Abstract
This paper discusses otorhinolaryngological symptoms associated with functional disorders of the upper cervical spine. Hints aimed to avoid misdiagnoses of cross-organ otorhinolaryngological symptoms as phobic or psychogenic disorders are presented. Clinically relevant neuroanatomical convergence of the upper cervical spine (occiput to C3) is fundamental for the interpretation of functional otorhinolaryngological symptoms. Based thereon, evidence for the most common cervical differential diagnoses of dizziness, tinnitus, dysphagia, and craniomandibular dysfunction is presented separately. The corresponding therapeutic options and their contraindications are discussed in the concluding chapter. The importance of interdisciplinary cooperation in related fields is emphasized.
Zusammenfassung
Der vorliegende Artikel beschäftigt sich mit denjenigen Symptombildern aus dem HNO-ärztlichen Behandlungsgebiet, die auf funktionelle Störungen der oberen Halswirbelsäule zurückgeführt werden können. Es werden Hinweise gegeben, wann Vorsicht geboten ist, organübergreifende HNO-Symptome vorschnell als phobisch oder psychogen einzustufen. Als Grundlage für funktionelle Symptome im HNO-Bereich werden einleitend die klinisch relevanten neuroanatomischen Konvergenzen der oberen Halswirbelsäule (Okziput bis C3) aufgezeigt. Darauf aufbauend werden separat empirische und evidenzbasierte Charakteristika der wichtigsten zervikalen Differenzialdiagnosen von Schwindel, Tinnitus, Schluckstörungen und kraniomandibulärer Dysfunktion dargestellt. Die zugehörigen Therapieoptionen und deren Kontraindikationen werden im abschließenden Kapitel abgehandelt. Hervorgehoben wird die Bedeutung der interdisziplinären Zusammenarbeit der angrenzenden Fachgebiete.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
Generate understanding of the neuroanatomical foundation of the craniovertebral joints
-
Illustrate connections of the spinal cord to the trigeminal nucleus of the spinal cord
-
Illustrate connections of the spinal cord to the temporomandibular joint
-
Elucidate the differentiation between functional and structural disorders
-
Identify functional therapy options
Definition of the upper cervical spine
The cervical spine is not a unitary system, but is divided into the craniovertebral joints (occiput to C3) and the lower cervical spine (C3 to C7). The difference is manifested in the morphology and joint mechanics as well as in the muscle dynamics and neurophysiology [1].
The segments of the craniovertebral joints comprise the atlanto-occipital joint (Oc-C1) and the atlantoaxial joint (C1/C2). In addition, C2/C3 must be accounted for as an additional part of the system in neuroanatomical, functional, and clinical terms, because the cervico-trigeminal neuroanatomy, described below, converges toward the spinal trigeminal nucleus from the cervical spinal roots of C1–C3.
The muscle groups of the suboccipital musculature show an uncommonly high population of muscle spindle: The region of the craniovertebral joints is virtually a sensory organ for the perception of body position and movement in the three-dimensional environment. These muscles contain up to 312 muscle spindles per gram of muscle tissue (normal averaging at about 30 muscle spindles per gram muscle tissue; [2]).
The craniovertebral joint region is a sensory organ for the perception of body position and movement
For the most part, afferent fibers originating from muscle spindles and tendon organs terminate in the central cervical nucleus (CCN). The main responsibility of this nucleus is the activation of interneurons, especially for the activation of the m. longissimus dorsi down to the lumbar region—thus, in summary, for control of upright motion [3].
The segmental nerves of the craniovertebral joints are as follows [4]:
C1: Suboccipital nerve
-
This nerve is not associated with a distinct dermatome. However, it gives off a meningeal ramus to the dura in the area of the clivus. C1 does not have a dorsal root, the deep somatic afferent fibers (e. g., from the joint occiput/C1) run via an anastomosis from the major occipital nerve to the dorsal root of C2.
-
The suboccipital nerve innervates the Mm. obliquus capitis superior/inferior as well as Mm. rectus capitis posterior minor/major.
-
The nerve also innervates the atlas indentations of some long extensors of the neck (e. g., m. splenius) with dorsal rami.
-
It contains the deep somatic afferences of all the aforementioned structures.
