Abstract
Purpose
Little information is available on the relationship between cervical sagittal alignment and health-related quality of life (HRQOL) in ankylosing spondylitis (AS) patients. The aim of this study was to identify relationships between cervical sagittal alignment and HRQOL in AS.
Methods
The study and control groups comprised 102 AS patients (15 women and 87 men) and age- and sex-matched 50 controls, respectively. All underwent anteroposterior and lateral radiographs and completed clinical questionnaires. The radiographic parameters examined were C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA), T1 slope and T1 slope minus C2–C7 lordosis (TS-CL). A visual analogue scale (VAS 0–10) score for neck pain, the neck disability index (NDI), neck pain and disability (NPAD) scale and bath ankylosing spondylitis disease activity index (BASDAI) were administered to evaluate QOL. Statistical analysis was performed to determine the significances of differences between the study and control groups. In addition, correlations between radiological parameters and clinical questionnaires were sought.
Results
AS patients and controls were found to be different significantly in terms of C2–C7 SVA, T1 slope, and TS-CL. However, no significant intergroup difference was observed for C2–C7 lordosis (P > 0.05). Correlation analysis revealed significant relationships between radiographic parameters and QOL. Multiple regression analysis was performed to identify predictors of QOL, and the results obtained revealed that C2–C7 SVA significantly predicted VAS, NDI, and NPAD scores and that age predicted NPAD score.
Conclusions
Cervical sagittal parameters were found to be significantly different in AS patients and normal controls. Correlation analysis revealed significant relationships between radiographic parameters and QOL. In particular, C2–C7 SVA was found to be a significant predictor of QOL in AS patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a chronic, inflammatory rheumatic disease characterized by the formation of syndesmophytes leading to ankylosis and inflammatory back pain due to sacroiliitis and spondylitis [21], and it is believed to be the most common and typical form of spondyloarthropathy [2]. The advanced stages of the disease are characterized by progressive stiffening of the spine and thorax [20], and during the course of the disease, sagittal balance deteriorates to produce rigid thoracolumbar kyphosis [20], which when severe results in downward tilting of the head and face [20]. Furthermore, ability to see above the level of horizontal gaze progressively worsens [4], and the center of gravity moves anteriorly to cause a stooped, downward-looking posture, which is characteristic of advanced AS [4], and which contributes to many disabilities and limits social activities.
Although thoracolumbar kyphotic deformities are most common, the cervical and/or upper thoracic spines can also be involved, and the resulting cervical kyphosis can be extremely debilitating because of the development of chin-on-chest deformity with significant compromise of horizontal gaze [1, 13]. Neurologic deficits can also arise in addition to other debilitating symptoms, such as, limitations of speech and/or the ability to swallow [13]. Therefore, we considered that knowledge of correlations between cervical sagittal alignment and health-related quality of life (HRQOL) would provide information useful for treatment decision making and planning in AS.
Correlations between HRQOL and sagittal spinal alignment parameters, including spinopelvic parameters, have been previously reported, and some authors have reported on the importance of cervical sagittal balance [6, 9, 15]. However, no relationships have been established between cervical sagittal alignment and HRQOL in AS. Accordingly, the aim of this study was to identify relationships between cervical sagittal parameters and HRQOL in AS patients. In addition, we attempted to identify cervical sagittal parameters that predict HRQOL.
Materials and methods
One hundred and two consecutive AS patients were prospectively enrolled at times of examinations conducted between January 2012 and February 2013 at an orthopaedic outpatient clinic. Demographic and clinical characteristics and visual analogue scale (VAS 0–10) scores for neck pain were recorded, and the neck disability index (NDI) [18], neck pain and disability (NPAD) scale [12], and bath ankylosing spondylitis disease activity index (BASDAI) were administered. BASDAI is a composite index comprising visual analogue scale (1–10) based assessments of fatigue, axial pain, peripheral pain, stiffness, and enthesopathy [3]. 15 female and 87 male AS patients of average age 42.9 ± 13.3 years were recruited. 50 age- and sex-matched normal subjects that underwent whole spine radiographs during health checkups were recruited as controls. The study was approved by the Clinical Research Ethics Committee of our institution.
All 102 AS patients met the most recent modified New York criteria [19] and were eligible to participate if they had received medical treatment for at least 1 year. Pain originating from the neck (cervical spine) was scored, but pain originating from other parts of the body, such as, hips, knees, or shoulders was excluded. The exclusion criteria applied were an age older than 60 or concomitant neurological or psychiatric disease. Patients with a history of or orthopaedic disease of the spine (fracture, spinal disc herniation, spinal surgery, etc.) or lower extremities (e.g., prosthesis) were also excluded.
