Abstract
Purpose
Aim of this study was to record and compare the functional and activity level as well as the manifestations of osteoarthritis after isolated ACL ruptures between patients with conservative treatment and ACL reconstruction with hamstrings tendon graft.
Methods
Thirty-two patients diagnosed with ACL rupture were recorded. Clinical examination included the Tegner and Lysholm activity scale, the International Knee Documentation Committee Subjective Form and KT-1000 arthrometer. Narrowing of the medial and lateral joint spaces was assessed using the IKDC knee examination score.
Results
Median follow-up was 10.3 years (range 10–11). Fifteen patients were conservatively treated (median age 33 years, range 25–39). Seventeen patients were operated (median age 31 years, range 20–36). There was significant difference between the mean values of IKDC scores in favour of the ACL-reconstruction group of patients, 86.8 (SD 6.5) versus 77.5 (SD 13.8), respectively (p = 0.04). The mean value of anteroposterior tibial translation was 1.5 mm (SD 0.2) for ACL-reconstruction group of patients, while the corresponding mean value for ACL-conservative group was 4.5 mm (SD 0.5), p = 0.03. Four patients in ACL-reconstruction group had radiological findings of grade C or D according to IKDC form. In ACL-conservative group, five patients presented similar signs (n.s.).
Conclusions
ACL reconstruction using hamstrings autograft resulted in better functional outcome and laxity measurements than ACL-conservative management. However, the incidence of radiological osteoarthritis was similar between the two groups and independent on the pre-operative grade of laxity and functional status of the patients. Equally, bone bruises were not found as a risk factor for the development of osteoarthritis after ACL rupture.
Level of evidence
Prospective randomized study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) is an important ligament for proper knee function, and a rupture of this structure can be a debilitating musculoskeletal injury, especially for the young athletes. Treatment depends on the previous activity level, characteristics of the injury and degree of the instability. Low-demand patients with partial tears and no symptoms of instability can restore their knee function following a non-surgical management with progressive physical therapy and rehabilitation [3]. However, complete ACL ruptures have a much less favourable outcome, and surgery is considered to be the ideal treatment [6].
Although a successful ACL reconstruction provides an adequate stability, its long-term effect on the articular cartilage has not yet been clarified [19]. The prevalence of radiographic knee osteoarthritis (OA) has been reported to range between 40 and 70 % after an ACL injury [21, 37]. This percentage becomes higher (80–85 %) when the ACL reconstruction is combined with meniscectomy [29]. A previous review of the literature reported that ACL reconstruction does not reduce the incidence of further osteoarthritis and concluded that whatever the treatment, surgical or conservative, the risk of knee degeneration remains high [7]. Another study have supported that a younger age at the time of ACL reconstruction can be a significant risk factor in developing radiographically visible osteoarthritic changes in the operated knee [24].
In contrast, Roemer reported that a higher age in combination with the athlete status and a previous ACL surgery could strongly increase the risk of radiographic osteoarthritis [32]. Comparison between the conservative and surgical ACL treatment using a bone–patellar tendon–bone (BPTB) graft has been reported by several studies, but the results are still on debate regarding the functional outcome, activity level and osteoarthritis incidence [9, 10, 16, 27]. However, a recent meta-analysis of prospective trials revealed that ACL reconstruction with BPTB autografts resulted in increased anterior knee pain and incidence of OA compared with hamstring autografts although the functional outcomes were not significantly different [40].
The purpose of this prospective study was to evaluate the treatment outcome and clarify the manifestations of osteoarthritis comparing isolated ACL ruptures either treated with conservative methods or with hamstrings tendon graft. Our hypothesis was that the ACL reconstruction could result in better functional outcome than the conservative treatment, but the impact on osteoarthritis risk would be indifferent for both treatment methods.