C2: Greater occipital nerve (dorsal root)
-
This nerve contains fibers deriving from C3 and innervates a large occipital dermatome. In addition, it innervates—as has been mentioned for C1—parts of the posterior dura.
-
In conjunction with C1, it innervates almost all atlas muscles.
-
The dorsal root ganglion of C2 is situated directly next to the C1/C2 joint and may be irritated by osteophytes.
-
The efferent motoric fibers innervate parts of the so-called autochthonic muscles (m. semispinalis capitis, m. longissimus capitis, and m. splenius capitis).
C2: Lesser occipital nerve (anterior root)
-
The sensory area innervated comprises the posterior head.
-
The motor neurons (including the C3 nerves) innervate the anterior cervical muscles (m. longus capitis, m. rectus capitis anterior/lateralis).
C3: Third occipital nerve (TON)
-
This nerve innervates a small dermatome situated occipitally and suboccipitally including an area anterior to the ear (terminal branch: greater auricular nerve).
-
The motor neurons innervate the atlas indentations of the levator scapulae muscle and the longissimus cervicis muscle with its anterior branch.
-
It sends dorsal sensory branches to the cervical joints of C3.
The aforementioned spinal nerves send afferent neurons to the medulla oblongata. Here, they send unfiltered convergences to the reticular formation and to different cranial nerves—especially the trigeminal nerve. Included are also close convergences of the facial nerve, glossopharyngeal nerve, vagus nerve, accessory nerve (roots of C1–C3), and hypoglossal nerve [5].
Consequently, the brain stem forms the sensory center for coordinating balance and movement against gravity.
For our contemplation of the joints between the head bones and the first vertebrae and their connections with the cranial nerves, the segments C1–C3 are of special importance. These connections are intimately associated with the spinal nucleus of the trigeminus from the medulla upward: The distinct areas of the three cervical segments and the trigeminal structures are grouped in a chess-board-like arrangement and are interconnected with numerous interneurons. This is true for dermal afferences as well as afferences from muscles, joints, and bones. This exchange of afferent information exists not only for the spinal trigeminal nucleus but also for the vestibular complex [6] and the cochlear nuclei [7]. These projections intersect at the central cervical nucleus and reach the cerebellum (Fig. 1).
Conclusion.
For years there has been a feasible neuroanatomic model for various otolaryngological symptoms. However, in scientific terms the underlying pathophysiology is under debate.
In the following, empirical and evidence-based characteristics for the most common cervical differential diagnoses are reviewed.
Cervical vertigo
The existence of a phenomenon called “cervical vertigo” or “cervicogenic dizziness” represents an academic feud with a fine tradition. Interesting neuroanatomic vestibulocervical facts have arisen in recent years. These may have the potential to shed new light on this topic.
Longstanding neurologic doubts about the existence of vestibulocervical disturbances have recently been discussed in a new light in the neurologic literature [8]. The otolaryngeal association with the craniocervical junction is as follows:
The peripheral vestibular organ also is a generator for motor action potentials for the reflectory motor innervation especially for the muscles of the craniovertebral joints.
The postural regulation mediated via the lateral vestibulospinal tract is known as the vestibulospinal reaction and the latter is accessible to manual therapy [9]. The distinct importance of this vestibular key competence is recognizable by the fact that there exists a distinct neuronal connection to the muscles of the craniovertebral joints. Via the medial vestibulospinal tract, a direct innervation from the vestibular nuclei to the motor neurons of the axial musculature of the joints between the head bones and the first cervical vertebrae is mediated ([10]; Table 1). This innervation from the vestibular nuclei then interacts with the cortical innervation on a spinal level (via the pyramidal tract) and the extrapyramidal impulses.
For optimized motor control, the vestibulocervical efference is in need of intensive cervicovestibular afference from proprioceptors of the craniovertebral joints. These are needed to close the reflex loop of head–body coordination. In addition, they can help coordinate vestibular compensation mechanisms in clinical daily routine. One of the ground-breaking publications on the cervicovestibular afferences was presented by Cullen et al. in 2012 [18]. They performed labyrinthectomies in monkeys and found a weak vestibulo-ocular reflex after 3 weeks even without a vestibular organ. The authors attributed this phenomenon to cervicovestibular compensation mechanisms.
