Abstract
Cervical spine deformity represents a broad spectrum of pathologies that are both complex in etiology and debilitating towards quality of life for patients. Despite advances in the understanding of drivers and outcomes of cervical spine deformity, only one classification system and one system of nomenclature for osteotomy techniques currently exist. Moreover, there is a lack of standardization regarding the indications for each technique. This article reviews the adult cervical deformity (ACD) and current classification and nomenclature for osteotomy techniques, highlighting the need for further work to develop a unified approach for each case and improve communication amongst the spine community with respect to ACD.
Zusammenfassung
Deformitäten der Halswirbelsäule (HWS) umfassen ein breites Spektrum an Pathologien, die sowohl komplex in ihrer Ätiologie sind als auch die Lebensqualität der Patienten belasten. Trotz der verbesserten Kenntnisse von Einflussfaktoren und Ergebnissen der HWS-Deformitäten existieren bisher nur ein einziges Klassifikationssystem und eine Nomenklatur für Osteotomieverfahren. Zudem fehlt eine Standardisierung bezüglich der Indikationsstellung zu den einzelnen Verfahren. Dieser Beitrag gibt eine Übersicht über die Deformitäten der Halswirbelsäule bei Erwachsenen („adult cervical deformity“, ACD) sowie die aktuellen Klassifikationen und Nomenklaturen für Osteotomieverfahren. Hierbei soll betont werden, dass es weiterer Arbeiten zur Entwicklung eines einheitlichen Verfahrens für einzelne Fälle sowie einer Verbesserung der Kommunikation in der Spine Community in Bezug auf ACD bedarf.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Historical perspective
Before the radiographic X‑ray era, the term “neck deformity” was used to describe burn and mass-driven cervical deformities by Wood in 1863 and Heath in 1911, respectively [30, 83]. During the first half of the twentieth century, the advent of radiological techniques allowed clinicians to precisely describe degenerative changes of the cervical spine and subsequent deformity. In 1946, Whiteleather identified loss of cervical lordosis (CL) as a consequence of disk degeneration in the aging spine [81]. Cervical kyphosis was also described after acute injuries such as whiplash accidents, demonstrated by Nagle in 1957 [55]. Multiple attempts to measure CL in lateral X‑rays were also performed during that era. However, the methods most commonly used now include the Cobb method, developed by Dr. John Cobb at the Hospital for Special Surgery, and the Harrison posterior tangent method ([14, 21, 29, 65]; Fig. 1). Quantifying cervical deformity by radiographic parameters led to the first steps toward clinically relevant classifications. Moreover, there have been recent advances in formulating a widely-accepted, standardized classification or nomenclature system for cervical soft tissue release and osteotomy to manage cervical deformity [70]. This article offers evidence-based recommendations for management of adult cervical deformity (ACD) and highlights available algorithms.
Diagnosis of adult cervical deformity
Clinical presentation of cervical deformity
An ACD can occur due to multiple etiologies, ranging from inflammatory and non-inflammatory spondyloarthropathies to neuromuscular pathologies as well as the development of proximal junctional kyphosis (PJK) following long thoracolumbar spinal fusion [20, 23, 44, 53]. They can present with focal and global cervical deformities, which may lead to increased compensation at adjacent spinal segments in an attempt to maintain horizontal gaze. Patients experience functional impairments in horizontal gaze, posture, gait, and, if severe, they may also complain of dysphagia and dyspnea. Furthermore, patients often present with neck pain, and stiffness, as well as paresthesia and sensorimotor deficits due to compression of neural elements and impaired cord perfusion [75]. Smith et al. [69] reported that the mean EuroQuol‑5 Dimensions (EQ-5D) score for ACD patients was below the bottom 25th percentile compared to several other chronic disorders and very close to blindness. Similarly, Iyer et al. [35] demonstrated that increasing cervical sagittal malalignment correlated with higher preoperative morbidity, as measured by the neck disability index (NDI) score. In 2013, Smith et al. observed association between modified Japanese Orthopaedic Association (mJOA) scores, sagittal alignment, and spinal cord volume calculated from magnetic resonance imaging (MRI), demonstrating a relationship between deformity and myelopathy [68]. Surgical management of ACD focuses on achieving symptomatic relief, neurologic recovery, and deformity correction and has a well-documented efficacy [45, 66, 74, 78].