Materials and methods
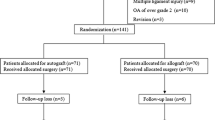
Thirty-two patients diagnosed with ACL rupture were evaluated. Inclusion criteria for the study were patients with isolated ACL injuries, a body mass index of <30, no previous major injury or surgery of the knee and patients who successfully completed the final follow-up. Exclusion criteria were patients having combined ACL injuries, a body mass index of >30 and those having prior knee surgery. The patients were randomly dispersed to one of the two treatment options by the use of sealed envelopes containing cards, indicating the treatment for each patient.
Demographical data, any medication uptake and comorbidities were recorded. Operations were performed by the same orthopaedic surgeon specialized in knee surgery. Pre-operative and follow-up examinations were performed by an independent consultant knee surgeon. Clinical examination and functional status evaluation included the Tegner and Lysholm activity scale and the 2000 Revised International Knee Documentation Committee (IKDC) Subjective Form, while quantitative laxity testing was performed with a KT-1000 arthrometer (MED-metric, San Diego, CA). Three anterior forces of 67, 89 and 134 Newton were successively applied as well as a manual maximum anterior displacement was performed. However, the value of 134 N was used in the analysis to decrease the bias. Tests were also repeated on the uninvolved extremity to determine normal values. Narrowing of the medial and lateral joint spaces was assessed using the IKDC knee examination score performing double-leg postero-anterior weight-bearing roentgenogram at 35°–45° of knee flexion. The contralateral normal knee was used as a control. Radiological evaluation was made by a blinded consultant specialized in musculoskeletal radiology. Any perioperative complication was also recorded. Magnetic resonance imaging (MRI) was performed pre- and post-operatively in all the patients to evaluate any concomitant injury (meniscal, cartilage, bone bruises).
The median time interval between the initial injury and the beginning of treatment was 6 weeks (range 4–8) for both the ACL-reconstruction and ACL-conservative groups. ACL reconstruction was performed via an arthroscopic technique by use of four-stranded semitendinosus–gracilis tendon autografts. The anteromedial portal was used to create femoral tunnels. The grafts were fixed in the femoral side by use of a suspensory device (Endobutton, Acufex; Smith and Nephew Endoscopy, Andover and Mansfield, Oklahoma, USA). Bioabsorbable screws were used for the fixation of the grafts in the tibial tunnel. Post-fixation was made every time using screws or staples.
All the patients participated in the same rehabilitation programme. Passive knee motions started immediately after surgery, while partial weight-bearing was permitted for the first 6 weeks. A full-time knee extension brace was ordered for all cases for the same period. Stationary bike, proprioception exercises, short arc quadriceps sets and hamstring curls were performed for the next 6 weeks. At the third post-operative month, jogging, swimming in straight line and bicycle were started. At the sixth post-operative month, pivot sports such as ski, tennis and squash were started, while contact sports were permitted at the eighth–ninth post-operative month.
The study was approved by the scientific board after obtaining the informed consent from all the patients. No specific institutional review board (IRB) form and identification number were necessary according to the current policy of the institution.
Statistical analysis
Quantitative data were recorded and statistically analysed using the Student’s t test for unpaired and paired samples. Qualitative data were analysed using the Pearson Chi-square and Fisher’s exact tests. Significance levels were set at p < 0.05 with confidence intervals at 95 %. All tests were calculated using the SPSS Inc. Data Access Pack for Windows, version 17.0.1 (IBM, Chicago III).
The demographical data, follow-up, time interval between the initial injury and the surgical treatment as well as the Tegner scale scores were measured using median (range) values. Measurements with KT-1000, IKDC, were performed using mean (standard deviation) values. Calculations were rounded to the nearest millimetre.
Results
Median follow-up was 10.1 years (range 10–11 years). All the patients were males. Fifteen patients (47 %) with a median age of 33 years (range 25–39 years) were conservatively treated. Seventeen patients (53 %) with a median age of 31 years (range 20–36 years) were operated. According to IKDC scores, ACL-reconstruction group of patients presented better clinical and functional outcomes as compared to ACL-conservative group. There was significant difference (p = 0.04) between the mean values of IKDC scores (86.7, SD 6.5 vs. 77.5, SD 13, respectively) as depicted in Fig. 1. The same was found comparing laxity measurements using KT-1000 arthrometer. The mean value of anteroposterior tibial translation with a 134 N applied force was 1.5 mm (SD 0.2) for ACL-reconstruction group of patients, while the corresponding mean value for ACL-conservative group was 4.5 mm (SD 0.5), (p = 0.03).
