Abstract
There are contradictory results in the relevant literature about the relationship between objective determinants of craniocervical posture and temporomandibular disorder (TMD), whereas no study has worked on ankylosing spondylitis (AS) and TMD relationship. We conducted this study to test the predictors of TMD in AS patients and its relationship with craniocervical posture. AS patients aged between 18 and 50 years consecutively admitted to our outpatient clinics were recruited. TMD was diagnosed by ‘Diagnostic Criteria for Temporomandibular Disorders (DC/TMD)’. Spinal mobility was assessed by BASMI; disease activity by ASDAS-CRP and neck disability by Neck Disability Index. Craniocervical posture was assessed on lateral cervical X-ray by measuring the craniocervical angle, cervical curvature angle, suboccipital distance, atlas–axis distance, and anterior translation distance. A total of 98 (58.2% female) patients with a mean age of 37.4 ± 8.2 years were enrolled in this study. TMD was diagnosed in 58 (59.2%) patients. Spinal mobility and craniocervical posture measurements were similar among the two groups. Smoking, bruxism (in females), neck disability and AS disease activity (in males) were higher in TMD patients. Multivariate analysis revealed active smoking (aOR 6.9; 95% CI 1.8–25.6; p = 0.004), bruxism in females (aOR 17.9; 95% CI 2.0–159.2; p = 0.01), high ASDAS in males (aOR 11.8; 95% CI 1.2–122.5; p = 0.038) and neck disability (aOR 12.7; 95% CI 3.8–42.9; p < 0.001) as independent risk factors for TMD in AS patients. No relationship between the craniocervical posture measurements and TMD was found in AS patients. Active smoking, high disease activity in males, bruxism in females and neck disability were found as predictors of TMD in AS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductıon
Temporomandibular disorders (TMD) are one of the most important public health problems which affect approximately 5–12% of the overall population. Temporomandibular disorders are a group of musculoskeletal problems that principally originated from temporomandibular joint (TMJ), masticatory muscles and neighbouring tissues [1]. Pain, crepitation, click, and locking are the most common symptoms. Trauma, para-functional habits, stress, bruxism, and malocclusion are potential risk factors for the development of TMD [2].
Ankylosing spondylitis (AS), commonly seen in males, is characterized by inflammatory back pain. It primarily involves sacroiliac joints and spine, less commonly peripheral joints may be affected. According to very little data, the prevalence of TMD is 4–35% in AS patients [3,4,5]. Although the underlying mechanisms are poorly defined, primary synovial involvement of TMJ, destruction of joint capsule or components of the disc, and postural changes related to AS have been postulated as possible mechanisms [5, 6].
Several studies proposed a relationship between craniocervical postural changes and TMD [7,8,9]. Projected mechanism of this association is that the distorted craniocervical posture may change the position of the chin by affecting surrounding muscle and tendons and resulting pressure overload on TMJ leading to TMD [10]. Contrarily, there are also some findings indicating no relation between craniocervical posture and TMD [11,12,13]. Cervical kyphosis is the most common cervical deformity in AS patients and causes head-forward position. To the best of our knowledge, no data has been published about the relationship between craniocervical postural changes and TMD in AS patients.
The aims of this study are to determine the frequency of TMD in a group of AS patients, and to test whether there is a relationship between craniocervical posture and TMD and to determine the risk factors for the development of TMD in AS patients.
Patıents and methods
Patient enrollment
In this cross-sectional observational study, we enrolled AS patients who consecutively admitted to the Departments of Physical Medicine and Rehabilitation and Rheumatology, Hacettepe University, Ankara, Turkey between September 2018 and April 2019. The patients with a diagnosis of AS according to the modified New York criteria [14] and aged between 18 and 50 years were included in this study. Modified New York criteria are the combination of 1 clinical component with the radiographic sacroiliitis. Clinical components are low back pain and stiffness which improves with activity for more than three months, limited range of motion of the lumbar spine in both forward and lateral bending and limitation of chest expansion relative to normal values correlated for age and sex. Radiographic criteria were the at least bilateral grade 2 sacroiliitis or unilateral at least grade 3 sacroiliitis [14]. Diagnosis of each patient was confirmed by UK and OO, independent of each other. The exclusion criteria were as follows: patients with neurological or cognitive deficits, presence of active dental or periodontal pain, history of orthodontic treatment, history of tumor, surgery, radiotherapy or trauma to head and neck region. Local Ethics Committee (Hacettepe University-GO 18/755, Date: 24 July 2018) approved the study protocol, and the written informed consents were obtained from all patients.
