Abstract
Purpose
The primary intent of total knee arthroplasty is the restoration of normal knee kinematics, with ligamentous constraint being a key influential factor. Displacement of the joint line may lead to alterations in ligament attachment sites relative to knee flexion axis and variance of ligamentous constraints on tibiofemoral movement. This study aimed to investigate collaterals strains and tibiofemoral kinematics with different joint line levels.
Methods
A previously validated knee model was employed to analyse the change in length of the collateral ligaments and tibiofemoral motion during knee flexion. The models shifted the joint line by 3 and 5 mm both proximally and distally from the anatomical level. The data were captured from full extension to flexion 135°.
Results
The elevated joint line revealed a relative increase in distance between ligament attachments for both collateral ligaments in comparison with the anatomical model. Also, tibiofemoral movement decreased with an elevation in the joint line. Conversely, lowering the joint line led to a significant decrease in distance between ligament attachments, but greater tibiofemoral motion.
Conclusion
Elevation of the joint line would strengthen the capacity of collateral ligaments for knee motion constraint, whereas a distally shifted joint line might have the advantage of improving tibiofemoral movement by slackening the collaterals. It implies that surgeons can appropriately change the joint line position in accordance with patient’s requirement or collateral tensions. A lowered joint line level may improve knee kinematics, whereas joint line elevation could be useful to maintain knee stability.
Level of evidence
V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has been demonstrated excellent longevity, but clinical scores after TKA are not equivalent to patient satisfaction [35]. With pain relief, patients may expect to increase their activity levels of daily living [17, 46]. Nevertheless, TKAs had exhibited poor kinematics [5, 8, 29] and an inadequate flexion range [15, 38] when compared with the natural knee. Knee kinematics after TKAs is heavily dependent on a complicated interaction between passive soft tissue restraint, implant design, component alignment, muscle force, and the joint line (JL) [4, 33, 41, 45, 47]. This study explored the influence the variation of the joint line has on soft tissue tension and tibiofemoral motion during knee flexion.
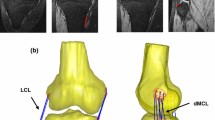
The lateral collateral ligament (LCL) and the medial collateral ligament (MCL) are not only major stabilizers of knee varus/valgus rotation but the MCL also resists tibial rotation and anterior–posterior translation [12, 16]. Therefore, alteration of the collateral ligaments’ function may affect knee movements and subsequent range of motion after TKA. In the work of Amis and Zavras [2], it was revealed that the change in length of the cruciate ligaments was significantly related to the location of the ligament’s femoral attachment site relative to knee flexion axis. If the JL level of TKA is shifted proximally or distally, it alters the knee flexion axis relative to the location of the collateral ligaments’ femoral attachment sites. Changes in joint line can probably cause varied lengthening or shortening of the collateral ligaments during knee flexion [6]. Thus, the constraint of the collateral ligaments on tibiofemoral movements might be affected, resulting in different TKA kinematics.
Precise restoration of the joint line is difficult to achieve during operation. Surgeons may have to accept slight joint line change and it is, therefore, important to know the effects of small variations in joint line on the TKA biomechanics. Although one study reported kinematic behaviour and soft tissue elongations after TKA [14], there has been little biomechanical analysis of the influence the joint line variation has on the knee kinematics or the collaterals strains. This study aimed to quantify the tibiofemoral motion and length change patterns in the collaterals.
For in vivo studies, it is difficult to clarify the influential factors due to multiple variables that cannot be controlled including patient-specific variation, surgical technique, or implant design. Computational models, however, can be used to control all variables and assess the influence of selected parameters. This study employed a validated computer knee model to understand how displacement of the JL affects the distance between the femoral and tibial attachment sites and subsequent tibiofemoral motion during knee flexion. It was hypothesized that JL variation and the accompanying change in the location of femoral collateral attachment sites relative to knee flexion axis affect the change in length of the collateral ligaments and significantly influences knee kinematics.