The center of gravity of the head lies in front of the upper cervical joint axes
In 2010 Matyssek reported that the center of gravity of the head is situated anterior to the axes of the upper cervical joints [19]. As a result, a continuous vestibulocervical resting tone is needed to adjust head position from occipital direction—even in static movement phases. If the occipital musculature stops working, the head tilts toward the sternum (e. g., falling asleep in a sitting position). In dynamic scenarios, all head accelerations have to be coordinated by minute neuro-otologically controlled correctional movements in a three-dimensional system [20,21,22,23,24].
For didactic purposes, the authors classify the vestibular system into relevant intra- and extracranial sensors (Table 2).
In clinical daily routine, there are no specific key points to reveal cervicogenic vertigo. One explanation could be that the neuronal complexity leads to unspecific anamnestic clues. In addition, there may be a great inter-individual variance of compensating mechanisms. As a result, the evidence level for the characterization of cervical vertigo is low.
Conclusion.
Every movement of the body in three-dimensional space creates an acceleration of the head. As a result of the unfavorable balance point of the head, a vestibular-triggered regulation of muscle movement in the craniovertebral joints is needed to coordinate a stable gaze and a stable body position.
This results in the following possible definition of cervical vertigo:
A disturbed cervicovestibular proprioception in the craniovertebral joints results in a malfunction of neuro-otologically regulated coordination of minute accelerations of the head.
The associated manual therapy is discussed in detail.
Tinnitus
A significant somatosensory influence on the cochlear system was postulated at an early stage [25]. The clinical observations were then supported by neurophysiologic research [26, 27]. Over the years, the research performed by Shore et al. added insights into the influences of the cervical vertebral unit and the trigeminal nerve [28, 29]. The modulation capacity of tinnitus based on these analyses has been reproducible in up to 60% of all patients with tinnitus [30]!
As a result of these interrelations, practical examples can be cited such as chiropractic manipulations, massages of the cervical spine, or accidents with torsion trauma of the cervical spine that often result in tinnitus [31]. Patients often report that their tinnitus first occurred after dental treatments or trauma of the shoulder or thoracic spine etc. [30].
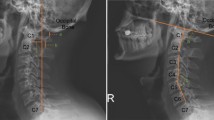
A case report may help clarify the characteristics of cervical tinnitus: A patient felt a growing restriction in head movement accentuated during head turning. He went to see a masseur. The latter diagnosed a “blockade” in C0/1 and mobilized this segment. The patient felt a sudden pain, tinnitus in the right ear, and vertigo. In addition, the patient had a sudden hearing loss in the low frequencies. The symptoms were caused by a previously undiagnosed bony abnormality in the C0/1 segment rendering functional therapy impossible and leading to injury of the previously neuropathological “silent” segment (Fig. 2).
Radiograph of the cervical spine, a.p., through the open mouth. Unilateral arthrosis in C0/C1 on the right side. (From [32])
Such a reflexive pathologic reaction is made possible by the monosynaptic interconnection between dorsal root neurons and the cochlear nuclei on a spinal level [33]. These afferences are mainly channeled via the roots of C2/3. This is underlined by the positive effects of de-afferentation of the dorsal root of C2/3, as published by Gritsenko et al. [34]. The case described here is a rare occurrence, but may serve as an “experimental clinical case” owing to the exemplary development of the symptoms. It is not clear yet which neuronal factors and processes lead to the clinical phenomenon of tinnitus. Inhibitive and reinforcing neuronal activation patterns have been described in animal experiments [28].
No specific audiological findings exist yet to characterize somatosensory tinnitus. A connection between tinnitus and the musculoskeletal system may be founded on the anamnestic description, as reported in the aforementioned case and the fact that of volume and frequency of the tinnitus may be influenced by distinct movements of the head, the temporomandibular joint, or by stimulation of certain pressure points.
Tinnitus may be influenced by arm and head movements
To make sure that the patient is able to perceive the distinct modulations in tinnitus, the testing must be performed in a soundproofed setting. Audiological testing should be standardized and the modulations of the tinnitus after provocation should be reproducible. A demonstration of a possible setting and testing may be viewed in the YouTube video “Biesinger somatosensorischer Tinnitus” [35].