The diagnosis of TMD has been established according to the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) which is the most recent criteria set published in 2016 [15]. The study population was divided into two main groups: TMD ( +) and (−) groups. Demographic, clinical and radiographical parameters were compared between two groups.
Clinical assessment
Demographic and clinical features including age, gender, smoking history, comorbidities confirmed by both medical records and patient interviews, AS disease duration, current medications and presence of self-reported bruxism were recorded.
Ankylosing Spondylitis Disease Activity Score-C-reactive protein (ASDAS-CRP) was used to assess AS disease activity. Cut-off values of ASDAS-CRP score for inactive, low, and high/very high disease activity were 1.3, 2.1 and 3.5, respectively [16].
To assess spinal mobility; chin–sternum distance (measured according to ASAS) and the components of Bath Ankylosing Spondylitis Metrology Index (BASMI) score (lateral spinal flexion, tragus–wall distance, modified Schober test, maximal intermalleolar distance, and cervical rotation angle) were measured [17].
The Turkish version of Neck disability index (NDI) was used to assess how much does the neck pain affect the patients’ daily activities of living. This index is composed of ten questions with a maximum score of 50. Zero to four points indicate no disability, 5–14 points indicate mild disability, 15–24 points indicate moderate disability, 25–34 points indicate severe disability and 35–50 points indicate complete disability [18].
Radiological assessment
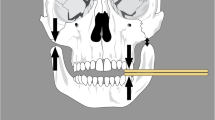
Craniocervical posture was assessed by measuring suboccipital, atlantoaxial and anterior translation distances (in millimeter), craniocervical and cervical curvature angle on lateral cervical X-ray which was taken while the patient was standing up, holding his or her head high and shoulders low. All these measurements were performed by the same researcher blinded to the patients’ clinical data. In accordance with previous studies, radiographic measurements were defined as follows: suboccipital distance (in millimeter); vertical distance between the base of occipital bone and posterosuperior point of first vertebrae, atlantoaxial distance (in millimeter); vertical distance between the most inferoposterior point of posterior arch of atlas and the most posterosuperior point of the spinous process of axis, anterior translation distance (in millimeter); horizontal distance between the vertical line passing by the superoposterior point of C2 vertebral body and vertical line passing by the posteroinferior point of C7 vertebral body, craniocervical angle; the angle between the McGregor plane and the line tangential to the backside of the odontoid apophysis, cervical curvature angle; the angle between the straight lines passing on the posterior borders of body of third and sixth vertebrae (Fig. 1a, b) [7, 8, 10]. Also, modified Stoke AS spine score (mSASSS) was calculated to compare the degree of spinal involvement of AS [19].
Sample size
We calculated the sample size based on the primary objective of the study. With the assumption that the rate of TMD is 10% in general population, we hypothesized the rate of TMD in AS as 20% in light of the previous studies [3, 5, 20, 21]. We used G power 3.1 computerized system with type 1 error of 0.05 and type 2 error of 0.20. At least 78 patients were needed to test our hypothesis.
Statistical analysis
The variables were investigated using visual (histogram, probability plots) and analytic methods (Kolmogorov–Smirnov, skewness and kurtosis) to determine whether they are normally distributed. The data of descriptive analysis were expressed as either mean ± standard deviation (SD) or the median (interquartile range). Categorical variables were compared with the Chi-square test or Fisher’s exact test where appropriate. The Student's t test was used to compare the normally distributed continuous data between two groups, Mann–Whitney U test was used to compare the non-normally distributed continuous data between two groups. For multivariate analysis, univariate analyses with a p value lower than 0.20 and detected interactions (effect modifications) were entered firstly with ‘’Backward LR’’, then ‘’Enter’’ for the final model to determine independent predictors of TMD development in AS patients. Hosmer–Lemeshow goodness-of-fit statistics were used to assess model fit. A 5% Type-I error level was used to infer statistical significance. Statistical analysis was performed using the Statistical Package for the Social Sciences software (version 23.0; IBM Corporation, Armonk, NY, USA).