Radiographic assessment of cervical deformity
While the importance of a thorough clinical assessment for obvious deformities, limitations in motion, and neurovascular function cannot be overstated, it is necessary to obtain full spine standing 36-inch (36”) X‑rays in order to appropriately evaluate the role of cervical alignment with respect to overall sagittal spinal alignment [2]. Similarly, it is important to obtain coronal views in order to assess for scoliosis as well as to identify any cervical ribs [17, 56]. Dynamic assessment by flexion-extension radiographs should also be incorporated in preoperative planning to evaluate cervical stiffness and range of motion (ROM) that is known to be correlated to patient-reported outcomes (PROs) [46]. Likewise, MRI is a well-known modality used for diagnosis and surgical planning for patients with cervical myelopathy [80]. Although distortion in both the coronal and sagittal planes occurs in cervical spinal deformity, sagittal plane deformities are more common [13, 73] and, when surgically-corrected, are closely related to better clinical outcomes [24]. Computerized tomography provides useful information boney anatomy and the presence of ossification of the posterior longitudinal ligament (OPLL) [50].
Alignment considerations
Normal cervical alignment
In healthy individuals, the cervical spine has a large variability of normal alignment due to its relative mobility and adaptability to full body alignment [25]. Originally, cervical kyphosis was found in 46 out of 116 asymptomatic subjects by Rubinstein et al. [21] in the early 1960s, ultimately concluding that it alone could not define cervical deformity. However, later in the 1990s Hardacker et al. [28] demonstrated that in healthy volunteers, the normal cervical alignment is lordotic, with a mean CL of –40.0 ± 9.7°, with the occiput-C1 segment being kyphotic. Moreover, they reported that the majority of lordosis was localized to C1-C2, with only 15% (6°) of lordosis occurring at the lowest three cervical levels (C4-C7) [28]. Yet, more recent studies supported Rubinstein et al. [21] by presenting cervical kyphosis as a normal variant. Faline et al. [19] and Le Huec et al. [34] evaluated asymptomatic subjects and found that more than 30% of subjects demonstrated cervical kyphosis.
What drives the cervical alignment in normal and deformity settings?
The cervical spine adapts to our different postures in order to maintain functional gaze [42]. In standing posture, Diebo et al. [16] found that thoracic kyphosis (TK) and global thoracolumbar alignment (C7-S1 sagittal vertical axis [SVA]) were independent drivers of cervical alignment in patients with a functional, horizontal gaze. The authors reported that cervical alignment may be kyphotic in a significant proportion of patients with negative global alignment or a hypokyphotic thoracic spine. However, in their study, patients with SVA >50 mm and increased TK required lordotic cervical alignment to maintain horizontal gaze. As a result, Diebo et al. [16] proposed cervical alignment thresholds to maintain horizontal gaze based on SVA and TK (Table 1). Their study presented cervical alignment as a patient-specific measure. For instance, a CL of 20° might be hyperlordotic, ideal, or hypolordotic for 3 different types of patients (Fig. 2).
X-ray images of three patients who maintain horizontal gaze, yet present with different alignment patterns. a Hyperlordotic cervical profile, with CL −32.3°, SVA 91.5 mm and TK 45.6°. b Ideal cervical profile, with CL –17.3°, SVA 72.6 mm and TK 50.3°. c Hypolordotic cervical profile, with CL −2.1°, SVA −16.9 mm and TK 23.9°
Recent work by Hey et al. [32] highlighted the same findings in sitting posture; 100% of patients had a lordotic cervical alignment when evaluated in a comfortable sitting position due to increased T1-slope and SVA.
The interplay between cervical and thoracolumbar alignment is apparent in the settings of deformity. Passias et al. [60] found that 47.7% of patients without prior cervical deformity who underwent thoracolumbar surgery for adult spinal deformity subsequently developed new-onset cervical deformity based on the current definition of ACD. In contrast, Smith et al. [71] found that patients with sagittal spinopelvic deformity who compensated with an abnormal increase in CL and underwent lumbar pedicle subtraction osteotomy (PSO) subsequently developed reciprocal changes in the cervical spine that resulted in an improvement in cervical hyperlordosis. This syndromic relationship between cervical and thoracolumbar alignments in both asymptomatic and deformity settings necessitates a great attention when planning surgical treatment for cervical deformity. An ACD can present as an isolated deformity of the cervical spine or concomitant with thoracolumbar deformity (cervicothoracolumbar CTL syndrome). Recent unpublished work by Staub/Lafage et al. [40] further emphasized the interplay between T1 slope [T1S] driven by thoracolumbar alignment and cervical lordosis. In their study, they showed that the T1S-CL mismatch is a constant for a given horizontal gaze. Their study proposed that a normative CL for a given patient can be predicted by the formula: CL = T1S – 16.5 ± 2. This formula, pending further research, is expected to provide a threshold for cervical deformity and aid in providing a goal for surgical correction at the cervical or upper thoracic levels.
Adult cervical deformity classification
First attempts to classify ACD were reported by Ames et al. [4]. They proposed a classification system for ACD to standardize communication among surgeons [61]. The system was built on basic deformity descriptors and five associated modifiers. Deformity descriptors differentiated deformity by type, ranging from sagittal to craniovertebral junction deformities, as well as regional location factoring thoracolumbar deformities. The selected modifiers accounted for various factors correlating with ACD and thoracolumbar deformity; however, this classification was criticized for being too complex for clinical application and that it classifies healthy subjects as deformed due to broad and imprecise thresholds of radiographic parameters [6, 43].