All the patients presented signs of cartilage degeneration at the final follow-up (Table 1). Four out of 17 patients (23.5 %) in ACL-reconstruction group had radiological findings of grade C or D according to IKDC examination form. No correlation was found between osteoarthritis and age (r = 0.65 for <30 years and r = 0.7 for >30 years patients, n.s.). In ACL-conservative group, five of 15 patients (33.3 %) presented similar signs. Also, no correlation was found between osteoarthritis and age (r = 0.75 for <30 years and r = 0.8 for >30 years patients, n.s.). No difference in the overall incidence of osteoarthritis was observed between the two groups (n.s.). In addition, there was no correlation between radiological findings and pain scores in both groups (r = 0.7 for ACL-reconstruction group and r = 0.8 for ACL-conservative group, n.s.).
No complications occurred and no revision surgeries were performed. No patients required any further meniscus surgery or surgery due to persistent instability. All the patients returned to their previous activities, although they did not fully restore the pre-injury level (Table 2).
Discussion
The most important finding of this prospective study was that the ACL reconstruction using hamstrings autograft could give better functional outcome and laxity measurements than the conservative treatment in male athletes having an isolated ACL rupture between the third and fourth decade of life. However, the long-term incidence of radiological osteoarthritic findings remains the same for both treatment methods despite the good integrity of the menisci and cartilage of the knee joint.
ACL deficiency is a well-recognized risk factor for the development of knee osteoarthritis and the incidence of cartilage degeneration after ACL rupture ranges from 16 to 70 % [21]. This percentage can be even higher if the initial injury is associated with meniscal and cartilage lesions or when a partial meniscectomy is performed [30]. Following a rupture of the ACL, several parameters such as the mechanical instability, hematoma, subchondral bone and marrow lesions and the inflammatory response mechanisms with the production of chemokines can have detrimental effects on chondrocytes [8, 20, 22]. Other potential risk factors for the degeneration of the cartilage have been reported including the body mass index, age, activity level and the quadriceps muscle activation [13, 17, 25]. Mansson et al. [24] have recently suggested that the adolescents with a ruptured ACL could have important radiographically visible osteoarthritic changes in their operated knee independently on the graft used to reconstruct the ligament. Accordingly, Roemer in his cross-sectional case–control study showed that the activity level of an athlete as well as any previous surgery could increase the risk of the osteoarthritis. Contrary to Mansson, he suggested that a higher age (32–36 years old) can be a strong risk factor for the degeneration of the knee [32].
In the present study, the pre-operative MRI revealed bone bruises in all the injured knees, but no concomitant meniscal or chondral lesions were noticed. All the patients had a reasonable body mass index, and they followed the same rehabilitation programme after the surgery. From the clinical point of view, the analysis of the functional scores showed a statistically significant difference in favour of the patients who followed the reconstructive treatment regimen; however, there was no difference regarding the radiological osteoarthritic changes, and no correlation was found between the radiological findings and pain scores. In addition, the age of the patients was not proved to have a correlation with an increased risk of osteoarthritis at 10-year follow-up. These results are definitely encouraging, although it seems necessary to prolong our follow-up in order to better understand the evolution of these injuries. This is supported in the interesting study of Nebelung and Wuschech who showed that the high-level athletes with definitive unstable knees have an increased risk of developing further meniscal and cartilage lesions over a 20-year period and they can become strong candidates of having a future total knee replacement [28].