Results
Study population
We recruited a total of 98 consecutive AS patients with a mean age of 37.4 ± 8.2 years. Fifty-seven (58.2%) of them were female and 33.7% were active smokers. Approximately 45% of the patients had at least one concomitant disease, the most common ones were familial Mediterranean fever (13 patients, 13.2%) and hypertension (11 patients, 11.2%). The mean duration of AS disease was 8.1 ± 5.7 years. Self-reported bruxism was present in 61 (62.2%) of all patients.
Of 98 patients, the diagnosis of TMD has been established in 58 (59.2%) patients (TMD ( +) group). Age, gender, presence of comorbidities, AS disease duration, current AS treatment were similar between TMD ( +) and (−) groups. The percent of active smokers (43.1% vs. 20.0%) and self-reported bruxism (74.1% vs. 45.0%) were significantly higher in TMD ( +) group (p = 0.017 and 0.003, respectively). When the interaction between gender and bruxism was investigated, it has been found that there was no significant difference in the presence of TMD whether the patients had bruxism or not (56.0% vs. 37.5%, p = 0.24) in males, however TMD was more prevalent in patients with bruxism (80.6% vs. 42.9%, p = 0.004) in females.
Details of the demographic and clinical features of the study population are given in Table 1.
Measurements related to ankylosing spondylitis and craniocervical posture
Tragus–wall distance, cervical rotation, chin–sternum distance, BASMI, and mSASSS were similar in both groups. ASDAS-CRP was significantly higher in TMD ( +) group [2.9 (2.0–3.2) vs. 1.9 (1.4–2.5), p < 0.001, respectively (Table 2); rate of high-very high ASDAS-CRP: 70.5% vs. 29.5%, p = 0.003, in TMD ( +) and (−) groups, respectively]. An interaction between gender and AS disease activity was found. While TMD was more frequent in male patients with higher disease activity (high-very high ASDAS vs low-inactive ASDAS; 73.7% vs. 27.3%, p = 0.005), the frequency of TMD was similar in female patients with high-very high ASDAS or low-inactive ASDAS AS (69.0% vs. 60.0%, p = 0.52).
No significant difference in the radiographic measurements of craniocervical posture were found between TMD ( +) and (−) groups (Table 2).
Neck disability was more prevalent in TMD ( +) group when compared to TMD (−) group (84.5% to 40.0%, p < 0.001). In TMD ( +) group; 32 (55.2%), 12 (20.7%) and 5 (8.6%) patients had mild, moderate and severe disability, respectively. However, in the TMD (−) group; 16 (40%) patients had a mild disability, none of them had moderate or severe disability (Table 2).
Univariate and multivariate analyses
A multivariate logistic regression analysis was performed to determine the independent effects of each parameter which had been determined by univariate analyses including gender, smoking, presence of self-reported bruxism, high ASDAS and presence of neck disability. As interactions were found between gender and bruxism and also between gender and high ASDAS, we included the following parameters to multivariate analysis: gender, smoking status, presence of bruxism and interaction of bruxism and gender, high ASDAS and interaction of high ASDAS and gender, and presence of neck disability.
As shown in Table 3, final multivariate analysis revealed active smoking (aOR 6.9; 95% CI 1.8–25.6; p = 0.004), presence of bruxism in females (aOR 17.9; 95% CI 2.0–159.2; p = 0.01), high ASDAS in males (aOR 11.8; 95% CI 1.2–122.5; p = 0.038), and presence of neck disability (aOR 12.7; 95% CI 3.8–42.9; p < 0.001) as independent risk factors for TMD in AS patients. Model fit was tested by Hosmer–Lemeshow test (p = 0.55).
Discussion
In this study, active smoking, high disease activity in males, bruxism in females and neck disability were found as predictors of TMD in AS patients, also we did not find any relationship between the objective determinants (measurements) of craniocervical posture and TMD in AS patients. In current literature, there are case reports related to TMJ involvement in AS [5, 20] and a few cross-sectional studies giving data about TMD symptoms in AS patients [3, 4].