If the tinnitus is modulated by reproducible structures or movements, these findings must lead to orthopedic diagnostic procedures and possible treatment by a physician and/or physiotherapist.
In treatment of cervical tinnitus, the targeted anesthesia of musculoskeletal structures (i. e., neural therapy) is of great importance. During the diagnostic testing of somatosensory tinnitus, conspicuous structures may be infiltrated with local anesthetic (e. g., lidocaine 1% without adrenaline) leading to a minimization or suppression of pathologic afferences. The anesthetization of the otic ganglion may be very effective in tinnitus originating from pathologic afferences in the trigeminal area [29]. This phenomenon is under investigation in a controlled study.
Conclusion.
There is such a wide spectrum of clinical references that a somatosensory component in the development of tinnitus should not be underestimated. In such cases, manual therapy of the functional disturbances of the craniovertebral joints and the temporomandibular joints must be undertaken (see below).
Dysphagia
Dysphagia comprises all painless restrictions in food intake and coordinated transport of food. Hence, it is more a symptom description than a diagnosis. The process of swallowing as a central function serves to transport saliva, secretions, fluid, and food from the mouth through the pharynx and esophagus to the stomach. Disorders of swallowing may stem from neurologic or muscular disturbances as well as oncologic or surgery-derived alterations in the head and neck area, the esophagus, or the stomach [36]. Cervicogenic swallowing disorders may be subdivided into three groups: functional disturbances of the cervical spine, morphological alterations of the cervical spine, and postoperative dysphagia after surgical procedures performed on the cervical spine. Functional disturbances of the cervical spine with dysphagia may present with a variation of symptoms; patients complain about persisting or variable pain during swallowing. In addition, patients experience the feeling of swallowing against resistance or a feeling of tightness or trepidation. Others describe a feeling as if a foreign body is present (globus).
Clinical examination usually begins with a functional endoscopic evaluation of swallowing. This may be completed with fluoroscopy or with a computed tomography scan or magnetic resonance imaging. The latter modalities aim at excluding oncologic causes of the dysphagia. If there is no evident cause for the dysphagia after these tests, a functional examination of the cervical spine is performed by palpating and segmentally examining the cervical spine. A snap judgement of the swallowing problems as psychogenic is not warranted. Seifert et al. even call a hasty diagnosis of “globus nervosus sive hystericus” wrong and therapeutically inefficient [37].
Our own clinical observations lead us to assume that cervicogenic dysphagia or globus often are caused by a functional, reflective disturbance within the cervical spine. They are mostly located within the craniovertebral joints. They usually develop independently of pathomorphologic disturbances or following the latter. Usually, they are fully reversible. If persisting, they can lead to pathomorphologic changes. Psychologic factors may also contribute to the development and persistence of functional swallowing disorders.
Patients with dysphagia often complain of pain during swallowing
The painful distensions of the muscle insertions on the hyoid bone are often caused by a functional disturbance of the craniovertebral joints (C0/C1 to C3/C4). This leads to a segmental hypomobility and hypertension of the muscles. This may cause the presenting symptom of odynophagia. Mostly, the C2/C3 and C3/C4 segments are the main segments causing dysphagia. The C3/C4 segment is mainly responsible for the globus or the sensation of swallowing against resistance. The main causes include wrong movement patterns, degenerative changes, or trauma as well as torsion trauma or distortions of the cervical spine. In addition, head trauma may lead to persisting functional disturbances of the cervical spine [37,38,39].
Consequently, treatment by a speech therapist may be less effective than manual therapy by a physiotherapist.
Conclusion.
Cervicogenic disorders of swallowing may be the least scientifically evaluated functional disturbances in the head and neck area. With adequate acceptance and attention, they could be diagnosed and treated on a broader basis.