Recent research by Kim et al. [40] has changed the way we address cervical deformity. As in initial step, the team revisited radiographic assessment of cervical deformity by consensus approach combined with discriminant analysis. Their study showed that the five most discriminate parameters are cSVA and T1 slope on lateral view, and maximum focal kyphosis, C2 slope and number of kyphotic levels on extension view. Those parameters were able to describe severe cervical deformity cases with +85% accuracy and canonical correlation of 0.689. Furthermore, and based on an experts’ panel and utilizing 2-step cluster analysis (a combination of hierarchical cluster and K‑mean cluster), the team proposed 3 distinct morphologies of sagittal cervical deformities based on lateral and extension radiographs ([40]; Fig. 3). Overall, the current classifications remain limited to radiographic or clinical description. There exists no classification system that dictates treatment modality and strongly predict outcomes. This is, however, the focus of an ongoing research.
New cervical deformity morphologies described by Kim et al [40]: Group 1 (46.1%): Flatneck with lack of compensation, large T1S-CL, flexible CL; Group 2 (30.8%): Focal deformity, large focal kyphosis between 2 segments, No large regional cervical kyphosis under the setting of a low T1S; Group 3 (23.1%): Cervico-thoracic deformity, very large T1S, hyperlordosis of the cervical spine, no extension reserve left
Management algorithm by passive correctability
A concept for selection of mode of management for cervical deformities has also been recently put forth by Albert [1], amalgamating the current literature in order to develop an algorithm that stratified patients by fixed (not passively correctable) or flexible (passively correctable) cervical deformities. Flexible deformities may be candidates for anterior cervical discectomy and fusion or corpectomy, posterior decompression and fusion, or combined antero-posterior approach, which may offer improved biomechanical stability and fusion rate. Fixed deformities can be sub-divided by ankylosis. Non-ankylosed fixed deformities may be candidates for anterior release/grafting with or without posterior fusion. Ankylosed fixed deformities are candidates for various osteotomies, based on the localization of fusion. Fused anterior columnar cervical deformities may undergo anterior osteotomy, grafting, and posterior instrumentation. Fused posterior columnar cervical deformities may undergo posterior osteotomy, anterior release, and interbody and posterior instrumentation. Circumferentially fused cervicothoracic junction lesions may be candidates for PSO (Fig. 4).
Algorithm for management of cervical deformity based on the ability to achieve passive correction of the deformity proposed by Albert [1]. ACDF Anterior Cervical Discectomy and Fusion, AP anteroposterior
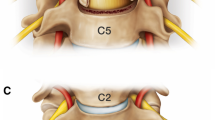
Osteotomy nomenclature and surgical indication
Ames et al. [3] proposed an anatomically-based, universal nomenclature of cervical osteotomies that progresses incrementally across seven grades of bone and soft tissue resection and destabilization. The system also incorporated modifiers to indicate the surgical approach utilized. Despite this attempt, there remains a lack of standardization and consensus among spine surgeons with respect to selection of surgical technique [27, 36, 56, 67]. The approach and technique selected depend on degrees of correction required and mobility of the spine. Posterior approaches can provide superior angular and translational corrections [39]. Etame at el. [18] reported that anterior approaches provided 11° to 32° of correction, dorsal PSO provided 23-54° of correction, and combined anterior and posterior approaches provided 24–61.4° of correction in Cobb angle. More recently, Kim and colleagues [38] described their technique and experience with anterior cervical osteotomies for fixed CD. They validated its safety in a consecutive series of patients and compared patients receiving only anterior cervical osteotomy to those with both anterior osteotomy and Smith-Petersen osteotomy (SPO). They reported improvements in NDI for both groups, though no difference was found between each group for NDI as well as mean angular correction (23° vs. 33°, p = 0.15). However, anterior cervical osteotomy alone provided less mean translational correction (1.3 vs. 3.7 cm, p = 0.03), leading the authors to conclude that anterior cervical osteotomies for fixed CDs were safe, effective, and could be combined with SPO for additional angular and translational correction. Kim et al. [39] also reported that isolated implementation of SPO, PSO, and anterior cervical osteotomy could provide 10°, 35°, and 17° of angular correction per level, respectively. More importantly, they demonstrated that combined anterior cervical osteotomy with SPOs yielded comparable or better correction than isolated SPO, especially for CDs requiring more translational than angular correction, while also reducing blood loss and requiring similar operative time. They ultimately concluded that the anterior approach, if feasible, is superior to an isolated PSO.