The prevalence of TMD varies between studies due to the differences in study populations and the diagnostic criteria. In previous population-based studies, the prevalence of TMD was found to be between 5 and 12% [21,22,23,24]. Data related to TMD in AS patients are very little and the frequency of TMD in these patients has been reported as 4 to 37% [3,4,5, 24,25,26,27]. However, standardized diagnostic criteria set for TMD was applied in none of these studies. In a study by Helenius and colleagues, 37% of AS patients reported TMD symptoms including tenderness of masticatory muscles, tenderness, clicking and crepitation of TMJ and this rate was higher than the rates in rheumatoid arthritis (RA) and mixed connective tissue disease patients enrolled in this study [3]. Locher et al. reported the frequency of radiographical involvement of TMJ as 22% in 50 AS patients [25]. In another study including 79 patients with various rheumatic diseases (39 with RA, 17 with AS, 23 with Sjögren’s syndrome), the frequency of subjective TMD symptoms reported by AS patients was 76.5% and this rate was significantly higher than healthy controls [4]. We found that 59.2% of our patients have TMD and this prevalence is higher than the general population.
Conflicting data are available about the relationship between the craniocervical posture changes and TMD. While a bunch of studies confirms the possible linkage [8, 9, 28, 29], others deny [11,12,13]. In a study comparing 32 TMD patients with 34 healthy controls, it has been reported that cervical curvature angle was higher in patients with muscle disorders, and atlantoaxial distance was higher in patients with disc displacement [7]. However; in a recent study conducted with 30 female TMD patients and 30 healthy controls, the craniocervical angles and atlantoaxial distances were found to be similar [30]. Overall, a recent review concluded that due to the methodological inadequacy and scantiness of relevant data, it is impossible to either approve or reject any relationship between craniocervical posture changes and TMD [31]. In our study, we found no significant association between the measurements of craniocervical posture and TMD in AS patients. To the best of our knowledge, this is the first study investigating the relationship between craniocervical posture and TMD diagnosed according to DC/TMD criteria set in patients with AS.
Age, gender, disease duration and medications were similar for TMD ( +) and (−) groups. The frequency of active smoking, presence of bruxism (in females), AS disease activity (in males) and neck disability were significantly higher in TMD ( +) group. As gender interacted with disease activity and bruxism, we analyzed these parameters according to gender.
As an oral para-functional habit, smoking has been proposed as an independent risk factor for the development of TMD [32, 33]. Sanders et al. reported approximately fourfold increase in TMD occurrence, the increase was substantially higher in young smokers—a similar age group to our study [32]. Smoking-related inflammation, especially by interleukin-1 and macrophage chemoattractant protein-1, and nicotine-related hyperalgesia has been suggested as the potential mechanisms of this association [34, 35]. In our study, we found an approximately sevenfold increase in the risk of TMD in AS patients who are active smokers.
Another para-functional habit, bruxism has been largely studied in TMD patients. In a well-designed study from Brazil, the rate of bruxism was found as 52% in TMD patients and bruxism-related TMD risk was reported as twofold. However, they reported no gender difference [36]. In our study, we found an approximately 18-fold increase in the risk of TMD occurrence in female AS patients who have bruxism. However, the confidence interval is large and this could be mediated by the high discordance of the bruxism rate between two groups. Although we found a strong relationship, numbers should be interpreted cautiously.
According to the results of our study, high AS disease activity, especially in men, was defined as a risk factor for the development of TMD in AS patients for the first time in literature. There is no other study trying to explain this association. However, in our results, ASDAS-CRP levels were higher in females. But females with and without TMD both had high ASDAS-CRP levels. This may explain why the disease activity was not found as a strong factor statistically predicting TMD in females. To explain higher disease activity in females compared to males, we also analyzed the TNF use, comorbidities and other possible factors, but no relevant factor was found. Limitations of ASDAS-CRP, psychosocial factors may be counted as reasons but all need to be verified with prospective studies. Although biologic DMARD utilization was similar in males and females, we did not exactly determine how long they are on these treatments and about their treatment compliance. On the other hand, we found no association between tragus–wall, chin–thorax distances and cervical rotation and indicators of structural damage like BASMI and mSASSS with TMD. Therefore, we may speculate that the relationship between AS and TMD is based on the inflammation rather than the mechanical and postural changes. Also, prospective studies are needed to see whether suppressing the disease activity also heals TMD or not to elucidate the relationship between disease activity and TMD.