Craniomandibular dysfunction
Craniomandibular dysfunction (CMD) is one of the most common chronic pain syndromes, in concert with chronic head, neck, or back pain. The prevalence of CMD is 3–5%. The high prevalence and the reduced quality of life render it an important socioeconomic factor. Craniomandibular dysfunction is a clearly defined musculoskeletal pain syndrome of the temporomandibular joint. The causes are multifactorial. Craniomandibular dysfunction is an umbrella term for a functional dysregulation of the masticatory muscles and the temporomandibular joints. Hence, it is associated with a broad variety of comorbidities and pain syndromes [40]. An important factor is the phylogenetic association of the temporomandibular joints and the craniovertebral joints. They form a cybernetic unit regulated by conjoint motoric programs via descending corticobulbar and corticospinal tracts. As a result, movements of the temporomandibular joints and the craniovertebral joints are performed in a coordinated fashion. Opening of the mouth is associated with extension of the upper cervical spine, closing of the mouth with a flexion of the upper cervical spine. CMD should not be examined as an isolated symptom but always in concert with a myofunctional disturbance of the upper cervical spine [41]. This explains why 80% of patients with CMD also present with a craniocervical dysfunction (CCD) and vice versa. Many studies have been performed where the patients present with atypical otalgia, vertigo, tinnitus, atypical facial pain, globus, dysphagia, weak voice, or sleep disturbances [42,43,44,45,46]. These imprecise complaints pose a challenge in attributing the symptoms to the precise definition of CMD. The interrelations clarify why the treatments of functional problems such as CMD and CCD warrant an interdisciplinary approach. Reference points for the diagnosis of CMD may be gathered by the ENT specialist: Questions targeting disturbances in the head and neck areas as well as problems with the musculoskeletal system should be asked including symptoms concerning teeth and temporomandibular joints. Unilateral facial pain, pain in the maxilla, or diffuse pain in the dental area without precise location to distinct teeth, as well as crunching and creaking during food intake may point the examining physician in the right direction. Patients often complain about bruxism, grinding, or compressing of their teeth independently of food intake. On inspection, they present with facial asymmetry: lines through brows, canthi, oral commissures, and mandibula do not run parallel/horizontal. Unilateral hypertrophy of facial or masticatory muscles may be a presenting symptom as well as dental impressions at the lingual border.
Craniomandibular dysfunction is one of the most common chronic pain syndromes
In addition, there are distinct manual therapeutic examination techniques that reveal a close relationship between the temporomandibular joint and the neuromuscular system (as recommended by the Deutschen Gesellschaft für Zahn‑, Mund- und Kieferheilkunde [DGZMK] und der Research Diagnostic Criteria for TMD [RDC/TMD]; [47, 48]). The Meersseman test is one such example.
The complaints may be appeased by a combined otolaryngological, osteopathic, and manual therapeutic approach. In addition, the positive influence of a manual therapy of the joints between the head bones and the cervical spine as well as the whole upper cervical spine has been objectified by electromyography (EMG) and magnetic kinesiography [15, 41]. The EMG shows an immediate normalization/reduction of the before hypertonic masticatory musculature. The magnetic kinesiography shows a reduction in the retroposition of the mandible characteristic of CMD by 1 to 1.5 mm [41]. These two factors—achieved by simple manual therapy of the craniovertebral joints—may significantly aid the treatment by a dentist using a dental splint.
Temporomandibular joints and craniovertebral joints form a cybernetic unit that is regulated by neuromuscular and neurophysiological reflexes. Myofunctional disturbances of the temporomandibular joints and craniovertebral joints may lead to overlapping complaints. As a result, treatment of CMD and/or CCD complaints has to be performed in a synchronous, interdisciplinary, and causal fashion targeting both areas. Otolaryngologists, dentists, and oral surgeons should synergistically orchestrate their treatment (Fig. 3).
Conclusion.
There has been a huge increase in the clinical significance of CMD in recent years and it should be kept in mind as a diagnosis by otolaryngologists. Manual therapy should be performed as well as myofunctional dental treatment.