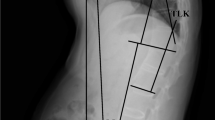
Participants underwent anteroposterior and lateral radiography. Radiographs were taken by one technician at a distance of 72 inches using a standard technique and the same machine in the standing position. Radiographic parameters examined included C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA), T1 slope, and T1 slope minus C2–C7 lordosis (TS-CL) (Fig. 1). C2–C7 SVA was defined as the distance between the C2 and the C7 sagittal plumb lines. The C2 sagittal plumb line was drawn with a lateral gravity line from the center of C2. The center of C2 was defined as the point of intersection of crossing diagonals of the vertebral body of C2 on a lateral radiograph. The C7 sagittal plumb line was defined as the lateral gravity plumb line from the center of C7. Anterior displacement of the sagittal plumb line was defined as positive. T1 slope was defined as an angle formed between the T1 upper end plate and the horizontal plane. All measurements were performed twice independently by three spine surgeons with an interval of 2 weeks between measurements to decrease intraobserver (Pearson’s correlation coefficient = 0.935, range 0.900–0.955) and interobserver errors (Pearson’s correlation coefficient = 0.929, range 0.895–0.951).
Statistical analysis was performed using SPSS ver. 11.5 for Windows (SPSS, Chicago, IL, USA). Results are expressed as means ± standard deviations. The patient and control groups were compared using the t test and correlation analysis was performed using Pearson’s correlation to explore relationships between variables. Multiple regression analysis was used to identify parameters that predicted QOL. P values of <0.05 were deemed statistically significant.
Results
Measurements of cervical sagittal parameters
Table 1 summarizes sagittal parameter measurements in the 102 AS patients and 50 age- and sex-matched controls. Patients and controls were found to be significantly different in terms of C2–C7 SVA, T1 slope, and TS-CL. However, no significant intergroup difference was observed for C2–C7 lordosis (P > 0.05).
Correlation between cervical sagittal parameters
Table 2 summarizes correlations between cervical sagittal parameters. Statistical significant correlations were observed between the following variables after stratification (Fig. 2): C2–C7 lordosis and C2–C7 SVA (r = 0.485, P = 0.004), C2–C7 lordosis and T1 slope (r = 0.786, P < 0.001), C2–C7 lordosis and TS-CL (r = −0.372, P = 0.03), C2–C7 SVA and T1 slope (r = 0.825, P < 0.001), and C2–C7 SVA and TS-CL (r = 0.486, P = 0.004).
Correlation between cervical sagittal parameters and HRQOL
Correlation analysis also revealed significant relationships between cervical sagittal parameters and QOL (Table 3). However, TS-CL was not found to be correlated with any of the four QOL scores and BASDAI was not correlated with the any of the cervical sagittal parameters.
Multiple regression analysis was performed to identify predictors of QOL, and showed C2–C7 SVA significantly predicted VAS, NDI, and NPAD, and that age significantly predicted NPAD (Table 4).
Discussion
Although the treatment of cervical spinal deformities associated with AS has become an increasingly important component in many spinal surgery practices, the relevance of cervical sagittal balance in AS remains unclear. Earlier studies addressed the surgical management of cervical deformities in AS [5, 8, 14], and some authors have investigated cervical alignment to predict the development of adjacent segment disease after anterior cervical surgery [15, 17]. However, relatively few studies have addressed relations between AS and specific radiologic cervical parameters. Furthermore, the relationships established between cervical sagittal parameters and HRQOL in AS are lacking.
Standing C2–C7 SVAs are closely maintained in a tight range in the normal cervical spine [7, 10, 11]. In particular, C2–S1 and C7–S1 SVAs are maintained to ensure alignment of the spine over the pelvis and femoral heads [11]. In degenerative cervical diseases, some parameters, that is, C2–C7 lordosis, C2–C7 SVA, T1 slope, and TS-CL, can be used to assess cervical sagittal balance [15, 17]. Therefore, if cervical sagittal parameters are changed by disease, one could theorize that alterations in cervical sagittal alignment might affect clinical outcomes.
Park et al. [15] suggested that malalignment of the cervical spine following anterior cervical surgery affects the development of clinical adjacent segment pathology requiring surgery. Faldini et al. [6] found that malalignment after cervical arthrodesis promotes degenerative changes at levels adjacent to fused segments; adjacent segment degeneration was found in 27 and 60 % of cases fused in lordosis or kyphosis, respectively. Katsuura et al. [9] evaluated 42 patients that underwent anterior cervical interbody fusion surgery using lateral radiographs of the cervical spine, and diagnosed radiographically adjacent segment pathology when radiographic findings were consistent with symptoms and signs. It was found that overall cervical sagittal alignments in postoperative radiographs were more kyphotic in patients with radiographically adjacent level degeneration. And Shin et al. [16] reported that there are significant relationships between global sagittal spinopelvic parameters and clinical outcomes in AS patients. Before we initiated the present study, we felt that a similar relation might be found by assessing sagittal balance in the cervical spine. To the best of our knowledge, no study has been previously conducted to determine relations between cervical sagittal parameters and HRQOL of the cervical spine in AS.