Furthermore, we found that neck disability is a strong and reliable factor for predicting TMD in AS patients. Silveria et al. reported that the score of NDI was significantly higher in 20 TMD patients compared to 20 healthy controls. Thus, they stated that the assessment of neck dysfunction should be considered in the diagnosis and treatment of TMD [37]. Another study with 154 patients, a strong correlation as 82% was found between TMD and NDI [38]. In addition, manual therapy for TMD resulted in significant improvement of NDI [39]. Similar to bruxism, the confidence interval is large, and this is because of the high discordance of the neck disability between two groups, thus numbers should be interpreted cautiously. Further studies are needed to test the availability and validity of NDI score for TMD assessment in AS patients.
Our study has some limitations and strengths. About 60% of our study group comprises females, this may be unusual when we consider the high prevalence of AS in males. This issue may be seen as a selection bias. However, during recruitment period, we asked all AS patients who consecutively applied to our departments to take part in the study, not all of them agreed. So, we did not select patients, we ‘’enrolled’’ the ‘’voluntary patients’’ and females volunteered to participated more. In fact, this situation could result from referral center bias. As a tertiary center, our patient profile is different from regular population. Because of referral bias, there seems an accumulation on female gender and this may create a selection bias-like picture. As the overlapping high frequency and discordance of predicting factors in TMD ( +) patients compared to (−) patients and selection bias could explain the large confidence intervals. To overcome this bias, we have checked all possible modifier effects of gender and included the relevant interactions to the final model. Secondly, a control group would have strengthened our results. On the other hand, blinded assessment of lateral X-rays and being the first study that applied the most recent TMD diagnostic criteria to AS patients may be counted as strong aspects of this study.
In conclusion, we found a high prevalence of TMD in AS patients. Clinicians should assess for TMD in AS patients during routine daily practice. We found active smoking, high disease activity in males, bruxism in females and neck disability as predictors of TMD in AS patients. No relationship between the objective determinants (measurements) of craniocervical posture and TMD in AS patients was found. Gender seems to have a role, and our results should be interpreted gender-selectively. Further studies with higher number of patients are needed to elucidate the possible underlying mechanisms that favor TMD development in AS patients.
References
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J Oral Facial Pain Headache 28(1):6–27. https://doi.org/10.11607/jop.1151
Durham J, Newton-John TR, Zakrzewska JM (2015) Temporomandibular disorders. BMJ 350:h1154. https://doi.org/10.1136/bmj.h1154
Helenius LM, Hallikainen D, Helenius I, Meurman JH, Kononen M, Leirisalo-Repo M, Lindqvist C (2005) Clinical and radiographic findings of the temporomandibular joint in patients with various rheumatic diseases. A case–control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99(4):455–463. https://doi.org/10.1016/j.tripleo.2004.06.079
Yildizer Keris E, Yaman SD, Demirag MD, Haznedaroglu S (2017) Temporomandibular joint findings in patients with rheumatoid arthritis, ankylosing spondylitis, and primary Sjogren's syndrome. J Investig Clin Dent 8(4):12255. https://doi.org/10.1111/jicd.12255
Arora P, Amarnath J, Ravindra SV, Rallan M (2013) Temporomandibular joint involvement in ankylosing spondylitis. BMJ Case Rep 2:2013. https://doi.org/10.1136/bcr-2013-009386
Gupta N, Gupta N, Tomar LR, Nair N (2016) Temporomandibular joint ankylosis in ankylosing spondylitis: a case report and review of literature. J Family Med Prim Care 5(3):716–718. https://doi.org/10.4103/2249-4863.197292