Treatment of cervical disturbances
If the clinical otolaryngological examination does not reveal significant results, functional disturbances of the cervical spine–cervical spine joints–temporomandibular joints–skull system have to be taken into account. Evidence of trauma, fractures, paresis, neurologic disturbances, herniation of vertebral discs, tumors, metastases, apoplexy etc. has to be considered, imaging studies have to be performed, and if there are primary structural disturbances, the expertise of specialists has to be sought (orthopedics, neurology, dentists etc.). Structural disturbances are rare but must not be overlooked. The manual/osteopathic examination is performed to reveal a “blockade” as a reversible, hypomobile, and segmental functional disturbance of the craniovertebral or the temporomandibular joints. The underlying causes may be arthrogenic, angular, muscular, neurogenic, lymphogenic, vascular, or fascial, and the complaints may also stem from the joint capsule or ligaments [49]. From an osteopathic point of view, this almost corresponds to somatic dysfunction. Somatic dysfunction is the indication for a manual/osteopathic therapy. The therapy results from a specific joint examination and the evaluation of three criteria (Table 3).
A “blockade” is a reversible dysfunction of the craniovertebral or temporomandibular joints
Treatment of somatic dysfunction may be achieved by differing approaches from manual and osteopathic universes ([52]; Table 4).
Other complementary treatment approaches have found their way into clinical treatment settings; these, however, lack scientific evidence in their efficacy. They include: acupuncture, therapeutic local anesthesia, physical therapy, transcutaneous electric nerve stimulation (TENS), infrared light short-wave therapy, and kinesiotaping. Techniques and treatment plans may be found elsewhere [53,54,55].
Before treatment, contraindications against immediate manual and osteopathic treatment have to be respected (Table 5).
If local and/or regional therapy is not successful or if recurrence is encountered after two or three treatment sessions, other possible causes have to be kept in mind. These include the whole musculoskeletal system. The osteopathic approach including visceral osteopathic techniques as well as craniosacral osteopathy should be the guiding principle.
Practical conclusion
-
A feasible neuroanatomical model exists for various otolaryngological symptoms.
-
In scientific terms, the underlying pathophysiology in humans is still under debate.
-
The unfavorable position of the center of gravity of the head requires a vestibular-triggered regulation of muscle movement in the craniovertebral joints to coordinate a stable gaze and posture.
-
A somatosensory component in the development of tinnitus should not be underestimated.
-
In such cases, functional disorders of the craniovertebral joints and the temporomandibular joints are adequately treated with manual therapy.
-
Cervicogenic swallowing disorders are functional disorders in the head and neck area, which have not had significant scientific evaluation but are likely relevant in daily practice.
-
The clinical significance of CMD is increasing and it should be considered carefully in the daily diagnostic spectrum of ENT care.
-
Manual therapy in CMD should be supplemented by myofunctional dental treatment.
References
Neuhuber WL (2005) Funktionelle Neuroanatomie des kraniozervikalen Übergangs. In: Hülse N, Wolff (eds) Die obere Halswirbelsäule. Springer, Heidelberg, pp 56–69
Voss H (1971) Tabulation of the absolute and relative muscular spindle numbers in human skeletal musculature. Anat Anz 129:562–572
Neuhuber WL (2005) M. longissimus als Vermittler zwischen kraniozervikalem Übergang und Becken. Manuelle Medizin 43:395–399
Müller A, Böhni U (2014) Praktische Neurologie der oberen HWS. In: Böhni L, Locher (eds) Manuelle Medizin 1. Thieme, Stuttgart, pp 394–398
Neuhuber WL (2004) Hirnstamm. In: Benninghoff-Breckhahn (ed) Anatomie, vol 2. Elsevier, München, pp 326–386
Pfaller K, Arvidsson J (1988) Central distribution of trigeminal and upper cervical primary afferents in the rat studied by anterograde transport of horseradish peroxidase conjugated to wheat germ agglutinin. J Comp Neurol 268:91–108