In the present study, cervical sagittal parameters were found to be significantly different in AS patients and controls, and to be related to each other. Although no correlations between cervical sagittal parameters and the development of spinal disorders have been confirmed in AS, differences and relationships between sagittal radiological parameters can provide clues when examining cervical spinal deformities in AS. In the present study, AS patients exhibited higher levels of C2–C7 SVA, T1 slope, and TS-CL, which suggests that cervical sagittal orientation is significantly different in AS. In addition, mean C2–C7 SVA in AS was more positive than in controls. Thus, it appears that cervical spinal misalignments are closely related in AS. However, no significant intergroup difference was observed for C2–C7 lordosis. Hyperextension of C0–C1 and/or C1–C2 joint might have occurred to compensate the increased T1 slope of AS patients.
Few studies have addressed relationships between HRQOL instruments and cervical sagittal measurements. However, these cervical parameters could be significantly correlated with HRQOL measures, and thus, could be important when analyzing radiographic alignment. In the present study, QOL scores were found to be significantly correlated with C2–C7 lordosis, C2–C7 SVA, and T1 slope. In fact, in the present study, multiple regression analysis showed C2–C7 SVA (defined as the distance between the C2 and the C7 sagittal plumb lines) was significantly related to HRQOL and a significant predictor of QOL. Furthermore, NPAD score was significantly influenced by age, which suggests younger patients are better able to control cervical pain. These findings indicate spinal misalignment is closely related to QOL and increases pain severity in AS, and suggest that spinal misalignment could be considered by surgeons when treating AS.
This study has several limitations that require consideration. First, the number of normal controls tested was relatively small, which diminished the statistical power of the study and its ability to detect correlations. Second, other radiological measurements (e.g., global sagittal balance) that could affect HRQOL were not included. Third, we did not examine interactions with hematologic factors, such as, erythrocyte sedimentation rate or C-reactive protein levels, and these considerations are important in AS because they influence pain.
Nonetheless, this study shows significant relationships exist between cervical sagittal parameters in AS patients, and that the cervical sagittal parameters of AS patients and normal controls differ significantly. Furthermore, correlation analysis revealed significant relationships between cervical sagittal parameters and QOL scores. In particular, C2–C7 SVA was found to significantly predict QOL in AS patients.
References
Belanger TA, Milam RA 4th, Roh JS, Bohlman HH (2005) Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. J Bone Jt Surg Am 87:1732–1738
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, Jenkinson T (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the bath ankylosing spondylitis functional index. J Rheumatol 21:2281–2285
Debarge R, Demey G, Roussouly P (2010) Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur Spine J 19:65–70
Etame AB, Than KD, Wang AC, La Marca F, Park P (2008) Surgical management of symptomatic cervical or cervicothoracic kyphosis due to ankylosing spondylitis. Spine 33:E559–E564
Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S (2011) Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res 469:674–681
Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22:1472–1480
Hoh DJ, Khoueir P, Wang MY (2008) Management of cervical deformity in ankylosing spondylitis. Neurosurg Focus 24:E9
Katsuura A, Kukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324
Knott PT, Mardjetko SM, Techy F (2010) The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 10:994–998
Kuntz C 4th, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ (2007) Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine 6:104–112
Lee JS, Suh KT, Kim JI, Lee HS, Goh TS (2013) Validation of the Korean version of the neck pain and disability scale. Asian Spine J 7:178–183
McMaster MJ (1997) Osteotomy of the cervical spine in ankylosing spondylitis. J Bone Jt Surg Br 79:197–203
Mehdian SM, Boreham B, Hammett T (2012) Cervical osteotomy in ankylosing spondylitis. Eur Spine J 21:2713–2717
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD (2013) Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J (in press)
Shin JK, Lee JS, Goh TS, Son SM (2014) Correlation between clinical outcome and spinopelvic parameters in ankylosing spondylitis. Eur Spine J 23:242–247
Song JS, Choi BW, Song KJ (2013) Risk factors for the development of adjacent segment disease following anterior cervical arthrodesis for degenerative cervical disease: Comparison between fusion methods. J Clin Neurosci (in press)
Song KJ, Choi BW, Choi BR, Seo GB (2010) Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine 20:E1045–E1049
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
White AA 3rd, Panjabi MM, Thomas CL (1977) The clinical biomechanics of kyphotic deformities. Clin Orthop Relat Res 128:8–17
Zochling J, van der Heijde D, Burgos-Vargas R, Collantes E, Davis JC Jr, Dijkmans B, Dougados M, Géher P, Inman RD, Khan MA, Kvien TK, Leirisalo-Repo M, Olivieri I, Pavelka K, Sieper J, Stucki G, Sturrock RD, van der Linden S, Wendling D, Böhm H, van Royen BJ, Braun J (2006) ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis 65:442–452
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.S., Youn, M.S., Shin, J.K. et al. Relationship between cervical sagittal alignment and quality of life in ankylosing spondylitis. Eur Spine J 24, 1199–1203 (2015). https://doi.org/10.1007/s00586-014-3491-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3491-8