Saddu SC, Dyasanoor S, Valappila NJ, Ravi BV (2015) The evaluation of head and craniocervical posture among patients with and without temporomandibular joint disorders—a comparative study. J Clin Diagn Res 9(8):55–58. https://doi.org/10.7860/JCDR/2015/12830.6343
de Farias Neto JP, de Santana JM, de Santana-Filho VJ, Quintans-Junior LJ, de Lima Ferreira AP, Bonjardim LR (2010) Radiographic measurement of the cervical spine in patients with temporomandibular dysfunction. Arch Oral Biol 55(9):670–678. https://doi.org/10.1016/j.archoralbio.2010.06.002
Chaves TC, Turci AM, Pinheiro CF, Sousa LM, Grossi DB (2014) Static body postural misalignment in individuals with temporomandibular disorders: a systematic review. Braz J Phys Ther 18(6):481–501. https://doi.org/10.1590/bjpt-rbf.2014.0061
Camara-Souza MB, Figueredo OMC, Maia PRL, Dantas IS, Barbosa GAS (2018) Cervical posture analysis in dental students and its correlation with temporomandibular disorder. Cranio 36(2):85–90. https://doi.org/10.1080/08869634.2017.1298226
Armijo-Olivo S, Rappoport K, Fuentes J, Gadotti IC, Major PW, Warren S, Thie NM, Magee DJ (2011) Head and cervical posture in patients with temporomandibular disorders. J Orofac Pain 25(3):199–209
Andrade AV, Gomes PF, Teixeira-Salmela LF (2007) Cervical spine alignment and hyoid bone positioning with temporomandibular disorders. J Oral Rehabil 34(10):767–772. https://doi.org/10.1111/j.1365-2842.2006.01698.x
Rocha T, Castro MA, Guarda-Nardini L, Manfredini D (2017) Subjects with temporomandibular joint disc displacement do not feature any peculiar changes in body posture. J Oral Rehabil 44(2):81–88. https://doi.org/10.1111/joor.12470
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27(4):361–368. https://doi.org/10.1002/art.1780270401
Polat S, Polat N, Çetinoğlu A Ohrbach R (eds) Diagnostic criteria for temporomandibular disorders: assessment instruments. Version 2. INFORM group https://ubwp.buffalo.edu/rdc-tmdinternational/tmd-assessmentdiagnosis/rdc-tmd/translations/Turkish/ Accessed 17 Sep 2018
Lukas C, Landewe R, Sieper J, Dougados M, Davis J, Braun J, van der Linden S, van der Heijde D (2009) Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis 68(1):18–24. https://doi.org/10.1136/ard.2008.094870
Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garrett SL, Calin A (1994) Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol 21(9):1694–1698
Bicer A, Yazici A, Camdeviren H, Erdogan C (2004) Assessment of pain and disability in patients with chronic neck pain: reliability and construct validity of the Turkish version of the neck pain and disability scale. Disabil Rehabil 26(16):959–962. https://doi.org/10.1080/09638280410001696755
Maksymowych WP, Learch T, Lambert RG, Ward M, Haroon N, Inman R, Salonen D, Gensler LS, Weisman MH (2014) Development and validation of the spondyloarthritis radiography module for calibration of readers using the modified Stoke Ankylosing Spondylitis Spine Score. Arthritis Care Res (Hoboken) 66(1):55–62. https://doi.org/10.1002/acr.22083
de Andrade Freitas Oliveira LS, de Oliveira-Santos C, de Melo DP, Gomes Torres MG, Flores Campos PS (2013) Unilateral bony ankylosis of the temporomandibular joint in a case of ankylosing spondylitis. Oral Maxillofac Surg 17(3):213–217. https://doi.org/10.1007/s10006-012-0365-2
Liu F, Steinkeler A (2013) Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin N Am 57(3):465–479. https://doi.org/10.1016/j.cden.2013.04.006
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6(4):301–355
Scrivani SJ, Keith DA, Kaban LB (2008) Temporomandibular disorders. N Engl J Med 359(25):2693–2705. https://doi.org/10.1056/NEJMra0802472
Atsu SS, Ayhan-Ardic F (2006) Temporomandibular disorders seen in rheumatology practices: a review. Rheumatol Int 26(9):781–787. https://doi.org/10.1007/s00296-006-0110-y
Locher MC, Felder M, Sailer HF (1996) Involvement of the temporomandibular joints in ankylosing spondylitis (Bechterew's disease). J Craniomaxillofac Surg 24(4):205–213. https://doi.org/10.1016/s1010-5182(96)80003-5