Materials and methods
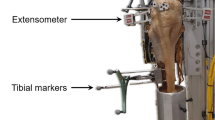
A dynamic multibody model of a replaced posterior-stabilized knee [21, 30] was utilized to calculate the change in length of the collateral ligaments during knee flexion (Fig. 1). The model comprised of a femur, tibia, fibula, and patella with implants and surrounding soft tissues, including collateral ligaments, quadriceps muscle, and patellar ligament. The MCL was divided into anterior (AMCL), oblique (OMCL), and deep bundles (DMCL), while the LCL was modelled as single bundle. Each fibre bundle was represented by nonlinear tension-only springs with reference strains and stiffness [1]:
where ε j is the strain of the j th element, K 1j and K 2j are the stiffness of the element for the parabolic and linear regions, respectively, and L 0j and L j are its current and slack lengths, respectively. The linear range threshold is specified as ε 1 = 0.03.
Quadriceps muscle, a dominant actuator during knee bending, and patellar ligament were modelled as two bundles with force–length relationships in accordance with Piazza and Delp [36]. Furthermore, in order to simulate the wrapping of the quadriceps tendon around femoral trochlea [44], each quadriceps tendon bundle was divided into two spring elements in series and connected by beads [26]. Solid to solid contact was then defined between the bead and the femoral component.
A line linking the flexion facet centres of the femoral condyle which acted as a reliable axis to describe kinematics [25] was designated as femoral flexion axis. The flexion facet centres were in compliance with the condylar radii of the femoral component. Knee flexion was ascribed to the femur via femoral flexion axis to simulate the lunging movement, whereas the tibia was unconstrained except in flexion–extension. An average ground reaction force of 1,100 N (about 1.5 times body weight) [9] was applied through the tibia. Solid to solid contacts were then modelled between femoral and tibial components and between the femoral component and the unresurfaced patella. The friction coefficient of the metal-to-polyethylene articulation was designated as 0.04 [13], and the patella-to-metal interface was assumed to be frictionless.
Two further assumptions were included in the dynamic knee model. First, the ground reaction force vector always acted in the proximal direction. This assumption was considered acceptable for the purpose of investigating variations in the joint line although the direction of ground reaction force would change during normal knee flexion [31]. Second, flexion of the femur was dependent on a fixed axis which was determined from the flexion facet centres of femoral condyles [23]. All degrees of freedom of the tibia were unconstrained except in flexion. This assumption was also reasonable because the design of the prosthetic components was symmetrical about medial and lateral tibiofemoral articulations.
For joint line variation, the displaced distance of 3 and 5 mm from the anatomical level was designated because a mild JL shift did not influence clinical outcomes [7, 37, 39]. For JL proximalization, tibial and femoral components were elevated and the insert was thickened to fill the gap caused by component translation (Fig. 2a). Distalization of the JL was also simulated by shifting prosthetic components inferiorly (Fig. 2b). Total five different JL positions were investigated in this study. Regardless of how the components were translated, the patella position and ligament length in full knee extension remained unchanged in all simulations.
A 0–135° of knee flexion was simulated referring to the claimed ROM of the TKA system. To assess the change in length of each bundle of the MCL and LCL, the distance between femoral and tibial insertion sites was recorded every 15° during flexion. The change in this distance relative to extended knee (0°) was calculated and expressed as a percentage of the length at full extension. The change in the length of ligament insertions with different JL positions was compared with that of the anatomically reconstructed knee. In addition, to acquire kinematics data, a Cartesian coordinate system was established by the longitudinal axis (z, internal and external rotation axis), the mediolateral axis (y, flexion and extension axis), and the anteroposterior axis (x, varus and valgus rotation axis; Fig. 2). Anteroposterior femoral translation was measured in x direction through medial and lateral condyle’s flexion facet centres relative to their original positions. Internal and external tibial rotations were measured in z direction on the local coordinate system of the tibia relative to the local coordinate of the femur. All analyses were carried out by MSC.ADAMS (MSC Software Corporation, Santa Ana, CA).
Results
Change in length of collateral ligaments
Lateral collateral ligament
For all JL levels, the distance between insertions in the LCL remained approximately constant at initial flexion angles; however, obvious changes occurred during high knee flexion (Fig. 3). Overall, elevation of the JL generated an increase in ligament length, whereas it was reduced with JL distalization. At 135° of flexion, the difference of LCL length as compared to the anatomically reconstructed knee is shown in Table 1 for all JL positions.