Other studies have revealed an increasing frequency of radiographic osteoarthritic signs in patients with an untreated ACL rupture, especially when a previous meniscectomy was performed. Sherman et al. [34] reported that chronic anterior instability can lead to knee degeneration and progressive functional deterioration, which is strongly correlated with the cartilage degenerative changes. Neyret et al. reviewed 195 knees in 167 patients after a rim-preserving meniscectomy. All the patients with an ACL-deficient knee presented worse functional results and greater reoperation rate than those with an ACL-intact knee. Authors stated that the majority of ACL-deficient patients will develop osteoarthritis and concluded that the long-term outcome of a partial meniscectomy depends on the consistency of the ACL [29].
On the other hand and despite its advantages on the biomechanics of the knee [31, 35], ACL reconstruction has not proven to prevent cartilage degeneration [1, 4, 26]. Fink et al. evaluated the clinical outcome of operative versus non-operative treatment of ACL deficiency, and they showed that the risk of the knee joint degeneration was similar to both the operative and the non-operative groups. A significant correlation between the high-risk pivoting sports and osteoarthritis was found for the non-operative group, and the authors mentioned activity level as an important variable affecting the treatment outcome [9].
Furthermore, Fithian et al. classified their patients according to the pre-injury sports participation and knee laxity measurements. They found that reconstruction did not prevent the appearance of late degenerative changes on radiographs and reported no difference in relationship between the bone contusion on initial magnetic resonance images and the finding of degenerative changes [10].
A recent randomized trial found no radiographic differences among patients with early ACL reconstruction, delayed ACL reconstruction or no ACL reconstruction (rehabilitation alone) after a follow-up of 5 years [11]. Similarly, the systematic review performed by Luc et al. [23] showed no evidence that ACL reconstruction is an adequate intervention to prevent knee osteoarthritis.
Equally, no correlation was observed between the pre-operative grade of laxity, functional status and osteoarthritic radiological findings in the present study. The classification of the cartilage degeneration was performed using the IKDC scale, which was recently proved to have the most favourable combination of reliability and correlation with arthroscopic findings [38]. Each compartment was separately analysed aiming to depict the degenerative lesions in a more detailed fashion (Table 1). Moreover, bone marrow lesions did not prove to be an independent risk factor for osteoarthritic degeneration. All the patients had bone bruises, but only 50 % of them suffered from osteoarthritis in each group. Confirming the initial hypothesis, the ACL reconstruction with hamstrings resulted in a better clinical outcome than the ACL-conservative management, but the incidence of further cartilage damage was similar in both groups.
The role of the graft in the development of osteoarthritis is still under debate. Cohen et al. reviewed 62 patients with ACL–patellar tendon graft reconstruction from 10- to 15-year follow-up. All the patients had a concomitant meniscectomy, and a statistically significant association was found between meniscal pathology and arthritis of the knee [5].
Struewer et al. evaluated 73 patients with an isolated ACL rupture and reconstruction with a BPTB autograft. Radiological assessment reported degenerative changes of grade II in 54.2 % of patients and grades III or IV in 20 % of patients using the Kellgren–Lawrence scale. The incidence of higher degree of osteoarthritis was significantly correlated with stability and function at long-term follow-up [36].
Leys et al. have prospectively investigated the results of isolated ACL reconstruction comparing four-strand hamstring tendon and patellar tendon grafts. The group of patients with hamstrings graft presented better clinical outcome and lower rate of radiological osteoarthritis [18]. Similar studies have reported on radiological findings in isolated ACL ruptures reconstruction after a follow-up of ≥10 years and showed that the incidence of osteoarthritis can range from 5 to 20 % independently on the type of the graft [12, 14, 15, 33, 39].