The following describes Ames et al. [3] osteotomy classification and the potential utilization of each grade:
Grade 1: partial facet joint resection
Grade 1 osteotomies are performed via anterior approach with discectomy and partial uncovertebral joint resection or posterior approach with facet capsular resection or partial facet resection. Grade 1 osteotomies are used in combination with other osteotomy and release procedures [3, 15, 54]; however, they afford minimal correction and their isolated use for ACD correction remains controversial. Partial facet resection has been documented in treatment of selected cases of cervical radiculopathy with minimal adjacent-segment degeneration and optimal ROM [11].
Grade 2: complete facet joint resection
Grade 2 osteotomies are performed via posterior approach but may be combined with anterior soft-tissue release and involve resection of both superior and inferior facets at the level of interest. The ligamentum flavum, lamina, and spinous processes may also be removed. Some degree of anterior column mobility is required to achieve proper alignment. Grade 2 osteotomies include the SPO [9, 72], the Chevron variety SPO [8], the extension osteotomy [48], and the Ponte osteotomy. They are generally indicated for sagittal plane deformities with a mobile anterior column in which multi-segment correction is required [8]. Specifically, when proximal junctional kyphosis (PJK) occurs in the cervicothoracic spine, Ponte osteotomy is commonly employed to restore proper alignment, as it is capable of correcting 10° at each treated level [10].
Grade 3: partial or complete corpectomy
Grade 3 osteotomies (partial or complete corpectomy) are performed with discectomy and are used for deformity correction as well as augmentation of foraminal and spinal canal decompression. Performed via an anterior approach, they may also be combined with posterior release. To attain optimal correction, the posterior column must maintain adequate mobility. Grade 3 osteotomies have been reported in the correction of cervical kyphotic sagittal deformity [57], cervical spondylotic myelopathy [58], and cervical radiculopathy [63]. The advantage of this technique is that it provides release and deformity correction along with spinal canal and foramina decompression. Gao et al. [22] reported significant improvement after 5‑year follow-up, as demonstrated by a 3.8 ± 1.3 increase in mJOA score in cervical spondylotic myelopathy patients treated with anterior corpectomy and fusion. Similarly, Andaluz et al. [5] reported significant long-term improvement, as demonstrated by a three-point improvement in modified JOA score following cervical corpectomy for treatment of symptomatic subaxial cervical spine spondylosis.
Grade 4: complete uncovertebral joint resection to the transverse foramen
Grade 4 osteotomies are performed via anterior approach. Unlike grade 1 osteotomies, grade 4 osteotomies involve bony resection that extend laterally through the lateral body and uncovertebral joints into the transverse foramen. Grade 4 osteotomies are particularly useful for patients with completely ankylosed anterior columns [3]. O’Shaughnessy et al. [59] reported on 16 patients successfully treated with grade 4 osteotomy for fixed cervical kyphosis with myelopathy, demonstrating mean Cobb angle correction of 48°. Similarly, Wang et al. [79] and Cheng et al. [12] demonstrated successful treatment of fixed cervical kyphosis and cervical spondylotic myelopathy, respectively, with grade 4 osteotomy.
Grade 5: opening wedge osteotomy
Grade 5 osteotomies, performed via anterior approach, involve full resection of laminae, spinous process, and facets with subsequent osteoclastic fracture and formation of an anterior wedge in the anterior column. This results in a fulcrum of rotation in the middle column and leads to anterior column lengthening with posterior column shortening. Grade 5 was first described by Mason et al. [49] and later modified by Urist et al. [77] for correction of ankylosing spondylitis (AS). Since then, numerous reports have documented their use for correction of ACD in patients with AS [7, 51, 52]. Koller et al. [41] demonstrated mean CBVA correction of 25° for AS patients treated with non-instrumented C7-T1 open-wedge osteotomy. However, the risk of neurovascular complications and risk to anterior soft tissue structures has led to replacement of open-wedge osteotomies by other techniques [31, 56].
Grade 6: closing wedge osteotomy
Grade 6 osteotomies involve complete resection of the laminae, spinous process, facets, and pedicles via posterior approach, with subsequent formation of a closing wedge in the vertebral body. Unlike Grade 5 osteotomies, they do not produce any anterior column lengthening, avoiding any associated vascular and neurological complications [7, 51]. The “eggshell” procedure, a posterior de-cancellation osteotomy or PSO, widely used within thoracolumbar correction [47, 84], is most similar to grade 6 osteotomies used in ACD correction. Grade 6 osteotomies are a safer alternative than grade 5 osteotomies, as they do not produce any elongation of the anterior spinal column [3]. Their use has been extensively documented within literature for ACD [37, 62, 64, 82]. Specifically, Tokala et al. [76] documented that fixed cervico-thoracic kyphosis patients treated with C7 de-cancellization closing wedge osteotomy had full restoration of normal forward gaze. Similarly, Deviren et al. [15] reported on 11 cases of cervico-thoracic junction PSO for patients with AS, cervical kyphosis, chin-on-chest deformity, and fixed coronal and sagittal plane ACD and showed that patients experienced mean CBVA correction of 36.7° and significant decrease in NDI and visual analogue scale (VAS) pain scores.