Medial collateral ligament
Similarly, joint line proximalization extended the distance between femoral and tibial attachment sites during knee flexion, while a decreased ligament length for a lowered JL (Fig. 4). In detail, although lowering the JL led to shortening of the distance between the attachments, the AMCL and the DMCL remained above the distance at full extension (Fig. 4a, b). However, beyond 105°, the OMCL was shorter than at full extension even with an elevated JL (Fig. 4c). Table 2 shows the difference of MCL length at flexion 135° in comparison with the anatomically reconstructed knee.
Tibiofemoral movement
Initial engagement of the post-cam occurred at 80° of knee flexion in the anatomical JL model. Post-cam engagement in 3 and 5 mm elevated models occurred at flexion angle of 92° and 100°, respectively, whereas it was 78° and 73° in the models with a 3 and 5 mm lowered JL.
Lateral condyle translation
Before post-cam engagement, lateral femoral condyle of all models moved forward (Fig. 5a). The amount of anterior movement of the lateral condyle was increased with lowering of the JL position. Maximal anterior translation of the lateral condyle was 5.7 mm when the JL was lowered by 5 mm. Thereafter, the lateral condyle moved backward. Posterior condyle translation was increased dramatically with greater knee flexion.
Medial femoral translation
For all models, the medial condyle displayed a similar pattern of movement with that of lateral condyle (Fig. 5b). It also moved forward before post-cam engagement, whereas the medial condyle rolled backward as the femoral cam contacted with the tibial post. Similarly, the more the JL was lowered, the greater the magnitude of medial condyle translation.
Tibial rotation
Internal tibial rotational angle increased following knee flexion in all models before post-cam engagement (Fig. 5c). At 75° of flexion, internal tibial rotation of the anatomically reconstructed knee reached 7.7°, whereas the model with a 5 mm lowered JL displayed the least tibial rotation of 5.1°. With higher flexion angles, the amount of internal tibial rotation decreased sharply for all JL positions. However, rotation increased after post-cam disengagement, especially when the JL was moved distally.
Discussion
The most important finding of the current study was that the lowered JL shortened the distance between collateral ligament attachments following knee flexion, whereas a greater tibiofemoral movement was observed. Conversely, an elevated JL produced a lengthening of the collateral ligament and less tibiofemoral motion.
Issues regarding knee kinematics after TKA have been of great concern. Numerous studies have investigated the effects of the prosthetic design features on knee motion in order to restore normal knee kinematics [29, 34, 43]. Nevertheless, the magnitude of the normal tibiofemoral movement was only partially recovered. This study discovered an alternative treatment, shifting the JL, which changed the constraint of the collaterals during knee flexion to enhance tibiofemoral movement.
The change in distance between ligament attachments with variations in the joint line could be explained from the relative position between the condylar centre and the ligament attachment site. From the sagittal view, a change in the JL level would simultaneously translate the condylar centres of the femoral component. Elevation of the JL caused a proximal shift of the condylar centre, locating it closer to the ligament attachment. Oppositely, lowering the JL translated the condylar centre distally (Fig. 6). During knee flexion, the elevated JL maintained a proximal displacement of the ligament attachment site, thus further increasing the length of the ligament. Lowering the JL produced a distal shift of the attachment sites, which reduced the DI.
Lowering the JL maintained a constant LCL length before 60° of flexion, but the length decreased significantly after 60°. However, there was a 5 % pre-strain in the LCL at full knee extension [1]. The LCL still elongated for a 3-mm lowering of the JL, while it was slackened with a 5-mm lowering during knee flexion. For the MCL, the AMCL was stretched with knee flexion although the lowered JL reduced the distance between the attachments. Maximum elongation of the AMCL with 3- and 5-mm lowering of the JL was 10.4 and 9.4 %, respectively. Even taking into account the 6 % reduction in length at full extension [1], the AMCL still had the ability to constrain tibiofemoral motion. The DMCL remained taut after lowering the JL by 3 and 5 mm. In addition, the OMCL was still stretched during low flexion due to a 3.1 % pre-strain [1].