In a systematic review, the conservative treatment and surgical treatment of ACL tears were compared. According to the authors, no evidence-based arguments were found to justify a systematic surgical reconstruction to any patient with a torn ligament. Moreover, it was not proved that the ACL reconstruction can prevent osteoarthritis which must be attributed to a combination of factors that could act independently on the chosen treatment of ACL-deficient knee [7]. On the other hand, Bourke et al. showed good results and a small percentage of osteoarthritis 15 years post-operatively in patients with isolated ACL injuries. They stated that the hamstring tendons are a reliable graft and can provide a satisfactory long-term outcome if the reconstruction is performed with a correct and accurate technique [2]. Most recently, a meta-analysis performed by Chinese authors has included over a thousand patients. It was revealed that ACL reconstruction with BPTB autografts can result in an increased incidence of anterior knee pain and osteoarthritis at a minimum of 5 years as compared with the ACL reconstruction using hamstrings [40].
Based on the presented results, this study can be very useful in daily clinical practice. Dealing with a male, relatively young patient who suffers from an isolated ACL rupture, a clear proposal for an ACL reconstruction should be made, because it can provide better long-term functional outcomes. Definitely, whether to choose the surgical or conservative treatment is also depended on the patient (expectations, subjective symptoms, cost). However, all these patients should be informed that whatever is the treatment option, the incidence of developing a future osteoarthritis will be similar and independent on the good integrity of their menisci and cartilage. Moreover, it must be notified that problems with the patellofemoral joint could happen even if the choice of the graft would be the hamstring tendons (Table 1).
Certain limitations have to be considered in the herein report including the small number of cases evaluated (type II statistical error) and the inclusion of male subjects only. However, this is one of the few prospective studies in the literature comparing the evolution of osteoarthritic changes in ACL–hamstrings reconstructed and ACL-deficient conservatively treated knees. Other strengths of this study include the long follow-up and the consistency of the surgical technique as one surgeon performed all the procedures. Moreover, the sample was homogenous since all the patients presented with similar profile and characteristics considering the possible risk factors for osteoarthritis. Another strength can also be considered the fact that the assessment of the knee osteoarthritis was based on the report of a senior radiologist being independent from the surgical team. Moreover, all the patients completed the final examination, which was supplemented by the clinical findings and the subjective reported outcome.
Conclusions
ACL reconstruction using hamstrings autograft resulted in better functional outcome and laxity measurements than ACL-conservative management. However, the incidence of radiological osteoarthritis was similar between the two groups and independent on the pre-operative grade of laxity and functional status of the patients. Equally, bone bruises were not found as a risk factor for the development of osteoarthritis after ACL rupture.
References
Ageberg E, Thomee´ R, Neeter C, Silbernagel KG, Roos EM (2008) Muscle strength and functional performance in patients with ACL injury treated with training and surgical reconstruction or training only: a two to five-year follow-up. Arthritis Rheum 59:1773–1779
Bourke HE, Gordon DJ, Salmon LJ, Waller A, Linklater J, Pinczewski LA (2012) The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for ‘isolated’ anterior cruciate ligament rupture. J Bone Joint Surg Br 94:630–637
Buss DD, Min R, Skyhar M, Galinat B, Warren RF, Wickiewicz TL (1995) Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med 23:160–165
Casteleyn PP, Handelberg F (1996) Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg 78-B:446–451
Cohen M, Tarouco Amaro J, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23:629–634
Delay BS, Smolinski RJ, Wind WM, Bowman DS (2001) Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg 14:85–91
Delincé P, Ghafil D (2012) Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20:48–61
Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ (1999) Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med 27:489–494
Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP (2001) Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture—Is sports activity a determining variable? Int J Sports Med 22:304–309
Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM (2005) Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament injured knee. Am J Sports Med 33:335–346