Grade 7: complete vertebral column resection
Grade 7 osteotomies involve complete resection of one or more entire vertebral bodies, associated discs, uncovertebral joints, posterior laminae, and facets and are performed via combined anterior and posterior approach. Grade 7 osteotomies are complex, high-risk procedures with sparsely documented indications. This technically demanding procedure is reserved for severe cases of AS [33] and cervical kyphosis [26].
Conclusion
The ACD of the spine represents a spectrum of complex and debilitating pathologies that significantly impact quality of life. Initial attempts for radiographic and osteotomy classifications are too complex and still lacking the ability to guide treatment. Based on integration of functional gaze and dynamic assessment of the cervical spine, emerging research is promising for a simplified, and clinician friendly language. Spine flexibility, surgical approach, osteotomy grade and alignment targets are expected to be integral parts of future classification that aims to dictate treatment.
Abbreviations
- ACD:
-
Adult cervical deformity
- AS:
-
Ankylosing spondylitis
- CBVA:
-
Chin-brow-to-vertical angle
- CK:
-
Cervical kyphosis
- CL:
-
Cervical lordosis
- EQ-5D:
-
EuroQuol-5Dimension questionnaire
- mJOA:
-
Modified Japanese Orthopaedic Association score
- NDI:
-
Neck disability index
- PJK:
-
Proximal junctional kyphosis
- PRO:
-
Patient-reported outcome
- PSO:
-
Pedicle subtraction osteotomy
- ROM:
-
Range of motion
- SVA:
-
Sagittal vertical axis
- TK:
-
Thoracic kyphosis
References
Albert TJ (2017) Complications in adult spinal deformity surgery from cervical to lumbar spine: latest concepts in treating cervical deformity. Scoliosis Res. Soc. 52nd Annu. Meet. Course Progr.
Ames CP, Blondel B, Scheer JK et al (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 38:S149–S160. https://doi.org/10.1097/BRS.0b013e3182a7f449
Ames CP, Smith JS, Scheer JK et al (2013) A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction. J Neurosurg Spine 19:269–278. https://doi.org/10.3171/2013.5.SPINE121067
Ames CP, Smith JS, Eastlack R et al (2015) Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 23:673–683. https://doi.org/10.3171/2014.12.SPINE14780
Andaluz N, Zuccarello M, Kuntz C (2012) Long-term follow-up of cervical radiographic sagittal spinal alignment after 1- and 2-level cervical corpectomy for the treatment of spondylosis of the subaxial cervical spine causing radiculomyelopathy or myelopathy: a retrospective study. J Neurosurg Spine 16:2–7. https://doi.org/10.3171/2011.9.SPINE10430
Bakouny Z, Khalil N, Salameh M et al (2017) Are the radiographic components of the Ames-ISSG classification specific to cervical deformity? EuroSpine.
Belanger TA, Milam RA, Roh JS, Bohlman HH (2005) Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. J Bone Joint Surg Am 87:1732–1738. https://doi.org/10.2106/JBJS.C.01472
Bridwell KH (2006) Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 31:S171–S188. https://doi.org/10.1097/01.brs.0000231963.72810.38
Burton DC (2006) Smith-Petersen osteotomy of the spine. Instr Course Lect 55:577–582
Cecchinato R, Berjano P, Bassani R, Lamartina C (2015) Osteotomies in proximal junctional kyphosis in the cervicothoracic area. Eur Spine J 24(Suppl 1):31–37. https://doi.org/10.1007/s00586-014-3654-7
Chang JC, Park HK, Choi SK (2011) Posterior cervical inclinatory foraminotomy for spondylotic radiculopathy preliminary. J Korean Neurosurg Soc 49:308–313. https://doi.org/10.3340/jkns.2011.49.5.308
Cheng J, Liu H, Lin X (2006) Preliminary application of anterior uncovertebral joint resection in cervical spondylotic treatment. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 20:380–382
Chi JH, Tay B, Stahl D, Lee R (2007) Complex deformities of the cervical spine. Neurosurg Clin N Am 18:295–304. https://doi.org/10.1016/j.nec.2007.01.003
Côté P, Cassidy JD, Yong-Hing K et al (1997) Apophysial joint degeneration, disc degeneration, and sagittal curve of the cervical spine. Can they be measured reliably on radiographs? Spine (Phila Pa 1976) 22:859–864
Deviren V, Scheer JK, Ames CP (2011) Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine 15:174–181. https://doi.org/10.3171/2011.3.SPINE10536
Diebo BG, Challier V, Henry JK et al (2016) Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine (Phila Pa 1976) 41:1795–1800. https://doi.org/10.1097/BRS.0000000000001698
Emery SE (2001) Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg 9:376–388