Ramos-Remus C, Major P, Gomez-Vargas A, Petrikowski G, Hernandez-Chavez A, Gonzalez-Marin E, Russell AS (1997) Temporomandibular joint osseous morphology in a consecutive sample of ankylosing spondylitis patients. Ann Rheum Dis 56(2):103–107. https://doi.org/10.1136/ard.56.2.103
Davidson C, Wojtulewski JA, Bacon PA, Winstock D (1975) Temporo-mandibular joint disease in ankylosing spondylitis. Ann Rheum Dis 34(1):87–91. https://doi.org/10.1136/ard.34.1.87
Munhoz WC, Marques AP, Siqueira JT (2004) Radiographic evaluation of cervical spine of subjects with temporomandibular joint internal disorder. Braz Oral Res 18(4):283–289
Wright EF, Domenech MA, Fischer JR Jr (2000) Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc 131(2):202–210
Raya CR, Plaza-Manzano G, Pecos-Martin D, Ferragut-Garcias A, Martin-Casas P, Gallego-Izquierdo T, Romero-Franco N (2017) Role of upper cervical spine in temporomandibular disorders. J Back Musculoskelet Rehabil 30(6):1245–1250. https://doi.org/10.3233/bmr-169620
Rocha CP, Croci CS, Caria PH (2013) Is there relationship between temporomandibular disorders and head and cervical posture? A systematic review J Oral Rehabil 40(11):875–881. https://doi.org/10.1111/joor.12104
Sanders AE, Maixner W, Nackley AG, Diatchenko L, By K, Miller VE, Slade GD (2012) Excess risk of temporomandibular disorder associated with cigarette smoking in young adults. J Pain 13(1):21–31. https://doi.org/10.1016/j.jpain.2011.08.003
Miettinen O, Anttonen V, Patinen P, Pakkila J, Tjaderhane L, Sipila K (2017) Prevalence of temporomandibular disorder symptoms and their association with alcohol and smoking habits. J Oral Facial Pain Headache 31(31):30–36. https://doi.org/10.11607/ofph.1595
Rawlinson A, Grummitt JM, Walsh TF, Ian Douglas CW (2003) Interleukin 1 and receptor antagonist levels in gingival crevicular fluid in heavy smokers versus non-smokers. J Clin Periodontol 30(1):42–48. https://doi.org/10.1034/j.1600-051x.2003.300107.x
Capelli A, Di Stefano A, Gnemmi I, Balbo P, Cerutti CG, Balbi B, Lusuardi M, Donner CF (1999) Increased MCP-1 and MIP-1beta in bronchoalveolar lavage fluid of chronic bronchitis. Eur Respir J 14(1):160–165. https://doi.org/10.1034/j.1399-3003.1999.14a27.x
Magalhaes BG, Freitas JLM, Barbosa A, Gueiros M, Gomes SGF, Rosenblatt A, Caldas Junior AF (2018) Temporomandibular disorder: otologic implications and its relationship to sleep bruxism. Braz J Ororhinololaryngol 84(5):614–619. https://doi.org/10.1016/j.bjorl.2017.07.010
Silveira A, Gadotti IC, Armijo-Olivo S, Biasotto-Gonzalez DA, Magee D (2015) Jaw dysfunction is associated with neck disability and muscle tenderness in subjects with and without chronic temporomandibular disorders. Biomed Res Int 2015:512792. https://doi.org/10.1155/2015/512792
Olivo SA, Fuentes J, Major PW, Warren S, Thie NM, Magee DJ (2010) The association between neck disability and jaw disability. J Oral Rehabil 37(9):670–679. https://doi.org/10.1111/j.1365-2842.2010.02098.x
da Costa DR, de Lima Ferreira AP, Pereira TA, Porporatti AL, Conti PC, Costa YM, Bonjardim LR (2015) Neck disability is associated with masticatory myofascial pain and regional muscle sensitivity. Arch Oral Biol 60(5):745–752. https://doi.org/10.1016/j.archoralbio.2015.02.009
Acknowledgements
This study was presented in 20th Turkish National Rheumatology Congress, 16–20 October 2019 as poster presentation (poster number: PP-250). There is no external editing support and/or statistical analyses support by any agents and agencies.
Funding
None.
Author information
Authors and Affiliations
Contributions
All co-authors satisfy all four criteria (participated in study design, data collection, analysis, interpretation and writing equally), and take full responsibility for the integrity of the study and the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bilgin, E., Bilgin, E., Özdemir, O. et al. Temporomandibular disorders in ankylosing spondylitis: a cross-sectional, monocentric study. Rheumatol Int 40, 933–940 (2020). https://doi.org/10.1007/s00296-020-04563-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04563-y