Harris K, Driban JB, Sitler MR, Cattano NM, Hootman JM (2014) Five-year clinical outcomes of a randomized trial of anterior cruciate ligament treatment strategies: an evidence-based practice paper. J Athl Train 50:110–112
Hart AJ, Buscombe J, Malone A, Dowd GS (2005) Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br 87:1483–1487
Hart JM, Turman KA, Diduch DR, Hart JA, Miller MD (2011) Quadriceps muscle activation and radiographic osteoarthritis following ACL revision. Knee Surg Sports Traumatol Arthrosc 19:634–640
Hoffelner T, Resch H, Moroder P, Atzwanger J, Wiplinger M, Hitzl W, Tauber M (2012) No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy 28:517–525
Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA (2011) Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med 39:89–98
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture:11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16:442–448
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft. A minimum 10-year follow-up. Am J Sports Med 36:1275–1282
Leys T, Salmon L, Waller A, Linklater J, Pinczewski L (2012) Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med 40:595–605
Linko E, Harilainen A, Malmivaara A, Seitsalo S (2005) Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev 2:CD001356
Lohmander LS, Atley LM, Pietka TA, Eyre DR (2003) The release of crosslinked peptides from type II collagen into human joint fluid is increased early after joint insult and in osteoarthritis. Arthritis Rheum 48:3130–3139
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50:3145–3152
Lohmander LS, Roos H (1994) Knee ligament injury, surgery and osteoarthrosis: truth or consequences? Acta Orthop Scand 65:605–609
Luc B, Gribble PA, Pietrosimone BG (2014) Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train 49:806–819
Månsson O, Sernert N, Rostgard-Christensen L, Kartus J (2014) Long-term clinical and radiographic results after delayed anterior cruciate ligament reconstruction in adolescents. Am J Sports Med 43:138–145
McAlindon TE, Wilson PWF, Aliabadi P, Weissman B, Felson DT (1999) Level of physical activity and the risk of radiographic and symptomatic knee osteoarthritis in the elderly: the Framingham study. Am J Med 106:151–157
Moksnes H, Risberg MA (2009) Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports 19:345–355
Myklebust G, Holm I, Mæhlum S, Engebretsen L, Bahr R (2003) Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury. A follow-up study. Am J Sports Med 31:981–989
Nebelung W, Wuschech H (2005) Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy 21(696–702):24
Neyret P, Donell ST, Dejour D, Dejour H (1993) Partial meniscectomy and anterior cruciate ligament rupture in soccer players. A study with a minimum 20-year follow-up. Am J Sports Med 21:455–460
Neyret P, Donell ST, Dejour H (1993) Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg 75:36–40
Plaweski S, Petek D, Saragaglia D (2011) Morphometric analysis and functional correlation of tibial and femoral footprints in anatomical and single bundle reconstructions of the anterior cruciate ligament of the knee. Orthop Traumatol Surg Res 97(6 Suppl):S75–S79
Roemer FW, Jarraya M, Niu J, Silva JR, PT RF, Guermazi A (2014) Increased risk for radiographic osteoarthritis features in young active athletes: a cross-sectional matched case-control study. Osteoarthr Cartil. doi:10.1016/j.joca.2014.11.011
Seon JK, Song EK, Park SJ (2006) Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop 30:94–98
Sherman MF, Warren RF, Marshall JL, Savatsky GJ (1988) A clinical and radiographical analysis of 127 anterior cruciate insufficient knees. Clin Orthop Relat Res 227:229–237
Siebold R (2011) The concept of complete footprint restoration with guidelines for single- and double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 19:699–706
Struewer J, Frangen TM, Ishaque B, Bliemel C, Efe T, Ruchholtz S, Ziring E (2012) Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop 36:171–177
Von Porat A, Roos EM, Roos HP (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Wright RW (2014) Osteoarthritis classification scales: interobserver reliability and arthroscopic correlation. J Bone Joint Surg Am 16(96):1145–1151
Wu WH, Hackett T, Richmond JC (2002) Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med 30:845–850
Xie X, Xiao Z, Li Q, Zhu B, Chen J, Chen H, Yang F, Chen Y, Lai Q, Liu X (2014) Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol 25:149–159
Conflict of interest
No benefits have been received in any form by any of the authors with regard to the preparation of this manuscript. All authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsoukas, D., Fotopoulos, V., Basdekis, G. et al. No difference in osteoarthritis after surgical and non-surgical treatment of ACL-injured knees after 10 years. Knee Surg Sports Traumatol Arthrosc 24, 2953–2959 (2016). https://doi.org/10.1007/s00167-015-3593-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3593-9