Etame AB, Wang AC, Than KD et al (2010) Outcomes after surgery for cervical spine deformity: review of the literature. Neurosurg Focus 28:E14. https://doi.org/10.3171/2010.1.FOCUS09278
Faline A, Szadkowski S, Berthonnaud E et al (2007) Morphological study of the lower cervical curvature: results of 230 asymptomatic subjects. Eur Spine J 16:25
Fehlings MG, Smith JS, Kopjar B et al (2012) Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study. J Neurosurg Spine 16:425–432. https://doi.org/10.3171/2012.1.SPINE11467
Fineman S, Borrelli FJ, Rubinstein BM, Epstein H, Jacobson HG (1963) The cervical spine: Transformation of the normal lordotic pattern into a linear pattern in the neutral posture. J Bone Joint Surg Am 45:1179–1183
Gao R, Yang L, Chen H et al (2012) Long term results of anterior corpectomy and fusion for cervical spondylotic myelopathy. PLoS ONE 7:e34811. https://doi.org/10.1371/journal.pone.0034811
Ghobrial GM, Lebwohl NH, Green BA, Gjolaj JP (2018) Changes in cervical alignment after multilevel Schwab grade II thoracolumbar osteotomies for adult spinal deformity. Spine (Phila Pa 1976) 43:E82–E91. https://doi.org/10.1097/BRS.0000000000002238
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688. https://doi.org/10.1097/01.brs.0000155425.04536.f7
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976) 26:2463–2466
Han K, Lu C, Li J et al (2011) Surgical treatment of cervical kyphosis. Eur Spine J 20:523–536. https://doi.org/10.1007/s00586-010-1602-8
Hann S, Chalouhi N, Madineni R et al (2014) An algorithmic strategy for selecting a surgical approach in cervical deformity correction. Neurosurg Focus 36:E5. https://doi.org/10.3171/2014.3.FOCUS1429
Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 22:1472–1480. https://doi.org/10.1097/00007632-199707010-00010
Harrison DED, Harrison DED, Cailliet R et al (2000) Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976) 25:2072–2078
Heath PM (1911) Deformity of the cervical spine. Proc R Soc Med 4:105
Herbert J (1959) Vertebral osteotomy for kyphosis, especially in Marie-Strumpell arthritis; a report on fifty cases. J Bone Joint Surg Am 41–A:291–302 passim
Hey HWD, Lau ET-C, Wong CG et al (2017) Cervical alignment variations in different postures and predictors of normal cervical kyphosis—a new understanding. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000002160
Hoh DJ, Khoueir P, Wang MY (2008) Management of cervical deformity in ankylosing spondylitis. Neurosurg Focus 24:E9. https://doi.org/10.3171/FOC/2008/24/1/E9
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J 25:1–8. https://doi.org/10.1007/s00586-016-4485-5
Iyer S, Nemani VM, Nguyen J et al (2016) Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976) 41:371–377. https://doi.org/10.1097/BRS.0000000000001221
Kandasamy R, Abdullah JM (2016) Cervical spine deformity correction: an overview. World Neurosurg 91:640–641. https://doi.org/10.1016/j.wneu.2016.04.109
Kim K-T, Lee S-H, Son E-S et al (2012) Surgical treatment of „chin-on-pubis“ deformity in a patient with ankylosing spondylitis: a case report of consecutive cervical, thoracic, and lumbar corrective osteotomies. Spine (Phila Pa 1976) 37:E1017–E1021. https://doi.org/10.1097/BRS.0b013e31824ee031
Kim HJ, Piyaskulkaew C, Riew KD (2014) Anterior cervical osteotomy for fixed cervical deformities. Spine (Phila Pa 1976) 39:1751–1757. https://doi.org/10.1097/BRS.0000000000000502
Kim HJ, Piyaskulkaew C, Riew KD (2015) Comparison of Smith-Petersen osteotomy versus pedicle subtraction osteotomy versus anterior-posterior osteotomy types for the correction of cervical spine deformities. Spine (Phila Pa 1976) 40:143–146. https://doi.org/10.1097/BRS.0000000000000707
Kim HJ, Lafage R, Elysee J et al (Unpubl. Data) The Morphology of Cervical Deformities A Two-Step Cluster analysis to Identify Cervical Deformity Patterns
Koller H, Meier O, Zenner J et al (2013) Non-instrumented correction of cervicothoracic kyphosis in ankylosing spondylitis: a critical analysis on the results of open-wedge osteotomy C7-T1 with gradual Halo-Thoracic-Cast based correction. Eur Spine J 22:819–832. https://doi.org/10.1007/s00586-012-2596-1
Lafage R, Challier V, Liabaud B et al (2016) Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and McGregor’s slope with health-related quality of life. Neurosurgery 79:108–115. https://doi.org/10.1227/NEU.0000000000001193
Lafage R, Kim HJ, Elysee J et al (2018) Radiographic characteristics of cervical deformity (CD) using a discriminant analysis: the value of extension radiographs. Cerv. Spine Res. Soc. 34th Annu. Meet..