Overall, lowering the JL decreased the distance between ligament attachments, resulting in ligament laxity. Several literatures showed that hyper-laxity of the ligament resulting from unbalanced flexion and extension gaps or substantial ligament release due to considerable joint deformity caused instability in flexion and posterior subluxation of the tibia. Some cases of subluxation were induced by using a total condylar knee prosthesis, which is designed without a mechanism for substituting cruciate ligaments [22, 40]. Others occurred with posterior-stabilized knee prostheses, but the tibial subluxation was mainly attributed to preoperative valgus knee with increased Q angle, preoperative patellar instability, or inadequate lateral release [32]. For a varus-deformed knee, the release side is the medial collateral, whereas the LCL, a passive stabilizer of posterior tibial movement [19], is generally designated as a reference for ligamentous balance. Our results revealed that a 3-mm lowering of the JL retained the LCL function as a posterior stabilizer, avoiding tibial subluxation. Furthermore, this mild JL variation did not influence clinical outcomes [7, 37, 39].
Therefore, appropriately lowering the JL could enhance tibiofemoral movement without compromising joint stability. This implies that this procedure is advantageous in improving high knee flexion. Specifically, the tibial insert of most contemporary TKA designs is concave in shape, and the articular surface is deeply dished in the coronal plane. This geometry could produce a greater constraint to femoral rollback and axial tibial rotation. In order to allow more relative movement between the femur and the tibia, a slightly loose ligament during knee flexion might be necessary to accommodate greater translation and rotation. Numerous investigations also suggested a lax knee joint can improve the range of flexion [3, 10]. In a clinical study with bilateral TKAs, patients preferred the laxer knee and felt more comfortable [28]. In addition, weight-bearing, high-flexion activities such as kneeling and squatting necessitate more than 20° of internal tibial rotation and the joint stiffness will increase with muscle contractions. On the other hand, a non-weight-bearing posture of cross-legged sitting requires 33° of tibial rotation [18]. Releasing the ligamentous constraint through a properly lowered JL may be suggested to improve tibial rotation, which helps knee flexion. However, it should be noted that over-internal rotation and rollback may cause excessive tightening in the iliotibial band and subsequent anterolateral knee pain [20].
As for JL elevation, the results exhibited that it further increased the distance between ligament attachments. König et al.’s study [27] also presented similar change in length of the collateral ligaments when the JL was moderately elevated. Considering that collateral ligaments are taut in knee extension, it is expected that further increased ligament length would lead to high motion constraints to the knee joint. The additional stretch in ligaments could also increase soft tissue tension, contributing to internal loading of the tibiofemoral joint, which has been correlated with wear of the polyethylene insert after TKA [11]. Jeffcote et al. [24] revealed an increased tibiofemoral force with a 2-mm proximal shift of components. Furthermore, the knee is exposed to considerable loading during daily activities [42, 48]. Any raised internal forces may result in overloading of the tibiofemoral joint, jeopardizing the polyethylene insert.
Some limitations of the present study should be considered. First, this study utilized a specific posterior-stabilized knee prosthesis which is not representative of contemporary TKA designs. However, we believe that the results are not unique to this specific design. Second, a cruciate-retaining knee prosthesis was not included in the current study. Further study of the effect of JL variation on the posterior cruciate ligament is needed. Third, all components included in this model were designated as rigid bodies, and thus, the results cannot reflect the influence of material properties on knee motion. Fourth, surrounding soft tissues were modelled with nonlinear behaviour, and their properties were simulated with simple force elements, and thus, the biological conditions may not be adequately represented. Obviating these limitations, the current study provides instructions for surgical treatment to help improve knee motion.
This work provides certain instructions for surgeons regarding their day by day clinical practice. It is suggested that surgeons could properly adjust the joint line position according to patient’s demands. A lowered joint line level might be advantageous for young patients or the populations who expect to increase their activity levels of daily living. On the other hand, once excessive collateral ligament laxity resulting from considerable knee deformity is recognized, an orthopaedic surgeon could augment the joint line with the goal of achieving knee joint stability.
Conclusion
A lowered JL reduced the distance between ligament attachments, relieving ligamentous constraint, while an elevation of the JL further strengthen the function of the collateral ligaments during knee flexion. A lowered JL had the advantage of enhancing tibiofemoral movement. However, elevation of the JL may not be allowed after TKA because it would induce catastrophic complications.