Shore SE, Vass Z, Wys NL et al (2000) Trigeminal ganglion innervates the auditory brainstem. J Comp Neurol 419:271–285
Brandt T, Huppert D (2016) A new type of cervical vertigo: Head motion-induced spells in acute neck pain. Baillieres Clin Neurol 86:974–975
Hülse M, Hölzl M (2000) Vestibulospinal reactions in cervicogenic disequilibrium. Cervicogenic imbalance. HNO 48:295–301
Mai J, Paxinos G (2011) The human nervous system. Elsevier, Amsterdam
Bronstein AM (2016) Multisensory integration in balance control. Handb Clin Neurol 137:57–66
Bronstein AM (1999) The interaction of otolith and proprioceptive information in the perception of verticality. The effects of labyrinthine and CNS disease. Ann N Y Acad Sci 871:324–333
Cutfield NJ, Scott G, Waldman AD et al (2014) Visual and proprioceptive interaction in patients with bilateral vestibular loss. Neuroimage Clin 4:274–282
Lappat A, Dorn LJ, Hölzl M (2016) The vestibular craniovertebral joints. HNO 64:320–327
Brandt T, Buchele W, Arnold F (1977) Arthrokinetic nystagmus and ego-motion sensation. Exp Brain Res 30:331–338
Lucertini M, De Angelis C, Martelli M et al (2011) Subjective visual vertical in erect/supine subjects and under microgravity: effects of lower body negative pressure. Eur Arch Otorhinolaryngol 268:1067–1075
Marano E, Marcelli V, Di Stasio E et al (2005) Trigeminal stimulation elicits a peripheral vestibular imbalance in migraine patients. Headache 45:325–331
Sadeghi SG, Minor LB, Cullen KE (2012) Neural correlates of sensory substitution in vestibular pathways following complete vestibular loss. J Neurosci 32:14685–14695
Matyssek C (2010) Funktionell-anatomische Analyse der kurzen, tiefen Nackenmuskulatur des Neugeborenen im Vergleich zum Erwachsenen. Medizinische Fakultät der Universität, Köln
Maurer C, Mergner T, Becker W et al (1998) Eye-head coordination in labyrinthine-defective humans. Exp Brain Res 122:260–274
Campos JL, Butler JS, Bulthoff HH (2014) Contributions of visual and proprioceptive information to travelled distance estimation during changing sensory congruencies. Exp Brain Res 232:3277–3289
Lang J, Ishikawa K, Hatakeyama K et al (2013) 3D body segment oscillation and gait analysis for vestibular disorders. Auris Nasus Larynx 40:18–24
Grossman GE, Leigh RJ (1990) Instability of gaze during locomotion in patients with deficient vestibular function. Ann Neurol 27:528–532
Pozzo T, Berthoz A, Vitte E et al (1991) Head stabilization during locomotion. Perturbations induced by vestibular disorders. Acta Otolaryngol Suppl 481:322–327
Decher H (1969) Die zervikalen Syndrome in der Hals-Nasen-Ohren-Heilkunde. Thieme, Stuttgart
Biesinger E (1997) Das C2/C3-Syndrom – Der Einfluß zervikaler Afferenzen auf HNO-Ärztliche Krankheitsbilder. Manuelle Medizin 35:12–19
Reisshauer A, Mathiske-Schmidt K, Kuchler I et al (2006) Functional disturbances of the cervical spine in tinnitus. HNO 54:125–131
Shore SE (2005) Multisensory integration in the dorsal cochlear nucleus: unit responses to acoustic and trigeminal ganglion stimulation. Eur J Neurosci 21:3334–3348
Zhou J, Shore S (2004) Projections from the trigeminal nuclear complex to the cochlear nuclei: a retrograde and anterograde tracing study in the guinea pig. J Neurosci Res 78:901–907
Ralli M, Greco A, Turchetta R et al (2017) Somatosensory tinnitus: current evidence and future perspectives. J Int Med Res 45:933–947
Singbartl F, Ernst A (2009) Hör- und Gleichgewichtsstörungen nach HWS-Weichteildistorsion. In: Graf M, Grill C, Wedig HD (eds) Beschleunigungsverletzung der Halswirbelsäule. Springer, Heidelberg
Biesinger E, Reisshauer A, Mazurek B (2008) Die Rolle der Halswirbelsäule und des Kiefergelenks bei Tinnitus. Der sog. somatosensorische Tinnitus (SST). HNO 56(7):673–677
Neuhuber WL, Zenker W (1989) Central distribution of cervical primary afferents in the rat, with emphasis on proprioceptive projections to vestibular, perihypoglossal, and upper thoracic spinal nuclei. J Comp Neurol 280:231–253
Gritsenko K, Caldwell W, Shaparin N et al (2014) Resolution of long standing tinnitus following radiofrequency ablation of C2–C3 medial branches—a case report. Pain Physician 17:E95–E98
https://www.youtube.com/watch?v=iux_uiums-m. Zugegriffen: 9. Feb 2018.