Lee JS, Youn MS, Shin JK et al (2015) Relationship between cervical sagittal alignment and quality of life in ankylosing spondylitis. Eur Spine J 24:1199–1203. https://doi.org/10.1007/s00586-014-3491-8
Liu Z, Li X-F, Zang W-P et al (2009) Combined pedicle subtraction osteotomy and polysegmental closing wedge osteotomy for correction of the severe thoracolumbar kyphotic deformity in ankylosing spondylitis. Zhonghua Wai Ke Za Zhi 47:681–684
Liu S, Lafage R, Smith JS et al (2014) The impact of dynamic alignment, motion, and center of rotation on myelopathy grade and regional disability in cervical spondylotic myelopathy. Int. Meet. Adv. Spine Tech. (IMAST), 16.–19.07.2014
Liu X, Yuan S, Tian Y et al (2015) Expanded eggshell procedure combined with closing-opening technique (a modified vertebral column resection) for the treatment of thoracic and thoracolumbar angular kyphosis. J Neurosurg Spine 23:42–48. https://doi.org/10.3171/2014.11.SPINE14710
Lu DC, Chou D (2007) Flatback syndrome. Neurosurg Clin N Am 18:289–294. https://doi.org/10.1016/j.nec.2007.01.007
Mason C, Cozen L, Adelstein L (1953) Surgical correction of flexion deformity of the cervical spine. Calif Med 79:244–246
McAfee PC, Regan JJ, Bohlman HH et al (1987) Cervical cord compression from ossification of the posterior longitudinal ligament in non-orientals. J Bone Joint Surg Br 69:569–575
McMaster MJ (1997) Osteotomy of the cervical spine in ankylosing spondylitis. J Bone Joint Surg Br 79:197–203. https://doi.org/10.1302/0301-620X.79B2.7095
Mehdian S, Arun R (2011) A safe controlled instrumented reduction technique for cervical osteotomy in ankylosing spondylitis. Spine (Phila Pa 1976) 36:715–720. https://doi.org/10.1097/BRS.0b013e3181fc1a5e
Moore RE, Dormans JP, Drummond DS et al (2009) Chin-on-chest deformity in patients with fibrodysplasia ossificans progressiva. A case series. J Bone Joint Surg Am 91:1497–1502. https://doi.org/10.2106/JBJS.H.00554
Mummaneni PV, Dhall SS, Rodts GE, Haid RW (2008) Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine 9:515–521. https://doi.org/10.3171/SPI.2008.10.08226
Nagle DB (1957) Whiplash injuries of the cervical spine. Radiology 69:823–827. https://doi.org/10.1148/69.6.823
Nemani VM, Derman PB, Kim HJ (2016) Osteotomies in the cervical spine. Asian Spine J 10:184–195. https://doi.org/10.4184/asj.2016.10.1.184
Nottmeier EW, Deen HG, Patel N, Birch B (2009) Cervical kyphotic deformity correction using 360-degree reconstruction. J Spinal Disord Tech 22:385–391. https://doi.org/10.1097/BSD.0b013e318180e672
Obeid I, Boissière L, Vital J-M (2013) C4 anterior cervical corpectomy with fusion for cervical spondylotic myelopathy. Eur Spine J 22:2907–2909. https://doi.org/10.1007/s00586-013-3102-0
O’Shaughnessy BA, Liu JC, Hsieh PC et al (2008) Surgical treatment of fixed cervical kyphosis with myelopathy. Spine (Phila Pa 1976) 33:771–778. https://doi.org/10.1097/BRS.0b013e3181695082
Passias PG, Soroceanu A, Smith J et al (2015) Postoperative cervical deformity in 215 thoracolumbar patients with adult spinal deformity. Spine (Phila Pa 1976) 40:283–291. https://doi.org/10.1097/BRS.0000000000000746
Passias PG, Jalai CM, Smith JS et al (2017) Characterizing adult cervical deformity and disability based on existing cervical and adult deformity classification schemes at presentation and following correction. Neurosurgery. https://doi.org/10.1093/neuros/nyx175
Post N, Naziri Q, Cooper C et al (2015) Pedicle reduction osteotomy in the upper cervical spine: technique, case report and review of the literature. Int J Spine Surg 9:57. https://doi.org/10.14444/2057
Rhee JM, Yoon T, Riew KD (2007) Cervical radiculopathy. J Am Acad Orthop Surg 15:486–494
Samudrala S, Vaynman S, Thiayananthan T et al (2010) Cervicothoracic junction kyphosis: surgical reconstruction with pedicle subtraction osteotomy and Smith-Petersen osteotomy. Presented at the 2009 Joint Spine Section Meeting. Clinical article. J Neurosurg Spine 13:695–706. https://doi.org/10.3171/2010.5.SPINE08608
Sevastikoglou JA, Bergquist E (1969) Evaluation of the reliability of radiological methods for registration of scoliosis. Acta Orthop Scand 40:608–613. https://doi.org/10.3109/17453676908989526