References
Abdel-Rahman EM, Hefzy MS (1998) Three-dimensional dynamic behaviour of the human knee joint under impact loading. Med Eng Phys 20:276–290
Amis AA, Zavras TD (1995) Isometricity and graft placement during anterior cruciate ligament reconstruction. Knee 2:5–17
Asano H, Hoshino A, Wilton TJ (2004) Soft tissue tension in total knee arthroplasty. J Arthroplasty 19:558–561
Baldwin MA, Laz PJ, Stowe JQ, Rullkoetter PJ (2009) Efficient probabilistic representation of tibiofemoral soft tissue constraint. Comput Methods Biomech Biomed Engin 12:651–659
Banks SA, Hodge WA (2004) Design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasty. J Arthroplasty 19:809–816
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Cope MR, O’Brien BS, Nanu AM (2002) The influence of the posterior cruciate ligament in the maintenance of joint line in primary total knee arthroplasty: a radiologic study. J Arthroplasty 17:206–208
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
D’Lima DD, Patil S, Steklov N, Chien S, Colwell CW Jr (2007) In vivo knee moments and shear after total knee arthroplasty. J Biomech 40(Suppl 1):11–17
Edwards E, Miller J, Chan KH (1988) The effect of postoperative collateral ligament laxity in total knee arthroplasty. Clin Orthop Relat Res 236:44–51
Estupiñán JA, Bartel DL, Wright TM (1998) Residual stresses in ultra-high molecular weight polyethylene loaded cyclically by a rigid moving indenter in nonconforming geometries. J Orthop Res 1:80–88
Gardiner JC, Weiss JA, Rosenberg TD (2001) Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop Relat Res 391:266–274
Godest AC, Beaugonin M, Haug E, Taylor M, Gregson PJ (2002) Simulation of a knee joint replacement during a gait cycle using explicit finite element analysis. J Biomech 35:267–275
Halewood C, Risebury M, Thomas NP, Amis AA (2014) Kinematic behaviour and soft tissue management in guided motion total knee replacement. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2933-5
Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD (2008) Midterm comparison of posterior cruciate-retaining versus–substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee 15:217–221
Harfe DT, Chuinard CR, Espinoza LM, Thomas KA, Solomonow M (1998) Elongation patterns of the collateral ligaments of the human knee. Clin Biomech (Bristol, Avon) 13:163–175
Healy WL, Iorio R, Lemos MJ (2000) Athletic activity after total knee arthroplasty. Clin Orthop Relat Res 380:65–71
Hemmerich A, Brown H, Smith S, Marthandam SS, Wyss UP (2006) Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res 24:770–781
Höher J, Harner CD, Vogrin TM, Baek GH, Woo SL (1998) In situ forces in the posterolateral structures of the knee under posterior tibial loading in the intact and posterior cruciate ligament-deficient knee. J Orthop Res 16:675–681
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21:2271–2280
Huang CH, Hsu LI, Lin KJ, Chang TK, Cheng CK, Lu YC, Chen CS, Huang CH (2014) Patellofemoral kinematics during deep knee flexion after total knee replacement: a computational simulation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2819-y
Insall J, Scott WN, Renawat CS (1979) The total condylar knee prosthesis: a report of two hundred and twenty cases. J Bone Joint Surg Am 61:173–180
Iwaki H, Pinskerova VP, Freeman MAR (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82:1189–1195
Jeffcote B, Nicholls R, Schirm A, Kuster MS (2007) The variation in medial and lateral collateral ligament strain and tibiofemoral forces following changes in the flexion and extension gaps in total knee replacement. A laboratory experiment using cadaver knees. J Bone Joint Surg Br 89:1528–1533
Kessler O, Dürselen L, Banks S, Mannel H, Marin F (2007) Sagittal curvature of total knee replacements predicts in vivo kinematics. Clin Biomech (Bristol, Avon) 22:52–58
Kessler O, Patil S, Colwell CWJ, D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41:3332–3339
König C, Matziolis G, Sharenkov A, Taylor WR, Perka C, Duda GN, Heller M (2011) Collateral ligament length change patterns after joint line elevation may not explain midflexion instability following TKA. Med Eng Phys 33:1303–1308