Arens C, Herrmann IF, Rohrbach S et al (2015) Position paper of the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery and the German Society of Phoniatrics and Pediatric Audiology—Current state of clinical and endoscopic diagnostics, evaluation, and therapy of swallowing disorders in children. GMS Curr Top Otorhinolaryngol Head Neck Surg 14:Doc2
Seifert K (1995) Hals. OtoRhinoLaryngologie in Klinik und Praxis, vol 3. Thieme, Stuttgart
Hülse M (1991) Cervical dysphonia. Folia Phoniatr (Basel) 43:181–196
Hülse M (1991) Functional dysphonia following cervical spine injuries. Laryngorhinootologie 70:599–603
Losert-Bruggner B, Hülse M, Hülse R (2017) Fibromyalgia in patients with chronic CCD and CMD—a retrospective study of 555 patients. Cranio:1–9. https://doi.org/10.1080/08869634.2017.1334376
Hülse M, Neuhuber WL, Wolff HD (2005) Die obere Halswirbelsäule-Pathophysiologie und Klinik. Springer, Heidelberg
De Felicio CM, Melchior Mde O, Ferreira CL et al (2008) Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio 26:118–125
Lam DK, Lawrence HP, Tenenbaum HC (2001) Aural symptoms in temporomandibular disorder patients attending a craniofacial pain unit. J Orofac Pain 15:146–157
Pereira TC, Brasolotto AG, Conti PC et al (2009) Temporomandibular disorders, voice and oral quality of life in women. J Appl Oral Sci 17(Suppl):50–56
Rener-Sitar K, John MT, Pusalavidyasagar SS et al (2016) Sleep quality in temporomandibular disorder cases. Sleep Med 25:105–112
Schmitter M, Kares-Vrincianu A, Kares H et al (2015) Sleep-associated aspects of myofascial pain in the orofacial area among Temporomandibular Disorder patients and controls. Sleep Med 16:1056–1061
Ohrbach R, Dworkin SF (2016) The evolution of TMD diagnosis: past, present, future. J Dent Res 95:1093–1101
Schiffman E, Ohrbach R, Truelove E et al (2014) Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J Oral Facial Pain Headache 28:6–27
Arens C, Scholz FG, Kropf S et al (2017) Reduction of post-surgical pain by Manual Medicine following tonsillectomy in adults. Laryngorhinootologie 96:831. https://doi.org/10.1055/s-0043-119885
Böhni U (2015) Biomechanische und kinematische Grundlagen. In: Böhni L, Locher (eds) Manuelle Medizin. Thieme, Stuttgart, pp 21–43
Greenman P (2000) Lehrbuch der Osteopathischen Medizin – Grundlagen und Konzepte, Techniken und Methoden, klinische Integration und Korrelation. Thieme, Stuttgart
Hülse M, Hölzl M (2004) The efficiency of spinal manipulation in otorhinolaryngology. A retrospective long-term study. HNO 52:227–234
Gautschi R (2015) Triggerpunkt-Therapie. In: Böhni L, Locher (eds) Manuelle Medizin. Thieme, Stuttgart, pp 296–302
Neumann HD (1999) Manuelle Medizin – Eine Einführung in Theorie, Diagnostik und Therapie. Springer, Heidelberg
Bischoff HP, Moll H (2007) Kurzgefasstes Lehrbuch der Manuellen Medizin. In: Chirodiagnostische und chirotherapeutische Technik. Spitta, Balingen
Besnard JM (2017) Red flags und yellow flags. In: Mayer J, Standen C (eds) Lehrbuch Osteopathische Medizin. Elsevier, Amsterdam, pp 287–291
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Hölzl, R. Behrmann, E. Biesinger, W. von Heymann, R. Hülse, U.R. Goessler, and C. Arens declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
The supplement containing this article is not sponsored by industry.
Rights and permissions
About this article
Cite this article
Hölzl, M., Behrmann, R., Biesinger, E. et al. Selected ENT symptoms in functional disorders of the upper cervical spine and temporomandibular joints. HNO 67 (Suppl 1), 1–9 (2019). https://doi.org/10.1007/s00106-019-0610-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00106-019-0610-1