Sharan AD, Krystal JD, Singla A et al (2015) Advances in the understanding of cervical spine deformity. Instr Course Lect 64:417–426
Smith JS, Klineberg E, Shaffrey CI et al (2016) Assessment of surgical treatment strategies for moderate to severe cervical spinal deformity reveals marked variation in approaches, osteotomies, and fusion levels. World Neurosurg 91:228–237. https://doi.org/10.1016/j.wneu.2016.04.020
Smith JS, Lafage V, Ryan DJ et al (2013) Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976) 38:S161–S170. https://doi.org/10.1097/BRS.0b013e3182a7eb9e
Smith JS, Line B, Bess S et al (2017) The health impact of adult cervical deformity in patients presenting for surgical treatment: comparison to United States population norms and chronic disease states based on the EuroQuol-5 Dimensions Questionnaire. Neurosurgery 80:716–725. https://doi.org/10.1093/neuros/nyx028
Smith JS, Shaffrey CI, Bess S et al (2017) Recent and emerging advances in spinal deformity. Neurosurgery 80:70–S85. https://doi.org/10.1093/neuros/nyw048
Smith JS, Shaffrey CI, Lafage V et al (2012) Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine 17:300–307. https://doi.org/10.3171/2012.6.SPINE1250
Smith-Petersen MN, Larson CCB, Aufranc OOE et al (1945) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg Am 27:1–11
Steinmetz MP, Stewart TJ, Kager CD et al (2007) Cervical deformity correction. Neurosurgery 60:90–97. https://doi.org/10.1227/01.NEU.0000215553.49728.B0
Tan LA, Riew KD (2017) Anterior cervical osteotomy: operative technique. Eur Spine J. https://doi.org/10.1007/s00586-017-5163-y
Tan LA, Riew KD, Traynelis VC (2017) Cervical spine deformity-part 1: biomechanics, radiographic parameters, and classification. Neurosurgery 81:197–203. https://doi.org/10.1093/neuros/nyx249
Tokala DP, Lam KS, Freeman BJC, Webb JK (2007) C7 decancellisation closing wedge osteotomy for the correction of fixed cervico-thoracic kyphosis. Eur Spine J 16:1471–1478. https://doi.org/10.1007/s00586-006-0290-x
Urist MR (1958) Osteotomy of the cervical spine; report of a case of ankylosing rheumatoid spondylitis. J Bone Joint Surg Am 40-A:833–843
Vaněk P, Votavová M, Ostrý S et al (2014) Correction of kyphotic deformity of the cervical spine in ankylosing spondylitis using pedicle subtraction osteotomy of the seventh cervical vertebra. Acta Chir Orthop Traumatol Cech 81:317–322
Wang VY, Aryan H, Ames CP (2008) A novel anterior technique for simultaneous single-stage anterior and posterior cervical release for fixed kyphosis. J Neurosurg Spine 8:594–599. https://doi.org/10.3171/SPI/2008/8/6/594
Weinberg D, Chugh A, Gebhart J, Eubanks J (2016) Magnetic resonance imaging of the cervical spine under-represents sagittal plane deformity in degenerative myelopathy patients. Int J Spine Surg 10:1–9. https://doi.org/10.14444/3032
Whiteleather JE, Semmes RE, Murphey F (1946) The roentgenographic signs of herniation of the cervical intervertebral disk. Radiology 46:213–219. https://doi.org/10.1148/46.3.213
Wollowick AL, Kelly MP, Riew KD (2012) Pedicle subtraction osteotomy in the cervical spine. Spine (Phila Pa 1976) 37:E342–E348. https://doi.org/10.1097/BRS.0b013e318245bcd4
Wood J (1863) Case of extreme deformity of the neck and forearm, from the cicatrices of a burn, cured by extension, excision, and transplantation of skin, adjacent and remote. Med Chir Trans 46:149–159
Yang Y, Liu B, Rong L et al (2016) Correction of thoracolumbar kyphoscoliosis by modified „eggshell“ osteotomy. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 30:72–76
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B.G. Diebo, N.V. Shah, M. Solow, V. Challier, C.B. Paulino, P.G. Passias, R. Lafage, V. Lafage, F.J. Schwab, and H.J. Kim declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Diebo, B.G., Shah, N.V., Solow, M. et al. Adult cervical deformity: radiographic and osteotomy classifications. Orthopäde 47, 496–504 (2018). https://doi.org/10.1007/s00132-018-3581-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-3581-0