier, Philadelphia, pp 1255–1268
Howell SM, Kuznik K, Hull ML, Siston RA (2008) Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 31(9):857–863
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 96-B(11 Supple A):96–100. doi:10.1302/0301-620X.96B11.34152
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2012) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc:1–7. doi:10.1007/s00167-012-2220-2
Howell SM, Kuznik K, Hull ML, Siston RA (2010) Longitudinal shapes of the tibia and femur are unrelated and variable. Clin Orthop Relat Res 468(4):1142–1148. doi:10.1007/s11999-009-0984-6
Nunley R, Ellison B, Zhu J, Ruh E, Howell S, Barrack R (2012) Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res 470(3):895–902. doi:10.1007/s11999-011-2222-2
Dossett H, Swartz G, Estrada N, Lefevre G, Kwasman B (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):160–169
Pearse AJ, Hooper GJ, Rothwell A, Frampton C (2010) Survival and functional outcome after revision of a unicompartmental to a total knee replacement: the New Zealand National Joint Registry. J Bone Joint Surg British 92(4):508–512. doi:10.1302/0301-620X.92B4.22659
Labek G, Neumann D, Agreiter M, Schuh R, Böhler N (2011) Impact of implant developers on published outcome and reproducibility of cohort-based clinical studies in arthroplasty. J Bone Joint Surg Am 93(Supplement_3):55–61. doi:10.2106/jbjs.k.01108
The New Zealand Joint Registry 14 Year Report: January 1999 to December 2012 (2013)
Gu Y, Roth JD, Howell SM, Hull ML (2014) How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? J Bone Joint Surg Am 96(12):e101
Delport H, Labey L, Innocenti B, De Corte R, Vander Sloten J, Bellemans J (2014) Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc:1–11. doi:10.1007/s00167-014-2971-z
Blazek K, Favre J, Asay J, Erhart-Hledik J, Andriacchi T (2014) Age and obesity alter the relationship between femoral articular cartilage thickness and ambulatory loads in individuals without osteoarthritis. J Orthop Res 32(3):394–402. doi:10.1002/jor.22530
Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE (2013) Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J 95-B(1):45–51. doi:10.1302/0301-620X.95B1.28573
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Howell, S.M., Papadopoulos, S., Kuznik, K. et al. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty?. International Orthopaedics (SICOT) 39, 2117–2124 (2015). https://doi.org/10.1007/s00264-015-2743-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2743-5