Kuster MS, Bitschnau B, Votruba T (2004) Influence of collateral ligament laxity on patient satisfaction after total knee arthroplasty: a comparative bilateral study. Arch Orthop Trauma Surg 124:415–417
Li G, Most E, Sultan PG, Schule S, Zayontz S, Park SE, Rubash HE (2004) Knee kinematics with a high-flexion posterior stabilized total knee prosthesis: an in vitro robotic experimental investigation. J Bone Joint Surg Am 86:1721–1729
Lin KJ, Huang CH, Liu YL, Chen WC, Chang TW, Yang CT, Lai YS, Cheng CK (2011) Influence of post-cam design of posterior stabilized knee prosthesis on tibiofemoral motion during high knee flexion. Clin Biomech (Bristol, Avon) 26:847–852
McFadyen BJ, Winter DA (1988) An integrated biomechanical analysis of normal stair ascent and descent. J Biomech 21:733–744
Merkow RL, Soudry M, Insall JN (1985) Patellar dislocation following total knee replacement. J Bone Joint Surg Am 67:1321–1327
Mesfar W, Shirazi-Adl A (2005) Biomechanics of the knee joint in flexion under various quadriceps forces. Knee 12:424–434
Moonot P, Mu S, Railton GT, Field RE, Banks SA (2009) Tibiofemoral kinematic analysis of knee flexion for a medial pivot knee. Knee Surg Sports Traumatol Arthrosc 17:927–934
Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB (2005) Does total knee replacement restore normal knee function? Clin Orthop Relat Res 431:157–165
Piazza SJ, Delp SL (2001) Three-dimensional dynamic simulation of total knee replacement motion during a step-up task. J Biomech Eng 123:599–606
Ritter MA, Montgomery TJ, Zhou H (1999) The clinical significance of proximal tibial resection level in total knee arthroplasty. Clin Orthop Relat Res 360:74–181
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am 85:1278–1285
Ryu J, Saito S, Yamamoto K, Sano S (1993) Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis 53:35–40
Sharkey PF, Hozack WJ, Booth RE, Balderston RA, Rothman RH (1992) Posterior dislocation of total knee arthroplasty. Clin Orthop Relat Res 278:128–133
Shoji H, Solomonow M, Yoshino S, D’Ambrosia R, Dabezies E (1990) Factors affecting postoperative flexion in total knee arthroplasty. Orthopedics 13:643–649
Taylor WR, Heller MO, Bergmann G, Duda GN (2004) Tibio-femoral loading during human gait and stair climbing. J Orthop Res 22:625–632
van Duren BH, Pandit H, Price M, Tilley S, Gill HS, Murray DW, Thomas NP (2012) Bicruciate substituting total knee replacement: how effective are the added kinematic constraints in vivo? Knee Surg Sports Traumatol Arthrosc 20:2002–2010
van Eijden TM, de Boer W, Weijs WA (1985) The orientation of the distal part of the quadriceps femoris muscle as a function of the knee flexion-extension angle. J Biomech 18:803–809
Wang ZW, Liu YL, Lin KJ, Qu TB, Dong X, Cheng CK, Hai Y (2012) The effects of implantation of tibio-femoral components in hyperextension on kinematics of TKA. Knee Surg Sports Traumatol Arthrosc 20:2032–2038
Weiss JM, Noble PC, Conditt MA, Kohl HW, Roberts S, Cook KF, Gordon MJ, Mathis KB (2002) What functional activities are important to patients with knee replacements? Clin Orthop Relat Res 404:172–188
Willing R, Kim IY (2011) Design optimization of a total knee replacement for improved constraint and flexion kinematics. J Biomech 44:1014–1020
Zhao D, Banks SA, D’Lima DD, Colwell CW, Fregly BJ (2007) In vivo medial and lateral tibial loads during dynamic and high flexion activities. J Orthop Res 25:593–602
Acknowledgments
We acknowledge the financial support of the Administrative Bureau of Southern Taiwan Science Park (BY-03-04-17-98).
Conflict of interest
No conflicts of interest on this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hung-Wen Wei and Chang-Hung Huang have equally contributed to this work.
Rights and permissions
About this article
Cite this article
Lin, KJ., Wei, HW., Huang, CH. et al. Change in collateral ligament length and tibiofemoral movement following joint line variation in TKA. Knee Surg Sports Traumatol Arthrosc 24, 2498–2505 (2016). https://doi.org/10.1007/s00167-014-3400-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3400-z